Holter ECG for Syncope Evaluation in the Internal Medicine Department—Choosing the Right Patients
Abstract
:1. Introduction
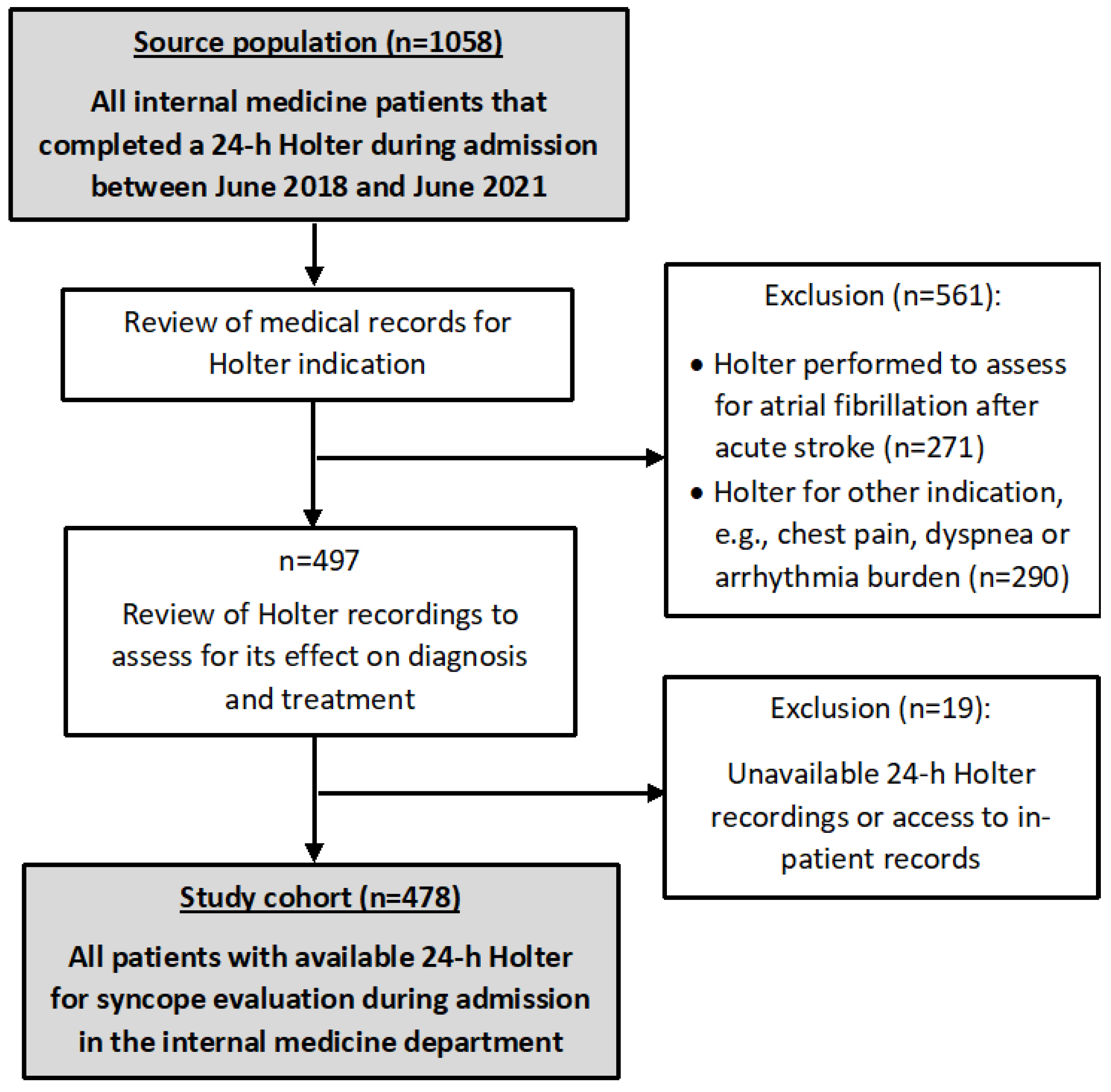
2. Materials and Methods
2.1. Study Design and Participants
2.2. ECG and Holter ECG
2.3. Outcomes
2.4. Statistical Analysis
3. Results
3.1. Subject Characteristics
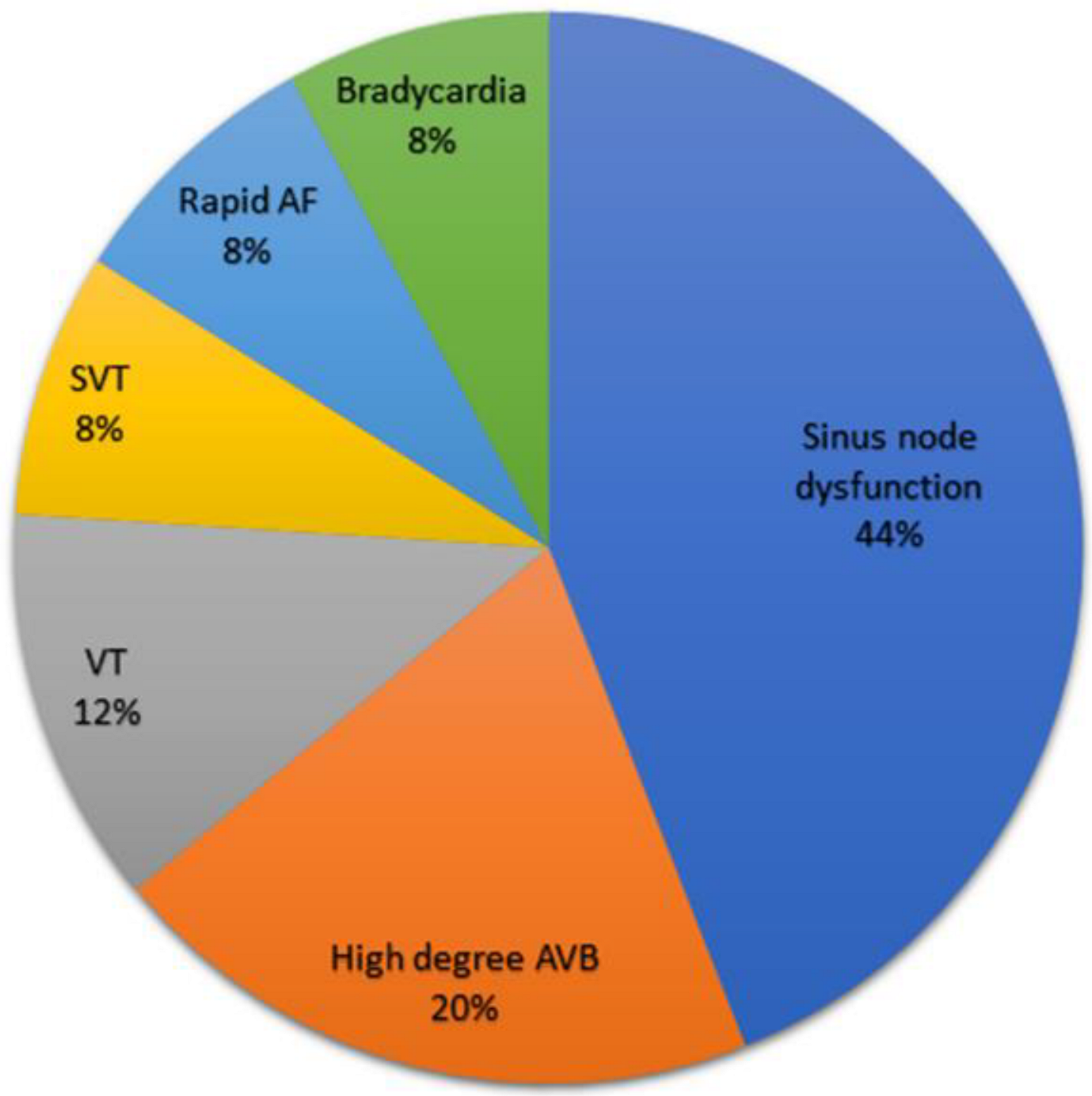
3.2. Holter Outcomes
3.3. Predictors for a Diagnostic Holter
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kapoor, W.N. Diagnostic evaluation of syncope. Am. J. Med. 1991, 90, 91–106. [Google Scholar] [CrossRef]
- Linzer, M.; Yang, E.H.; Estes, N.A.M.; Wang, P.; Vorperian, V.R.; Kapoor, W.N. Diagnosing syncope. Part 2: Unexplained syncope. Ann. Intern. Med. 1997, 127, 76–86. [Google Scholar] [CrossRef] [PubMed]
- Sheldon, R.S.; Grubb, B.P.; Olshansky, B.; Shen, W.K.; Calkins, H.; Brignole, M.; Satish, R.; Raj, S.R.; Krahn, A.D.; Morillo, C.A.; et al. 2015 Heart Rhythm Society Expert Consensus Statement on the Diagnosis and Treatment of Postural Tachycardia Syndrome, Inappropriate Sinus Tachycardia, and Vasovagal Syncope. Hear Rhythm. 2017, 12, E41–E63. [Google Scholar] [CrossRef] [PubMed]
- Shen, W.-K.; Sheldon, R.S.; Benditt, D.G.; Cohen, M.I.; Forman, D.E.; Goldberger, Z.D.; Grubb, B.P.; Hamdan, M.H.; Krahn, A.D.; Link, M.S.; et al. 2017 ACC/AHA/HRS Guideline for the Evaluation and Management of Patients with Syncope: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. Circulation 2017, 136, e60–e122. [Google Scholar] [CrossRef]
- Brignole, M.; Moya, A.; De Lange, F.J.; Deharo, J.-C.; Elliott, P.M.; Fanciulli, A.; Fedorowski, A.; Furlan, R.; Kenny, R.A.; Martínez, A.M.; et al. 2018 ESC Guidelines for the diagnosis and management of syncope. Eur. Heart J. 2018, 39, 1883–1948. [Google Scholar] [CrossRef] [PubMed]
