Current Epidemiology of the General Anesthesia Practice for Cesarean Delivery Using a Nationwide Claims Database in Japan: A Descriptive Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Data Source
2.2. Study Population
2.3. Patient- and Facility-Level Variables
2.4. Outcomes
2.5. Statistical Analysis
3. Results
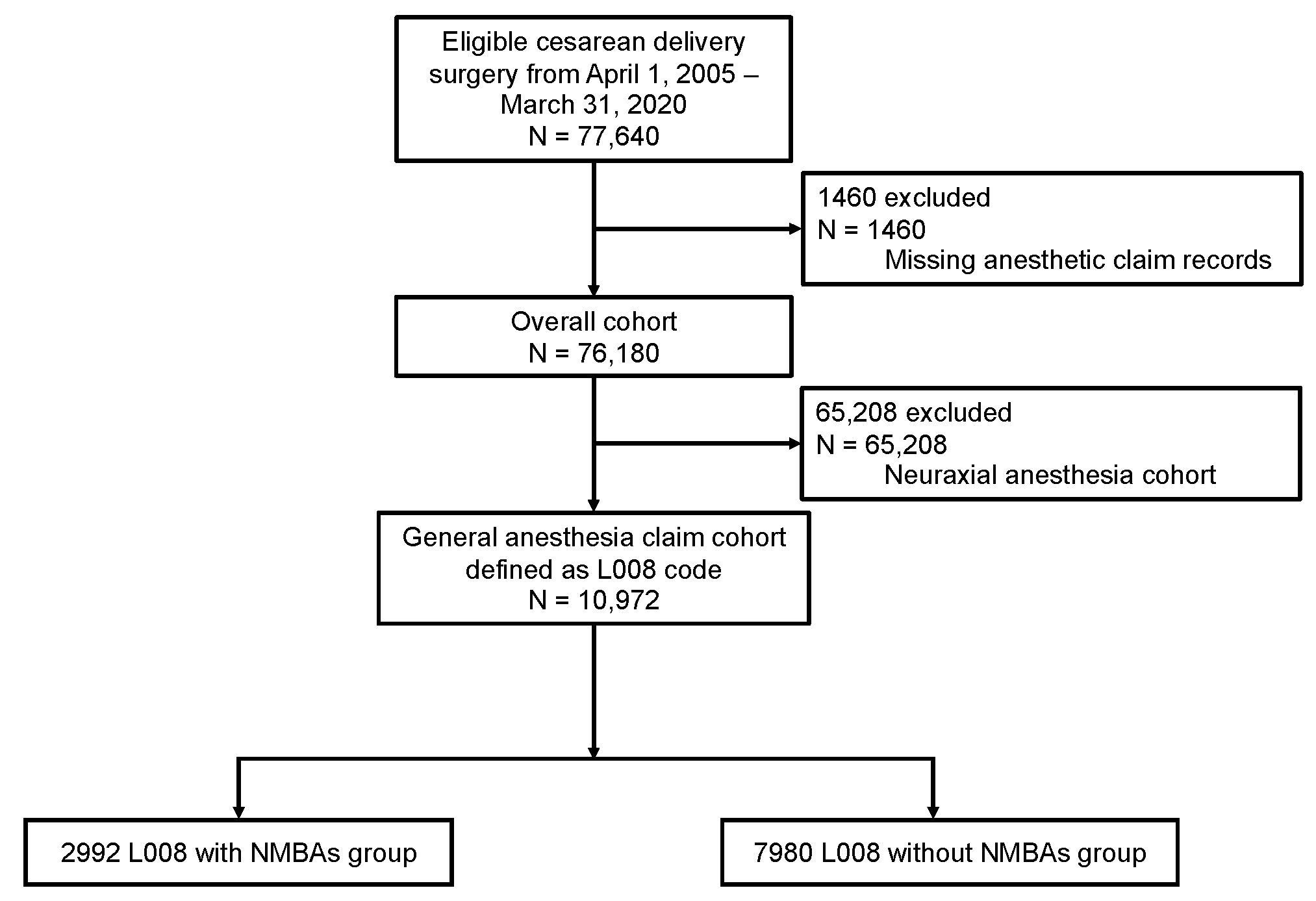
3.1. Study Cohort
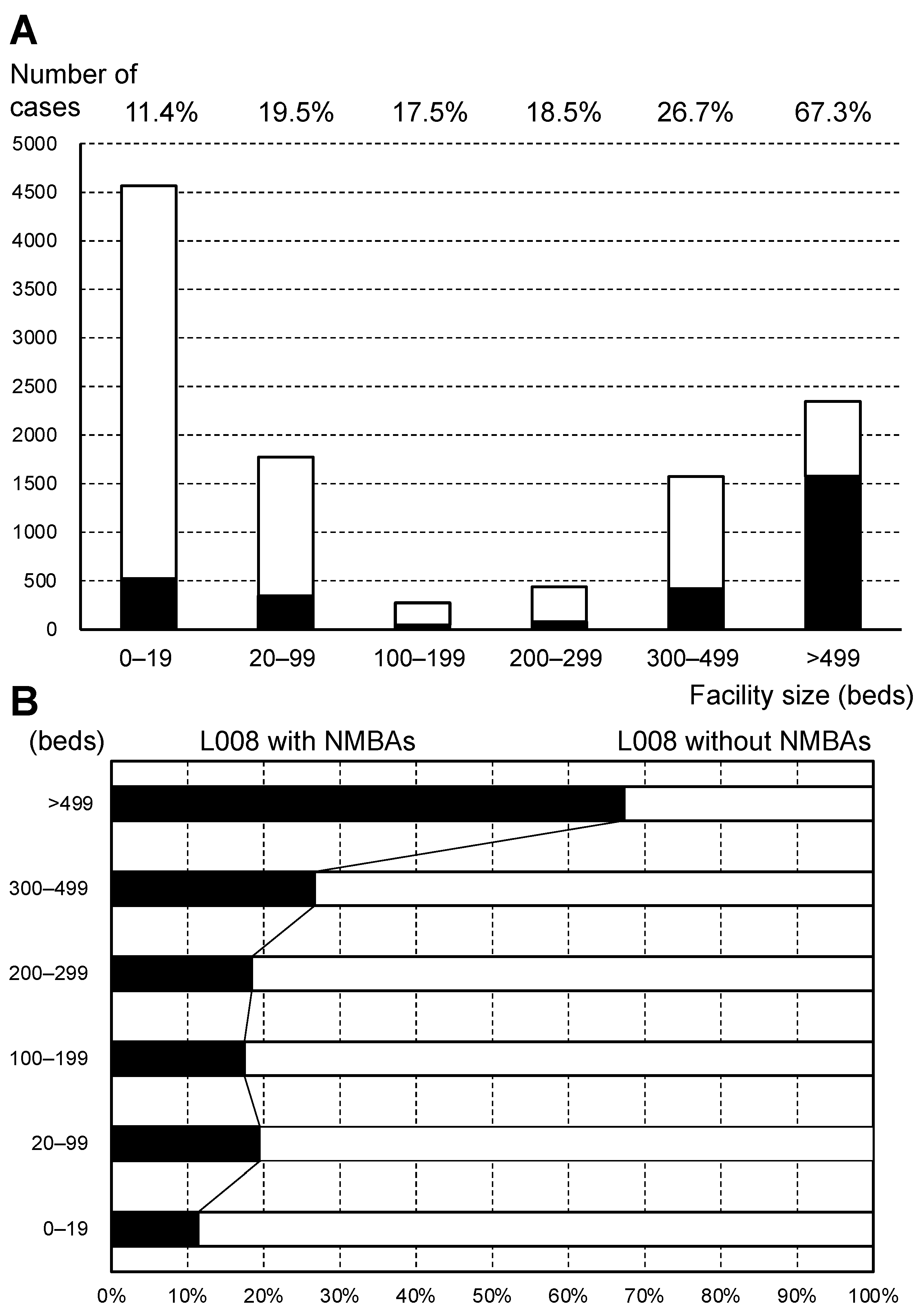
3.2. Patient and Medical Facility Characteristics
