Albumin-to-Alkaline Phosphatase Ratio as a Prognostic Biomarker for Spinal Fusion in Lumbar Degenerative Diseases Patients Undergoing Lumbar Spinal Fusion
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Patient Characteristics
2.2. Albumin-to-Alkaline Phosphatase Ratio (AAPR) and Disc Degeneration Assessment
2.3. Statistical Analysis
3. Results
3.1. Patient Demographics and Outcomes
3.2. IDD Severity Classification and Association with AAPR
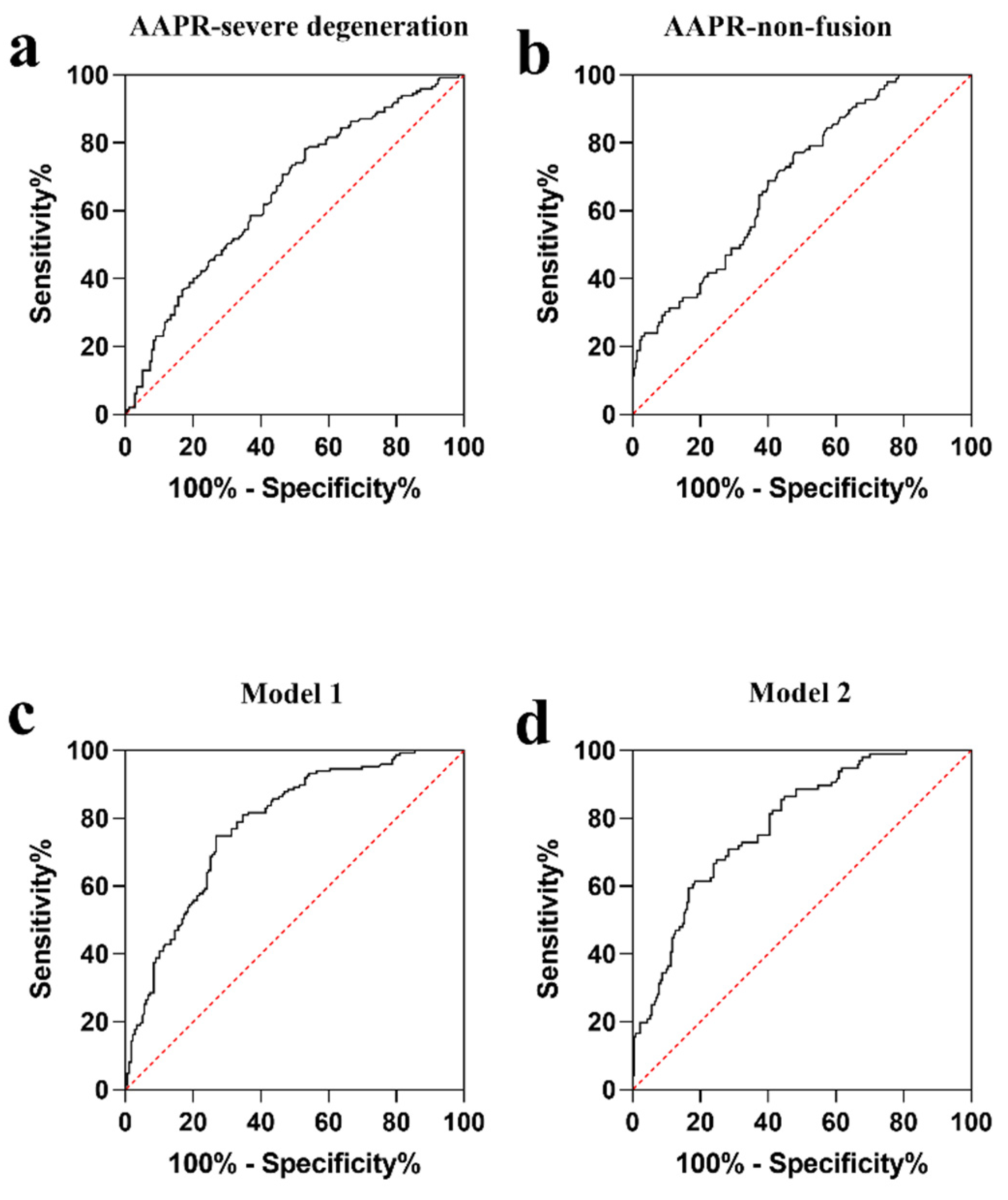
3.3. Univariable and Multivariable Analysis on Predictive Factors of Severe Disc Degeneration
3.4. Univariable and Multivariable Analysis on Risk Factors of Non-Fusion
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Luoma, K.; Riihimäki, H.; Luukkonen, R.; Raininko, R.; Viikari-Juntura, E.; Lamminen, A. Low Back Pain in Relation to Lumbar Disc Degeneration. Spine 2000, 25, 487–492. [Google Scholar] [CrossRef] [PubMed]
- Costi, J.J.; Stokes, I.; Gardner-Morse, M.; Iatridis, J. Frequency-Dependent Behavior of the Intervertebral Disc in Response to Each of Six Degree of Freedom Dynamic Loading. Spine 2008, 33, 1731–1738. [Google Scholar] [CrossRef] [PubMed]
- Suthar, P. MRI Evaluation of Lumbar Disc Degenerative Disease. J. Clin. Diagn. Res. 2015, 9, TC04–TC09. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.; Rui, Y.; Lu, J.; Wang, C. Cell and molecular biology of intervertebral disc degeneration: Current understanding and implications for potential therapeutic strategies. Cell Prolif. 2014, 47, 381–390. [Google Scholar] [CrossRef] [PubMed]
- Vergroesen, P.-P.; Kingma, I.; Emanuel, K.; Hoogendoorn, R.; Welting, T.; van Royen, B.; van Dieën, J.; Smit, T. Mechanics and biology in intervertebral disc degeneration: A vicious circle. Osteoarthr. Cartil. 2015, 23, 1057–1070. [Google Scholar] [CrossRef]
- Molinos, M.; Almeida, C.R.; Caldeira, J.; Cunha, C.; Gonçalves, R.M.; Barbosa, M.A. Inflammation in intervertebral disc degeneration and regeneration. J. R. Soc. Interface 2015, 12, 20150429. [Google Scholar] [CrossRef] [PubMed]
- Taniguchi, K.; Karin, M. NF-κB, inflammation, immunity and cancer: Coming of age. Nat. Rev. Immunol. 2018, 18, 309–324. [Google Scholar] [CrossRef] [PubMed]
- Eck, J.C.; Sharan, A.; Ghogawala, Z.; Resnick, D.K.; Watters, W.C.; Mummaneni, P.V.; Dailey, A.T.; Choudhri, T.F.; Groff, M.W.; Wang, J.C.; et al. Guideline update for the performance of fusion procedures for degenerative disease of the lumbar spine. Part 7: Lumbar fusion for intractable low-back pain without stenosis or spondylolisthesis. J. Neurosurg. Spine 2014, 21, 42–47. [Google Scholar] [CrossRef] [PubMed]
