Association between Immediate Postoperative Radiographic Findings and Failed Internal Fixation for Trochanteric Fractures: Systematic Review and Meta-Analysis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Eligibility Criteria
2.1.1. Study Type
2.1.2. Study Participants
2.2. Exposures
2.3. Reduction Quality
- 1.
- The Baumgaertner reduction criteria: The reduction quality is classified as good, acceptable, or poor [12]. Poor reduction indicates varus on the AP radiograph and angulation greater than 20 degrees on the lateral radiograph and displacement more than 4 mm on both views. Here, we classified it into two categories: not poor (good or acceptable) or poor.
- 2.
- Overall alignment using AP radiography: We classified it as either varus or nonvarus (adequate reduction quality). When the femoral neck angle of the operated hip was reduced compared with that of the contralateral hip, we defined it as varus alignment. The original authors have established a detailed definition of varus.
- 3.
2.4. Screw Placement in the Femoral Head
- 4.
- 5.
2.5. Outcomes
2.6. Search Method
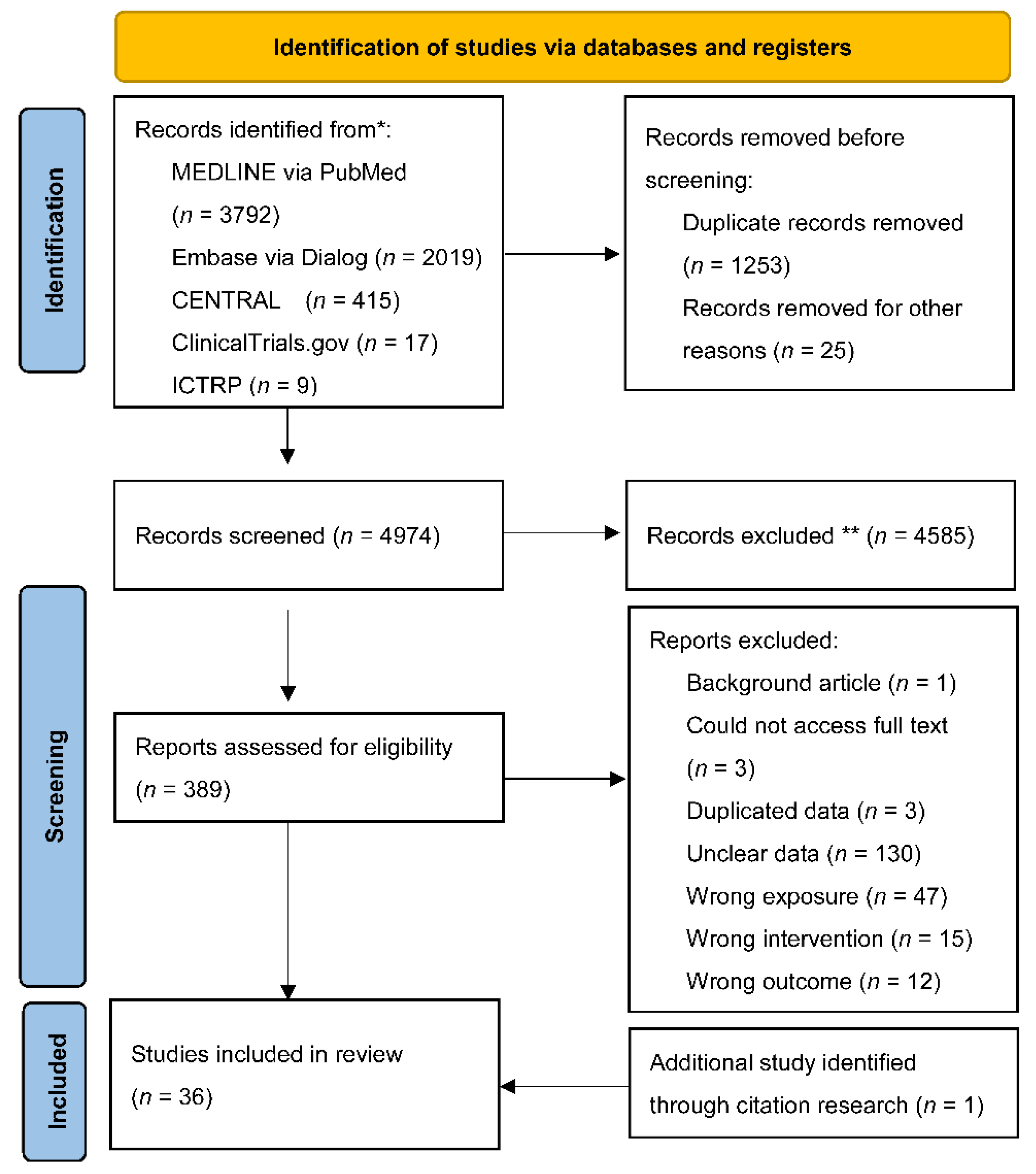
2.7. Study Selection and Data Extraction
2.8. Risk of Bias (Quality) Assessment
2.9. Statistical Analysis
3. Results
3.1. Association between Immediate Postoperative Radiographic Findings and Failed Internal Fixations
3.2. Association between Immediate Postoperative Radiographic Findings and Cut-Outs
3.3. Subgroup and Sensitivity Analyses
4. Discussion
4.1. Limitations
4.2. Strengths
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Dhanwal, D.K.; Dennison, E.M.; Harvey, N.C.; Cooper, C. Epidemiology of hip fracture: Worldwide geographic variation. Indian J. Orthop. 2011, 45, 15–22. [Google Scholar] [CrossRef] [PubMed]
