Benefits of Pulmonary Rehabilitation in Patients with Idiopathic Pulmonary Fibrosis Receiving Antifibrotic Drug Treatment
Abstract
:1. Introduction
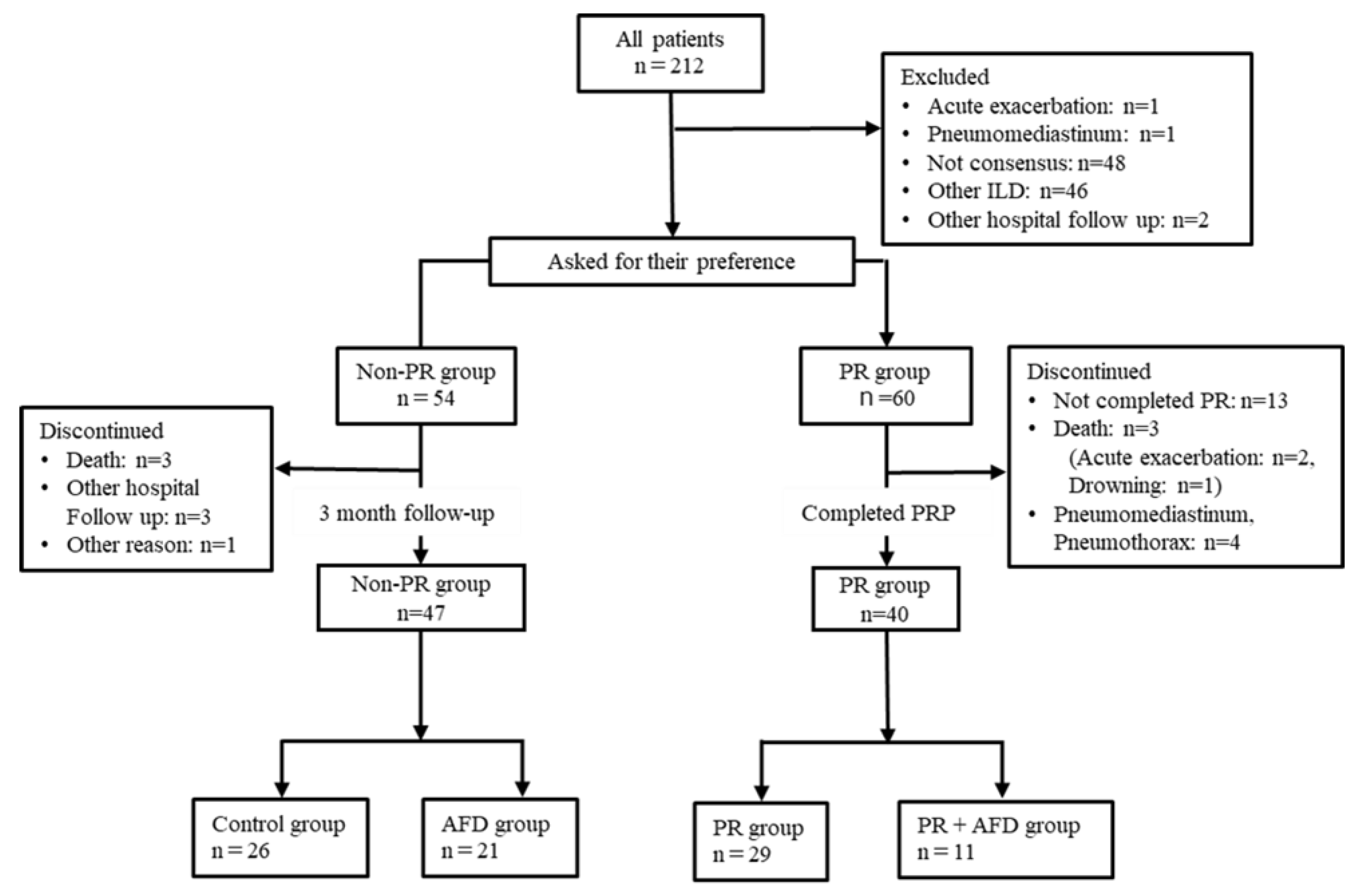
2. Materials and Methods
2.1. Study Design
2.2. Participants
2.3. Pulmonary Rehabilitation Program
2.4. Measurements
2.5. Statistical Analysis
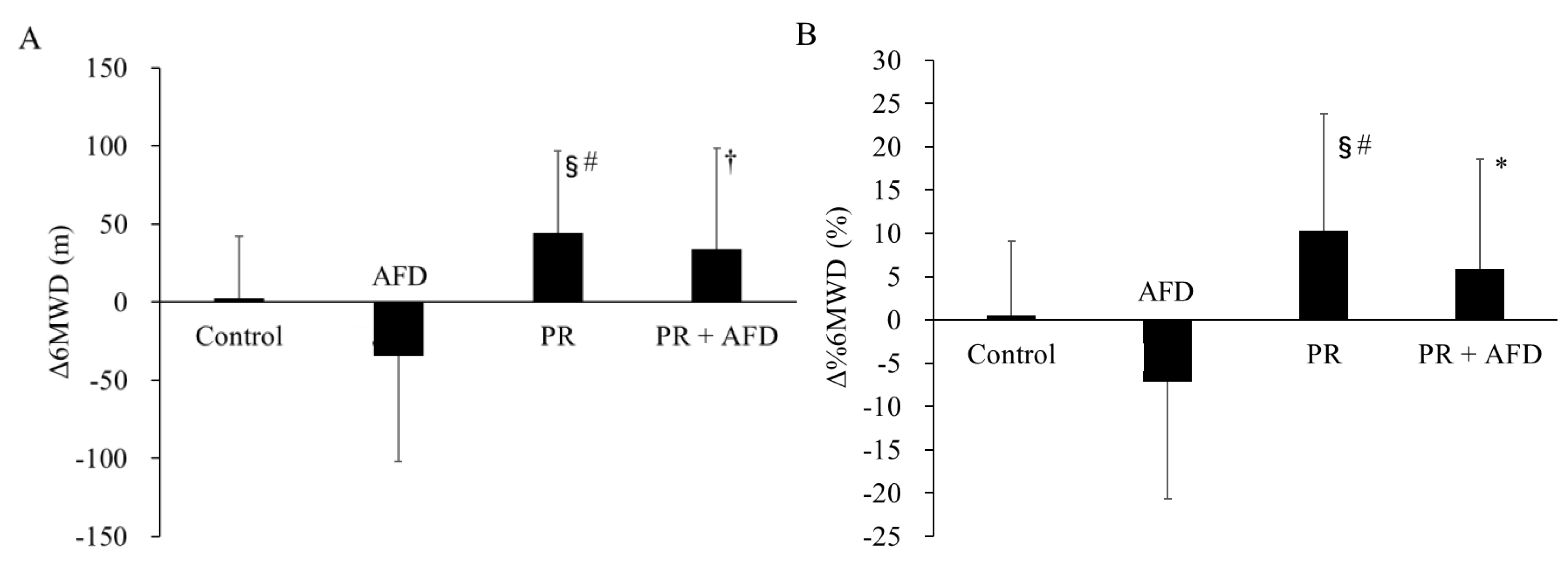
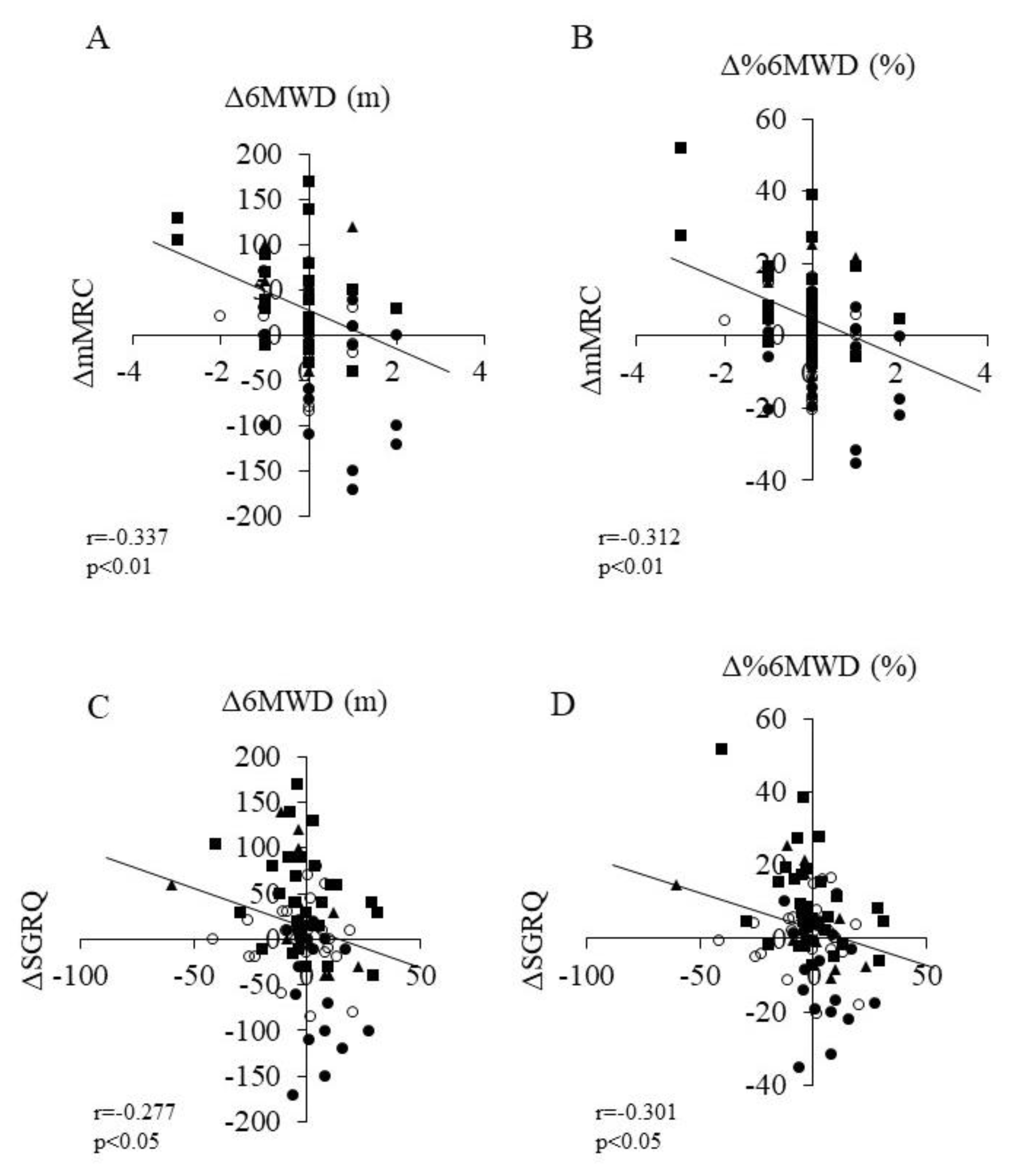
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Raghu, G.; Remy-Jardin, M.; Myers, J.L.; Richeldi, L.; Ryerson, C.J.; Lederer, D.J.; Behr, J.; Cottin, V.; Danoff, S.K.; Morell, F.; et al. Diagnosis of Idiopathic Pulmonary Fibrosis. An Official ATS/ERS/JRS/ALAT Clinical Practice Guideline. Am. J. Respir. Crit. Care Med. 2018, 198, e44–e68. [Google Scholar] [CrossRef] [PubMed]
- Raghu, G.; Rochwerg, B.; Zhang, Y.; Cuello-Garcia, C.; Azuma, A.; Behr, J.; Brozek, J.L.; Collard, H.R.; Cunningham, W.; Homma, S.; et al. An Official ATS/ERS/JRS/ALAT Clinical Practice Guideline: Treatment of Idiopathic Pulmonary Fibrosis. An Update of the 2011 Clinical Practice Guideline. Am. J. Respir. Crit. Care Med. 2015, 192, e3–e19. [Google Scholar] [CrossRef] [PubMed]
- Natsuizaka, M.; Chiba, H.; Kuronuma, K.; Otsuka, M.; Kudo, K.; Mori, M.; Bando, M.; Sugiyama, Y.; Takahashi, H. Epidemiologic Survey of Japanese Patients with Idiopathic Pulmonary Fibrosis and Investigation of Ethnic Differences. Am. J. Respir. Crit. Care Med. 2014, 190, 773–779. [Google Scholar] [CrossRef] [PubMed]
- King, T.E., Jr.; Bradford, W.Z.; Castro-Bernardini, S.; Fagan, E.A.; Glaspole, I.; Glassberg, M.K.; Gorina, E.; Hopkins, P.M.; Kardatzke, D.; Lancaster, L.; et al. A phase 3 trial of pirfenidone in patients with idiopathic pulmonary fibrosis. N. Engl. J. Med. 2014, 370, 2083–2092. [Google Scholar] [CrossRef]