- Loi, F.; Córdova, L.A.; Pajarinen, J.; Lin, T.; Yao, Z.; Goodman, S.B. Inflammation, fracture and bone repair. Bone 2016, 86, 119–130. [Google Scholar] [CrossRef]
- Małkowski, P.; Rozga, J.; Piątek, T. Human albumin: Old, new, and emerging applications. Ann. Transplant. 2013, 18, 205–217. [Google Scholar] [CrossRef] [PubMed]
- Eckart, A.; Struja, T.; Kutz, A.; Baumgartner, A.; Baumgartner, T.; Zurfluh, S.; Neeser, O.; Huber, A.; Stanga, Z.; Mueller, B.; et al. Relationship of Nutritional Status, Inflammation, and Serum Albumin Levels during Acute Illness: A Prospective Study. Am. J. Med. 2020, 133, 713–722.e7. [Google Scholar] [CrossRef] [PubMed]
- Vimalraj, S. Alkaline phosphatase: Structure, expression and its function in bone mineralization. Gene 2020, 754, 144855. [Google Scholar] [CrossRef]
- Demer, L.L.; Tintut, Y. Inflammatory, Metabolic, and Genetic Mechanisms of Vascular Calcification. Arter. Thromb. Vasc. Biol. 2014, 34, 715–723. [Google Scholar] [CrossRef]
- Estaki, M.; DeCoffe, D.; Gibson, D.L. Interplay between intestinal alkaline phosphatase, diet, gut microbes and immunity. World J. Gastroenterol. 2014, 20, 15650–15656. [Google Scholar] [CrossRef]
- Bottini, A.; Berruti, A.; Brizzi, M.P.; Bersiga, A.; Generali, D.; Allevi, G.; Aguggini, S.; Bolsi, G.; Bonardi, S.; Bertoli, G.; et al. Pretreatment haemoglobin levels significantly predict the tumour response to primary chemotherapy in human breast cancer. Br. J. Cancer 2003, 89, 977–982. [Google Scholar] [CrossRef]
- Li, D.; Yu, H.; Li, W. Albumin-to-alkaline phosphatase ratio at diagnosis predicts survival in patients with metastatic non-small-cell lung cancer. OncoTargets Ther. 2019, 12, 5241–5249. [Google Scholar] [CrossRef]
- Nie, M.; Sun, P.; Chen, C.; Bi, X.; Wang, Y.; Yang, H.; Liu, P.; Li, Z.; Xia, Y.; Jiang, W. Albumin-to-Alkaline Phosphatase Ratio: A Novel Prognostic Index of Overall Survival in Cisplatin-based Chemotherapy-treated Patients with Metastatic Nasopharyngeal Carcinoma. J. Cancer 2017, 8, 809–815. [Google Scholar] [CrossRef]
- Fauran-Clavel, M.; Oustrin, J. Alkaline phosphatase and bone calcium parameters. Bone 1986, 7, 95–99. [Google Scholar] [CrossRef]
- Skaliczki, G.; Schandl, K.; Weszl, M.; Major, T.; Kovács, M.; Skaliczki, J.; Szendrői, M.; Dobó-Nagy, C.; Lacza, Z. Serum albumin enhances bone healing in a nonunion femoral defect model in rats: A computer tomography micromorphometry study. Int. Orthop. 2013, 37, 741–745. [Google Scholar] [CrossRef]