- Drew, B.J.; Califf, R.M.; Funk, M.; Kaufman, E.S.; Krucoff, M.W.; Laks, M.M.; Macfarlane, P.W.; Sommargren, C.; Swiryn, S.; Van Hare, G.F. Practice standards for electrocardiographic monitoring in hospital settings: An American Heart Association scientific statement from the councils on cardiovascular nursing, clinical cardiology, and cardiovascular disease in the young. Circulation 2004, 110, 2721–2746. [Google Scholar] [CrossRef]
- Chua, S.K.; Chen, L.C.; Lien, L.M.; Lo, H.M.; Liao, Z.Y.; Chao, S.P.; Chuang, C.-Y.; Chiu, C.-Z. Comparison of arrhythmia detection by 24-hour holter and 14-day continuous electrocardiography patch monitoring. Acta Cardiol. Sin. 2020, 36, 251–259. [Google Scholar] [CrossRef]
- Croci, F.; Brignole, M.; Alboni, P.; Menozzi, C.; Raviele, A.; Del Rosso, A.; Dinelli, M.; Solano, A.; Bottoni, N.; Donateo, P. The application of a standardized strategy of evaluation in patients with syncope referred to three syncope units. Europace 2002, 4, 351–355. [Google Scholar] [CrossRef]
- Kühne, M.; Schaer, B.; Sticherling, C.; Osswald, S. Holter monitoring in syncope: Diagnostic yield in octogenarians. J. Am. Geriatr. Soc. 2011, 59, 1293–1298. [Google Scholar] [CrossRef]
- Chiu, D.T.; Shapiro, N.I.; Sun, B.C.; Mottley, J.L.; Grossman, S.A. Are echocardiography, telemetry, ambulatory electrocardiography monitoring, and cardiac enzymes in emergency department patients presenting with syncope useful tests? A preliminary investigation. J. Emerg. Med. 2014, 47, 113–118. [Google Scholar] [CrossRef]
- Farwell, D.; Sulke, N. How do we diagnose syncope? J. Cardiovasc. Electrophysiol. 2002, 13 (Suppl. 1), S9–S13. [Google Scholar] [CrossRef] [PubMed]
- Del Rosso, A.; Ungar, A.; Maggi, R.; Giada, F.; Petix, N.R.; De Santo, T.; Menozzi, C.; Brignole, M. Clinical predictors of cardiac syncope at initial evaluation in patients referred urgently to a general hospital: The EGSYS score. Heart 2008, 94, 1620–1626. [Google Scholar] [CrossRef] [PubMed]
- Sud, S.; Klein, G.J.; Skanes, A.C.; Gula, L.J.; Yee, R.; Krahn, A.D. Predicting the cause of syncope from clinical history in patients undergoing prolonged monitoring. Hear Rhythm. 2009, 6, 238–243. [Google Scholar] [CrossRef] [PubMed]
