Obstetric Anesthesia Practice in the Tertiary Care Center: A 7-Year Retrospective Study and the Impact of the COVID-19 Pandemic on Obstetric Anesthesia Practice
Abstract
:1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Caesarean Sections Rate—OECD Data. Available online: https://data.oecd.org/healthcare/caesarean-sections.htm (accessed on 20 March 2022).
- Kinsella, S.M.; Winton, A.L.; Mushambi, M.C.; Ramaswamy, K.; Swales, H.; Quinn, A.C.; Popat, M. Failed tracheal intubation during obstetric general anaesthesia: A literature review. Int. J. Obstet. Anesth. 2015, 24, 356–374. [Google Scholar] [CrossRef] [Green Version]
- Odor, P.M.; Bampoe, S.; Lucas, D.N.; Moonesinghe, S.R.; Andrade, J.; Pandit, J.J.; Pan-London Peri-operative Audit and Research Network (PLAN), for the DREAMY Investigators Group. Incidence of accidental awareness during general anaesthesia in obstetrics: A multicentre, prospective cohort study. Anaesthesia 2021, 76, 759–776. [Google Scholar] [CrossRef]
- Kearns, R.J.; Shaw, M.; Gromski, P.S.; Iliodromiti, S.; Pell, J.P.; Lawlor, D.A.; Nelson, S.M. Neonatal and early childhood outcomes following maternal anesthesia for cesarean section: A population-based cohort study. Reg. Anesth. Pain Med. 2021, 46, 482–489. [Google Scholar] [CrossRef]
- Carvalho, B.; Mhyre, J.M. Centers of excellence for anesthesia care of obstetric patients. Anesth. Analg. 2019, 128, 844–846. [Google Scholar] [CrossRef]
- Raising the Standard: A compendium of Audit Recipes for Continuous Quality Improvement in Anaesthesia. The Royal College of Anaesthetists. Available online: https://www.rcoa.ac.uk/sites/default/files/documents/2019-09/CSQ-ARB-2012_0.pdf (accessed on 20 March 2022).
- Bampoe, S.; Odor, P.; Lucas, D. Novel coronavirus SARS-CoV-2 and COVID-19. Practice recommendations for obstetric anesthesia: What we have learned thus far. Int. J. Obstet. Anesth. 2020, 43, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Shatil, B.; Smiley, R. Neuraxial analgesia for labour. BJA Educ. 2020, 20, 96–102, Erratum in BJA Educ. 2020, 20, 250. [Google Scholar] [CrossRef] [PubMed]
- R Core Team. R: A Language and Environment for Statistical Computing. 2022. R Foundation for Statistical Computing, Vienna, Austria. Available online: https://www.R-project.org/ (accessed on 20 March 2022).
- Association of Anaesthetists of Great Britain & Ireland; Obstetric Anaesthetists’ Association; Regional Anaesthesia UK. Regional anaesthesia and patients with abnormalities of coagulation. Anaesthesia 2013, 68, 966–972. [Google Scholar] [CrossRef] [PubMed]
