Psycho-Behavioral Profiles of Pediatric Inpatients with Past and Recent Onset of Nonsuicidal Self-Injury: A Cluster Analysis Approach
Abstract
1. Introduction
The Current Study
- (a)
- To define the clinical and psycho-behavioral profiles of inpatients according to the onset of NSSI (i.e., past vs. recent). Specifically, since previous works have highlighted the relevance of emotion regulation function in maintaining NSSI behavior over time [30], we expected inpatients with past NSSI onset (i.e., NSSI for more than one year at the time of hospitalization) to present less interpersonal difficulties and more affective problems compared to inpatients with recent NSSI onset (i.e., NSSI for less than one year).
- (b)
- To explore which personal and clinical variables may constitute risk factors for the maintenance of NSSI behavior over time. We considered some of the main factors previously found to be linked to nonsuicidal self-harming behavior per se, namely, bullying [18], school problems [19], family problems [21], psychiatric familiarity [14], alcohol and substance abuse [20], traumatic life events [17], and borderline intrapsychic functioning [15]. Given that, to the best of our knowledge, no research has investigated the role of these variables in the specific comparison between recent and past NSSI onset yet, we did not formulate any specific hypothesis.
2. Materials and Methods
2.1. Participants
2.2. Procedure
2.3. Measures
2.4. Statistical Analysis
3. Results
3.1. Sociodemographic and Clinical Characteristics of Patients according to the NSSI Onset
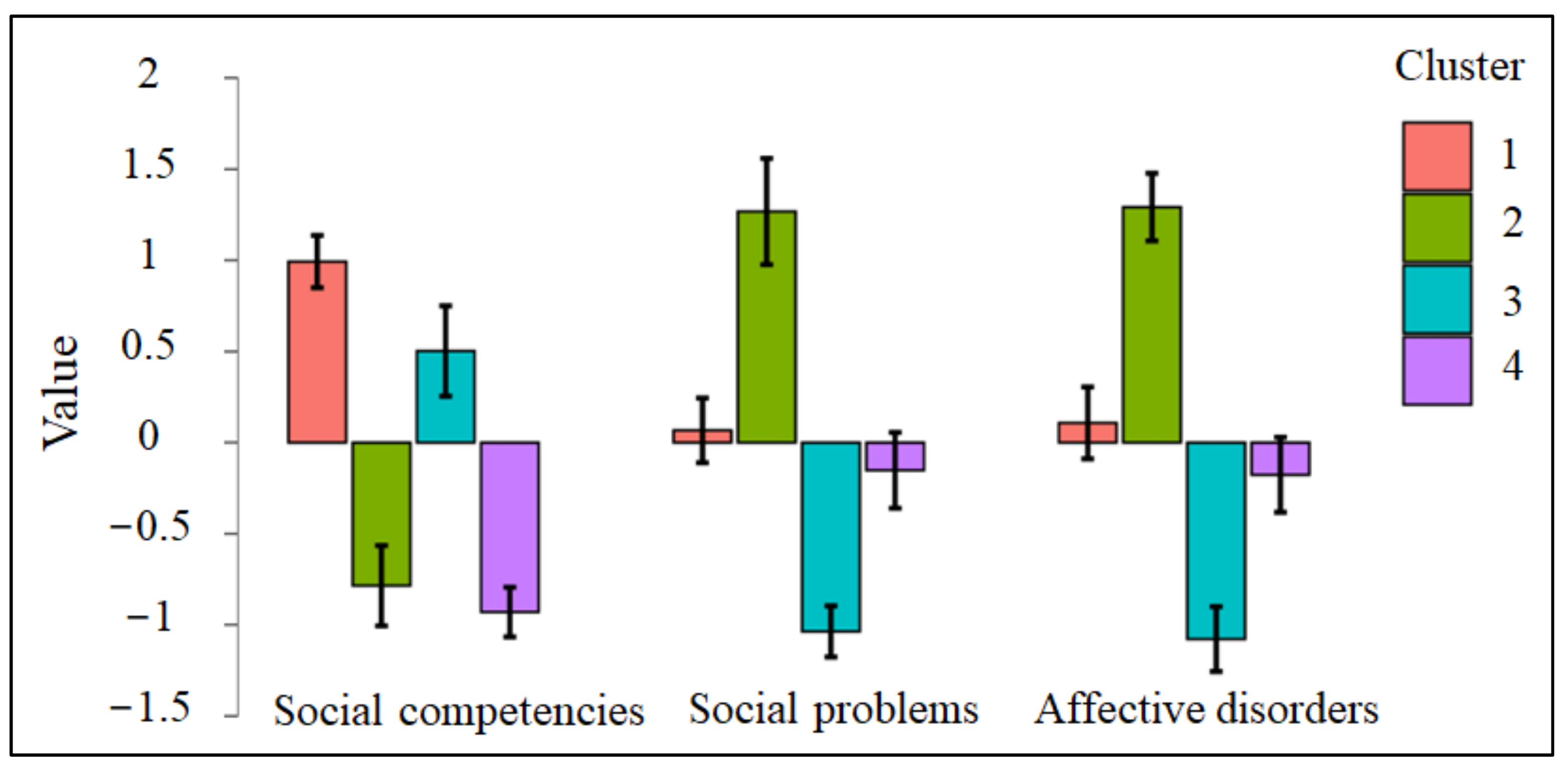
3.2. The Cluster Solution
3.3. Risk Factors for the Maintenance of NSSI over Time
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Nock, M.; Joinerjr, T.; Gordon, K.; Lloydrichardson, E.; Prinstein, M. Non-Suicidal Self-Injury among Adolescents: Diagnostic Correlates and Relation to Suicide Attempts. Psychiatry Res. 2006, 144, 65–72. [Google Scholar] [CrossRef] [PubMed]