- Richeldi, L.; Costabel, U.; Selman, M.; Kim, D.S.; Hansell, D.M.; Nicholson, A.G.; Brown, K.K.; Flaherty, K.R.; Noble, P.W.; Raghu, G.; et al. Efficacy of a Tyrosine Kinase Inhibitor in Idiopathic Pulmonary Fibrosis. N. Engl. J. Med. 2011, 365, 1079–1087. [Google Scholar] [CrossRef]
- Richeldi, L.; Du Bois, R.M.; Raghu, G.; Azuma, A.; Brown, K.K.; Costabel, U.; Cottin, V.; Flaherty, K.R.; Hansell, D.M.; Inoue, Y.; et al. Efficacy and Safety of Nintedanib in Idiopathic Pulmonary Fibrosis. N. Engl. J. Med. 2014, 370, 2071–2082. [Google Scholar] [CrossRef]
- Aravena, C.; Labarca, G.; Venegas, C.; Arenas, A.; Rada, G. Correction: Pirfenidone for Idiopathic Pulmonary Fibrosis: A Systematic Review and Meta-Analysis. PLoS ONE 2015, 10, e0140288. [Google Scholar]
- Homma, S.; Bando, M.; Azuma, A.; Sakamoto, S.; Sugino, K.; Ishii, Y.; Izumi, S.; Inase, N.; Inoue, Y.; Ebina, M.; et al. Japanese guideline for the treatment of idiopathic pulmonary fibrosis. Respir. Investig. 2018, 56, 268–291. [Google Scholar] [CrossRef]
- Dowman, L.; Hill, C.J.; May, A.; Holland, A.E. Pulmonary rehabilitation for interstitial lung disease. Cochrane Database Syst Rev. 2021, 2, CD006322. [Google Scholar] [CrossRef]
- Yu, X.; Li, X.; Wang, L.; Liu, R.; Xie, Y.; Li, S.; Li, J. Pulmonary Rehabilitation for Exercise Tolerance and Quality of Life in IPF Patients: A Systematic Review and Meta-Analysis. BioMed Res. Int. 2019, 2019, 8498603. [Google Scholar] [CrossRef]
- Kozu, R.; Senjyu, H.; Jenkins, S.C.; Mukae, H.; Sakamoto, N.; Kohno, S. Differences in response to pulmonary rehabilitation in idiopathic pulmonary fibrosis and chronic obstructive pulmonary disease. Respiration 2011, 81, 196–205. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Noble, P.W.; Albera, C.; Bradford, W.Z.; Costabel, U.; Du Bois, R.M.; Fagan, E.A.; Fishman, R.S.; Glaspole, I.; Glassberg, M.K.; Lancaster, L.; et al. Pirfenidone for idiopathic pulmonary fibrosis: Analysis of pooled data from three multinational phase 3 trials. Eur. Respir. J. 2015, 47, 243–253. [Google Scholar] [CrossRef]
