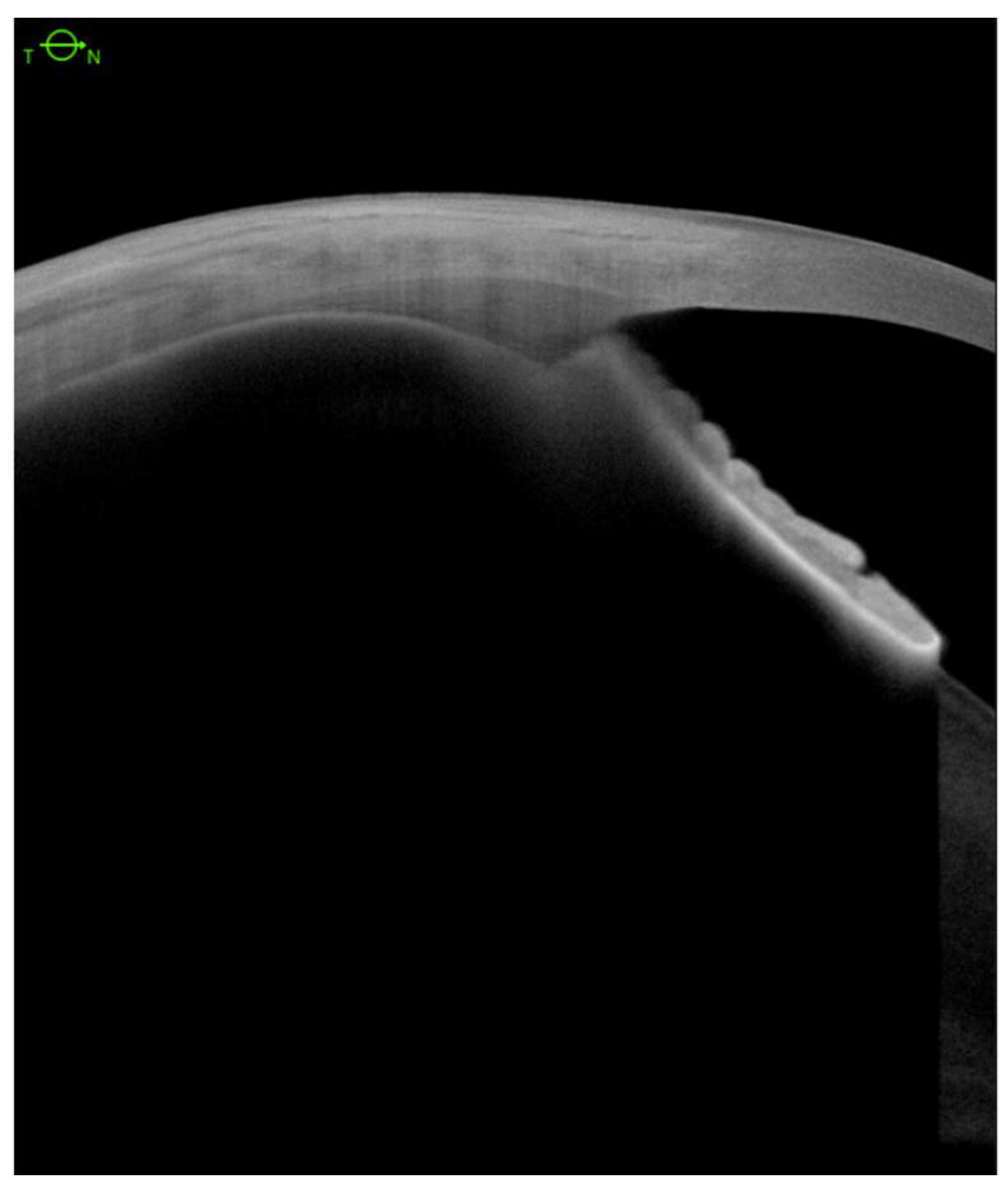
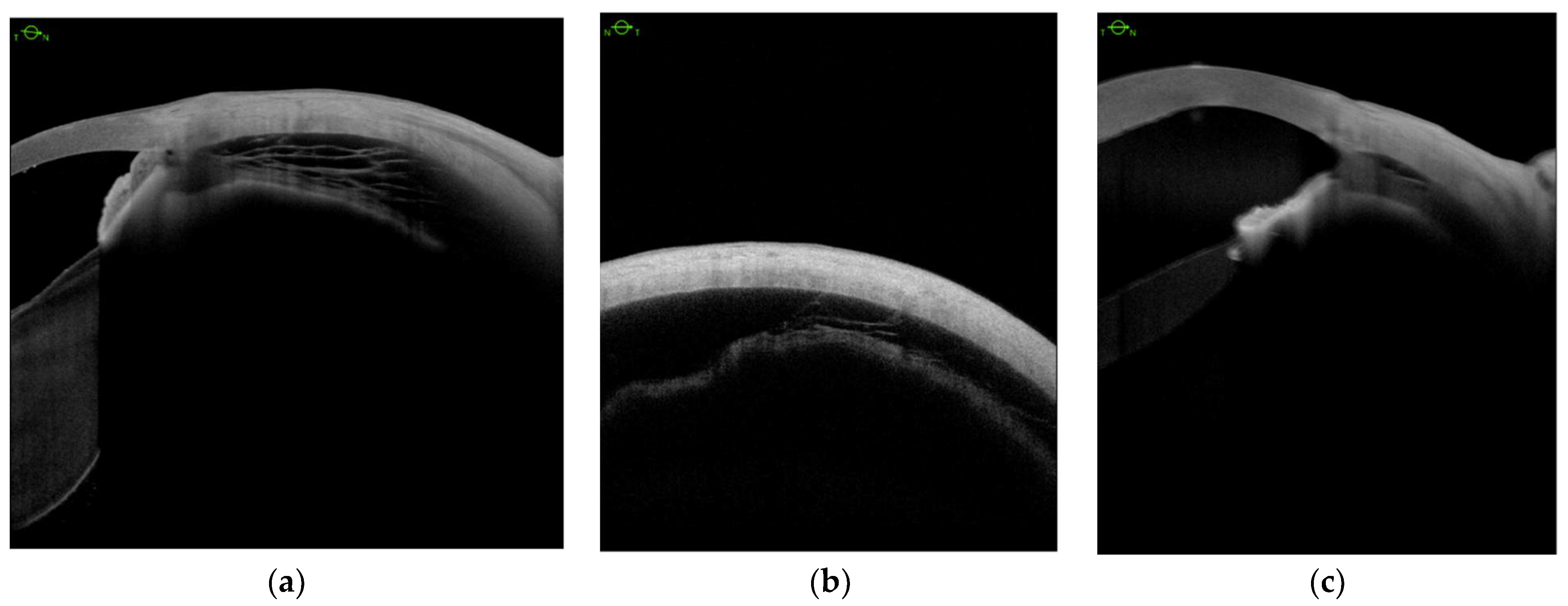
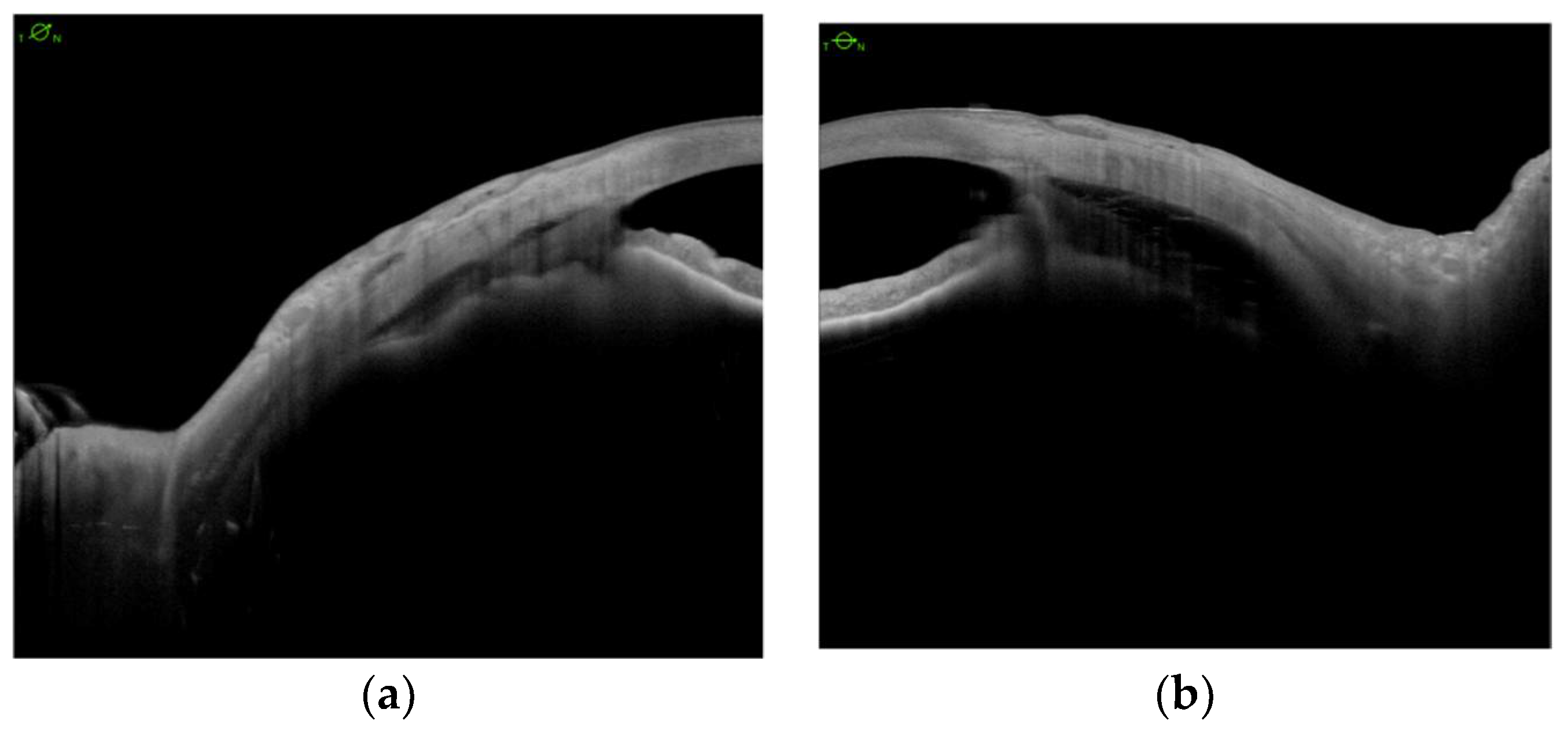
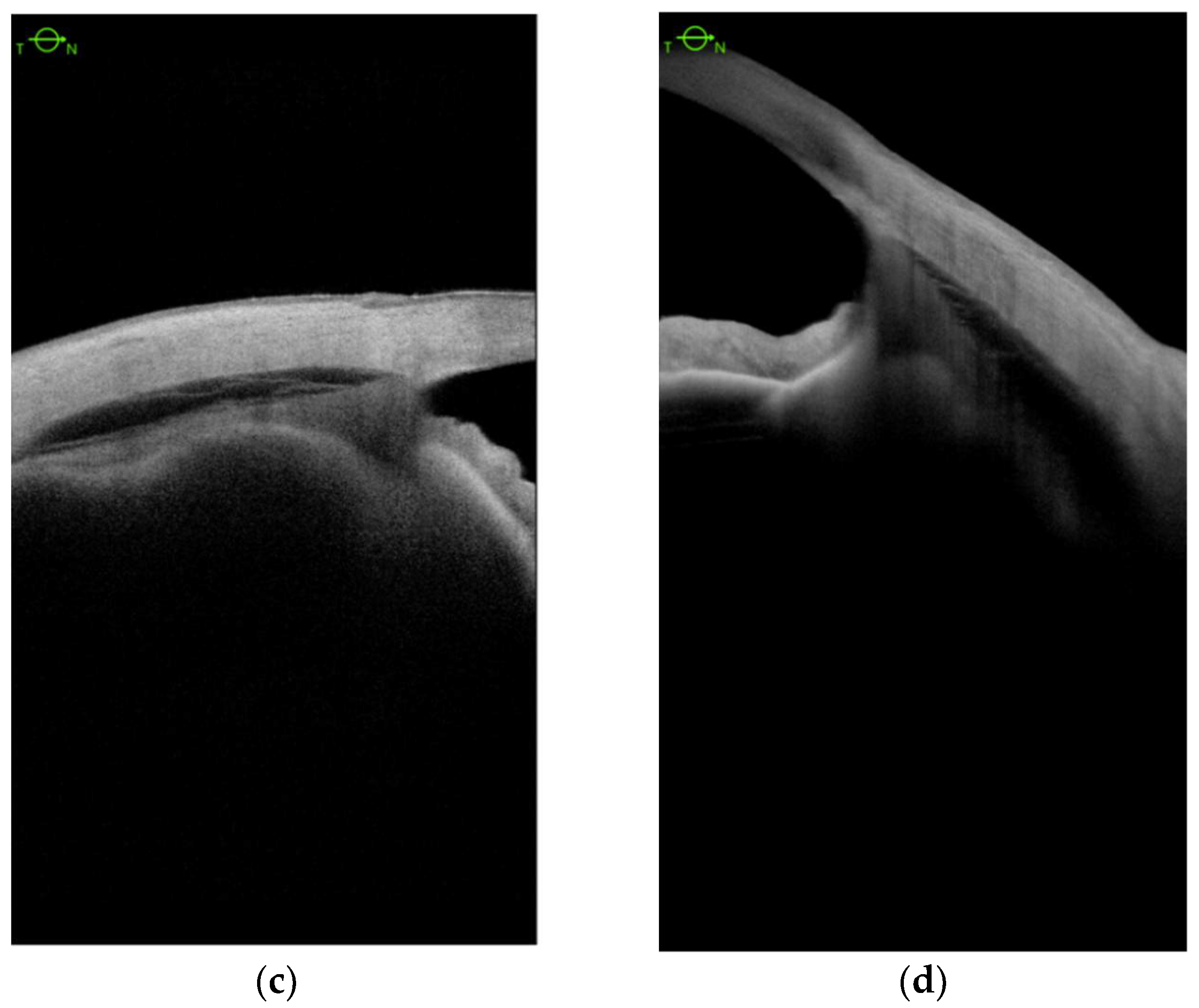
Encircling Scleral Buckling Surgery for Severe Hypotony with Ciliary Body Detachment on Anterior Segment Swept-Source Optical Coherence Tomography: A Case Series
Abstract
:1. Introduction
2. Materials and Methods
360° Scleral Buckling Surgery
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ursea, R.; Silverman, R.H. Anterior-segment imaging for assessment of glaucoma. Expert Rev. Ophthalmol. 2010, 5, 59–74. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Asam, J.S.; Polzer, M.; Tafreshi, A.; Hirnschall, N.; Findl, O. Anterior segment OCT. In High Resolution Imaging in Microscopy and Ophthalmology: New Frontiers in Biomedical Optics; Bille, J.F., Ed.; Springer: Cham, Switzerland, 2019; pp. 154–196. [Google Scholar]
- Krohn, J. Cryotherapy in the treatment of cyclodialysis cleft induced hypotony. Acta Ophthalmol. Scand. 1997, 75, 96–98. [Google Scholar] [CrossRef] [PubMed]
- Li, H.; Cai, J.; Li, X. Continuous ab interno repairing of traumatic cyclodialysis cleft using a 30-gauge needle in severe ocular trauma: A clinical observation. BMC Ophthalmol. 2019, 19, 266. [Google Scholar] [CrossRef] [PubMed]