3.3. Trends in the Rate of General Anesthesia Use
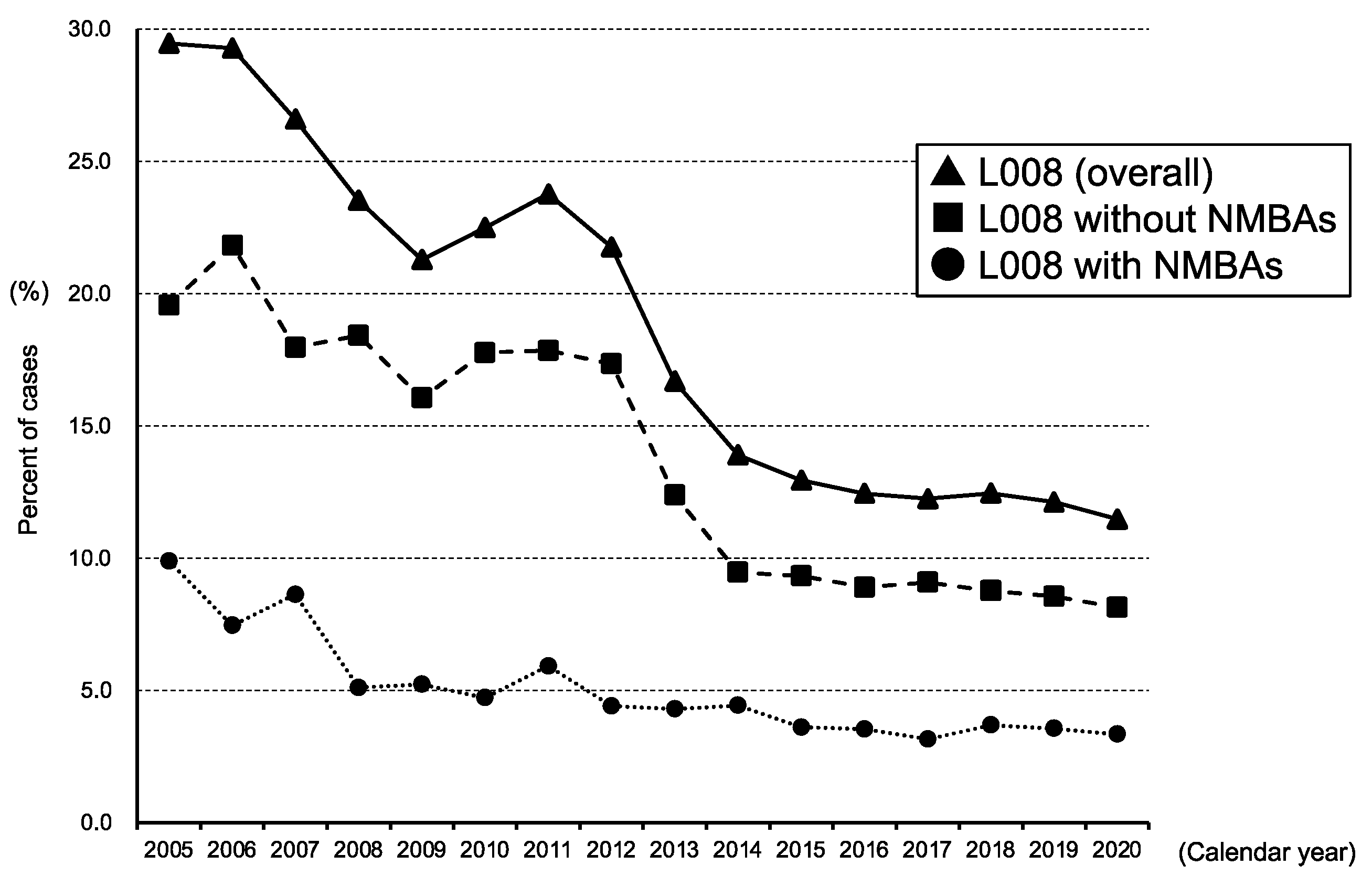
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hasegawa, J.; Katsuragi, S.; Tanaka, H.; Kurasaki, A.; Nakamura, M.; Murakoshi, T.; Nakata, M.; Kanayama, N.; Sekizawa, A.; Isamu, I.; et al. Decline in Maternal Death Due to Obstetric Haemorrhage between 2010 and 2017 in Japan. Sci. Rep. 2019, 9, 11026. [Google Scholar] [CrossRef]
- Maeda, E.; Ishihara, O.; Tomio, J.; Miura, H.; Kobayashi, Y.; Terada, Y.; Murata, K.; Nomura, K. Cesarean Delivery Rates for Overall and Multiple Pregnancies in Japan: A Descriptive Study Using Nationwide Health Insurance Claims Data. J. Obstet. Gynaecol. Res. 2021, 47, 2099–2109. [Google Scholar] [CrossRef]
- Survey of Medical Institutions. Available online: https://www.mhlw.go.jp/toukei/saikin/hw/iryosd/17/dl/02sisetu29-3.pdf (accessed on 14 January 2022).