- Kreuter, M.; Wuyts, W.A.; Wijsenbeek, M.; Bajwah, S.; Maher, T.; Stowasser, S.; Male, N.; Stansen, W.; Schoof, N.; Orsatti, L.; et al. Health-related quality of life and symptoms in patients with IPF treated with nintedanib: Analyses of patient-reported outcomes from the INPULSIS® trials. Respir. Res. 2020, 21, 36. [Google Scholar] [CrossRef] [PubMed]
- Igarashi, A.; Iwanami, Y.; Sugino, K.; Gocho, K.; Homma, S.; Ebihara, S. Using 6-Min Walk Distance Expressed as a Percentage of Reference to Evaluate the Effect of Pulmonary Rehabilitation in Elderly Patients With Interstitial Lung Disease. J. Cardiopulm. Rehabilitation Prev. 2018, 38, 342–347. [Google Scholar] [CrossRef] [PubMed]
- Miller, M.R.; Hankinson, J.; Brusasco, V.; Burgos, F.; Casaburi, R.; Coates, A.; Crapo, R.; Enright, P.; Van Der Grinten, C.P.M.; Gustafsson, P.; et al. Standardisation of spirometry. Eur. Respir. J. 2005, 26, 319–338. [Google Scholar] [CrossRef]
- MacIntyre, N.; Crapo, R.O.; Viegi, G.; Johnson, D.C.; Van Der Grinten, C.P.M.; Brusasco, V.; Burgos, F.; Casaburi, R.; Coates, A.; Enright, P.; et al. Standardisation of the single-breath determination of carbon monoxide uptake in the lung. Eur. Respir. J. 2005, 26, 720–735. [Google Scholar] [CrossRef]
- Ley, B.; Ryerson, C.J.; Vittinghoff, E.; Ryu, J.; Tomassetti, S.; Lee, J.S.; Poletti, V.; Buccioli, M.; Elicker, B.M.; Jones, K.D.; et al. A Multidimensional Index and Staging System for Idiopathic Pulmonary Fibrosis. Ann. Intern. Med. 2012, 156, 684–691. [Google Scholar] [CrossRef]
- Natori, H.; Kawayama, T.; Suetomo, M.; Kinoshita, T.; Matsuoka, M.; Matsunaga, K.; Okamoto, M.; Hoshino, T. Evaluation of the Modified Medical Research Council Dyspnea Scale for Predicting Hospitalization and Exacerbation in Japanese Patients with Chronic Obstructive Pulmonary Disease. Intern. Med. 2016, 55, 15–24. [Google Scholar] [CrossRef]