- Ioannidis, A.S.; Bunce, C.; Barton, K. The evaluation and surgical management of cyclodialysis clefts that have failed to respond to conservative management. Br. J. Ophthalmol. 2014, 98, 544–549. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Selvan, H.; Gupta, V.; Gupta, S. Cyclodialysis: An updated approach to surgical strategies. Acta Ophthalmol. 2019, 97, 744–751. [Google Scholar] [CrossRef] [PubMed]
- Sood, G.; Rajendran, V.; George, R.; Sharma, T.; Raman, R. Comparison of encirclage and cryotherapy with argon laser in the management of traumatic cyclodialysis cleft. Int. J. Ophthalmol. 2019, 12, 165–168. [Google Scholar] [PubMed]
- Burés-Jelstrup, A.; Navarro, R.; Mateo, C.; Adan, A.; Corcóstegui, B. Detection of ciliary body detachment with anterior segment optical coherence tomography. Acta Ophthalmol. 2008, 86, 810–811. [Google Scholar] [CrossRef] [PubMed]
- González-Martín-Moro, J.; Contreras-Martín, I.; Muñoz-Negrete, F.J.; Gómez-Sanz, F.; Zarallo-Gallardo, J. Cyclodialysis: An update. Int. Ophthalmol. 2017, 37, 441–457. [Google Scholar] [CrossRef] [PubMed]