- Horváthy, D.B.; Schandl, K.; Schwarz, C.M.; Renner, K.; Hornyák, I.; Szabó, B.T.; Niculescu-Morzsa, E.; Nehrer, S.; Dobó-Nagy, C.; Doros, A.; et al. Serum albumin-coated bone allograft (BoneAlbumin) results in faster bone formation and mechanically stronger bone in aging rats. J. Tissue Eng. Regen. Med. 2019, 13, 416–422. [Google Scholar] [CrossRef]
- Khalooeifard, R.; Oraee-Yazdani, S.; Keikhaee, M.; Shariatpanahi, Z.V. Protein Supplement and Enhanced Recovery after Posterior Spine Fusion Surgery: A Randomized, Double-blind, Placebo-controlled Trial. Clin. Spine Surg. 2022, 35, E356–E362. [Google Scholar] [CrossRef] [PubMed]
- Inose, H.; Yamada, T.; Mulati, M.; Hirai, T.; Ushio, S.; Yoshii, T.; Kato, T.; Kawabata, S.; Okawa, A. Bone Turnover Markers as a New Predicting Factor for Nonunion After Spinal Fusion Surgery. Spine 2018, 43, E29–E34. [Google Scholar] [CrossRef] [PubMed]
- Siepe, C.J.; Stosch-Wiechert, K.; Heider, F.; Amnajtrakul, P.; Krenauer, A.; Hitzl, W.; Szeimies, U.; Stäbler, A.; Mayer, H.M. Anterior stand-alone fusion revisited: A prospective clinical, X-ray and CT investigation. Eur. Spine J. 2015, 24, 838–851. [Google Scholar] [CrossRef]
- Pfirrmann, C.; Metzdorf, A.; Zanetti, M.; Hodler, J.; Boos, N. Magnetic Resonance Classification of Lumbar Intervertebral Disc Degeneration. Spine 2001, 26, 1873–1878. [Google Scholar] [CrossRef] [PubMed]
- Farrugia, A. Albumin Usage in Clinical Medicine: Tradition or Therapeutic? Transfus. Med. Rev. 2010, 24, 53–63. [Google Scholar] [CrossRef]
- Don, B.R.; Kaysen, G. Poor Nutritional Status and Inflammation: Serum Albumin: Relationship to Inflammation and Nutrition. Semin. Dial. 2004, 17, 432–437. [Google Scholar] [CrossRef] [PubMed]
- Deveci, B.; Gazi, E. Relation Between Globulin, Fibrinogen, and Albumin with the Presence and Severity of Coronary Artery Disease. Angiology 2021, 72, 174–180. [Google Scholar] [CrossRef] [PubMed]
- Belcher, D.A.; Williams, A.T.; Palmer, A.F.; Cabrales, P. Polymerized albumin restores impaired hemodynamics in endotoxemia and polymicrobial sepsis. Sci. Rep. 2021, 11, 10834. [Google Scholar] [CrossRef]
- Galata, C.; Busse, L.; Birgin, E.; Weiß, C.; Hardt, J.; Reissfelder, C.; Otto, M. Role of Albumin as a Nutritional and Prognostic Marker in Elective Intestinal Surgery. Can. J. Gastroenterol. Hepatol. 2020, 2020, 7028216. [Google Scholar] [CrossRef]
- Kawashima, A.; Yamamoto, Y.; Sato, M.; Nakata, W.; Kakuta, Y.; Ishizuya, Y.; Yamaguchi, Y.; Yamamoto, A.; Yoshida, T.; Takayama, H.; et al. FAN score comprising fibrosis-4 index, albumin–bilirubin score and neutrophil–lymphocyte ratio is a prognostic marker of urothelial carcinoma patients treated with pembrolizumab. Sci. Rep. 2021, 11, 21199. [Google Scholar] [CrossRef]