- Practice Guidelines for Obstetric Anesthesia: An Updated Report by the American Society of Anesthesiologists Task Force on Obstetric Anesthesia and the Society for Obstetric Anesthesia and Perinatology. Anesthesiology 2016, 124, 270–300. [CrossRef]
- Ring, L.; Landau, R.; Delgado, C. The current role of general anesthesia for cesarean delivery. Curr. Anesthesiol. Rep. 2021, 11, 18–27. [Google Scholar] [CrossRef]
- Juang, J.; Gabriel, R.A.; Dutton, R.P.; Palanisamy, A.; Urman, R.D. Choice of anesthesia for cesarean delivery: An analysis of the national anesthesia clinical Outcomes Registry. Anesth. Analg. 2017, 124, 1914–1917. [Google Scholar] [CrossRef]
- Vandenbroucke, J.P.; von Elm, E.; Altman, D.G.; Gøtzsche, P.C.; Mulrow, C.D.; Pocock, S.J.; Poole, C.; Schlesselman, J.J.; Egger, M. STROBE Initiative Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): Explanation and Elaboration. Epidemiology 2007, 18, 805–835. [Google Scholar] [CrossRef]
- Kimura, S.; Sato, T.; Ikeda, S.; Noda, M.; Nakayama, T. Development of a database of health insurance claims: Standardization of disease classifications and anonymous record linkage. J. Epidemiol. 2010, 20, 413–419. [Google Scholar] [CrossRef]
- Yonekura, H.; Seto, K.; Ide, K.; Kawasaki, Y.; Tanaka, S.; Nahara, I.; Takeda, C.; Kawakami, K. Preoperative blood tests conducted before low-risk surgery in Japan: A retrospective observational study using a nationwide insurance claims database. Anesth. Analg. 2018, 126, 1633–1640. [Google Scholar] [CrossRef]
- Yamana, H.; Moriwaki, M.; Horiguchi, H.; Kodan, M.; Fushimi, K.; Yasunaga, H. Validity of diagnoses, procedures, and laboratory data in Japanese administrative data. J. Epidemiol. 2017, 27, 476–482. [Google Scholar] [CrossRef]
- Abe, H.; Sumitani, M.; Uchida, K.; Ikeda, T.; Matsui, H.; Fushimi, K.; Yasunaga, H.; Yamada, Y. Association between mode of anaesthesia and severe maternal morbidity during admission for scheduled caesarean delivery: A nationwide population-based study in Japan, 2010–2013. Br. J. Anaesth. 2018, 120, 779–789. [Google Scholar] [CrossRef]
- Guglielminotti, J.; Landau, R.; Li, G. Adverse events and factors associated with potentially avoidable use of general anesthesia in cesarean deliveries. Anesthesiology 2019, 130, 912–922. [Google Scholar] [CrossRef]
- Bateman, B.T.; Mhyre, J.M.; Hernandez-Diaz, S.; Huybrechts, K.F.; Fischer, M.A.; Creanga, A.A.; Callaghan, W.M.; Gagne, J.J. Development of a comorbidity index for use in obstetric patients. Obstet. Gynecol. 2013, 122, 957–965. [Google Scholar] [CrossRef]
- Quan, H.; Sundararajan, V.; Halfon, P.; Fong, A.; Burnand, B.; Luthi, J.-C.; Saunders, L.D.; Beck, C.A.; Feasby, T.E.; Ghali, W.A. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med. Care 2005, 43, 1130–1139. [Google Scholar] [CrossRef]
- Aoyama, K.; D’Souza, R.; Inada, E.; Lapinsky, S.E.; Fowler, R.A. Measurement properties of comorbidity indices in maternal health research: A systematic review. BMC Pregnancy Childbirth 2017, 17, 372. [Google Scholar] [CrossRef]