- Lávaque, E.B.; Iros, M.; Real, J.P.; Zambrano, A. Encircling scleral buckling for traumatic severe hypotony. Ophthalmic Surg. Lasers Imaging Retin. 2019, 51, 58–63. [Google Scholar] [CrossRef] [PubMed]
- Xu, W.-W.; Huang, Y.-F.; Wang, L.-Q.; Zhang, M.-N. Cyclopexy versus vitrectomy combined with intraocular tamponade for treatment of cyclodialysis. Int. J. Ophthalmol. 2013, 6, 187–192. [Google Scholar] [PubMed]
- Murta, F.; Mitne, S.; Allemann, N.; Paranhos Junior, A. Direct cyclopexy surgery for post-traumatic cyclodialysis with persistent hypotony: Ultrasound biomicroscopic evaluation. Arq. Bras. Oftalmol. 2014, 77, 50–53. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mandava, N.; Kahook, M.Y.; Mackenzie, D.L.; Olson, J.L. Anterior scleral buckling procedure for cyclodialysis cleft with chronic hypotony. Ophthalmic Surg. Lasers Imaging 2006, 37, 151–153. [Google Scholar] [CrossRef] [PubMed]
- Portney, G.L.; Purcell, T.W. Surgical repair of cyclodialysis induced hypotony. Ophthalmic Surg. 1974, 5, 30–32. [Google Scholar] [PubMed]
- Inukai, A.; Tanaka, S.; Hirose, A.; Tomimitsu, S.; Mochizuki, M. Three cases of hypotonic maculopathy due to blunt trauma, treated by 360-degree scleral buckling. Nippon Ganka Gakkai Zasshi 2003, 107, 337–342. [Google Scholar] [CrossRef] [PubMed]
