Abstract
Background: To date, various forms of physiotherapy are used in the treatment of cubital tunnel syndrome (CuTS). The effectiveness of physiotherapy for CuTS is inconclusive. The aim of this systematic review was to evaluate the effects of physiotherapy in the conservative treatment of CuTS. Methods: The six databases were searched from December 2020 to March 2022. The inclusion criteria were randomised controlled trials, case series, and case reports that evaluate the effects of physiotherapy in the treatment of adult participants with diagnosis CuTS. A total of 11 studies met the eligibility criteria, capturing a total of 187 participants. Results: In three types of papers, pain, muscle strength, and limitation of upper limb function were the most frequently assessed characteristics. Physiotherapy was most often based on manual therapy, neurodynamic techniques, and electrical modalities. One clinical trial rated the risk of bias “high” and the other two “some concerns”. In case-series designs, five studies rated the risk of bias as “serious” and three as “moderate”. Most of the studies showed a significant improvement in the clinical condition, also in the follow-up study. Only one clinical trial showed no therapeutic effect. Conclusion: There is no possibility of recommending the best method of physiotherapy in clinical practice for people with CuTS based on the results of this systematic review. More high-quality studies are required.
1. Introduction
Cubital tunnel syndrome (CuTS) is a compressive neuropathy of the ulnar nerve. It is the second most prevalent peripheral neuropathy of the upper extremity after carpal tunnel syndrome [1,2]. The mean annual incidence of CuTS is estimated at 24.7 cases per 100,000 people [3], and its prevalence is 2–6% in the general population [4]. In the early stages of CuTS, sensory symptoms such as paraesthesia and slight hypoesthesia are reported, occurring mostly paroxysmally and related to the position of the elbow. Over time, these symptoms worsen. This is followed by motor disturbances, mostly weakness and atrophy of the intrinsic muscles of the hand [1,5]. The stages of this neuropathy can be divided into three degrees of severity: mild, moderate, and severe [6]. The progressive course of CuTS over time leads to the impairment of hand function, which adversely affects the activities of daily living, and professional life, and deteriorates the overall health-related quality of life. With the significant prevalence of CuTS, this neuropathy is a major medical, economic, and social problem.
CuTS is referred to as compression neuropathy that occurs around the cubital tunnel. The most common sites of potential compression of the ulnar nerve are the arcade of Struthers, the medial intermuscular septum, the medial epicondyle, the cubital tunnel, and the deep flexor–pronator aponeurosis [7]. This neuropathy is usually divided into primary (idiopathic) and secondary (symptomatic) [8]. In idiopathic forms of CuTS, no morphological abnormalities can be found in the tissues surrounding the ulnar nerve [8]. Furthermore, there are several causes of secondary forms of CuTS (anatomical changes after trauma, degenerative changes, systemic diseases such as rheumatoid arthritis, lipomas, ganglion cysts, inflammatory processes, etc.) [8,9,10]. Other risk factors for CuTS are related to upper extremity motor activity, overhead activity, heavy physical work, obesity, and nicotinism [11]. Therefore, it can be concluded that CuTS is just a synonym for ulnar nerve neuropathy occurring in the elbow area. The difficulty in finding the aetiology of CuTS also affects the choice of the most appropriate treatment modality for this neuropathy.
The treatment of CuTS is divided into surgical and conservative [12]. Palmer and Hughes [10] showed various surgical techniques for ulnar nerve decompression and emphasised that no “gold standard” for surgical treatment has been developed to date. In situ decompression, intramuscular transposition, subcutaneous transposition, submuscular transposition, medial epicondylectomy, and endoscopic techniques are most commonly used [10]. However, surgical treatment is only recommended when muscle strength is weakened, and conservative methods do not bring the expected therapeutic effect [13]. Hence, conservative treatment is used as first-line therapy, usually in the early and mild-to-moderate stages of CuTS [5]. Conservative treatment includes modification of activities of daily living with the avoidance of prolonged elbow joint flexion [10], nonsteroidal anti-inflammatory drugs, steroid injections, and physical therapy approaches [14]. To the best of our knowledge, there is also no standardised procedure for CuTS conservative treatment with well-documented effectiveness. It seems that physiotherapy is one of the most important forms of conservative treatment, which has been proven to be effective in other peripheral neuropathies [15,16,17,18,19]. To date, various forms of physiotherapy have been used in the treatment of CuTS [20,21,22,23]. However, the effectiveness of physiotherapy intervention as a conservative treatment of CuTS is inconclusive. Therefore, it was decided to conduct, for the first time, a systematic review of papers evaluating the effectiveness of physiotherapy treatment for CuTS. Such an analysis determines the quality of the research conducted to date and provides directions for future research.