- Thiruganasambandamoorthy, V.; Hess, E.P.; Turko, E.; Tran, M.-L.; Wells, G.A.; Stiell, I.G. Defining abnormal electrocardiography in adult emergency department syncope patients: The Ottawa Electrocardiographic Criteria. Can. J. Emerg. Med. 2012, 14, 252–262. [Google Scholar] [CrossRef]
- Kühne, M.; Schaer, B.; Moulay, N.; Sticherling, C.; Osswald, S. Holter monitoring for syncope: Diagnostic yield in different patient groups and impact on device implantation. Qjm 2007, 100, 771–777. [Google Scholar] [CrossRef]
- Mendu, M.L.; McAvay, G.; Lampert, R.; Stoehr, J.; Tinetti, M.E. Yield of diagnostic tests in evaluating syncopal episodes in older patients. Arch. Intern. Med. 2009, 169, 1299–1305. [Google Scholar] [CrossRef]
- Locati, E.; Moya, A.; Oliveira, M.; Tanner, H.; Willems, R.; Lunati, M.; Brignole, M. External prolonged electrocardiogram monitoring in unexplained syncope and palpitations: Results of the SYNARR-flash study. Europace 2016, 18, 1265–1272. [Google Scholar] [CrossRef]
- Benezet-Mazuecos, J.; Ibanez, B.; Rubio, J.M.; Navarro, F.; Martín, E.; Romero, J.; Farre, J. Utility of in-hospital cardiac remote telemetry in patients with unexplained syncope. Europace 2007, 9, 1196–1201. [Google Scholar] [CrossRef]
- Goldberger, Z.D.; Petek, B.J.; Brignole, M.; Shen, W.-K.; Sheldon, R.S.; Solbiati, M.; Deharo, J.-C.; Moya, A.; Hamdan, M.H. ACC/AHA/HRS Versus ESC Guidelines for the Diagnosis and Management of Syncope: JACC Guideline Comparison. J. Am. Coll. Cardiol. 2019, 74, 2410–2423. [Google Scholar] [CrossRef]
- Krahn, A.D.; Klein, G.J.; Norris, C.; Yee, R. The Etiology of Syncope in Patients With Negative Tilt Table and Electrophysiological Testing. Circulation 1995, 92, 1819–1824. [Google Scholar] [CrossRef]
- Sarasin, F.P.; Carballo, D.; Slama, S.; Louis-Simonet, M. Usefulness of 24-h Holter monitoring in patients with unexplained syncope and a high likelihood of arrhythmias. Int. J. Cardiol. 2005, 101, 203–207. [Google Scholar] [CrossRef] [PubMed]