- Traynor, A.J.; Aragon, M.; Ghosh, D.; Choi, R.S.; Dingmann, C.; Vu, T.Z.; Bucklin, B.A. Obstetric anesthesia workforce survey: A 30-year update. Anesth. Analg. 2016, 122, 1939–1946. [Google Scholar] [CrossRef]
- Butwick, A.; El-Sayed, Y.; Blumenfeld, Y.; Osmundson, S.; Weiniger, C. Mode of anaesthesia for preterm Caesarean delivery: Secondary analysis from the maternal-fetal medicine units network caesarean registry. Br. J. Anaesth. 2015, 115, 267–274. [Google Scholar] [CrossRef] [Green Version]
- Bhatia, K.; Columb, M.; Bewlay, A.; Eccles, J.; Hulgur, M.; Jayan, N.; Lie, J.; Verma, D.; Parikh, R. The effect of COVID-19 on general anaesthesia rates for caesarean section. A cross-sectional analysis of six hospitals in the north-west of England. Anaesthesia 2021, 76, 312–319. [Google Scholar] [CrossRef]
- Ikeda, T.; Kato, A.; Bougaki, M.; Araki, Y.; Ohata, T.; Kawashima, S.; Imai, Y.; Ninagawa, J.; Oba, K.; Chang, K.; et al. A retrospective review of 10-year trends in general anesthesia for cesarean delivery at a university hospital: The impact of a newly launched team on obstetric anesthesia practice. BMC Health Serv. Res. 2020, 13, 421. [Google Scholar] [CrossRef]
- Ring, L.; Landau, R.; Delgado, C. The current role of general anesthesia for cesarean delivery. Curr. Anesthesiol. Rep. 2021, 11, 18–27. [Google Scholar] [CrossRef]
- Bauer, M.E.; Arendt, K.; Beilin, Y.; Gernsheimer, T.; Botero, J.P.; James, A.H.; Yaghmour, E.; Toledano, R.D.; Turrentine, M.; Houle, T.; et al. The Society for Obstetric Anesthesia and Perinatology Interdisciplinary Consensus Statement on neuraxial procedures in obstetric patients with thrombocytopenia. Anesth. Analg. 2021, 132, 1531–1544. [Google Scholar] [CrossRef]
- Mushambi, M.C.; Kinsella, S.M.; Popat, M.; Swales, H.; Ramaswamy, K.K.; Winton, A.L.; Quinn, A.C.; Obstetric Anaesthetists’ Association; Difficult Airway Society. Obstetric Anaesthetists’ Association and Difficult Airway Society guidelines for the management of difficult and failed tracheal intubation in obstetrics. Anaesthesia 2015, 70, 1286–1306. [Google Scholar] [CrossRef]
- Mayzner-Zawadzka, E.; Kruszyński, Z.; Gaca, M.; Maciejewski, D.; Nowacka, E.; Grupa Robocza Zarzadu Głównego Polskiego Towarzystwa Anestezjologii i Intensywnej Terapii. Analgezja zewnatrzoponowa porodu—Wytyczne [Guidelines for obstetric analgesia services]. Anestezjol. Intens. Ter. 2009, 41, 114–118. [Google Scholar]
- Kinsella, S.M. A prospective audit of regional anaesthesia failure in 5080 Caesarean sections. Anaesthesia 2008, 63, 822–832. [Google Scholar] [CrossRef]