2. Methods
This systematic review adheres to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement [24]. The protocol was registered in the International Prospective Register of Systematic Reviews (PROSPERO) database, registration number CRD 42020219297.
2.1. Data Sources and Searchers
The literature review was conducted between December 2020 and March 2022. Six electronic databases (MEDLINE via PubMed, Cochrane, Embase, Web of Science, Scopus, and PEDro) were searched to identify relevant papers. The search strategy was developed during a panel meeting after an initial article search. It was based on the use of key phrases and/or their abbreviations based on a metadata system (MeSH) and various combinations of these phrases to increase search efficiency. An extensive list of terms to describe the target population based on the PICO acronym was formulated:
- P (population)—cubital tunnel syndrome;
- I (intervention)—physiotherapy treatment;
- C (comparator)—control group, placebo group, and sham therapy;
- O (outcomes)—nerve conduction study, discrimination and threshold sensation, functional assessment, and ultrasound imaging measurements (Supplementary Material S1).
All papers were accepted regardless of the year of publication. However, the search was limited to papers available in English. Titles and abstracts of scientific papers retrieved from the databases were analysed for inclusion criteria. The papers that did not show relevance to the subject area studied were excluded. The lists of references in the publications included in the review were also analysed to make sure that other papers that may meet the inclusion criteria were not missed. The resulting papers were combined using the EndNote x9 software (version 19.2.0.13018, Philadelphia, PA, USA).
2.2. Study Selection
The review of the retrieved papers was conducted in two stages. The first step was to review the titles and abstracts of papers identified as potentially relevant to the research questions. In the next step, the full texts of the papers identified during the initial selection were reviewed. In both stages, the review was performed by two independent reviewers (T.W., T.B.), and by a third independent reviewer (P.L.) in contentious cases. The inclusion criteria were all experimental studies such as randomised controlled trials (RTCs) and case reports that evaluate the effects of physiotherapy in the treatment of adult participants (>16 years old) with diagnosis CuTS. Participants not diagnosed as CuTS or exposed to any form of surgical procedure and/or with other neuropathies of the upper limb were excluded from the study. The characteristics of the RTC and CS types of studies were presented separately.
2.3. Data Extraction
Two reviewers independently extracted and documented data from each included study using Excel (Microsoft, Redmond, WA, USA) according to the Centre for Reviews and Dissemination recommendations [25]. We extracted data including the year of publication, study design, sample size, gender, age, target population, description of interventions, outcome measures, and study results. The main study outcomes expressed as means and SDs were also extracted.
2.4. Methodological Quality Assessment
The methodological quality of randomised clinical trials was assessed using the revised Cochrane risk-of-bias tool for randomised trials (RoB 2) [26]. According to the Cochrane guidelines, this tool evaluates possible errors as follows: “low risk”, “some concern”, or “high risk”. Due to the fact that the remaining works that qualified for the review were case studies, their quality was assessed in two stages. In the first stage, the article quality was assessed using The Critical Appraisal Checklist for Case Reports developed by Moola et al. [27]. If five of the eight evaluation criteria are met, the quality is assessed as satisfactory (such a study was included). In the second stage, the quality was assessed using the Risk of Bias in Non-randomised Studies of Interventions (ROBINS-I) assessment tool [28]. This tool evaluates possible errors as follows: “low risk of bias”, “moderate risk of bias”, “serious risk of bias”, “critical risk of bias”, or “no information”. In both cases, the evaluation was conducted by two independent reviewers (T.W. and T.B.). The Cohen κ statistic was applied to determine the agreement between assessors.
2.5. Data Synthesis and Analysis
The extracted data from all included studies were tabulated, including the study authors and sample characteristics, the measurements of the outcome variables, and key results. All the identified studies were included in a qualitative synthesis and are presented in the tables. Initially, it was intended to synthesise the data quantitatively by conducting a meta-analysis. However, because of high heterogeneity in terms of study design, population examined, and various interventions, we could not perform a meta-analysis.