- Hauck, K.; Zhao, X. How dangerous is a day in hospital? A model of adverse events and length of stay for medical inpatients. Med. Care 2011, 49, 1068–1075. [Google Scholar] [CrossRef] [PubMed]
- Rockx, M.A.; Hoch, J.S.; Klein, G.J.; Yee, R.; Skanes, A.C.; Gula, L.J.; Krahn, A.D. Is ambulatory monitoring for “community-acquired” syncope economically attractive? A cost-effectiveness analysis of a randomized trial of external loop recorders versus Holter monitoring. Am. Heart J. 2005, 150, 1065. [Google Scholar] [CrossRef] [PubMed]
- Brignole, M.; Menozzi, C.; Bartoletti, A.; Giada, F.; Lagi, A.; Ungar, A.; Ponassi, I.; Mussi, C.; Maggi, R.; Re, G.; et al. A new management of syncope: Prospective systematic guideline-based evaluation of patients referred urgently to general hospitals. Eur. Heart J. 2006, 27, 76–82. [Google Scholar] [CrossRef]
| SVT or AF with a ventricular response of more than 150 bpm, lasting over 32 beats. |
| VT lasting over 32 beats. |
| Sinus pauses longer than 3 s. |
| Bradycardia of less than 40 bpm. |
| Complete AV block or second-degree AV block Mobitz type 2. |
| Alternating bundle branch block. |
| Characteristic | Study Cohort n = 478 (%) | Diagnostic Holter n = 25 (%) | Non-Diagnostic n = 453 (%) | p Value |
|---|---|---|---|---|
| Age, mean ± SD, y | 75 ± 14 | 82 ± 6.2 | 74 ± 14.5 | <0.001 |
| Female gender | 217 (45) | 9 (36) | 16 (64) | 0.332 |
| Hypertension | 295 (62) | 19 (76) | 276 (61) | 0.131 |
| Diabetes mellitus | 140 (29) | 11 (44) | 129 (28.5) | 0.097 |
| Hyperlipidemia | 263 (55) | 17 (68) | 246 (54.5) | 0.188 |
| TIA/CVA | 82 (17) | 8 (32) | 74 (16) | 0.043 |
| Heart Failure * | 0.004 | |||
| HFrEF | 16 (3.3) | 1 (4) | 15 (3.3) | |
| HFpEF | 35 (7.3) | 6 (24) | 29 (6.4) | |
| Ischemic heart disease | 119 (25) | 6 (24) | 113 (25) | 0.910 |
| Structural heart disease † | 83 (17) | 8 (32) | 75 (17) | 0.047 |
| Atrial fibrillation | 88 (18) | 10 (40) | 78 (17) | 0.004 |
| Beta blocker use | 193 (40) | 17 (68) | 176 (39) | 0.004 |