- Metodiev, Y.; Mushambi, M. Supraglottic airway devices for Caesarean delivery under general anaesthesia: For all, for none, or for some? Br. J. Anaesth. 2020, 125, e7–e11. [Google Scholar] [CrossRef]
- Powers, J.R.; Loxton, D.J.; O’Mara, A.T.; Chojenta, C.L.; Ebert, L. Regardless of where they give birth, women living in non-metropolitan areas are less likely to have an epidural than their metropolitan counterparts. Women Birth 2013, 26, e77–e81. [Google Scholar] [CrossRef]
- Räisänen, S.; Kokki, M.; Kokki, H.; Gissler, M.; Kramer, M.; Heinonen, S. The use of epidural analgesia for intrapartum pain relief in publicly funded healthcare. Acta Anaesthesiol. Scand. 2014, 58, 291–297. [Google Scholar] [CrossRef]
- Laine, K.; Räisänen, S. Effect of maternal country of birth on intrapartum epidural use—A population-based register study of 602 095 deliveries. Eur. J. Obstet. Gynecol. Reprod. Biol. 2020, 250, 41–47. [Google Scholar] [CrossRef]
- Waldum, H.; Jacobsen, A.F.; Lukasse, M.; Staff, A.C.; Falk, R.S.; Vangen, S.; Sørbye, I.K. The provision of epidural analgesia during labor according to maternal birthplace: A Nor-wegian register study. BMC Pregnancy Childbirth 2020, 26, 321. [Google Scholar] [CrossRef]
| Procedure | 2014 | 2015 | 2016 | 2017 | 2018 | 2019 | 2020 |
|---|---|---|---|---|---|---|---|
| Vaginal delivery * | 332 (29.72%) | 478 (36.23%) | 401 (32.73%) | 353 (26.20%) | 357 (27.56%) | 389 (32.99%) | 360 (32.90%) |
| Cesarean sections | 1816 | 1819 | 1914 | 1852 | 1837 | 1669 | 1550 |
| Other obstetric procedures | 101 | 129 | 124 | 116 | 123 | 104 | 106 |
| Cesarean Section | |||||||
|---|---|---|---|---|---|---|---|
| Anesthesia | Year | ||||||
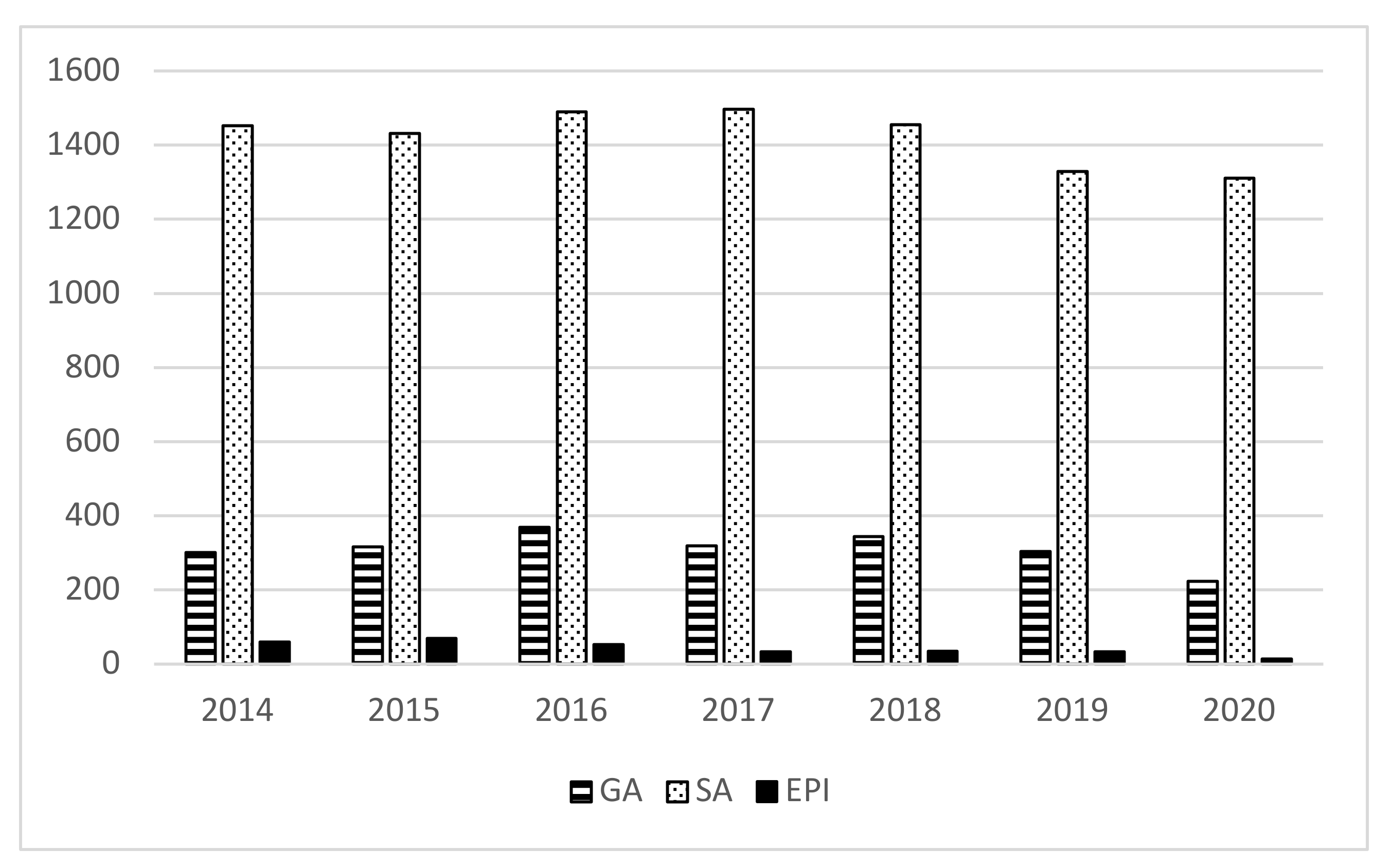
| 2014 (n = 1816) | 2015 (n = 1819) | 2016 (n = 1914) | 2017 (n = 1852) | 2018 (n = 1837) | 2019 (n = 1669) | 2020 * (n = 1550) | |
| GA | 246 (13.55%) | 242 (13.30%) | 293 (15.31%) | 280 (15.11%) | 296 (16.10%) | 258 (15.46%) | 184 (11.87%) |
| SA | 1447 (79.68%) | 1408 (77.41%) | 1459 (76.23%) | 1467 (79.21%) | 1435 (78.22%) | 1308 (78.37%) | 1263 (81.48%) |
| EPI | 61 (3.36%) | 70 (3.85%) | 54 (2.82%) | 34 (1.84%) | 36 (1.96%) | 34 (2.04%) | 15 (0.97%) |
| SA >> GA | 39 (2.15%) | 51 (2.80%) | 41 (2.11%) | 22 (1.19%) | 31 (1.68%) | 27 (1.62%) | 33 (2.13%) |
| EPI >> GA | 17 (0.94%) | 24 (1.32%) | 35 (1.83%) | 18 (0.97%) | 18 (0.98%) | 20 (1.20%) | 7 (0.45%) |
| EPI >> SA | 6 (0.33%) | 24 (1.32%) | 32 (1.67%) | 31 (1.67%) | 21 (1.14%) | 22 (1.32%) | 48 (3.10%) |
| Other Obstetric Procedures (Manual Removal of Retained Placenta, Inspection, and Suturing of the Perineum) | |||||||
| Anesthesia | Year | ||||||