- Metcalfe, A.; Lix, L.M.; Johnson, J.-A.; Currie, G.; Lyon, A.W.; Bernier, F.; Tough, S.C. Validation of an obstetric comorbidity index in an external population. BJOG 2015, 122, 1748–1755. [Google Scholar] [CrossRef]
- Odor, P.M.; Bampoe, S.; Moonesinghe, S.R.; Andrade, J.; Pandit, J.J.; Lucas, D.N. Pan-London Perioperative Audit and Research Network (PLAN), for the DREAMY Investigators Group General Anaesthetic and Airway Management Practice for Obstetric Surgery in England: A Prospective, Multicentre Observational Study*. Anaesthesia 2021, 76, 460–471. [Google Scholar] [CrossRef]
- Austin, P.C. Using the standardized difference to compare the prevalence of a binary variable between two groups in observational research. Commun. Stat. Simul. Comput. 2009, 38, 1228–1234. [Google Scholar] [CrossRef]
- Guglielminotti, J.; Wong, C.A.; Landau, R.; Li, G. Temporal trends in anesthesia-related adverse events in cesarean deliveries, New York State, 2003–2012. Anesthesiology 2015, 123, 1013–1023. [Google Scholar] [CrossRef]
- Raising the Standards: RCoA Quality Improvement Compendium. Available online: https://www.rcoa.ac.uk/safety-standards-quality/quality-improvement/raising-standards-rcoa-quality-improvement-compendium (accessed on 14 January 2022).
- Traynor, A.J.; Aragon, M.; Ghosh, D.; Choi, R.S.; Dingmann, C.; Vu Tran, Z.; Bucklin, B.A. Obstetric anesthesia workforce survey: A 30-year update. Anesth. Analg. 2016, 122, 1939–1946. [Google Scholar] [CrossRef]
- Stourac, P.; Kosinova, M.; Blaha, J.; Grochova, M.; Klozova, R.; Noskova, P.; Seidlova, D.; Richterova, S.; Firment, J.; OBAAMA-INT Study Group. Changes in Caesarean Section Anaesthesia between 2011 and 2015: Czech and Slovak National Surveys. Eur. J. Anaesthesiol. 2019, 36, 801–803. [Google Scholar] [CrossRef]
- Butwick, A.J.; Palanisamy, A. Mode of anaesthesia for caesarean delivery and maternal morbidity: Can we overcome confounding by indication? Br. J. Anaesth. 2018, 120, 621–623. [Google Scholar] [CrossRef]
- Ikeda, T.; Kato, A.; Bougaki, M.; Araki, Y.; Ohata, T.; Kawashima, S.; Imai, Y.; Ninagawa, J.; Oba, K.; Chang, K.; et al. A retrospective review of 10-year trends in general anesthesia for cesarean delivery at a university hospital: The impact of a newly launched team on obstetric anesthesia practice. BMC Health Serv. Res. 2020, 20, 421. [Google Scholar] [CrossRef]
- Guasch, E.; Brogly, N.; Mercier, F.J.; Ioscovich, A.; Weiniger, C.F.; Lucas, N.; Chassard, D.; Kranke, P.; Whitaker, D.; Geldner, G.; et al. European minimum standards for obstetric analgesia and anaesthesia departments: An experts’ consensus. Eur. J. Anaesthesiol. 2020, 37, 1115–1125. [Google Scholar] [CrossRef]