| ND-CCB use | 4 (0.8) | 0 | 4 (0.9) | 0.637 |
| Antiarrhythmic drugs | 18 (3.8) | 0 | 18 (4) | 0.310 |
| COPD | 40 (8.4) | 5 (20) | 35 (8) | 0.031 |
| Study Cohort n = 478 (%) | Diagnostic Holter n = 25 (%) | Non-Diagnostic n = 453 (%) | p Value | |
|---|---|---|---|---|
| Time from event to Holter, mean ± SD, d | 3.22 ± 3.23 | 2.04 ± 2.05 | 3.28 ± 3.35 | <0.001 |
| Time from admission to Holter, mean ± SD, d | 2.63 ± 2.63 | 1.24 ± 0.92 | 2.71 ± 2.67 | <0.001 |
| Recurrent syncope * | 82 (17) | 6 (24) | 76 (17) | 0.351 |
| Prior syncope admission | 72 (15) | 2 (8) | 70 (15.5) | 0.309 |
| Pre-syncopal symptoms † | 226 (47) | 9 (36) | 217 (48) | 0.242 |
| Chest pain | 22 (4.6) | 0 | 22 (5) | 0.259 |
| Palpitations | 26 (5.4) | 0 | 26 (6) | 0.218 |
| Event during effort | 23 (4.8) | 1 (4) | 22 (5) | 0.846 |
| Event at rest | 150 (31) | 10 (40) | 140 (40) | 0.340 |
| Oxygen saturation ≤ 93% § | 39 (8.1) | 1 | 38 (8) | 0.435 |
| Fever > 38 °C | 13 (3.0) | 0 | 13 (3) | 0.390 |
| Hemoglobin (g/dL) ¶ | 13.0 ± 1.8 | 12.8 ± 1.5 | 13.0 ± 1.8 | 0.584 |
| Cardiac exam findings # | 114 (24) | 9 (36) | 105 (23) | 0.143 |
| Abnormal ECG | 245 (51) | 18 (72) | 227 (50) | 0.033 |
| Traumatic syncope | 46 (9.6) | 4 (16) | 42 (9) | 0.267 |
| Hospital stay duration, mean ± SD, d | 7.4 ± 6.4 | 9.6 ± 9.9 | 7.3 ± 6.1 | 0.260 |
| In hospital death | 2 (0.4) | 0 | 2 (0.4) | 0.739 |
| Variable | Univariate Analysis | Multivariate Analysis | ||
|---|---|---|---|---|
| Standardized β | p | Standardized β | p | |
| Age | 0.15 | <0.01 | 0.08 | 0.07 |
| Heart disease * | 0.06 | 0.17 | 0.01 | 0.78 |
| COPD | −0.01 | 0.76 | −0.03 | 0.51 |
| Abnormal ECG | 0.11 | 0.02 | 0.07 | 0.11 |
| Time from admission to Holter | 0.34 | <0.01 | 0.33 | <0.01 |
| Variable | Univariate Analysis | Multivariate Analysis | ||
|---|---|---|---|---|
| Odds Ratio (95% CI) | p | Odds Ratio (95% CI) | p | |
| Age per 5 years | 1.86 (1.61–2.15) | <0.01 | 1.35 (1.08–1.68) | <0.01 |