- Singh, S.B.; Lin, H.C. Role of Intestinal Alkaline Phosphatase in Innate Immunity. Biomolecules 2021, 11, 1784. [Google Scholar] [CrossRef] [PubMed]
- Vercalsteren, E.; Vranckx, C.; Lijnen, H.R.; Hemmeryckx, B.; Scroyen, I. Adiposity and metabolic health in mice deficient in intestinal alkaline phosphatase. Adipocyte 2018, 7, 149–155. [Google Scholar] [CrossRef]
- Gutman, A.B. Serum alkaline phosphatase activity in diseases of the skeletal and hepatobiliary systems: A consideration of the current status. Am. J. Med. 1959, 27, 875–901. [Google Scholar] [CrossRef]
- Peach, H.; Compston, J.E.; Vedi, S.; Horton, L.W. Value of plasma calcium, phosphate, and alkaline phosphatase measurements in the diagnosis of histological osteomalacia. J. Clin. Pathol. 1982, 35, 625–630. [Google Scholar] [CrossRef] [PubMed]
- Chen, Z.-H.; Zhang, X.-P.; Cai, X.-R.; Xie, S.-D.; Liu, M.-M.; Lin, J.-X.; Ma, X.-K.; Chen, J.; Lin, Q.; Dong, M.; et al. The Predictive Value of Albumin-to-Alkaline Phosphatase Ratio for Overall Survival of Hepatocellular Carcinoma Patients Treated with Trans-Catheter Arterial Chemoembolization Therapy. J. Cancer 2018, 9, 3467–3478. [Google Scholar] [CrossRef] [PubMed]
- Li, H.; Li, J.; Wang, J.; Liu, H.; Cai, B.; Wang, G.; Wu, H. Assessment of Liver Function for Evaluation of Long-Term Outcomes of Intrahepatic Cholangiocarcinoma: A Multi-Institutional Analysis of 620 Patients. Front. Oncol. 2020, 10, 525. [Google Scholar] [CrossRef] [PubMed]
- Acikgoz, Y.; Bal, O.; Dogan, M. Albumin-to-Alkaline Phosphatase Ratio: Does It Predict Survival in Grade 1 and Grade 2 Neuroendocrine Tumors? Pancreas 2021, 50, 111–117. [Google Scholar] [CrossRef]
- Li, J.; Zuo, M.; Zhou, X.; Xiang, Y.; Zhang, S.; Feng, W.; Liu, Y. Prognostic Significance of Preoperative Albumin to Alkaline Phosphatase Ratio in Patients with Glioblastoma. J. Cancer 2021, 12, 5950–5959. [Google Scholar] [CrossRef]
- Chen, J.; Shao, Y.; Sasore, T.; Moiseyev, G.; Zhou, K.; Ma, X.; Du, Y.; Ma, J.-X. Interphotoreceptor Retinol-Binding Protein Ameliorates Diabetes-Induced Retinal Dysfunction and Neurodegeneration through Rhodopsin. Diabetes 2021, 70, 788–799. [Google Scholar] [CrossRef]
- Wang, J.; Chen, H.; Liu, Y.; Zhou, W.; Sun, R.; Xia, M. Retinol binding protein 4 induces mitochondrial dysfunction and vascular oxidative damage. Atherosclerosis 2015, 240, 335–344. [Google Scholar] [CrossRef]
- Rutges, J.; Duit, R.; Kummer, J.; Oner, F.; van Rijen, M.; Verbout, A.; Castelein, R.; Dhert, W.; Creemers, L. Hypertrophic differentiation and calcification during intervertebral disc degeneration. Osteoarthr. Cartil. 2010, 18, 1487–1495. [Google Scholar] [CrossRef] [PubMed]