- Tiihonen, R.; Alaranta, R.; Helkamaa, T.; Nurmi-Lüthje, I.; Kaukonen, J.P.; Lüthje, P. A 10-Year retrospective study of 490 hip fracture patients: Reoperations, direct medical costs, and survival. Scand. J. Surg. 2019, 108, 178–184. [Google Scholar] [CrossRef]
- Kaufer, H. Mechanics of the treatment of hip injuries. Clin. Orthop. Relat. Res. 1980, 146, 53–61. [Google Scholar] [CrossRef]
- Rubio-Avila, J.; Madden, K.; Simunovic, N.; Bhandari, M. Tip to apex distance in femoral intertrochanteric fractures: A systematic review. J. Orthop. Sci. 2013, 18, 592–598. [Google Scholar] [CrossRef]
- Ng, M.; Shah, N.S.; Golub, I.; Ciminero, M.; Zhai, K.; Kang, K.K.; Emara, A.K.; Piuzzi, N.S. No difference between lag screw and helical blade for cephalomedullary nail cut-out a systematic review and meta-analysis. Eur. J. Orthop. Surg. Traumatol. 2021. [Google Scholar] [CrossRef]
- Lim, E.J.; Sakong, S.; Son, W.S.; Cho, J.W.; Oh, J.K.; Kim, C.H. Comparison of sliding distance of lag screw and nonunion rate according to anteromedial cortical support in intertrochanteric fracture fixation: A systematic review and meta-analysis. Injury 2021, 52, 2787–2794. [Google Scholar] [CrossRef] [PubMed]
- Stroup, D.F.; Berlin, J.A.; Morton, S.C.; Olkin, I.; Williamson, G.D.; Rennie, D.; Moher, D.; Becker, B.J.; Sipe, T.A.; Thacker, S.B. Meta-analysis of observational studies in epidemiology: A proposal for reporting. Meta-analysis of Observational Studies in Epidemiology (MOOSE) group. JAMA 2000, 283, 2008–2012. [Google Scholar] [CrossRef]
- Higgins, J.P.T.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.J.; Welch, V.A. Cochrane Handbook for Systematic Reviews of Interventions Version 6.2: Cochrane. 2021. Available online: https://training.cochrane.org/handbook/archive/v6.2 (accessed on 7 June 2022).