- Dowman, L.; McDonald, C.F.; Hill, C.J.; Lee, A.; Barker, K.; Boote, C.; Glaspole, I.; Goh, N.; Southcott, A.; Burge, A.; et al. Reliability of the hand held dynamometer in measuring muscle strength in people with interstitial lung disease. Physiotherapy 2015, 102, 249–255. [Google Scholar] [CrossRef]
- Ringbaek, T.; Martinez, G.; Lange, P. A comparison of the assessment of quality of life with CAT, CCQ, and SGRQ in COPD patients participating in pulmonary rehabilitation. COPD J. Chronic Obstr. Pulm. Dis. 2012, 9, 12–15. [Google Scholar] [CrossRef]
- Jones, P.W.; Quirk, F.H.; Baveystock, C.M.; Littlejohns, P. A self-complete measure of health status for chronic airflow limitation: The St. George’s Respiratory Questionnaire. Am. Rev. Respir. Dis. 1992, 145, 1321–1327. [Google Scholar] [CrossRef]
- Chang, J.A.; Curtis, J.R.; Patrick, D.L.; Raghu, G. Assessment of health-related quality of life in patients with interstitial lung disease. Chest 1999, 116, 1175–1182. [Google Scholar] [CrossRef] [PubMed]
- Nagata, K.; Tomii, K.; Otsuka, K.; Tachikawa, R.; Otsuka, K.; Takeshita, J.; Tanaka, K.; Matsumoto, T.; Monden, K. Evaluation of the chronic obstructive pulmonary disease assessment test for measurement of health-related quality of life in patients with interstitial lung disease. Respirology 2012, 17, 506–512. [Google Scholar] [CrossRef] [PubMed]
- ATS Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories. ATS statement: Guidelines for the six-minute walk test. Am. J. Respir. Crit. Care Med. 2002, 166, 111–117. [Google Scholar] [CrossRef] [PubMed]
- Enright, P.L. The six-minute walk test. Respir Care 2003, 48, 783–785. [Google Scholar]
- Noble, P.W.; Albera, C.; Bradford, W.Z.; Costabel, U.; Glassberg, M.K.; Kardatzke, D.; King, T.E., Jr.; Lancaster, L.; Sahn, S.A.; Szwarcberg, J.; et al. Pirfenidone in patients with idiopathic pulmonary fibrosis (CAPACITY): Two randomised trials. Lancet 2011, 377, 1760–1769. [Google Scholar] [CrossRef]