- Hawellek, T.; Hubert, J.; Hischke, S.; Rolvien, T.; Krause, M.; Püschel, K.; Rüther, W.; Niemeier, A. Microcalcification of lumbar spine intervertebral discs and facet joints is associated with cartilage degeneration, but differs in prevalence and its relation to age. J. Orthop. Res. 2017, 35, 2692–2699. [Google Scholar] [CrossRef]
- Shih, T.-Y.; Wu, Y.-C.; Tseng, S.-C.; Chen, K.-H.; Pan, C.-C.; Lee, C.-H. Correlation between Preoperative Serum Levels of Calcium, Phosphate, and Intact Parathyroid Hormone and Radiological Outcomes in Spinal Interbody Fusion among End-Stage Renal Disease Patients. J. Clin. Med. 2021, 10, 5447. [Google Scholar] [CrossRef] [PubMed]
- Sheng, G.; Peng, N.; Hu, C.; Zhong, L.; Zhong, M.; Zou, Y. The albumin-to-alkaline phosphatase ratio as an independent predictor of future non-alcoholic fatty liver disease in a 5-year longitudinal cohort study of a non-obese Chinese population. Lipids Health Dis. 2021, 20, 50. [Google Scholar] [CrossRef] [PubMed]
| All | Low Score Group | High Score Group | p-Value | |
|---|---|---|---|---|
| (Accumulative Grade ≤ 18) | (Accumulative Grade > 18) | |||
| Subjects, n (%) | 326 | 179 | 147 | |
| Age (year) | 63.48 ± 13.38 | 60.49 ± 14.93 | 67.11 ± 10.13 | <0.001 |
| Gender | 0.562 | |||
| Male, n (%) | 141 (43.3) | 80 (44.7) | 61 (41.5) | |
| Female, n (%) | 185 (56.7) | 99 (55.3) | 86 (58.5) | |
| BMI (kg/m2) | 24.80 ± 3.54 | 24.96 ± 3.49 | 24.60 ± 3.60 | 0.371 |
| Smoking (y) | 42 (12.9) | 22 (12.3) | 20 (13.6) | 0.724 |
| Alcohol abuse (y) | 27 (8.3) | 11 (6.1) | 16 (10.9) | 0.122 |
| Hypertension (y) | 155 (47.5) | 76 (42.5) | 79 (53.7) | 0.042 |
| DM (y) | 57 (17.5) | 30 (16.8) | 27 (18.4) | 0.704 |
| CHD (y) | 40 (12.3) | 24 (13.4) | 16 (10.9) | 0.490 |
| Osteoporosis (y) | 115 (35.3) | 53 (29.6) | 62 (42.2) | 0.018 |
| Calcification (y) | 164 (50.3) | 60 (33.5) | 104 (70.7) | <0.001 |
| ALB (g/L) | 42.49 ± 3.29 | 42.56 ± 3.19 | 42.41 ± 3.41 | 0.923 |
| ALP (U/L) | 74.18 ± 27.27 | 68.65 ± 24.02 | 80.90 ± 29.47 | <0.001 |
| AAPR | 0.64 ± 0.22 | 0.69 ± 0.24 | 0.58 ± 0.17 | <0.001 |
| Calcium (mmol/L) | 2.26 ± 0.10 | 2.25 ± 0.09 | 2.27 ± 0.10 | 0.092 |
| Phosphorus (mmol/L) | 1.14 ± 0.17 | 1.15 ± 0.16 | 1.14 ± 0.17 | 0.505 |
| FBG (mmol/L) | 5.54 ± 1.47 | 5.45 ± 1.36 | 5.65 ± 1.60 | 0.394 |
| BUN (mmol/L) | 6.04 ± 1.77 | 6.05 ± 1.73 | 6.02 ± 1.82 | 0.547 |
| Scr (μmol/L) | 72.33 ± 23.22 | 72.09 ± 21.65 | 72.62 ± 25.06 | 0.779 |
| UA (μmol/L) | 320.44 ± 82.57 | 323.42 ± 80.03 | 316.82 ± 85.69 | 0.597 |
