Lung Transplant for ARDS after COVID-19: Long-Term Outcomes and Considerations about Detrimental Issues
Abstract
:1. Introduction
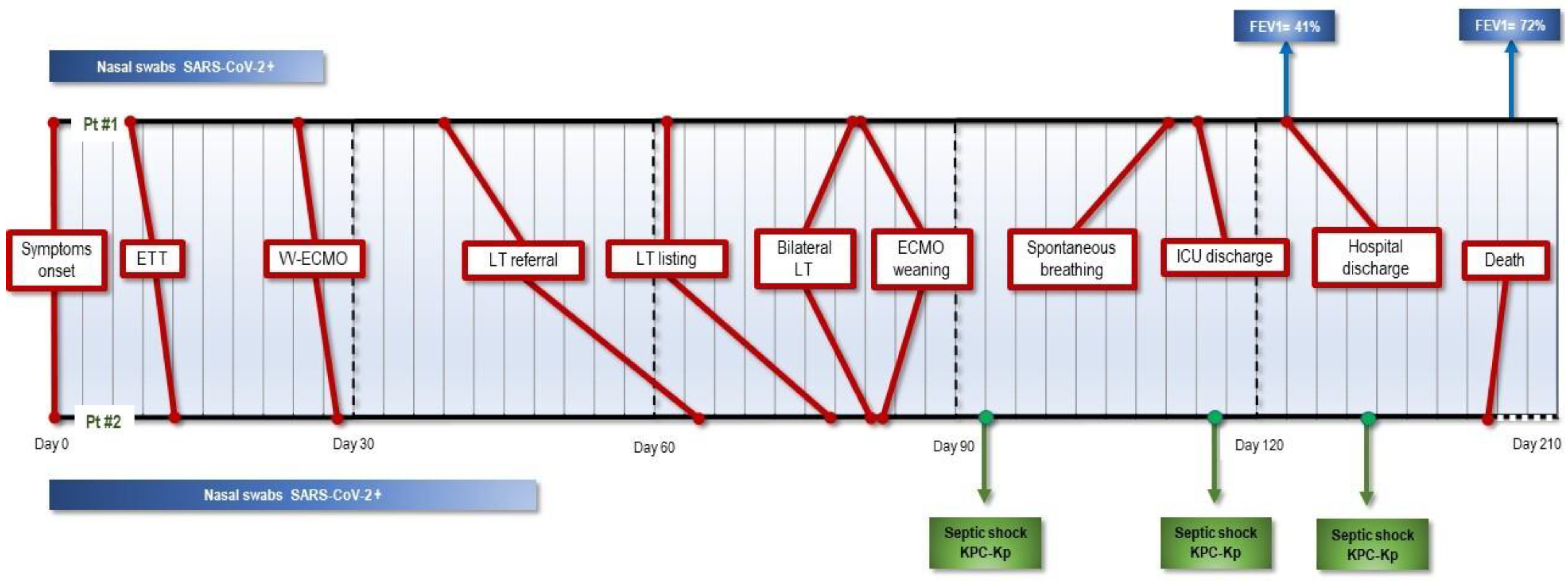
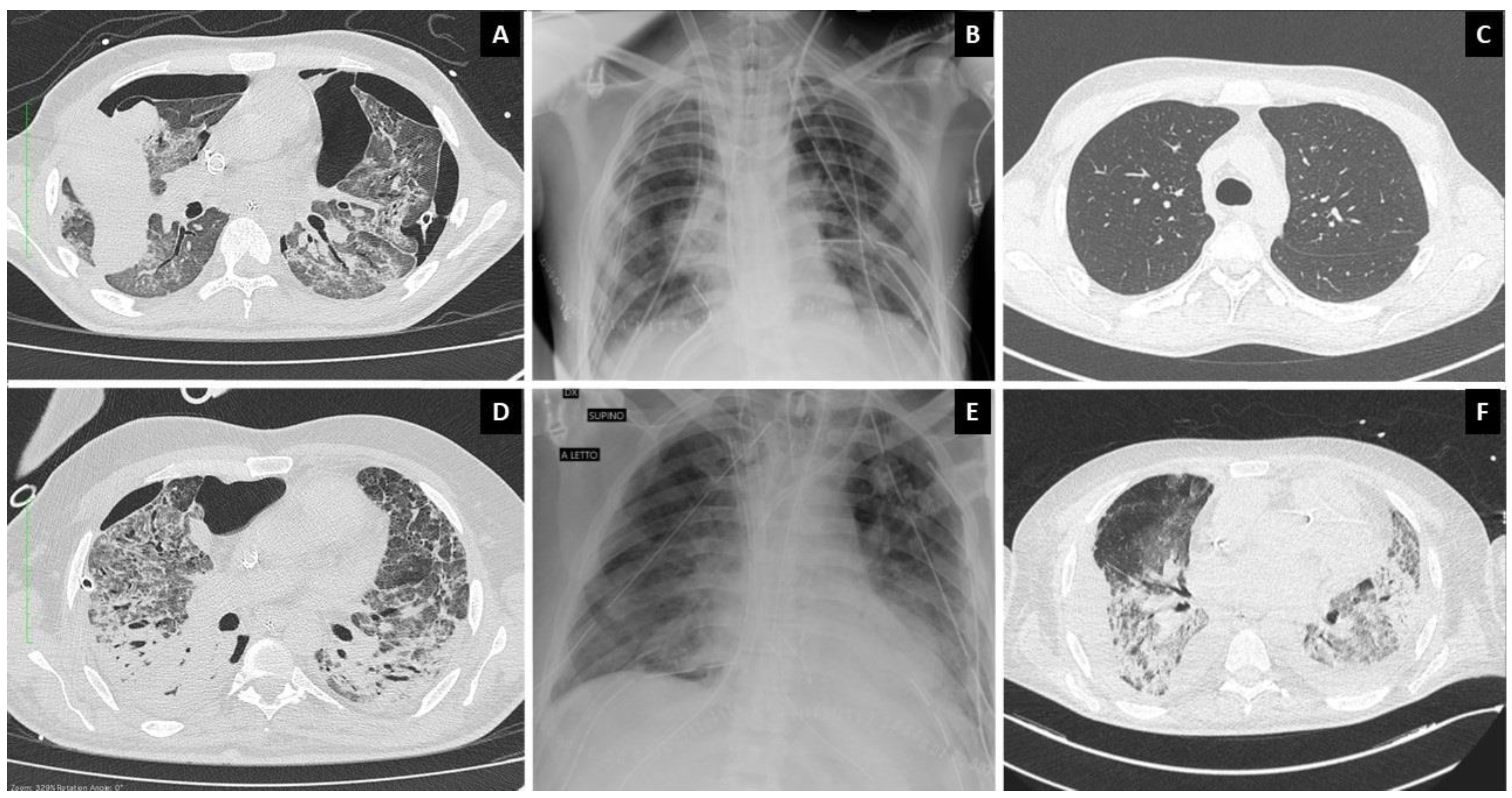
2. Presentation of Cases
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Chen, J.Y.; Qiao, K.; Liu, F.; Wu, B.; Xu, X.; Jiao, G.Q.; Lu, R.G.; Li, H.X.; Zhao, J.; Huang, J.; et al. Lung transplantation as therapeutic option in acute respiratory distress syndrome for coronavirus disease 2019-related pulmonary fibrosis. Chin. Med. J. 2020, 133, 1390–1396. [Google Scholar] [CrossRef] [PubMed]
- Bharat, A.; Machuca, T.N.; Querrey, M.; Kurihara, C.; Garza-Castillon, R., Jr.; Kim, S.; Manerikar, A.; Pelaez, A.; Pipkin, M.; Shahmohammadi, A.; et al. Early outcomes after lung transplantation for severe COVID-19: A series of the first consecutive cases from four countries. Lancet Respir. Med. 2021, 9, 487–497. [Google Scholar] [CrossRef]
- Lang, C.; Ritschl, V.; Augustin, F.; Lang, G.; Moser, B.; Taghavi, S.; Murakoezy, G.; Lambers, C.; Flick, H.; Koestenberger, M.; et al. Clinical relevance of lung transplantation for COVID-19 ARDS: A nationwide study. Eur. Respir. J. 2022, 17, 2102404. [Google Scholar] [CrossRef]
- Kurihara, C.; Manerikar, A.; Querrey, M.; Felicelli, C.; Yeldandi, A.; Garza-Castillon, R., Jr.; Lung, K.; Kim, S.; Ho, B.; Tomic, R.; et al. Clinical Characteristics and Outcomes of Patients With COVID-19-Associated Acute Respiratory Distress Syndrome Who Underwent Lung Transplant. JAMA 2022, 327, 652–661. [Google Scholar] [CrossRef] [PubMed]