- Gelb, A.W.; Morriss, W.W.; Johnson, W.; Merry, A.F.; Gelb, A.W.; Merry, A.F.; Morriss, W.; Abayadeera, A.; Belîi, N.; Brull, S.J.; et al. World Health Organization-World Federation of Societies of Anaesthesiologists (WHO-WFSA) International Standards for a Safe Practice of Anesthesia. Can. J. Anesth./J. Can. Anesth. 2018, 65, 698–708. [Google Scholar] [CrossRef]
| Characteristic | L008 with NMBA, n = 2992 | L008 without NMBA, n = 7980 | Absolute SMD (%) |
|---|---|---|---|
| Age, year | 5.0 | ||
| Mean ± SD | 33.4 ± 5.1 | 33.1 ± 4.9 | |
| <35 | 1826 (61.0) | 5060 (63.4) | 4.9 |
| 35–39 | 869 (29.0) | 2241 (28.1) | 2.1 |
| 40–44 | 266 (8.9) | 616 (7.7) | 4.2 |
| >44 | 31 (1.0) | 63 (0.8) | 2.6 |
| Maternal Comorbidity Index | |||
| Alcohol abuse | 2 (0.1) | 2 (0.0) | 1.9 |
| Asthma | 241 (8.1) | 616 (7.7) | 1.2 |
| Cardiac valvular disease | 23 (0.8) | 16 (0.2) | 8.2 |
| Chronic congestive heart failure | 5 (0.2) | 1 (0.0) | 5.2 |
| Chronic ischemic heart disease | 32 (1.1) | 27 (0.3) | 8.8 |
| Chronic renal disease | 26 (0.9) | 26 (0.3) | 7.1 |
| Congenital heart disease | 24 (0.8) | 15 (0.2) | 8.8 |
| Drug abuse | 0 (0) | 0 (0) | |
| Gestational hypertension | 32 (1.1) | 51 (0.6) | 4.7 |
| Human immunodeficiency virus | 0 (0) | 0 (0) | |
| Mild/unspecified pre-eclampsia | 113 (3.8) | 246 (3.1) | 3.8 |
| Multiple gestation | 120 (4.0) | 198 (2.5) | 8.6 |
| Placenta previa | 270 (9.0) | 374 (4.7) | 17.2 |
| Pre-existing diabetes mellitus | 41 (1.4) | 40 (0.5) | 9.0 |
| Pre-existing hypertension | 88 (2.9) | 106 (1.3) | 11.2 |
| Previous cesarean delivery | 193 (6.5) | 938 (11.8) | 18.5 |
| Pulmonary hypertension | 4 (0.1) | 0 (0) | 5.2 |
| Severe pre-eclampsia | 111 (3.7) | 246 (3.1) | 3.5 |
| Sickle cell disease | 0 (0) | 0 (0) | |
| Systemic lupus erythematosus | 21 (0.7) | 13 (0.2) | 8.2 |
| Maternal Comorbidity Index score, median (IQR) | 1 (0–2) | 1 (0–1) | |
| 0 | 1298 (43.4) | 3767 (47.2) | 7.7 |
| 1–2 | 1237 (41.3) | 3407 (42.7) | 2.7 |
| >2 | 457 (15.3) | 806 (10.1) | 15.6 |
| Obstetrical/maternal/fetal emergency | |||
| Amniotic fluid embolism | 8 (0.3) | 0 (0) | 7.3 |
| Chorioamnionitis | 287 (9.6) | 418 (5.2) | 16.7 |
| Fetal distress | 675 (22.6) | 1260 (15.8) | 17.3 |
| Obstetric hemorrhage | 8 (0.3) | 8 (0.1) | 3.9 |
| Placental abruption | 375 (12.5) | 87 (1.1) | 46.6 |
| Placenta accreta | 51 (1.7) | 27 (0.3) | 13.6 |
| Placental dysfunction | 353 (11.8) | 476 (6.0) | 20.6 |
| Umbilical cord prolapse | 70 (2.3) | 102 (1.3) | 8.0 |
| Uterine rupture | 20 (0.7) | 12 (0.2) | 8.1 |
| Type of cesarean delivery | |||
| Elective (K898-2) | 1093 (36.5) | 5343 (67.0) | 63.9 |
| Emergency (K898-1) | 1726 (57.7) | 2575 (32.3) | 52.8 |
| Cesarean delivery with placenta previa or preterm birth (K898-3) * | 173 (5.8) | 62 (0.8) | 28.4 |
| Fiscal year | |||
| 2005–2009 | 231 (7.7) | 626 (7.8) | 0.5 |
| 2010–2014 | 874 (29.2) | 2588 (32.4) | 7.0 |
| 2015–2020 | 1887 (63.1) | 4766 (59.7) | 6.9 |
| Number of beds | |||
| 0–19 | 520 (17.4) | 4047 (50.7) | 75.1 |
| 20–99 | 346 (11.6) | 1429 (17.9) | 18.0 |
| 100–199 | 48 (1.6) | 227 (2.8) | 8.4 |
| 200–299 | 81 (2.7) | 358 (4.5) | 9.6 |