3. Results
3.1. Study Selection
An initial search of the databases together with a manual search and analysis of the references identified 1719 papers. This number was reduced to 995 after deleting duplicates. Based on exclusion and qualification criteria, 16 papers met the eligibility criteria (Figure 1). Of these papers, five were excluded after further analysis because they neither concerned CuTS patients nor addressed physiotherapy management. One paper discussed ulnar tunnel syndrome, another described the case of a patient who developed CuTS due to venous thrombosis, while another dealt with the ultrasonographic diagnosis of CuTS. One paper focused on the surgical treatment of CuTS caused by anconeus epitrochlearis, and one evaluated the effectiveness of electrostimulation after traumatic ulnar nerve injury. Finally, 11 articles were included in the final review comprising 3 RCT-type studies [13,29,30] (Table 1) and 8 case-series-type studies [20,21,22,23,31,32,33,34] (Table 2).
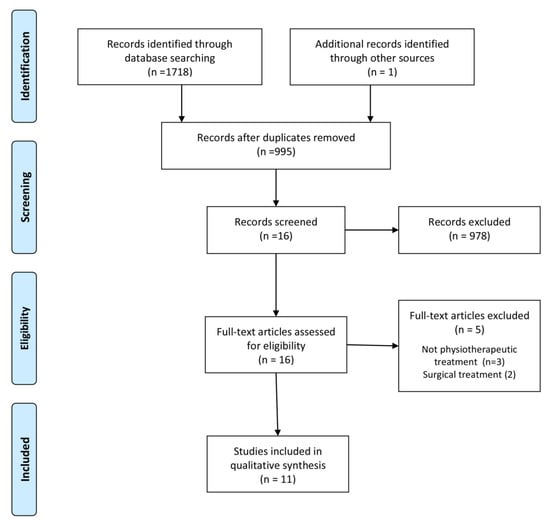
Figure 1.
Flowchart.

Table 1.
Characteristics of included randomised clinical trials (RTCs).

Table 2.
Characteristics of included case studies design.
3.2. Randomised Controlled Trials
3.2.1. Participants
In all RCTs, the subjects were clinically/neurophysiologically diagnosed with CuTS (two studies clinically and neurophysiologically; one study only clinically). A total of 163 subjects aged 16–79 years old were examined and underwent therapy. The RCT involved 87 women and 76 men [13,29,30].
3.2.2. Outcome Measures
All studies evaluated pain (3/3 papers) and muscle strength (3/3 papers) [13,29,30]. Two papers evaluated upper extremity function and nerve conduction [13,30]. In addition, one study assessed sensory threshold [30] and overall health quality [29].
3.2.3. Interventions
Each study used a different therapeutic procedure: orthosis (experimental intervention), neurodynamic techniques (experimental intervention), ergonomic physical activity instruction (control group) [13], continuous shortwave diathermy (experimental intervention) and placebo (control group) [29], and low-level laser therapy (experimental intervention) and ultrasound (experimental intervention) [30].
3.2.4. Risk of Bias
Based on the reviewers’ assessment using the ROB 2 tool to evaluate the risk of bias, the overall bias was considered to be “high” in one study [13], while “some concerns” were indicated in the remaining two RCTs [29,30] (Table 3). The most common flaws were the high risk of bias in domain 4 (risk of bias in measurement of the outcome) in one RTC [13] and domain 2 (risk of bias due to deviations from the intended interventions) in all RTC studies [13,29,30].

Table 3.
Risk of Bias in randomised clinical trials (RTCs).
3.2.5. Synthesis of the Results
Two RCTs reported significant improvements in the clinical condition of the subjects (pain reduction, improved function, increase in muscle strength, improvement in the sensory threshold, and improvement in nerve conduction), which occurred not only after the therapy but also persisted at 1, 3, and 6 months of follow-up [13,30]. In one study, there were no changes in pain muscle strength, function, and overall health evaluated after therapy in comparison with the control group [29].