- Cypel, M.; Keshavjee, S. When to consider lung transplantation for COVID-19. Lancet Respir. Med. 2020, 8, 944–946. [Google Scholar] [CrossRef]
- Rossi, V.; Tammaro, S.; Santambrogio, M.; Retucci, M.; Gallo, F.; Crotti, S.; Mantero, M.; Nosotti, M.; Privitera, E.; Palleschi, A. Physiotherapy approach after lung transplantation in a critically ill COVID-19 patient: A case report. Monaldi. Arch. Chest. Dis. 2021, 92. [Google Scholar] [CrossRef] [PubMed]
- Lang, C.; Jaksch, P.; Hoda, M.A.; Lang, G.; Staudinger, T.; Tschernko, E.; Zapletal, B.; Geleff, S.; Prosch, H.; Gawish, R.; et al. Lung transplantation for COVID-19-associated acute respiratory distress syndrome in a PCR-positive patient. Lancet Respir. Med. 2020, 8, 1057–1060. [Google Scholar] [CrossRef]
- Rogers, J.P.; Chesney, E.; Oliver, D.; Pollak, T.A.; McGuire, P.; Fusar-Poli, P.; Zandi, M.S.; Lewis, G.; David, A.S. Psychiatric and neuropsychiatric presentations associated with severe coronavirus infections: A systematic review and meta-analysis with comparison to the COVID-19 pandemic. Lancet Psychiatry 2020, 7, 611–627. [Google Scholar] [CrossRef]
- Helms, J.; Kremer, S.; Merdji, H.; Clere-Jehl, R.; Schenck, M.; Kummerlen, C.; Collange, O.; Boulay, C.; Fafi-Kremer, S.; Ohana, M.; et al. Neurologic Features in Severe SARS-CoV-2 Infection. N. Engl. J. Med. 2020, 382, 2268–2270. [Google Scholar] [CrossRef] [PubMed]
- Tiri, B.; Sensi, E.; Marsiliani, V.; Cantarini, M.; Priante, G.; Vernelli, C.; Martella, L.A.; Costantini, M.; Mariottini, A.; Andreani, P.; et al. Antimicrobial Stewardship Program, COVID-19, and Infection Control: Spread of Carbapenem-Resistant Klebsiella Pneumoniae Colonization in ICU COVID-19 Patients. What Did Not Work? J. Clin. Med. 2020, 9, 2744. [Google Scholar] [CrossRef] [PubMed]