- Swigris, J.J.; Wamboldt, F.S.; Behr, J.; Du Bois, R.M.; King, T.E.; Raghu, G.; Brown, K.K. The 6 minute walk in idiopathic pulmonary fibrosis: Longitudinal changes and minimum important difference. Thorax 2009, 65, 173–177. [Google Scholar] [CrossRef]
- Eakin, E.G.; Resnikoff, P.M.; Prewitt, L.M.; Ries, A.L.; Kaplan, R.M. Validation of a new dyspnea measure: The UCSD Shortness of Breath Questionnaire. University of California, San Diego. Chest 1998, 113, 619–624. [Google Scholar] [CrossRef]
- Jones, P.W. Health status measurement in chronic obstructive pulmonary disease. Thorax 2001, 56, 880–887. [Google Scholar] [CrossRef]
- Verma, G.; Marras, T.; Chowdhury, N.; Singer, L. Health-related quality of life and 6 min walk distance in patients with idiopathic pulmonary fibrosis. Can. Respir J. 2011, 18, 283–287. [Google Scholar] [CrossRef]
- Brunetti, G.; Malovini, A.; Maniscalco, M.; Balestrino, A.; Carone, M.; Visca, D.; Capelli, A.; Vitacca, M.; Bellazzi, R.; Piaggi, G.; et al. Pulmonary rehabilitation in patients with interstitial lung diseases: Correlates of success. Respir. Med. 2021, 185, 106473. [Google Scholar] [CrossRef] [PubMed]
- Nishiyama, O.; Kataoka, K.; Ando, M.; Arizono, S.; Morino, A.; Nishimura, K.; Ogawa, T.; Shiraki, A.; Watanabe, F.; Kozu, R.; et al. Protocol for long-term effect of pulmonary rehabilitation under nintedanib in idiopathic pulmonary fibrosis. ERJ Open Res. 2021, 7, 00321–2021. [Google Scholar] [CrossRef] [PubMed]
| All (n = 87) | Control (n = 26) | AFD (n = 21) | PR (n = 29) | PR+AFD (n =11) | p Value | |
|---|---|---|---|---|---|---|
| Age, year | 72.0 ± 8.1 | 73.0 ± 8.5 | 70.3 ± 6.6 | 73.5 ± 8.9 | 69.0 ± 7.4 | 0.29 a |
| Sex, male/female | 61/26 | 14/12 | 18/3 | 18/11 | 11/0 | <0.05 b |