| ALT (U/L) | 19.51 ± 14.34 | 20.12 ± 16.06 | 18.77 ± 11.92 | 0.549 |
| AST (U/L) | 19.12 ± 8.64 | 18.75 ± 9.80 | 19.56 ± 6.99 | 0.048 |
| RBP (mg/L) | 41.26 ± 9.54 | 42.83 ± 9.49 | 39.35 ± 9.27 | <0.001 |
| Fusion (y) | 230 (70.6) | 140 (78.2) | 90 (61.2) | 0.001 |
| VAS | 3.91 ± 1.84 | 3.73 ± 1.84 | 4.13 ± 1.84 | 0.067 |
| Hospital stay (day) | 12.21 ± 4.39 | 12.20 ± 4.36 | 12.21 ± 4.45 | 0.854 |
| CT value (HU) | 131.26 ± 49.20 | 140.51 ± 52.51 | 120.01 ± 42.35 | <0.001 |
| 1 | 2 | 3 | 4 | 5 | |
|---|---|---|---|---|---|
| All (n = 326) | |||||
| L1/2 | 0 | 136 (41.7) | 106 (32.5) | 50 (15.3) | 34 (10.4) |
| L2/3 | 0 | 79 (24.2) | 117 (35.9) | 78 (23.9) | 52 (16.0) |
| L3/4 | 1 (0.3) | 49 (15.0) | 106 (32.5) | 105 (32.2) | 65 (19.9) |
| L4/5 | 0 | 24 (7.4) | 82 (25.2) | 124 (38.0) | 96 (29.4) |
| L5/S1 | 0 | 27 (8.3) | 53 (16.3) | 103 (31.6) | 143 (43.9) |
| Low score group (n = 179) | |||||
| L1/2 | 0 | 114 (63.7) | 47 (26.3) | 14 (7.8) | 4 (2.2) |
| L2/3 | 0 | 77 (43.0) | 81 (45.3) | 19 (10.6) | 2 (1.1) |
| L3/4 | 1 (0.6) | 49 (27.4) | 90 (50.3) | 37 (20.7) | 2 (1.1) |
| L4/5 | 0 | 24 (13.4) | 64 (35.8) | 74 (41.3) | 17 (9.5) |
| L5/S1 | 0 | 27 (15.1) | 42 (23.5) | 65 (36.3) | 45 (25.1) |
| High score group (n = 147) | |||||
| L1/2 | 0 | 22 (15.0) | 59 (40.1) | 36 (24.5) | 30 (20.4) |
| L2/3 | 0 | 2 (1.4) | 36 (24.5) | 59 (40.1) | 50 (34.0) |
| L3/4 | 0 | 0 | 16 (10.9) | 68 (46.3) | 63 (42.9) |
| L4/5 | 0 | 0 | 18 (12.2) | 50 (34.0) | 79 (53.7) |
| L5/S1 | 0 | 0 | 11 (7.5) | 38 (25.9) | 98 (66.7) |
| AAPR | p | ||
|---|---|---|---|
| L1/2 | Pfirrmann grade < 4 | 0.65 ± 0.21 | 0.003 |
| Pfirrmann grade ≥ 4 | 0.59 ± 0.22 | ||
| L2/3 | Pfirrmann grade < 4 | 0.68 ± 0.23 | <0.001 |
| Pfirrmann grade ≥ 4 | 0.58 ± 0.18 | ||
| L3/4 | Pfirrmann grade < 4 | 0.70 ± 0.25 | <0.001 |
| Pfirrmann grade ≥ 4 | 0.58 ± 0.17 | ||
| L4/5 | Pfirrmann grade < 4 | 0.68 ± 0.19 | <0.001 |
| Pfirrmann grade ≥ 4 | 0.62 ± 0.23 | ||
| L5/S1 | Pfirrmann grade < 4 | 0.67 ± 0.23 | 0.181 |
| Pfirrmann grade ≥ 4 | 0.63 ± 0.21 |
| r | p | |
|---|---|---|
| Age | −0.110 | 0.046 |
| Gender | 0.070 | 0.210 |
| BMI | 0.028 | 0.611 |
| Smoking | 0.026 | 0.640 |
| Alcohol abuse | −0.070 | 0.209 |
| Hypertension | −0.045 | 0.417 |
| DM | −0.014 | 0.796 |
| CHD | −0.058 | 0.295 |
| Osteoporosis | −0.167 | 0.002 |
| Calcification | −0.422 | <0.001 |
| Calcium | 0.025 | 0.656 |
| phosphorus | 0.080 | 0.150 |
| FBG | −0.034 | 0.546 |
| BUN | 0.046 | 0.408 |
| Scr | 0.179 | 0.001 |
| UA | 0.108 | 0.052 |
| ALT | −0.019 | 0.728 |
| AST | −0.064 | 0.249 |