- François, B.; Laterre, P.F.; Luyt, C.E.; Chastre, J. The challenge of ventilator-associated pneumonia diagnosis in COVID-19 patients. Crit. Care 2020, 24, 289. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Palleschi, A.; Crotti, S.; Scandroglio, A.M.; Lissoni, A.; Fominskiy, E.; Rosso, L.; Tosi, D.; Musso, V.; Blasi, F.; Gori, A.; et al. Lung Transplant for ARDS after COVID-19: Long-Term Outcomes and Considerations about Detrimental Issues. J. Clin. Med. 2022, 11, 4754. https://doi.org/10.3390/jcm11164754
Palleschi A, Crotti S, Scandroglio AM, Lissoni A, Fominskiy E, Rosso L, Tosi D, Musso V, Blasi F, Gori A, et al. Lung Transplant for ARDS after COVID-19: Long-Term Outcomes and Considerations about Detrimental Issues. Journal of Clinical Medicine. 2022; 11(16):4754. https://doi.org/10.3390/jcm11164754
Chicago/Turabian StylePalleschi, Alessandro, Stefania Crotti, Anna Mara Scandroglio, Alfredo Lissoni, Evgeny Fominskiy, Lorenzo Rosso, Davide Tosi, Valeria Musso, Francesco Blasi, Andrea Gori, and et al. 2022. "Lung Transplant for ARDS after COVID-19: Long-Term Outcomes and Considerations about Detrimental Issues" Journal of Clinical Medicine 11, no. 16: 4754. https://doi.org/10.3390/jcm11164754
APA StylePalleschi, A., Crotti, S., Scandroglio, A. M., Lissoni, A., Fominskiy, E., Rosso, L., Tosi, D., Musso, V., Blasi, F., Gori, A., & Nosotti, M. (2022). Lung Transplant for ARDS after COVID-19: Long-Term Outcomes and Considerations about Detrimental Issues. Journal of Clinical Medicine, 11(16), 4754. https://doi.org/10.3390/jcm11164754