| 300–499 | 419 (14.0) | 1152 (14.4) | 1.2 |
| >499 | 1578 (52.7) | 767 (9.6) | 105.2 |
| Academic hospital | 656 (21.9) | 174 (2.2) | 63.6 |
| DPC payment system hospital | 2109 (70.5) | 2380 (29.8) | 89.0 |
| L008 with NMBAs, n = 2992 | L008 without NMBAs, n = 7980 | Absolute SMD (%) | |
|---|---|---|---|
| NMBAs * | 2992 (100) | 0 (0) | |
| Rocuronium | 2349 (78.5) | 0 (0) | 270.3 |
| Suxamethonium | 1014 (33.9) | 0 (0) | 101.2 |
| Vecuronium | 298 (10.0) | 0 (0) | 47.0 |
| Pancuronium | 36 (1.2) | 0 (0) | 15.6 |
| Anesthetics | |||
| Propofol | 1855 (62.0) | 3425 (42.9) | 38.9 |
| Barbiturate | 1422 (47.5) | 326 (4.1) | 114.3 |
| Benzodiazepine | 391 (13.1) | 1487 (18.6) | 15.3 |
| Volatile halogenated agents | 2030 (67.8) | 1202 (15.1) | 126.9 |
| Nitrous oxide | 1237 (41.3) | 5064 (63.5) | 45.4 |
| Ketamine | 212 (7.1) | 791 (9.9) | 10.1 |
| Analgesics | |||
| Fentanyl | 2040 (68.2) | 2951 (37.0) | 65.8 |
| Remifentanil | 1447 (48.4) | 15 (0.2) | 135.8 |
| Morphine (any route) | 239 (8.0) | 1171 (14.7) | 21.2 |
| Local anesthetic for spinal anesthesia | 423 (14.1) | 5103 (63.9) | 118.7 |
| Bupivacaine for spinal anesthesia | 410 (13.7) | 4637 (58.1) | 104.4 |
| Local anesthetic for epidural anesthesia | 1032 (34.5) | 4463 (55.9) | 44.1 |
| 2% Lidocaine | 85 (2.8) | 602 (7.5) | 21.3 |
| 2% Mepivacaine | 65 (2.2) | 1154 (14.5) | 45.6 |
| Ropivacaine | 728 (24.3) | 3012 (37.7) | 29.3 |
| Levobupivacaine | 232 (7.8) | 378 (4.7) | 12.5 |
| Bupivacaine, excluding for spinal anesthesia | 46 (1.5) | 881 (11.0) | 39.9 |
| Code L003: continuous infusion of local anesthetic after epidural anesthesia | 349 (11.7) | 3105 (38.9) | 66.0 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yonekura, H.; Mazda, Y.; Noguchi, S.; Tsunobuchi, H.; Shimaoka, M. Current Epidemiology of the General Anesthesia Practice for Cesarean Delivery Using a Nationwide Claims Database in Japan: A Descriptive Study. J. Clin. Med. 2022, 11, 4808. https://doi.org/10.3390/jcm11164808
Yonekura H, Mazda Y, Noguchi S, Tsunobuchi H, Shimaoka M. Current Epidemiology of the General Anesthesia Practice for Cesarean Delivery Using a Nationwide Claims Database in Japan: A Descriptive Study. Journal of Clinical Medicine. 2022; 11(16):4808. https://doi.org/10.3390/jcm11164808
Chicago/Turabian StyleYonekura, Hiroshi, Yusuke Mazda, Shohei Noguchi, Hironaka Tsunobuchi, and Motomu Shimaoka. 2022. "Current Epidemiology of the General Anesthesia Practice for Cesarean Delivery Using a Nationwide Claims Database in Japan: A Descriptive Study" Journal of Clinical Medicine 11, no. 16: 4808. https://doi.org/10.3390/jcm11164808
APA StyleYonekura, H., Mazda, Y., Noguchi, S., Tsunobuchi, H., & Shimaoka, M. (2022). Current Epidemiology of the General Anesthesia Practice for Cesarean Delivery Using a Nationwide Claims Database in Japan: A Descriptive Study. Journal of Clinical Medicine, 11(16), 4808. https://doi.org/10.3390/jcm11164808






