Intentional Replantation as a Starting Approach for a Multidisciplinary Treatment of a Mandibular Second Molar: A Case Report
Abstract
:1. Introduction
2. Case Report
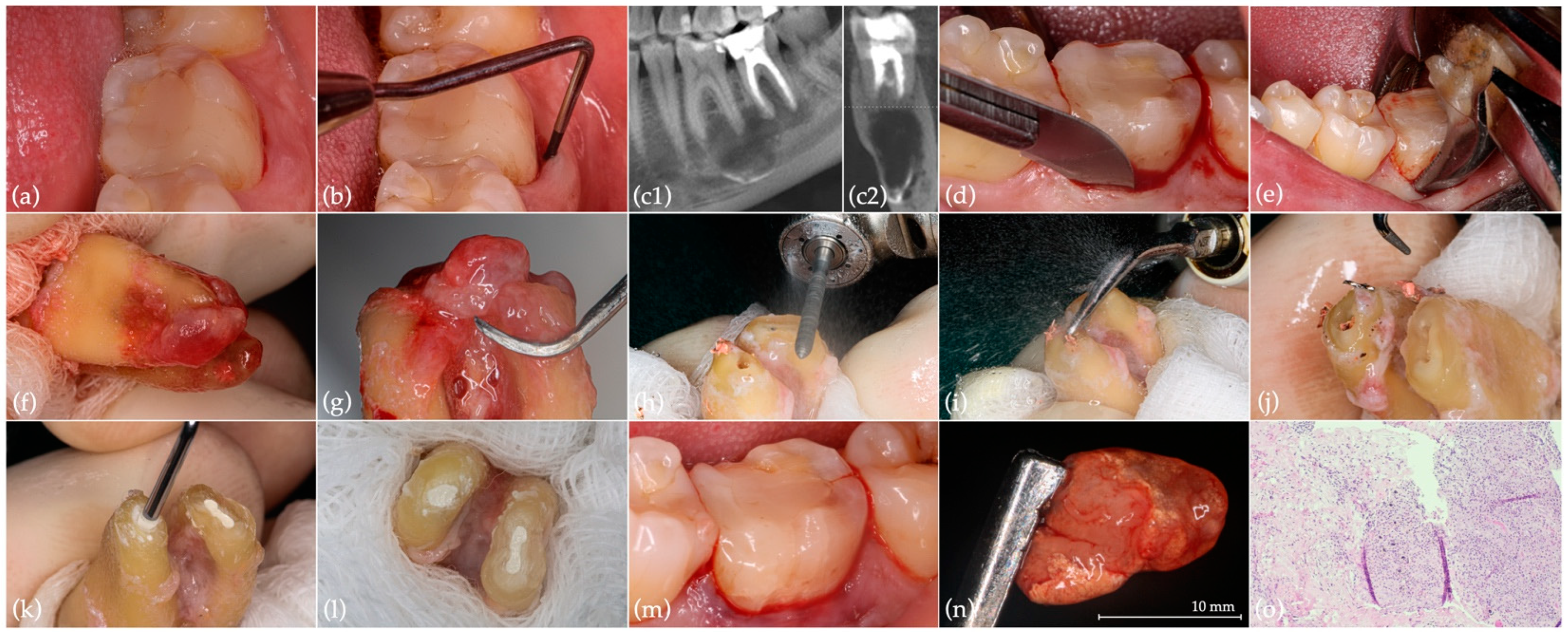
2.1. Intentional Replantation
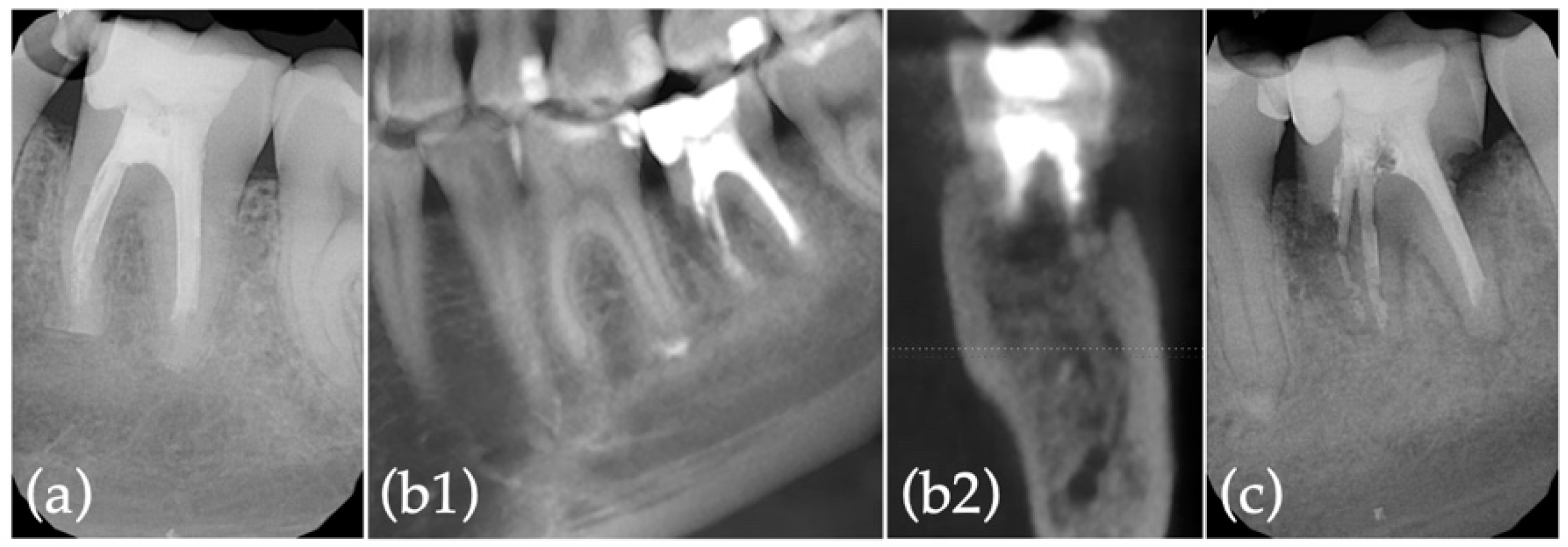
2.2. Extraction with Alveolar Ridge Preservation Using Leukocyte-Platelet Rich Fibrin (L-PRF)
2.3. Implant Surgery
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Mainkar, A. A Systematic Review of the Survival of Teeth Intentionally Replanted with a Modern Technique and Cost-Effectiveness Compared with Single-Tooth Implants. J. Endod. 2017, 43, 1963–1968. [Google Scholar] [CrossRef] [PubMed]
- Peer, M. Intentional replantation—A ‘last resort’ treatment or a conventional treatment procedure? Nine case reports. Dent. Traumatol. 2004, 20, 48–55. [Google Scholar] [CrossRef] [PubMed]
- Torabinejad, M.; White, S.N. Endodontic Treatment Options after Unsuccessful Initial Root Canal Treatment Alternatives to Single-Tooth Implants. J. Am. Dent. Assoc. 2016, 147, 214–220. [Google Scholar] [CrossRef] [PubMed]
- Grossman, L.I. Intentional Replantation of Teeth. J. Am. Dent. Assoc. 1966, 72, 1111–1118. [Google Scholar] [CrossRef] [PubMed]
- Grossman, L.I. Intentional Replantation of Teeth: A Clinical Evaluation. J. Am. Dent. Assoc. 1982, 104, 633–639. [Google Scholar] [CrossRef]
- Becker, B.D. Intentional Replantation Techniques: A Critical Review. J. Endod. 2018, 44, 14–21. [Google Scholar] [CrossRef]
- Andreasen, J.O.; Hjorting-Hansen, E. Replantation of teeth. II. Histological study of 22 replanted anterior teeth in humans. Acta Odontol. Scand. 1966, 24, 287–306. [Google Scholar] [CrossRef]
- Choi, Y.H.; Bae, J.H.; Kim, Y.K.; Kim, H.Y.; Kim, S.K.; Cho, B.H. Clinical Outcome of Intentional Replantation with Preoperative Orthodontic Extrusion: A Retrospective Study. Int. Endod. J. 2014, 47, 1168–1176. [Google Scholar] [CrossRef]
- Torabinejad, M.; Dinsbach, N.A.; Turman, M.; Handysides, R.; Bahjri, K.; White, S.N. Survival of Intentionally Replanted Teeth and Implant-Supported Single Crowns: A Systematic Review. J. Endod. 2015, 41, 992–998. [Google Scholar] [CrossRef]