- Foroutan, F.; Guyatt, G.; Zuk, V.; Vandvik, P.O.; Alba, A.C.; Mustafa, R.; Vernooij, R.; Arevalo-Rodriguez, I.; Munn, Z.; Roshanov, P.; et al. GRADE Guidelines 28: Use of GRADE for the assessment of evidence about prognostic factors: Rating certainty in identification of groups of patients with different absolute risks. J. Clin. Epidemiol. 2020, 121, 62–70. [Google Scholar] [CrossRef] [PubMed]
- Yamamoto, N.; Tsujimoto, Y.; Yokoo, S.; Demiya, K.; Inoue, M.; Noda, T.; Ozaki, T.; Yorifuji, T. Protocol: Association between immediate postoperative radiographic findings and mechanical failure: A systematic review and meta-analysis. Open Sci. Framew. 2021. [Google Scholar] [CrossRef]
- Meinberg, E.G.; Agel, J.; Roberts, C.S.; Karam, M.D.; Kellam, J.F. Fracture and Dislocation Classification Compendium-201. J. Orthop. Trauma 2018, 32 (Suppl. 1), S1–S170. [Google Scholar] [CrossRef]
- Baumgaertner, M.R.; Curtin, S.L.; Lindskog, D.M.; Keggi, J.M. The value of the tip-apex distance in predicting failure of fixation of peritrochanteric fractures of the hip. J. Bone Jt. Surg. Am. 1995, 77, 1058–1064. [Google Scholar] [CrossRef] [PubMed]
- Ito, J.; Takakubo, Y.; Sasaki, K.; Sasaki, J.; Owashi, K.; Takagi, M. Prevention of excessive postoperative sliding of the short femoral nail in femoral trochanteric fractures. Arch. Orthop. Trauma Surg. 2015, 135, 651–657. [Google Scholar] [CrossRef] [PubMed]
- Yamamoto, N.; Imaizumi, T.; Noda, T.; Inoue, T.; Kawasaki, K.; Ozaki, T. Postoperative computed tomography assessment of anteromedial cortex reduction is a predictor for reoperation after intramedullary nail fixation for pertrochanteric fractures. Eur. J. Trauma Emerg. Surg. 2022, 48, 1437–1444. [Google Scholar] [CrossRef] [PubMed]
- Cleveland, M.; Bosworth, D.M.; Thompson, F.R.; Wilson, H.J.; Ishizuka, T. A ten-year analysis of intertrochanteric fractures of the femur. J. Bone Jt. Surg. Am. 1959, 41-A, 1399–1408. [Google Scholar] [CrossRef]
- Hsueh, K.K.; Fang, C.K.; Chen, C.M.; Su, Y.P.; Wu, H.F.; Chiu, F.Y. Risk factors in cutout of sliding hip screw in intertrochanteric fractures: An evaluation of 937 patients. Int. Orthop. 2010, 34, 1273–1276. [Google Scholar] [CrossRef]
- Parker, M.J. Cutting-out of the dynamic hip screw related to its position. J. Bone Jt. Surg. Br. 1992, 74, 625. [Google Scholar] [CrossRef]
- National Clinical Guideline Centre (UK). The Management of Hip Fracture in Adults. London: Royal College of Physicians (UK); 2011. National Institute for Health and Care Excellence (NICE). Hip Fracture Management: Clinical Guideline. Available online: https://www.nice.org. (accessed on 7 June 2022).
- American Academy of Orthopaedic Surgeons. Management of Hip Fractures in the Elderly: Evidence-Based Clinical Practice Guideline. Available online: https://www.aaos.org/quality/quality-programs/lower-extremity-programs/hip-fractures-in-the-elderly/ (accessed on 7 June 2022).