| RBP | 0.036 | 0.521 |
| Non-fusion | −0.132 | 0.017 |
| VAS | −0.132 | 0.017 |
| Hospital stay, day | 0.087 | 0.118 |
| CT value | 0.198 | <0.001 |
| Accumulative grade | −0.379 | <0.001 |
| Variables | Univariate | Multivariate | ||
|---|---|---|---|---|
| OR (95% CI) | p | OR (95% CI) | p | |
| Age (year) | 1.042 (1.023–1.062) | <0.001 | 1.027 (0.999–1.055) | 0.062 |
| Gender (male) | 0.878 (0.565–1.364) | 0.562 | 0.953 (0.478–1.903) | 0.892 |
| BMI | 0.971 (0.913–1.034) | 0.358 | 0.979 (0.903–1.061) | 0.604 |
| Smoking | 1.124 (0.587–2.151) | 0.724 | 1.492 (0.623–3.574) | 0.369 |
| Alcohol abuse | 1.865 (0.837–4.155) | 0.127 | 2.037 (0.735–5.646) | 0.172 |
| Hypertension | 1.574 (1.015–2.443) | 0.043 | 1.179 (0.649–2.141) | 0.588 |
| DM | 1.117 (0.630–1.982) | 0.704 | 0.935 (0.397–2.201) | 0.877 |
| CHD | 0.789 (0.402–1.548) | 0.490 | 0.360 (0.155–0.834) | 0.017 |
| Osteoporosis | 1.734 (1.096–2.742) | 0.019 | 1.045 (0.581–1.880) | 0.883 |
| Calcification | 4.797 (2.993–7.689) | <0.001 | 3.215 (1.848–5.594) | <0.001 |
| AAPR | 0.055 (0.015–0.194) | <0.001 | 0.114 (0.027–0.482) | 0.003 |
| Calcium | 6.241 (0.649–59.996) | 0.113 | 14.486 (0.796–263.562) | 0.071 |
| phosphorus | 0.618 (0.166–2.308) | 0.474 | 1.456 (0.296–7.161) | 0.644 |
| FBG | 1.096 (0.944–1.274) | 0.229 | 1.080 (0.868–1.344) | 0.489 |
| BUN | 0.988 (0.873–1.118) | 0.850 | 0.975 (0.822–1.157) | 0.773 |
| Scr | 1.001 (0.992–1.010) | 0.839 | 1.004 (0.988–1.021) | 0.590 |
| UA | 0.999 (0.996–1.002) | 0.472 | 1.001 (0.997–1.004) | 0.755 |
| ALT | 0.993 (0.977–1.009) | 0.405 | 0.996 (0.961–1.032) | 0.832 |
| AST | 1.011 (0.985–1.038) | 0.408 | 1.003 (0.947–1.061) | 0.928 |
| RBP | 0.960 (0.937–0.984) | 0.001 | 0.948 (0.919–0.977) | 0.001 |
| Variable | Cases | Model 1 (Degeneration Model) | Model 2 (Non-Fusion Model) | ||
|---|---|---|---|---|---|
| OR [95% CI] | p for Trend | OR [95% CI] | p for Trend | ||
| AAPR (Median [Range]) | |||||
| Q1 (0.42 [≤0.49]) | 82 | Reference | Reference | ||
| Q2 (0.56 [0.49–0.61]) | 81 | 0.632 [0.306–1.306] | 0.653 [0.320–1.334] | ||
| Q3 (0.67 [0.61–0.75]) | 82 | 0.731 [0.342–1.563] | 0.400 [0.184–0.873] | ||
| Q4 (0.85 [>0.75]) | 81 | 0.316 [0.139–0.719] | 0.010 | 0.103 [0.038–0.277] | <0.001 |
| Variables | Univariate | Multivariate | ||
|---|---|---|---|---|
| OR (95% CI) | p | OR (95% CI) | p | |
| Age (year) | 0.995 (0.977–1.013) | 0.569 | 0.987 (0.960–1.014) | 0.345 |
| Gender (male) | 0.630 (0.385–1.031) | 0.066 | 0.570 (0.261–1.247) | 0.159 |
| BMI | 0.973 (0.909–1.042) | 0.432 | 0.959 (0.880–1.046) | 0.345 |
| Smoking | 1.086 (0.538–2.191) | 0.819 | 1.915 (0.743–4.936) | 0.179 |