| BMI, kg/m2 | 22.9 ± 3.9 | 24.0 ± 3.6 | 22.3 ± 4.2 | 22.5 ± 3.9 | 22.5 ± 4.1 | 0.38 a |
| Oxygen use (%) | 21 (30) | 3 (15) | 6 (40) | 9 (33) | 3 (37.5) | 0.34 b |
| Smoking status (current/former/never) | 1/44/25 | 1/13/12 | 0/14/7 | 0/19/10 | 0/9/2 | 0.47 b |
| Medications | ||||||
| Azathioprine | 0 | 0 | 0 | 0 | 0 | |
| Cyclophosphamide | 0 | 0 | 0 | 0 | 0 | |
| Cyclosporine | 2 | 1 | 0 | 1 | 0 | |
| Tacrolimus | 0 | 0 | 0 | 0 | 0 | |
| Prednisolone | 19 | 5 | 6 | 3 | 4 | |
| Pirfenidone | 15 | 0 | 10 | 0 | 5 | |
| Nintedanib | 17 | 0 | 11 | 0 | 6 | |
| N-Acetylcysteine | 18 | 4 | 4 | 6 | 2 | |
| Severity | ||||||
| GAP stage | 1.6 ± 0.7 | 1.4 ± 0.6 | 1.6 ± 0.7 | 1.7 ± 0.7 | 2.0 ± 0.7 | 0.15 a |
| (I/II/III) | 26/32/12 | 16/8/2 | 10/8/3 | 11/13/5 | 3/5/3 | |
| Pulmonary function | ||||||
| FVC, % pred | 77.1 ± 20.5 | 84.2 ± 18.2 | 71.6 ± 15.7 | 77.9 ± 23.2 | 68.5 ± 22.1 | 0.08 a |
| FEV1, % pred | 91.2 ± 22.6 | 95.7 ± 18.6 | 85.5 ± 17.3 | 95.1 ± 28.6 | 81.5 ± 19.5 | 0.15 a |
| FEV1/FVC, % | 86.1 ± 13.2 | 79.9 ± 8.0 c | 90.5 ± 14.5 | 87.7 ± 15.7 | 88.3 ± 9.4 | <0.05 a |
| DLCO, % pred | 60.1 ± 21.1 | 69.6 ± 22.4 | 55.8 ± 22.1 | 57.8 ± 18.1 | 53.1 ± 18.9 | 0.056 a |
| PaO2, torr | 81.9 ± 13.4 | 86.1 ± 13.2 | 84.1 ± 14.2 | 77.2 ± 12.0 | 79.9 ± 13.8 | 0.07 a |
| PaCO2, torr | 41.7 ± 5.2 | 41.2 ± 4.1 | 41.4 ± 3.6 | 41.7 ± 6.7 | 43.7 ± 5.6 | 0.61 a |
| IP marker | ||||||
| KL-6, U/mL | 1040.3 ± 743.5 | 790.8 ± 428.0 | 1185.8 ± 921.6 | 1098.9 ± 759.5 | 1198.0 ± 859.2 | 0.22 a |
| SP-A, U/mL | 68.3 ± 30.9 | 67.6 ± 33.7 | 68.5 ± 36.5 | 67.5 ± 27.8 | 71.7 ± 22.7 | 0.98 a |
| SP-D, U/mL | 239.5 ± 163.6 | 176.7 ± 102.5 | 258.5 ±108.6 | 282.4 ± 236.9 | 239.1 ± 82.6 | 0.10 a |
| Control | AFD | PR | PR+AFD | |||||
|---|---|---|---|---|---|---|---|---|
| Baseline | 3 Months | Baseline | 3 Months | Baseline | 3 Months | Baseline | 3 Months | |