- Marsh, J.L.; Slongo, T.F.; Agel, J.; Broderick, J.S.; Creevey, W.; DeCoster, T.A.; Prokuski, L.; Sirkin, M.S.; Ziran, B.; Henley, B.; et al. Fracture and dislocation classification compendium—2007: Orthopaedic Trauma Association classification, database and outcomes committee. J. Orthop. Trauma 2007, 21, S1–S133. [Google Scholar] [CrossRef]
- Hayden, J.A.; van der Windt, D.A.; Cartwright, J.L.; Côté, P.; Bombardier, C. Assessing bias in studies of prognostic factors. Ann. Intern. Med. 2013, 158, 280–286. [Google Scholar] [CrossRef]
- Santesso, N.; Glenton, C.; Dahm, P.; Garner, P.; Akl, E.A.; Alper, B.; Brignardello-Petersen, R.; Carrasco-Labra, A.; De Beer, H.; Hultcrantz, M.; et al. GRADE guidelines 26: Informative statements to communicate the findings of systematic reviews of interventions. J. Clin. Epidemiol. 2020, 119, 126–135. [Google Scholar] [CrossRef]
- Barlow, E.; Larsen, M.P.; Vijayasurej, K.; Burczy, M.; Burczy, J.; Mullins, M. The impact of COVID-19 on dynamic hip screw fixation and training. Pol. Merkur. Lek. 2021, 49, 273–277. [Google Scholar]
- Hwang, J.; Hadeed, M.; Sapp, T.; Mauffrey, C.; Koval, K.J.; Haidukewych, G.H.; Langford, J.L.; Parry, J.A. Varus displacement of intertrochanteric femur fractures on injury radiographs is associated with screw cutout. Eur. J. Orthop. Surg. Traumatol. 2021, 31, 683–687. [Google Scholar] [CrossRef] [PubMed]
- Aicale, R.; Maffulli, N. Greater rate of cephalic screw mobilisation following proximal femoral nailing in hip fractures with a tip-apex distance (TAD) and a calcar referenced TAD greater than 25 mm. J. Orthop. Surg. Res. 2018, 13, 106. [Google Scholar] [CrossRef] [PubMed]
- Mingo-Robinet, J.; Torres-Torres, M.; Martínez-Cervell, C.; Alonso Del Olmo, J.A.; Rivas Laso, J.A.; Aguado-Hernández, H.; Burón-Alvarez, I. Comparative study of the second and third generation of gamma nail for trochanteric fractures: Review of 218 cases. J. Orthop. Trauma 2015, 29, e85–e90. [Google Scholar] [CrossRef] [PubMed]
- De Bruijn, K.; den Hartog, D.; Tuinebreijer, W.; Roukema, G. Reliability of predictors for screw cutout in intertrochanteric hip fractures. J. Bone Jt. Surg. Am. 2012, 94, 1266–1272. [Google Scholar] [CrossRef] [PubMed]
- Pervez, H.; Parker, M.J.; Vowler, S. Prediction of fixation failure after sliding hip screw fixation. Injury 2004, 35, 994–998. [Google Scholar] [CrossRef] [PubMed]
- Kawaguchi, S.; Sawada, K.; Nabeta, Y. Cutting-out of the lag screw after internal fixation with the Asiatic gamma nail. Injury 1998, 29, 47–53. [Google Scholar] [CrossRef]
- Baumgaertner, M.R.; Solberg, B.D. Awareness of tip-apex distance reduces failure of fixation of trochanteric fractures of the hip. J. Bone Jt. Surg. Br. 1997, 79, 969–971. [Google Scholar] [CrossRef]
- Cordero-Ampuero, J.; Peix, C.; Marcos, S.; Cordero G.-G., E. Influence of surgical quality (according to postoperative radiography) on mortality, complications and recovery of walking ability in 1425 hip fracture patients. Injury 2021, 52 (Suppl. 4), S32–S36. [Google Scholar] [CrossRef]