3.3. Case Studies
In all case series [21,22] and case reports [20,23,31,32,33,34], subjects were clinically and neurophysiologically diagnosed with CuTS (four studies clinically and neurophysiologically; four studies only clinically). In eight case studies, 24 subjects ranging in age from 17 to 71 years were examined and treated. The gender of the subjects was determined in six of the eight papers [20,23,31,32,33,34]. Studies by Oskay et al. and Shen et al. [21,22] failed to specify gender. In total, 48 women and 5 men participated in the study, and in 14 cases, the gender was not specified.
3.3.1. Outcome Measures
The most frequently evaluated symptom was pain (six of the eight papers) [20,21,22,23,33,34]. Symptom provocation tests (five of the eight papers) [20,21,31,32,34] and functional limitations of the upper extremity (five of the eight papers) were also frequently assessed [21,22,23,32,34]. Muscle strength was assessed in three of the eight papers [21,23,31]. Range of motion was assessed in two papers [20,32] as was the severity of paraesthesia [20,31]. In two of the eight papers, authors evaluated subjective improvements following therapy [23,33]. Furthermore, one study evaluated nerve conduction [33] and sensory threshold [21].
3.3.2. Interventions
Neurodynamic techniques (3/8 papers) [21,32,34] and chiropractic manipulation (two of the eight papers) [20,31] were the most frequently used in therapy. Other papers used dry needling [23], percutaneous electrical stimulation [34], pulsed radiofrequency [33], combined ultrasound and cold therapy [21], and extracorporeal shock wave therapy [22].
3.3.3. Therapeutic Effect
In all case studies, significant improvements in the clinical status of the subjects (reduction in pain and subjective symptoms, improved function, increase in grip and pinch strength, reduction in symptoms in provocation tests such as Tinel’s sign or elbow flexion test) were reported, which occurred not only after therapy [20,21,22,23,31,32,33] but were also maintained in the 6-, 8-, 10- and 12-month follow-up periods [21,22,23,32,33,34].
3.3.4. Risk of Bias
The Critical Appraisal Checklist for Case Reports values ranged from 5 to 7 in all case studies, which was considered sufficient [20,21,22,23,31,32,33,34] (Table 4). In the second stage based on the reviewer’s evaluation using the ROBINS-I tool for non-randomised studies of interventions to evaluate the risk of bias, the overall bias was serious in five of the eight papers [20,21,31,32,34] and moderate in three of them [22,23,33] (Table 5). The most common flaws were a serious risk of bias in “bias due to confounding” in five of the eight studies [20,21,31,32,34]; “bias in classification of interventions” in five out of the total eight papers [20,21,31,32,34]; “bias due to deviations from intended interventions” in five of the eight studies [20,21,32,34]; “bias in measurement of outcomes” in another combination of five studies out of the total eight [20,21,31,32,34], and the “overall bias” in five of the eight papers [20,21,31,32,34].

Table 4.
Critical appraisal checklist for case studies design.

Table 5.
Risk of bias in case studies design.
4. Discussion
The aim of the present systematic review was to evaluate the effects of physiotherapy in the conservative treatment of CuTS. Based on the search strategy used, 11 papers were included in the review, consisting of 3 RCTs [13,29,30] 2 case series [21,22], and 6 case reports [20,23,31,32,33,34]. In two-thirds (66.6%) of the RCT included, the authors reported beneficial effects immediately after physiotherapy and in the long-term in pain, function, muscle strength, sensory thresholds, and nerve conduction [13,30]. One RCT reported no significant treatment effect on pain scores, muscle strength, function, and health status [29]. In all case studies, the authors emphasised the positive effects of different physiotherapy procedures concerning the reduction in pain symptoms, improved function, increased pinch-grip strength, and a reduction in symptoms in provocation tests (Tinel’s sign, elbow flexion test), both immediately after treatment [20,21,22,23,31,32,33] and in the long-term follow-up [21,22,23,32,33,34].
Although 91% of the included papers reported beneficial effects of physiotherapy [13,20,21,22,23,31,32,33,34], the results obtained have to be viewed with caution. This is due to the fact that 73% of current publications were case studies [20,21,22,23,31,32,33,34] with small numbers of subjects (24 in total), very heterogeneous research methodology and physiotherapy programs, and a high risk of bias. Furthermore, 3 RCTs [13,29,30] examined 163 people, but even in this case, due to methodological differences, it is difficult to draw firm conclusions about the effectiveness of physiotherapy treatment in CuTS, particularly when one RCT did not observe any significant effect [29].