| Alcohol abuse | 0.826 (0.337–2.023) | 0.675 | 0.808 (0.262–2.489) | 0.710 |
| Hypertension | 0.855 (0.530–1.379) | 0.520 | 1.101 (0.582–2.081) | 0.767 |
| DM | 0.742 (0.385–1.432) | 0.374 | 0.666 (0.237–1.873) | 0.441 |
| CHD | 0.470 (0.200–1.102) | 0.082 | 0.357 (0.128–0.998) | 0.049 |
| Osteoporosis | 1.222 (0.746–2.002) | 0.426 | 1.129 (0.591–2.156) | 0.713 |
| Calcification | 1.581 (0.977–2.559) | 0.062 | 0.834 (0.439–1.586) | 0.580 |
| AAPR | 0.009 (0.002–0.047) | <0.001 | 0.003 (0.0003–0.022) | <0.001 |
| Calcium | 1.616 (0.144–18.189) | 0.697 | 0.397 (0.017–9.500) | 0.569 |
| phosphorus | 9.892 (2.270–43.106) | 0.002 | 16.677 (2.794–99.552) | 0.002 |
| FBG | 1.024 (0.873–1.201) | 0.770 | 1.104 (0.868–1.405) | 0.418 |
| BUN | 0.985 (0.859–1.128) | 0.823 | 1.007 (0.837–1.212) | 0.938 |
| Scr | 0.988 (0.976–1.001) | 0.062 | 0.996 (0.976–1.016) | 0.673 |
| UA | 1.001 (0.998–1.004) | 0.531 | 1.005 (1.001–1.010) | 0.014 |
| ALT | 1.002 (0.986–1.018) | 0.808 | 0.988 (0.952–1.025) | 0.510 |
| AST | 1.014 (0.987–1.041) | 0.318 | 1.016 (0.959–1.076) | 0.595 |
| RBP | 0.988 (0.963–1.014) | 0.356 | 0.986 (0.956–1.016) | 0.344 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Guo, Y.; Zhao, H.; Xu, H.; Gu, H.; Cao, Y.; Li, K.; Li, T.; Hu, T.; Wang, S.; Zhao, W.; et al. Albumin-to-Alkaline Phosphatase Ratio as a Prognostic Biomarker for Spinal Fusion in Lumbar Degenerative Diseases Patients Undergoing Lumbar Spinal Fusion. J. Clin. Med. 2022, 11, 4719. https://doi.org/10.3390/jcm11164719
Guo Y, Zhao H, Xu H, Gu H, Cao Y, Li K, Li T, Hu T, Wang S, Zhao W, et al. Albumin-to-Alkaline Phosphatase Ratio as a Prognostic Biomarker for Spinal Fusion in Lumbar Degenerative Diseases Patients Undergoing Lumbar Spinal Fusion. Journal of Clinical Medicine. 2022; 11(16):4719. https://doi.org/10.3390/jcm11164719
Chicago/Turabian StyleGuo, Youfeng, Haihong Zhao, Haowei Xu, Huida Gu, Yang Cao, Kai Li, Ting Li, Tao Hu, Shanjin Wang, Weidong Zhao, and et al. 2022. "Albumin-to-Alkaline Phosphatase Ratio as a Prognostic Biomarker for Spinal Fusion in Lumbar Degenerative Diseases Patients Undergoing Lumbar Spinal Fusion" Journal of Clinical Medicine 11, no. 16: 4719. https://doi.org/10.3390/jcm11164719
APA StyleGuo, Y., Zhao, H., Xu, H., Gu, H., Cao, Y., Li, K., Li, T., Hu, T., Wang, S., Zhao, W., & Wu, D. (2022). Albumin-to-Alkaline Phosphatase Ratio as a Prognostic Biomarker for Spinal Fusion in Lumbar Degenerative Diseases Patients Undergoing Lumbar Spinal Fusion. Journal of Clinical Medicine, 11(16), 4719. https://doi.org/10.3390/jcm11164719