- Jamshad, O.P.; Mathew, J.; Karuppal, R. Functional and radiological outcome of unstable intertrochanteric fracture in old age treated with proximal femoral nail antirotation-2. J. Clin. Diagn. Res. 2021, 15, RC05–RC07. [Google Scholar] [CrossRef]
- Hancloǧlu, S.; Gem, K.; Tosyali, H.K.; Okçu, G. Clinical and radiological outcomes of trochanteric AO/OTA 31A2 fractures: Comparison between helical blade and lag screw—A retrospective cohort study. Z. Orthop. Unfall. 2022, 160, 278–286. [Google Scholar] [CrossRef]
- Swaroop, S.; Gupta, P.; Bawari, R.; Marya, S.K.; Patnaik, S. Factors affecting the outcome of unstable intertrochanteric fractures managed with proximal femoral nail anti-rotation 2: A prospective outcome study in elderly Indian population. Cureus 2020, 12, e11973. [Google Scholar] [CrossRef] [PubMed]
- Temiz, A.; Durak, A.; Atici, T. Unstable intertrochanteric femur fractures in geriatric patients treated with the DLT trochanteric nail. Injury 2015, 46 (Suppl. 2), S41–S46. [Google Scholar] [CrossRef] [PubMed]
- Chang, S.M.; Zhang, Y.Q.; Ma, Z.; Li, Q.; Dargel, J.; Eysel, P. Fracture reduction with positive medial cortical support: A key element in stability reconstruction for the unstable pertrochanteric hip fractures. Arch. Orthop. Trauma Surg. 2015, 135, 811–818. [Google Scholar] [CrossRef] [PubMed]
- Ertürer, R.E.; Sönmez, M.M.; Sarı, S.; Seçkin, M.F.; Kara, A.; Oztürk, I. Intramedullary osteosynthesis of instable intertrochanteric femur fractures with Profin® nail in elderly patients. Acta Orthop. Traumatol. Turc. 2012, 46, 107–112. [Google Scholar] [CrossRef] [PubMed]
- Morvan, A.; Boddaert, J.; Cohen-Bittan, J.; Picard, H.; Pascal-Mousselard, H.; Khiami, F. Risk factors for cut-out after internal fixation of trochanteric fractures in elderly subjects. Orthop. Traumatol. Surg. Res. 2018, 104, 1183–1187. [Google Scholar] [CrossRef]
- Murena, L.; Moretti, A.; Meo, F.; Saggioro, E.; Barbati, G.; Ratti, C.; Canton, G. Predictors of cut-out after cephalomedullary nail fixation of pertrochanteric fractures: A retrospective study of 813 patients. Arch. Orthop. Trauma Surg. 2018, 138, 351–359. [Google Scholar] [CrossRef]
- Kim, K.H.; Han, K.Y.; Kim, K.W.; Lee, J.H.; Chung, M.K. Local postoperative complications after surgery for intertrochanteric fractures using cephalomedullary nails. Hip Pelvis 2018, 30, 168–174. [Google Scholar] [CrossRef]
- Ciufo, D.J.; Zaruta, D.A.; Lipof, J.S.; Judd, K.T.; Gorczyca, J.T.; Ketz, J.P. Risk factors associated with cephalomedullary nail cutout in the treatment of trochanteric hip fractures. J. Orthop. Trauma 2017, 31, 583–588. [Google Scholar] [CrossRef]
- Hsu, C.E.; Huang, K.C.; Lin, T.C.; Tong, K.M.; Lee, M.H.; Chiu, Y.C. Integrated risk scoring model for predicting dynamic hip screw treatment outcome of intertrochanteric fracture. Injury 2016, 47, 2501–2506. [Google Scholar] [CrossRef]
- Çepni, Ş.; Subaşı, İ.Ö.; Şahin, A.; Bozkurt, İ.; Fırat, A.; Kılıçarslan, K. Tip-neck distance ratio as a novel predictor for failure in cephalomedullary nailing of unstable trochanteric fractures (UTF). Arch. Orthop. Trauma Surg. 2021. [Google Scholar] [CrossRef]