It should be pointed out that the method used for the diagnosis of CuTS was problematic in most of the papers included in the review. Although a nerve conduction study (NCS) was performed in 54% of papers [13,22,29,30,32,33], the result was negative in one paper, despite the symptoms that could indicate CuTS [32]. In the other papers, the diagnosis was based on clinical and orthopaedic examinations [20,21,23,31,34]. As NCS-based diagnosis of peripheral neuropathies is the gold standard [35] in some compression neuropathies (as is the case in CTS), it appears that it should also apply to other peripheral neuropathies. According to the accepted study protocol, it was decided to include the analysis papers in which patients were diagnosed as CuTS despite the absence of a nerve conduction study but only based on history and clinical and orthopaedic examinations. Therefore, the results of some studies and their findings must be viewed with caution. It seems that electrodiagnostic tests are necessary not only to make an accurate diagnosis of CuTS but also to assess the severity of the condition and objectively evaluate improvements after therapy [36]. Although some authors have demonstrated the high sensitivity and specificity of clinical tests in the diagnosis of CuTS [37,38], there is no agreement [39]. It is important to note that, regardless of the differences in the assessment of the various clinical tests, this will be a much more subjective assessment than it is in the case of NCS. Furthermore, NCS provides specific information such as conduction velocity in nerve fibres, latency, and amplitude, information that cannot be obtained from a functional test. However, it should also be noted that some authors indicated that symptoms often precede nerve conduction disturbances [40,41], especially in the early stages of peripheral neuropathy. In these cases, for obvious reasons, the diagnosis must be based only on clinical symptoms and orthopaedic examination, which can also explain the failure to use NCS study in some papers to some extent. It would be unethical to omit clinical cases or delay therapeutic management in patients who have subjective symptoms but do not have a disrupted NCS. On the other hand, the lack of a certain diagnosis does not allow the use of therapy aimed at the cause but only at reducing the patient’s symptoms.
Significant differences in the offered therapeutic programs are another major problem in assessing the effectiveness of physiotherapy approaches in CuTS based on the papers included in this review. In fact, it is difficult to find any similarities in the therapeutic programs used. In 64% of the papers, physiotherapy was based just on one form of therapy [13,20,22,23,29,30,33]. However, in each of them, this was a different type of therapy. The remaining 36% of papers [21,31,32,34] used a total of multiple therapeutic measures, not only targeting the elbow region but also the cervical spine and thorax [31,32]. Neurodynamic techniques were used in 36% of the papers [13,21,32,34] but with different methodologies and often as a component of other treatments. In 18% of the papers, neurodynamic techniques were used as a self-therapy program, which may make it even more difficult to control the correctness of their performance and regular use.
A major weakness of all qualified papers is their low methodological quality, which was confirmed by the RoB results. Regardless of study type (case series, case reports, or RCTs), low RoB was not reported in any of the papers included. Therefore, this review indicated a complete lack of high-quality studies evaluating the effectiveness of physiotherapy in the conservative treatment of CuTS. Taking into account the prevalence of CuTS and the strong evidence confirming the effectiveness of physiotherapy in other peripheral neuropathies [15,16,17,18,19], it is difficult to indicate the reason for such low interest in CuTS conservative treatment.
4.1. Limitations
This systematic review has some potential limitations. The number of papers included in the review was small, and only three RCTs were identified. The sample size was small, with only 186 subjects. Some of the papers lacked clinical information about the patients’ condition and severity of CuTS, which may have also affected the obtained results. The lack of an NCS study conducted not only to make an accurate diagnosis but also to assess the effects achieved after the therapeutic cycle is another limitation of many of the included papers and, thus, of the review itself. Only papers published in English were included in this review, which may have resulted in the omission of some studies evaluating the effectiveness of physiotherapy in the conservative treatment of CuTS. Further, the papers included in the review were characterised by different therapeutic programs, which made it difficult to assess the therapeutic effects.