| mMRC scale | 1.3 ± 1.1 | 1.2 ± 0.9 | 1.4 ± 1.0 | 1.7 ± 1.2 | 1.5 ± 1.0 | 1.1 ± 0.8 a | 1.9 ± 1.1 | 1.7 ±1.1 |
| 6 min walk test | ||||||||
| 6MWD (m) | 410.5 ± 98.1 | 413.2 ± 112.3 | 409.2 ± 115.1 | 374.7 ± 155.2 | 365.8 ± 96.9 | 410.5 ± 107.1 b | 386.3 ± 91.1 | 420.4 ±124.4 |
| % 6MWD (%) | 86.0 ± 21.6 | 86.6 ± 24.8 | 83.1 ± 21.2 | 76.0 ± 30.4 | 73.5 ± 20.2 | 84.1 ± 23.7 b | 78.5 ± 16.5 | 84.5 ±19.1 |
| Muscle strength | ||||||||
| QF (Nm/kg) | 1.2 ± 0.4 | 1.2 ± 0.5 | 1.3 ± 0.3 | 1.4 ± 0.5 | 1.3 ± 0.4 | 1.3 ± 0.3 | 1.3 ± 0.5 | 1.3 ±0.6 |
| HGS (kg) | 24.0 ± 7.8 | 24.2 ± 7.8 | 29.1 ± 7.3 | 28.5 ± 7.0 | 26.2 ± 8.3 | 26.4 ± 8.0 | 29.4 ± 7.7 | 30.2 ±7.8 |
| HRQOL | ||||||||
| SGRQ total | 32.3 ± 20.1 | 30.3 ± 16.5 | 38.3 ± 21.1 | 42.9 ± 20.4 | 39.6 ± 18.5 | 40.0 ± 20.2 | 52.1 ± 20.2 | 52.0 ±20.2 |
| CAT | 11.8 ± 9.1 | 11.8 ± 7.5 | 13.2 ± 9.1 | 15.9 ± 7.2 c | 14.0 ±7.4 | 14.5 ± 7.4 | 20.1 ± 9.5 | 21.5 ±10.2 |
| Control | AFD | PR | PR+AFD | |
|---|---|---|---|---|
| Dyspnea | ||||
| ΔmMRC scale | −0.07 ± 0.6 | 0.3 ± 0.9 a | −0.4 ± 0.9 | −0.1 ± 0.6 |
| (−0.3 to 0.2) | (−0.1 to 0.7) | (−0.7 to −0.06) | (−0.5 to 0.2) | |
| Peripheral muscle strength | ||||
| ΔQF (Nm/kg) | 0.06 ± 0.2 | 0.1 ± 0.4 | −0.01 ±0.3 | −0.04 ± 0.4 |
| (−0.03 to 0.1) | (−0.08 to 0.3) | (−0.1 to 0.1) | (−0.3 to 0.3) | |
| ΔHGS (kg) | 0.2 ± 2.8 | −0.5 ± 2.8 | 0.2 ± 2.1 | 0.6 ± 1.5 |
| (−0.9 to 1.3) | (−1.8 to 0.7) | (−0.5 to 1.0) | (−0.2 to 1.8) | |
| HRQOL | ||||
| ΔSGRQ total | −1.9 ± 13.7 | 4.5 ± 9.6 | 0.4 ± 14.9 | −0.04 ± 12.5 |
| (−7.5 to 3.6) | (0.7 to 8.9) | (−5.2 to 6.0) | (−8.4 to 8.4) | |
| ΔCAT | −0.03 ± 6.2 | 2.6 ± 5.6 | 0.5 ± 6.6 | 1.3 ± 7.6 |
| (−2.5 to 2.4) | (0.04 to 5.1) | (−2.0 to 3.0) | (−3.7 to 6.5) |
| AFD | PR+AFD | p Value | |
|---|---|---|---|
| Duration of AFD treatment at baseline, (days) | 6.9 ±13.4 | 6.2 ±15.2 | 0.85 a |
| Number of patients with adverse events, n (%) | 0.37 b | ||