- Fang, C.; Lau, T.W.; Wong, T.M.; Lee, H.L.; Leung, F. Sliding hip screw versus sliding helical blade for intertrochanteric fractures: A propensity score-matched case control study. Bone Jt. J. 2015, 97-B, 398–404. [Google Scholar] [CrossRef] [PubMed]
- Buyukdogan, K.; Caglar, O.; Isik, S.; Tokgozoglu, M.; Atilla, B. Risk factors for cut-out of double lag screw fixation in proximal femoral fractures. Injury 2017, 48, 414–418. [Google Scholar] [CrossRef] [PubMed]
- Fujii, T.; Nakayama, S.; Hara, M.; Koizumi, W.; Itabashi, T.; Saito, M. Tip-apex distance is most important of six predictors of screw cutout after internal fixation of intertrochanteric fractures in women. JBJS Open Access 2017, 2, e0022. [Google Scholar] [CrossRef] [PubMed]
- Gunay, C.; Atalar, H.; Altay, M.; Yavuz, O.Y.; Yildirim, A.O.; Oken, O.F. Does the wedge wing in the neck screw prevent cut-out failure in Ota/AO 31-A2 trochanteric fractures in elderly patients. Acta Orthop. Belg. 2014, 80, 26–33. [Google Scholar] [PubMed]
- Yamamoto, N.; Tomita, Y.; Noda, T.; Inoue, T.; Mochizuki, Y.; Ozaki, T. Reduction quality and nail fixation ratio as bone-implant stability factors associated with reoperation for trochanteric fractures. Injury 2021, 52, 1813–1818. [Google Scholar] [CrossRef]
- Shon, O.J.; Choi, C.H.; Park, C.H. Factors associated with mechanical complications in intertrochanteric fracture treated with proximal femoral nail antirotation. Hip Pelvis 2021, 33, 154–161. [Google Scholar] [CrossRef]
- Goto, K.; Murakami, T.; Saku, I. Postoperative subtype P as a risk factor for excessive postoperative sliding of cephalomedullary nail in femoral trochanteric fractures in old patients: A case series of 263 patients using computed tomography analysis. Injury 2022, 53, 2163–2171. [Google Scholar] [CrossRef]
- Momii, K.; Fujiwara, T.; Mae, T.; Tokunaga, M.; Iwasaki, T.; Shiomoto, K.; Kubota, K.; Onizuka, T.; Miura, T.; Hamada, T.; et al. Risk factors for excessive postoperative sliding of femoral trochanteric fracture in elderly patients: A retrospective multicenter study. Injury 2021, 52, 3369–3376. [Google Scholar] [CrossRef]
- Li, C.; Xie, B.; Chen, S.; Lin, G.; Yang, G.; Zhang, L. The effect of local bone density on mechanical failure after internal fixation of pertrochanteric fractures. Arch. Orthop. Trauma Surg. 2016, 136, 223–232. [Google Scholar] [CrossRef]
- Takigawa, N.; Moriuchi, H.; Abe, M.; Yasui, K.; Eshiro, H.; Kinoshita, M. Complications and fixation techniques of trochanteric fractures with the TARGON(®) PF. Injury 2014, 45 (Suppl. 1), S44–S48. [Google Scholar] [CrossRef]
- Karampinas, P.K.; Vlamis, J.A.; Papadelis, E.; Pneumaticos, S.; Schwartsmann, C.R. Clinical outcome of peritrochanteric fractures treatment with an antegrade trochanteric static lag screw nail (Inter TAN). J. Adv. Med. Med. Res. 2016, 18, 1–7. [Google Scholar] [CrossRef]