4.2. Implications for Future Research
The results of this review allow for several recommendations for future research. First of all, there is a need for more well-designed RCT studies with two or more representative groups of subjects. Due to the prevalence of CuTS, case series and case reports have no substantive justification. It is also important to perform the diagnosis of CuTS based on NCS and ultrasound imaging, while clinical symptoms and other tests should be considered as supplementary information about the study population. The diagnosis of CuTS should be supplemented with the determination of the CuTS stage, which is also important in the assessment of the effectiveness of the offered therapy. Since most of the papers included in the review had a beneficial therapeutic effect, randomised controlled trials should be conducted based on similar therapeutic programs such as manual therapy including neurodynamic techniques, ultrasound therapy, low-level laser therapy, percutaneous electrical stimulation, or dry needling. Future studies should be multi-central and (if possible) blinded or even double-blinded.
5. Conclusions
Although physiotherapy could have the potential to demonstrate a positive effect in the treatment of CuTS, most published studies to date are of questionable methodological quality. Thus, at this stage of knowledge, there is no possibility to recommend the best method, duration, and interval of physiotherapy in the clinical practice of people with CuTS. More high-quality studies are required.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/jcm11144247/s1, Supplementary Material S1: Search terms and number of items identified in the PubMed database.
Author Contributions
Conceptualisation, T.W.; methodology, T.W., P.L., and M.D.; software, P.L. and A.G.; formal analysis, T.W. and P.L.; investigation, P.L., T.W., C.F.-d.-l.P., M.D., and T.B.; resources, M.D. and T.B.; data curation, M.D. and T.B.; writing—original draft preparation, T.W.; writing—review and editing, P.L., C.F.-d.-l.P., T.B., M.D., and A.G.; visualisation, M.D.; supervision, T.W.; project administration, T.W.; funding acquisition, P.L. and A.G. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Data are available upon request.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Elhassan, B.; Steinmann, S.P. Entrapment neuropathy of the ulnar nerve. J. Am. Acad. Orthop. Surg. 2007, 15, 672–681. [Google Scholar] [CrossRef] [PubMed]
- Robertson, C.; Saratsiotis, J. A review of compression ulnar neuropathy at the elbow. J. Manip. Physiol. Ther. 2005, 28, 345. [Google Scholar] [CrossRef] [PubMed]
- Mondelli, M.; Giannini, F.; Ballerini, M.; Ginanneschi, F.; Martorelli, M. Incidence of ulnar neuropathy at the elbow in the province of Siena (Italy). J. Neurol. Sci. 2005, 234, 5–10. [Google Scholar] [CrossRef] [PubMed]
- An, T.W.; Evanoff, B.A.; Boyer, M.I.; Osei, D.A. The Prevalence of Cubital Tunnel Syndrome: A Cross-Sectional Study in a U.S. Metropolitan Cohort. J. Bone Jt. Surg. 2017, 99, 408–416. [Google Scholar] [CrossRef] [Green Version]
- Kooner, S.; Cinats, D.; Kwong, C.; Matthewson, G.; Dhaliwal, G. Conservative treatment of cubital tunnel syndrome: A systematic review. Orthop. Rev. 2019, 11, 7955. [Google Scholar] [CrossRef] [Green Version]
- McGowan, J. The results of transposition of the ulnar nerve for traumatic ulnar neuritis. J. Bone Jt. Surg. Br. 1950, 32, 293–301. [Google Scholar] [CrossRef]
- Ochiai, N.; Honmo, J.; Tsunjino, A.; Nisiura, Y. Electrodiagnosis in entrapment neuropathy by the arcade of struthers. Clin. Orthop. Relat. Res. 2001, 378, 129–135. [Google Scholar] [CrossRef]