- Jang, Y.; Lee, S.J.; Yoon, T.C.; Roh, B.D.; Kim, E. Survival Rate of Teeth with a C-Shaped Canal after Intentional Replantation: A Study of 41 Cases for up to 11 Years. J. Endod. 2016, 42, 1320–1325. [Google Scholar] [CrossRef]
- Grzanich, D.; Rizzo, G.; Silva, R.M. Saving Natural Teeth: Intentional Replantation—Protocol and Case Series. J. Endod. 2017, 43, 2119–2124. [Google Scholar] [CrossRef] [PubMed]
- Cho, S.Y.; Lee, Y.; Shin, S.J.; Kim, E.; Jung, I.Y.; Friedman, S.; Lee, S.J. Retention and Healing Outcomes after Intentional Replantation. J. Endod. 2016, 42, 909–915. [Google Scholar] [CrossRef] [PubMed]
- Aidos, H.; Diogo, P.; Santos, J.M. Root Resorption Classifications: A Narrative Review and a Clinical Aid Proposal for Routine Assessment. Eur. Endod. J. 2018, 3, 134–145. [Google Scholar] [CrossRef] [PubMed]
- Choukroun, J.; Adda, F.; Schoeffler, C.; Vervelle, A. An Opportunity in Perioimplantology: The PRF. Implantodontie 2001, 42, 55–62. [Google Scholar]
- Pinto, N.R.; Castro, A.; Leuven, K.U. Consensus Guidelines on the Use of L-PRF from the 1st European Meeting on Enhanced Natural Healing in Dentistry; Optimisation of Guided Bone Regeneration Techniques View Project; Research Gate: Berlin, Germany, 2016. [Google Scholar] [CrossRef]
- Cho, S.Y.; Lee, S.J.; Kim, E. Clinical Outcomes after Intentional Replantation of Periodontally Involved Teeth. J. Endod. 2017, 43, 550–555. [Google Scholar] [CrossRef] [PubMed]
- Adnan, S.; Lone, M.M.; Khan, F.R.; Hussain, S.M.; Nagi, S.E. Which Is the Most Recommended Medium for the Storage and Transport of Avulsed Teeth? A Systematic Review. Dent. Traumatol. 2018, 34, 59–70. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.; Kratchman, S. Modern Endodontic Surgery Concepts and Practice: A Review. J. Endod. 2006, 32, 601–623. [Google Scholar] [CrossRef] [PubMed]
- Friedman, S. Prognosis of Healing in Treated Teeth with Endodontic Infections. In Endodontic Microbiology; Fouad, A.F., Ed.; John Wiley & Sons, Inc.: Hoboken, NJ, USA, 2017. [Google Scholar]
- Palma, P.J.; Marques, J.A.; Casau, M.; Santos, A.; Caramelo, F.; Falacho, R.I.; Santos, J.M. Evaluation of Root-End Preparation with Two Different Endodontic Microsurgery Ultrasonic Tips. Biomedicines 2020, 8, 383. [Google Scholar] [CrossRef]