- Caruso, G.; Bonomo, M.; Valpiani, G.; Salvatori, G.; Gildone, A.; Lorusso, V.; Massari, L. A six-year retrospective analysis of cut-out risk predictors in cephalomedullary nailing for pertrochanteric fractures: Can the tip-apex distance (TAD) still be considered the best parameter. Bone Jt. Res. 2017, 6, 481–488. [Google Scholar] [CrossRef] [PubMed]
| Predictive Factors | Outcomes | Anticipated Absolute Effects a (95% CI) | Relative Effect (95% CI) | No. of Participants (Observational Studies) | Certainty of Evidence (Grade) c | |
|---|---|---|---|---|---|---|
| Assumed Risk with Comparator b | Corresponding Risk with Predictive Factor | |||||
| Poor reduction by Baumgaertner criteria | Failed internal fixation | 14 per 1000 | 16 per 1000 (0–568) | OR 1.17 (0.01–92.75) | 427 (2 studies) | Very low d,e,f,g |
| Cut-out | 42 per 1000 | 255 per 1000 (130–439) | OR 7.78 (3.41–17.76) | 3250 (9 studies) | Low d,h | |
| Varus malreduction | Failed internal fixation | 45 per 1000 | 174 per 1000 (46–478) | OR 4.48 (1.03–19.46) | 832 (2 studies) | Low f,g |
| Cut-out | 25 per 1000 | 61 per 1000 (30–119) | OR 4.54 (2.17–9.49) | 1194 (5 studies) | Low d,g | |
| Intramedullary malreduction on anteromedial cortex | Failed internal fixation | 8 per 1000 | 55 per 1000 (20–145) | OR 7.23 (2.49–21.01) | 1146 (4 studies) | Moderate d |
| Cut-out | 3 per 1000 | 22 per 1000 (8–54) | OR 7.35 (2.83–19.10) | 1383 (6 studies) | Low d,g | |
| TAD ≥ 25 | Failed internal fixation | 14 per 1000 | 19 per 1000 (9–41) | OR 1.39 (0.65–2.98) | 1013 (4 studies) | Very low d,e,g |
| Cut-out | 11 per 1000 | 81 per 1000 (36–173) | OR 7.92 (3.33–18.82) | 4196 (13 studies) | Low d,e | |
| Inadequate screw placement in femoral head | Failed internal fixation | 43 per 1000 | 215 per 1000 (43–626) | OR 6.11 (1.00–37.27) | 998 (5 studies) | Low d,g |
| Cut-out | 41 per 1000 | 105 per 1000 (42–239) | OR 2.75 (1.03–7.33) | 2399 (9 studies) | Very low d,e,g,h | |
| SHS | CMN | |||||||
|---|---|---|---|---|---|---|---|---|
| Prognostic Factors | Outcomes | No of Studies | I2 (%) | Pooled Odds Ratio (95% CI) | No of Studies | I2 (%) | Pooled Odds Ratio (95% CI) | p for Interaction |
| Poor reduction by Baumgaertner criteria | Failed internal fixation | 1 | – | 7.72 (1.85–32.23) | 1 | – | 9.46 (2.36–37.83) | – |
| Cut-out | 1 | – | 1.99 (1.05–3.79) | 4 | 48 | 10.47 (3.68–29.79) | 0.008 | |
| Varus malreduction | Failed internal fixation | 1 | – | 4.60 (1.02–20.85) | 1 | – | 2.89 (0.006–1418.51) | – |
| Cut-out | 1 | – | 4.38 (1.34–14.24) | 3 | 0 | 3.59 (1.25–10.33) | 0.807 | |
| Intramedullary malreduction | Failed internal fixation | – | – | – | 4 | 0 | 6.73 (2.42–18.71) | – |
| Cut-out | – | – | – | 6 | 0 | 7.35 (2.83–19.10) | – | |
| TAD ≥ 25 | Failed internal fixation | 1 | – | 0.71 (0.21–2.41) | 3 | 0 | 2.13 (0.81–5.60) | 0.168 |
| Cut-out | 1 | – | 24.56 (12.52–48.18) | 9 | 62 | 4.68 (1.55–14.09) | 0.012 | |
| Inadequate screw placement in femoral head | Failed internal fixation | 1 | – | 1.53 (0.53–4.44) | 4 | 72 | 11.39 (0.83–156.91) | 0.165 |
| Cut-out | 1 | – | 0.36 (0.22–0.59) | 8 | 2.9 | 3.30 (1.96–5.56) | <0.001 | |