- Sunderland, S. Nerves and Nerve Injuries; Churchill Livingstone: Edinburgh, UK; London, UK; New York, NY, USA, 1978. [Google Scholar]
- Assmus, H.; Antoniadis, G.; Bischoff, C.; Hoffmann, R.; Martini, A.-K.; Preissler, K.; Scheglmann, K.; Schwerdtfeger, K.; Wessels, K.D.; Wustner-Hofmann, M. Cubital tunnel syndrome—a review and management guidelines. Cent. Eur. Neurosurg. 2011, 72, 90–98. [Google Scholar] [CrossRef]
- Palmer, B.A.; Hughes, T.B. Cubital tunnel syndrome. J. Hand Surg. Am. 2010, 35, 153–163. [Google Scholar] [CrossRef]
- Bartels, R.H.; Verbeek, A.L. Risk factors for ulnar nerve compression at the elbow: A case control study. Acta Neurochir. 2007, 149, 669–674. [Google Scholar] [CrossRef] [Green Version]
- Cutts, S. Cubital tunnel syndrome. Postgrad. Med. J. 2007, 83, 28–31. [Google Scholar] [CrossRef] [PubMed]
- Svernlov, B.; Larsson, M.; Rehn, K.; Adolfsson, L. Conservative treatment of the cubital tunnel syndrome. J. Hand Surg. 2009, 34B, 201–207. [Google Scholar] [CrossRef] [PubMed]
- Lund, A.T.; Amadio, P.C. Treatment of cubital tunel syndrome: Perspectives for the therapist. J. Hand Ther. 2006, 19, 170–178. [Google Scholar] [CrossRef] [PubMed]
- Wolny, T.; Saulicz, E.; Linek, P.; Shacklock, M.; Myśliwiec, A. Efficacy of Manual Therapy Including Neurodynamic Techniques for the Treatment of Carpal Tunnel Syndrome: A Randomized Controlled Trial. J. Manip. Physiol. Ther. 2017, 40, 263–272. [Google Scholar] [CrossRef]
- Wolny, T.; Linek, P. Neurodynamic Techniques Versus “Sham” Therapy in the Treatment of Carpal Tunnel Syndrome: A Randomized Placebo-Controlled Trial. Arch. Phys. Med. Rehabil. 2018, 99, 843–854. [Google Scholar] [CrossRef]
- Wolny, T.; Linek, P. Is manual therapy based on neurodynamic techniques effective in the treatment of carpal tunnel syndrome? A randomized controlled trial. Clin. Rehabil. 2019, 33, 408–417. [Google Scholar] [CrossRef]
- Wolny, T.; Linek, P. Long-term patient observation after conservative treatment of carpal tunnel syndrome: A summary of two randomised controlled trials. PeerJ 2019, 7, e8012. [Google Scholar] [CrossRef]
- Fernández-de-las-Peñas, C.; Cleland, J.; Palacios-Ceña, M.; Fuensalida-Novo, S.; Alonso-Blanco, C.; Pareja, J.A.; Alburquerque-Sendín, F. Effectiveness of manual therapy versus surgery in pain processing due to carpal tunnel syndrome: A randomized clinical trial. Eur. J. Pain 2017, 21, 1266–1276. [Google Scholar] [CrossRef] [Green Version]
- Kearns, G.L.; Wang, S. Medical diagnosis of cubital tunnel syndrome ameliorated with thrust manipulation of the elbow and carpals. J. Man. Manip. Ther. 2012, 20, 90–95. [Google Scholar] [CrossRef] [Green Version]
- Oskay, D.; Meriç, A.; Nuray, K.; Firat, T.; Ayhan, C.; Leblebicioğlu, G. Neurodynamic mobilization in the conservative treatment of cubital tunnel syndrome: Long-term follow-up of 7 cases. J. Manip. Physiol. Ther. 2010, 33, 156–163. [Google Scholar] [CrossRef]
- Shen, Y.P.; Wu, Y.Y.; Chu, H.Y.; Li, T.Y.; Chen, L.C.; Wu, Y.T. Extracorporeal shock wave therapy in cubital tunnel syndrome: A pilot study. Neurol. Asia 2018, 23, 233–238. [Google Scholar]
- Anandkumar, S.; Manivasagam, M. Effect of dry needling on cubital tunnel syndrome: Three case reports. Physiother. Theory Pract. 2019, 35, 363–372. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; Group, T.P. Preffered Reporting Items for Systematic Reviews and Mata-Analyses: The PRISMA Statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Centre for Reviews and Dissemination. Systematic Reviews: CRD’s Guidance for Undertaking Reviews in Health Care; University of York: York, UK, 2008. [Google Scholar]
- Risk of Bias Tools—Current Version of RoB 2. Available online: https://www.riskofbias.info/welcome/rob-2-0-tool (accessed on 8 April 2021).