| 2014 (n = 101) | 2015 (n = 129) | 2016 (n = 124) | 2017 (n = 116) | 2018 (n = 123) | 2019 (n = 104) | 2020 * (n = 106) | |
| GA | 13 (12.87%) | 22 (17.05%) | 23 (18.55%) | 25 (21.55%) | 26 (21.14%) | 17 (16.35%) | 9 (8.49%) |
| IVA | 28 (27.72%) | 31 (24.03%) | 31 (25.00%) | 30 (25.86%) | 35 (28.46%) | 15 (14.42%) | 8 (7.55%) |
| SA | 48 (47.52%) | 51 (39.53%) | 45 (36.29%) | 53 (45.69%) | 45 (36.58%) | 46 (44.23%) | 65 (61.32%) |
| EPI | 11 (10.89%) | 23 (17.83%) | 23 (18.55%) | 6 (5.17%) | 15 (11.20%) | 21 (20.19%) | 19 (17.93%) |
| SA >> GA | 0 (0.00%) | 1 (0.78%) | 0 (0.00%) | 0 (0.00%) | 1 (0.81%) | 1 (0.96%) | 0 (0.00%) |
| EPI >> GA | 1 (0.99%) | 0 (0.00%) | 1 (0.81%) | 0 (0.00%) | 1 (0.81%) | 2 (1.92%) | 1 (0.94%) |
| EPI >> SA | 0 (0.00%) | 1 (0.78%) | 1 (0.81%) | 2 (1.72%) | 0 (0.00%) | 2 (1.92%) | 4 (3.77%) |
| Vaginal Delivery | |||||||
| Anesthesia | Year | ||||||
| 2014 (n = 332) | 2015 (n = 478) | 2016 (n = 401) | 2017 (n = 353) | 2018 (n = 357) | 2019 (n = 389) | 2020 (n = 360) | |
| SA | 63 (18.98%) | 64 (13.39%) | 56 (13.96%) | 73 (20.68%) | 44 (12.33%) | 56 (14.40%) | 63 (17.50%) |
| EPI | 269 (81.02%) | 412 (86.19%) | 342 (85.29%) | 275 (77.90%) | 311 (87.11%) | 331 (85.08%) | 293 (81.40%) |
| CSE | 0 (0.00%) | 2 (0.42%) | 3 (0.75%) | 5 (1.42%) | 2 (0.56%) | 2 (0.52%) | 4 (1.10%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Krawczyk, P.; Jaśkiewicz, R.; Huras, H.; Kołak, M. Obstetric Anesthesia Practice in the Tertiary Care Center: A 7-Year Retrospective Study and the Impact of the COVID-19 Pandemic on Obstetric Anesthesia Practice. J. Clin. Med. 2022, 11, 3183. https://doi.org/10.3390/jcm11113183
Krawczyk P, Jaśkiewicz R, Huras H, Kołak M. Obstetric Anesthesia Practice in the Tertiary Care Center: A 7-Year Retrospective Study and the Impact of the COVID-19 Pandemic on Obstetric Anesthesia Practice. Journal of Clinical Medicine. 2022; 11(11):3183. https://doi.org/10.3390/jcm11113183
Chicago/Turabian StyleKrawczyk, Paweł, Remigiusz Jaśkiewicz, Hubert Huras, and Magdalena Kołak. 2022. "Obstetric Anesthesia Practice in the Tertiary Care Center: A 7-Year Retrospective Study and the Impact of the COVID-19 Pandemic on Obstetric Anesthesia Practice" Journal of Clinical Medicine 11, no. 11: 3183. https://doi.org/10.3390/jcm11113183
APA StyleKrawczyk, P., Jaśkiewicz, R., Huras, H., & Kołak, M. (2022). Obstetric Anesthesia Practice in the Tertiary Care Center: A 7-Year Retrospective Study and the Impact of the COVID-19 Pandemic on Obstetric Anesthesia Practice. Journal of Clinical Medicine, 11(11), 3183. https://doi.org/10.3390/jcm11113183