| Reduced EF | 1.52 (0.19–12.11) | 0.69 | 1.31 (0.16–10.66) | 0.80 |
| Preserved EF | 4.70 (1.73–10.11) | <0.01 | 4.10 (1.43–11.72) | <0.01 |
| Event to Holter duration | 0.78 (0.67–0.93) | <0.01 | 0.73 (0.56–0.96) | 0.02 |
| Variable | Univariate Analysis | Multivariate Analysis | ||
|---|---|---|---|---|
| Odds Ratio (95% CI) | p | Odds Ratio (95% CI) | p | |
| Age | 1.07 (1.02–1.11) | <0.01 | 1.05 (0.99–1.10) | 0.06 |
| Heart disease † | 2.65 (1.15–6.10) | 0.022 | 1.79 (0.75–4.27) | 0.19 |
| Beta blocker use | 3.33 (1.41–7.88) | <0.01 | 2.36 (0.98–5.68) | 0.06 |
| Cardiac exam findings | 1.86 (0.80–4.34) | 0.14 | 1.21 (0.50–2.95) | 0.67 |
| Abnormal ECG | 2.56 (1.05–6.25) | 0.03 | 1.53 (0.59–3.96) | 0.38 |
| Traumatic syncope | 1.86 (0.61–5.68) | 0.27 | 1.77 (0.56–5.60) | 0.33 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Freund, O.; Caspi, I.; Shacham, Y.; Frydman, S.; Biran, R.; Abu Katash, H.; Zornitzki, L.; Bornstein, G. Holter ECG for Syncope Evaluation in the Internal Medicine Department—Choosing the Right Patients. J. Clin. Med. 2022, 11, 4781. https://doi.org/10.3390/jcm11164781
Freund O, Caspi I, Shacham Y, Frydman S, Biran R, Abu Katash H, Zornitzki L, Bornstein G. Holter ECG for Syncope Evaluation in the Internal Medicine Department—Choosing the Right Patients. Journal of Clinical Medicine. 2022; 11(16):4781. https://doi.org/10.3390/jcm11164781
Chicago/Turabian StyleFreund, Ophir, Inbar Caspi, Yacov Shacham, Shir Frydman, Roni Biran, Hytham Abu Katash, Lior Zornitzki, and Gil Bornstein. 2022. "Holter ECG for Syncope Evaluation in the Internal Medicine Department—Choosing the Right Patients" Journal of Clinical Medicine 11, no. 16: 4781. https://doi.org/10.3390/jcm11164781
APA StyleFreund, O., Caspi, I., Shacham, Y., Frydman, S., Biran, R., Abu Katash, H., Zornitzki, L., & Bornstein, G. (2022). Holter ECG for Syncope Evaluation in the Internal Medicine Department—Choosing the Right Patients. Journal of Clinical Medicine, 11(16), 4781. https://doi.org/10.3390/jcm11164781