| (−) | 12 (57.1) | 4 (36.3) | |
| (+) | 9 (42.8) | 7 (63.6) | |
| Adverse events | |||
| Nausea, n (%) | 0 | 1 (9.0) | 0.16 b |
| Diarrhea, n (%) | 5 (23.8) | 3 (27.2) | 0.37 b |
| Liver dysfunction, n (%) | 3 (14.2) | 1 (9.0) | 0.67 b |
| Decreased appetite, n (%) | 2 (9.5) | 3 (27.2) | 0.18 b |
| Fatigue, n (%) | 0 | 1 (9.0) | 0.16 b |
| Dizziness, n (%) | 0 | 1 (9.0) | 0.16 b |
| Photosensitivity reaction, n (%) | 1 (4.7) | 0 | 0.46 b |
| Thrombocytopenia, n (%) | 0 | 1 (9.0) | 0.16 b |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Iwanami, Y.; Ebihara, K.; Nakao, K.; Sato, N.; Miyagi, M.; Nakamura, Y.; Sakamoto, S.; Kishi, K.; Homma, S.; Ebihara, S. Benefits of Pulmonary Rehabilitation in Patients with Idiopathic Pulmonary Fibrosis Receiving Antifibrotic Drug Treatment. J. Clin. Med. 2022, 11, 5336. https://doi.org/10.3390/jcm11185336
Iwanami Y, Ebihara K, Nakao K, Sato N, Miyagi M, Nakamura Y, Sakamoto S, Kishi K, Homma S, Ebihara S. Benefits of Pulmonary Rehabilitation in Patients with Idiopathic Pulmonary Fibrosis Receiving Antifibrotic Drug Treatment. Journal of Clinical Medicine. 2022; 11(18):5336. https://doi.org/10.3390/jcm11185336
Chicago/Turabian StyleIwanami, Yuji, Kento Ebihara, Keiko Nakao, Naofumi Sato, Midori Miyagi, Yasuhiko Nakamura, Susumu Sakamoto, Kazuma Kishi, Sakae Homma, and Satoru Ebihara. 2022. "Benefits of Pulmonary Rehabilitation in Patients with Idiopathic Pulmonary Fibrosis Receiving Antifibrotic Drug Treatment" Journal of Clinical Medicine 11, no. 18: 5336. https://doi.org/10.3390/jcm11185336
APA StyleIwanami, Y., Ebihara, K., Nakao, K., Sato, N., Miyagi, M., Nakamura, Y., Sakamoto, S., Kishi, K., Homma, S., & Ebihara, S. (2022). Benefits of Pulmonary Rehabilitation in Patients with Idiopathic Pulmonary Fibrosis Receiving Antifibrotic Drug Treatment. Journal of Clinical Medicine, 11(18), 5336. https://doi.org/10.3390/jcm11185336