| Crude Odds Ratios | Adjusted Odds Ratios | Repeating the Main Analysis Excluding Studies with High Risk of Bias a | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Prognostic Factors | Outcomes | No of Studies | I2 (%) | Pooled Odds Ratio (95% CI) | No of Studies | I2 (%) | Pooled Odds Ratio (95% CI) | No of Studies | I2 (%) | Pooled Odds Ratio (95% CI) |
| Poor reduction by Baumgaertner criteria | Failed internal fixation | 2 | 0 | 8.57 (3.17–23.18) | 2 | 91.3 | 1.17 (0.02–92.75) | 2 | 91.3 | 1.17 (0.01–92.75) |
| Cut-out | 9 | 77.6 | 7.56 (3.18–18.00) | 4 | 47 | 11.18 (3.46–36.16) | 9 | 68 | 7.78 (3.41–17.76) | |
| Varus malreduction | Failed internal fixation | 2 | 0 | 5.45 (1.86–15.92) | 2 | 0 | 4.48 (1.03–19.46) | 2 | 0 | 4.48 (1.03–19.46) |
| Cut-out | 5 | 0 | 4.60 (2.31–9.17) | 2 | 0 | 5.66 (1.98–16.20) | 3 | 0 | 5.17 (1.92–13.90) | |
| Intramedullary malreduction | Failed internal fixation | 4 | 0 | 7.56 (2.80–20.45) | 1 | – | 9.58 (0.88–104.55) | 4 | 0 | 6.73 (2.42–18.71) |
| Cut-out | 6 | 0 | 8.81 (3.12–21.11) | 1 | – | 7.00 (0.81–60.89) | 6 | 0 | 7.35 (2.83–19.10) | |
| TAD ≥ 25 | Failed internal fixation | 4 | 0 | 1.42 (0.71–2.85) | 1 | - | 1.52 (0.21–11.08) | 3 | 0 | 1.07 (0.40–2.88) |
| Cut-out | 13 | 77.5 | 5.64 (2.50–12.72) | 2 | 0 | 20.81 (6.09–71.12) | 9 | 73.4 | 6.92 (2.30–20.78) | |
| Inadequate screw placement in femoral head | Failed internal fixation | 5 | 74.8 | 5.52 (1.71–17.81) | 2 | 0 | 4.86 (0.04–562.58) | 4 | 0 | 2.00 (0.91–4.37) |
| Cut-out | 9 | 84.3 | 3.01 (1.17–7.77) | 2 | 13 | 2.64 (0.78–8.94) | 7 | 85.6 | 3.15 (0.90–11.04) | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yamamoto, N.; Tsujimoto, Y.; Yokoo, S.; Demiya, K.; Inoue, M.; Noda, T.; Ozaki, T.; Yorifuji, T. Association between Immediate Postoperative Radiographic Findings and Failed Internal Fixation for Trochanteric Fractures: Systematic Review and Meta-Analysis. J. Clin. Med. 2022, 11, 4879. https://doi.org/10.3390/jcm11164879
Yamamoto N, Tsujimoto Y, Yokoo S, Demiya K, Inoue M, Noda T, Ozaki T, Yorifuji T. Association between Immediate Postoperative Radiographic Findings and Failed Internal Fixation for Trochanteric Fractures: Systematic Review and Meta-Analysis. Journal of Clinical Medicine. 2022; 11(16):4879. https://doi.org/10.3390/jcm11164879
Chicago/Turabian StyleYamamoto, Norio, Yasushi Tsujimoto, Suguru Yokoo, Koji Demiya, Madoka Inoue, Tomoyuki Noda, Toshifumi Ozaki, and Takashi Yorifuji. 2022. "Association between Immediate Postoperative Radiographic Findings and Failed Internal Fixation for Trochanteric Fractures: Systematic Review and Meta-Analysis" Journal of Clinical Medicine 11, no. 16: 4879. https://doi.org/10.3390/jcm11164879
APA StyleYamamoto, N., Tsujimoto, Y., Yokoo, S., Demiya, K., Inoue, M., Noda, T., Ozaki, T., & Yorifuji, T. (2022). Association between Immediate Postoperative Radiographic Findings and Failed Internal Fixation for Trochanteric Fractures: Systematic Review and Meta-Analysis. Journal of Clinical Medicine, 11(16), 4879. https://doi.org/10.3390/jcm11164879