- Elner, S.G.; Elner, V.M.; Díaz-Rohena, R.; Freeman, H.M.; Tolentino, F.I.; Albert, D.M. Anterior proliferative vitreoretinopathy. Clinicopathologic, light microscopic, and ultrastructural findings. Ophthalmology 1988, 95, 1349–1357. [Google Scholar] [CrossRef]
- Agrawal, P.; Shah, P. Long-term outcomes following the surgical repair of traumatic cyclodialysis clefts. Eye 2013, 27, 1347–1352. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Malandrini, A.; Balestrazzi, A.; Martone, G.; Tosi, G.M.; Caporossi, A. Diagnosis and management of traumatic cyclodialysis cleft. J. Cataract Refract. Surg. 2008, 34, 1213–12161. [Google Scholar] [CrossRef] [PubMed]
| Patient No. | Sex Age | BCVA before the Primary Surgery (Snellen, logMAR) | Final BCVA, 12 Months Post-Op. (Snellen, logMAR) | Primary Pathology and Previous Surgical Procedures | IOP Baseline | IOP Final, 12 Months Post-Op. | CB Baseline | CB Final, 12 Months Post-Op. |
|---|---|---|---|---|---|---|---|---|
| 1 | M 67 | HM (2.3 logMAR) | 0.01 (2.0 logMAR) | Globe injury with traumatic retinal detachment: 1. phacoppV+silicone oil 2. reppV+silicone oil exchange 3. 360° scleral buckling | 6 | 8 | CB detached in 3 quadrants | CB detached in 3 quadrants |