- Moola, S.; Munn, Z.; Tufanaru, C.; Aromataris, E.; Sears, K.; Sfetc, R.; Currie, M.; Lisy, K.; Qureshi, R.; Mattis, P.; et al. Chapter 7: Systematic reviews of etiology and risk. In Joanna Briggs Institute Reviewer’s Manual 2017; Joanna Briggs Institute: Adelaide, Australia, 2017. [Google Scholar]
- Sterne, J.A.C.; Hernán, M.A.; Reeves, B.C.; Savović, J.; Berkman, N.D.; Viswanathan, M.; Henry, D.; Altman, D.G.; Ansari, M.T.; Boutron, I.; et al. ROBINS-I: A tool for assessing risk of bias in non-randomized studies of interventions. BMJ 2016, 355, i4919. [Google Scholar] [CrossRef] [Green Version]
- Badur, N.B.; Ozkan, F.U.; Aktas, I. Efficacy of shortwave diathermy in ulnar nerve entrapment at the elbow: A double-blind randomized controlled clinical trial. Clin. Rehabil. 2020, 34, 1048–1055. [Google Scholar] [CrossRef]
- Ozkan, F.U.; Saygi, E.K.; Senol, S.; Kapci, S.; Aydeniz, B.; Aktas, I.; Gozke, E. New treatment alternatives in the ulnar neuropathy at the elbow: Ultrasound and low-level laser therapy. Acta Neurol. Belg. 2015, 115, 355–360. [Google Scholar] [CrossRef]
- Illes, J.D.; Johnson, T.L., Jr. Chiropractic management of a patient with ulnar nerve compression symptoms: A case report. J. Chirop. Med. 2013, 12, 66–73. [Google Scholar] [CrossRef] [Green Version]
- Coppieters, M.W.; Bartholomeeusen, K.E.; Stappaerts, K.H. Incorporating nerve-gliding techniques in the conservative treatment of cubital tunnel syndrome. J. Manip. Physiol. Ther. 2004, 27, 560–568. [Google Scholar] [CrossRef]
- Kwak, S.; Daeun, J.; Choo, Y.J.; Chang, M.C. Management of neuropathic pain induced by cubital tunnel syndrome using pulsed radiofrequency: Two case report. Medicine 2019, 98, e15599. [Google Scholar] [CrossRef]
- Fernández-de-Las-Peñas, C.; Arias-Buría, J.L.; El Bachiri, Y.R.; Plaza-Manzano, G.; Cleland, J.A. Ultrasound-guided percutaneous electrical stimulation for a patient with cubital tunnel syndrome: A case report with a one-year follow-up. Physiother. Theory Pract. 2020, 6, 1–6. [Google Scholar] [CrossRef]
- Johnson, E.W. Diagnosis of carpal tunnel syndrome. The gold standard. Am. J. Phys. Med. Rehabil. 1993, 72, 1. [Google Scholar] [CrossRef] [PubMed]
- David, C.; Preston, D.C.; Barbara, E.; Shapiro, B.E. Electromyography and Neuromuscular Disorders. Clinical-Electrophysiologic Correlations, 2nd ed.; Elsevier: Philadelphia, PA, USA, 1998. [Google Scholar]
- Nee, R.J.; Jull, G.A.; Vicenzino, B.; Coppieters, M.W. The validity of upper-limb neurodynamic tests for detecting peripheral neuropathic pain. J. Orthop. Sports Phys. Therapy 2012, 42, 413–424. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Novak, C.B.; Lee, G.W.; Mackinnon, S.E.; Lay, L. Provocative testing for cubital tunnel syndrome. J. Hand Surg. 1994, 19, 817–820. [Google Scholar] [CrossRef]
- Gillard, J.; Perez-Cousin, M.; Hachulla, E.; Remy, J.; Hurtevent, J.F.; Vinckier, L. Diagnosis thoracic outlet syndrome: Contribution of provocative test, ultrasonography, electrophysiology, and helical computed tomography in 48 patient. Jt. Bone Spine 2001, 68, 416–424. [Google Scholar] [CrossRef]
- Carlson, H.; Colbert, A.; Frydl, J.; Arnall, E.; Elliot, M.; Carlson, M. Current options for nonsurgical management of carpal tunnel syndrome. Int. J. Clin. Rheumtol. 2010, 5, 129–142. [Google Scholar] [CrossRef] [Green Version]
- Chang, M.H.; Chiang, H.T.; Ger, L.P.; Yang, D.A.; Lo, Y.K. The cause of slowed forearm median conduction velocity in carpal tunnel syndrome. Clin. Neurophysiol. 2000, 111, 1039–1044. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).