- Wang, Z. Bioceramic Materials in Endodontics. Endod. Top. 2015, 32, 3–30. [Google Scholar] [CrossRef]
- Torabinejad, M.; Parirokh, M.; Dummer, P.M.H. Mineral Trioxide Aggregate and Other Bioactive Endodontic Cements: An Updated Overview—Part II: Other Clinical Applications and Complications. Int. Endod. J. 2018, 51, 284–317. [Google Scholar] [CrossRef]
- Sarnadas, M.; Marques, J.A.; Baptista, I.P.; Santos, J.M. Impact of Periodontal Attachment Loss on the Outcome of Endodontic Microsurgery: A Systematic Review and Meta-Analysis. Medicina 2021, 57, 922. [Google Scholar] [CrossRef] [PubMed]
- Taha, N.A.; Aboyounes, F.B.; Tamimi, Z.Z. Root-End Microsurgery Using a Premixed Tricalcium Silicate Putty as Root-End Filling Material: A Prospective Study. Clin. Oral Investig. 2020, 25, 311–317. [Google Scholar] [CrossRef] [PubMed]
- Paolone, M.G.; Kaitsas, R.; Paolone, G.; Kaitsas, V. Lingual Orthodontics and Forced Eruption: A Means for Osseous and Tissue Regeneration. Prog. Orthod. 2008, 9, 46–57. [Google Scholar] [PubMed]
- Crisci, A.; de Crescenzo, U.; Crisci, M. Platelet-Rich Concentrates (L-PRF, PRP) in Tissue Regeneration: Control of Apoptosis and Interactions with Regenerative Cells. J. Clin. Mol. Med. 2018, 1, 1–2. [Google Scholar] [CrossRef]
- Castro, A.B.; Meschi, N.; Temmerman, A.; Pinto, N.; Lambrechts, P.; Teughels, W.; Quirynen, M. Regenerative Potential of Leucocyte- and Platelet-Rich Fibrin. Part B: Sinus Floor Elevation, Alveolar Ridge Preservation and Implant Therapy. A Systematic Review. J. Clin. Periodontol. 2017, 44, 225–234. [Google Scholar] [CrossRef]
- Anwandter, A.; Bohmann, S.; Nally, M.; Castro, A.B.; Quirynen, M.; Pinto, N. Dimensional Changes of the Post Extraction Alveolar Ridge, Preserved with Leukocyte- and Platelet Rich Fibrin: A Clinical Pilot Study. J. Dent. 2016, 52, 23–29. [Google Scholar] [CrossRef]
- Temmerman, A.; Vandessel, J.; Castro, A.; Jacobs, R.; Teughels, W.; Pinto, N.; Quirynen, M. The Use of Leucocyte and Platelet-Rich Fibrin in Socket Management and Ridge Preservation: A Split-Mouth, Randomized, Controlled Clinical Trial. J. Clin. Periodontol. 2016, 43, 990–999. [Google Scholar] [CrossRef]