| 2 | F 65 | 0.05 (1.30 logMAR) | 0.05 (1.30 logMAR) | Retinal detachment with subretinal hemorrhage, VH: 1. plombage 2. phacoppV+gas 3. ppV+silicone oil 4. 360° scleral buckling | 4 | 8 | CB detached in 4 quadrants | CB detached in 4 quadrants |
| 3 | F 48 | HM (2.3 logMAR) | 0.03 (1.52 logMAR) | Retinal detachment: 1. phacoppV (BIL)+gas 2. 360° scleral buckling 3. ppV+silicone oil + IOL reposition 4.ppV+silicone oil removal | 6 | 14 | CB detached in 1 quadrant | CB detahced in 1 quadrant |
| 4 | F 66 | 0.1 (1.0 logMAR) | 0.25 (0.60 logMAR) | Retinal detachment: 1. phacoppV+silicone oil 2. ppV+silicone oil removal 3. ppV+silicone oil 4.360° scleral buckling +silicone oil removal | 5 | 14 | CB detached in 3 quadrants | CB detached in 3 quadrants |
| 5 | F 82 | HM (2.3 logMAR) | HM (2.3 logMAR) | Retinal detachment: 1.ppV+gas 2.ppV+silicone oil 3.ppV+silicone oil removal 4.ppV+silicone oil 5.360° scleral buckling | 4 | 6 | CB detached in 4 quadrants | CB detached in 4 quadrants |
| 6 | F 66 | HM (2.3 logMAR) | 0.05 (1.30 logMAR) | Retinal detachment 1.ppV+gas 2.360° scleral buckling | 4 | 11 | CB detached in 4 quadrants | CB detached in 4 quadrants |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cisiecki, S.; Bonińska, K.; Bednarski, M. Encircling Scleral Buckling Surgery for Severe Hypotony with Ciliary Body Detachment on Anterior Segment Swept-Source Optical Coherence Tomography: A Case Series. J. Clin. Med. 2022, 11, 4647. https://doi.org/10.3390/jcm11164647
Cisiecki S, Bonińska K, Bednarski M. Encircling Scleral Buckling Surgery for Severe Hypotony with Ciliary Body Detachment on Anterior Segment Swept-Source Optical Coherence Tomography: A Case Series. Journal of Clinical Medicine. 2022; 11(16):4647. https://doi.org/10.3390/jcm11164647
Chicago/Turabian StyleCisiecki, Sławomir, Karolina Bonińska, and Maciej Bednarski. 2022. "Encircling Scleral Buckling Surgery for Severe Hypotony with Ciliary Body Detachment on Anterior Segment Swept-Source Optical Coherence Tomography: A Case Series" Journal of Clinical Medicine 11, no. 16: 4647. https://doi.org/10.3390/jcm11164647
APA StyleCisiecki, S., Bonińska, K., & Bednarski, M. (2022). Encircling Scleral Buckling Surgery for Severe Hypotony with Ciliary Body Detachment on Anterior Segment Swept-Source Optical Coherence Tomography: A Case Series. Journal of Clinical Medicine, 11(16), 4647. https://doi.org/10.3390/jcm11164647