- Marenzi, G.; Riccitiello, F.; Tia, M.; di Lauro, A.; Sammartino, G. Influence of Leukocyte- and Platelet-Rich Fibrin (L-PRF) in the Healing of Simple Postextraction Sockets: A Split-Mouth Study. BioMed Res. Int. 2015, 2015, 369273. [Google Scholar] [CrossRef]
- Dragonas, P.; Katsaros, T.; Avila-Ortiz, G.; Chambrone, L.; Schiavo, J.H.; Palaiologou, A. Effects of Leukocyte–Platelet-Rich Fibrin (L-PRF) in Different Intraoral Bone Grafting Procedures: A Systematic Review. Int. J. Oral. Maxillofac. Surg. 2019, 48, 250–262. [Google Scholar] [CrossRef]
- Elhakim, A.; Kim, S.; Kim, E.; Elshazli, A.H. Preserving the Vitality of Teeth Adjacent to a Large Radicular Cyst in Periapical Microsurgery: A Case Report with 4-Year Follow-Up. BMC Oral Health 2021, 21, 382. [Google Scholar] [CrossRef]


Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Santos, J.M.; Marques, J.A.; Esteves, M.; Sousa, V.; Palma, P.J.; Matos, S. Intentional Replantation as a Starting Approach for a Multidisciplinary Treatment of a Mandibular Second Molar: A Case Report. J. Clin. Med. 2022, 11, 5111. https://doi.org/10.3390/jcm11175111
Santos JM, Marques JA, Esteves M, Sousa V, Palma PJ, Matos S. Intentional Replantation as a Starting Approach for a Multidisciplinary Treatment of a Mandibular Second Molar: A Case Report. Journal of Clinical Medicine. 2022; 11(17):5111. https://doi.org/10.3390/jcm11175111
Chicago/Turabian StyleSantos, João Miguel, Joana A. Marques, Margarida Esteves, Vítor Sousa, Paulo J. Palma, and Sérgio Matos. 2022. "Intentional Replantation as a Starting Approach for a Multidisciplinary Treatment of a Mandibular Second Molar: A Case Report" Journal of Clinical Medicine 11, no. 17: 5111. https://doi.org/10.3390/jcm11175111
APA StyleSantos, J. M., Marques, J. A., Esteves, M., Sousa, V., Palma, P. J., & Matos, S. (2022). Intentional Replantation as a Starting Approach for a Multidisciplinary Treatment of a Mandibular Second Molar: A Case Report. Journal of Clinical Medicine, 11(17), 5111. https://doi.org/10.3390/jcm11175111