- Nock, M.; Favazza, A.R. Non-Suicidal Self-Injury: Definition and Classification. In Understanding Non-Suicidal Self-Injury: Origins, Assessment, and Treatment; American Psychological Association: Washington, DC, USA, 2009; pp. 9–18. [Google Scholar]
- Nock, M.K. Self-Injury. Annu. Rev. Clin. Psychol. 2010, 6, 339–363. [Google Scholar] [CrossRef]
- Plener, P.L.; Fegert, J.M.; Kaess, M.; Kapusta, N.D.; Brunner, R.; Groschwitz, R.C.; In-Albon, T.; Resch, F.; Becker, K. Nonsuicidal Self-Injury in Adolescence: A Clinical Guideline for Diagnostics and Therapy. Z. Kinder Jugendpsychiatr. Psychother. 2017, 45, 463–474. [Google Scholar] [CrossRef]
- Baetens, I.; Claes, L.; Muehlenkamp, J.; Grietens, H.; Onghena, P. Non-Suicidal and Suicidal Self-Injurious Behavior among Flemish Adolescents: A Web-Survey. Arch. Suicide Res. 2011, 15, 56–67. [Google Scholar] [CrossRef] [PubMed]
- Zanus, C.; Battistutta, S.; Aliverti, R.; Montico, M.; Cremaschi, S.; Ronfani, L.; Monasta, L.; Carrozzi, M. Adolescent Admissions to Emergency Departments for Self-Injurious Thoughts and Behaviors. PLoS ONE 2017, 12, e0170979. [Google Scholar] [CrossRef] [PubMed]
- Cipriano, A.; Cella, S.; Cotrufo, P. Nonsuicidal Self-Injury: A Systematic Review. Front. Psychol. 2017, 8. [Google Scholar] [CrossRef]
- Kaess, M.; Parzer, P.; Mattern, M.; Plener, P.L.; Bifulco, A.; Resch, F.; Brunner, R. Adverse Childhood Experiences and Their Impact on Frequency, Severity, and the Individual Function of Nonsuicidal Self-Injury in Youth. Psychiatry Res. 2013, 206, 265–272. [Google Scholar] [CrossRef]
- Wolff, J.; Frazier, E.A.; Esposito-Smythers, C.; Burke, T.; Sloan, E.; Spirito, A. Cognitive and Social Factors Associated with NSSI and Suicide Attempts in Psychiatrically Hospitalized Adolescents. J. Abnorm. Child Psychol. 2013, 41, 1005–1013. [Google Scholar] [CrossRef]
- Cerutti, R.; Manca, M.; Presaghi, F.; Gratz, K.L. Prevalence and Clinical Correlates of Deliberate Self-Harm among a Community Sample of Italian Adolescents. J. Adolesc. 2011, 34, 337–347. [Google Scholar] [CrossRef]
- Giletta, M.; Scholte, R.H.J.; Engels, R.C.M.E.; Ciairano, S.; Prinstein, M.J. Adolescent Non-Suicidal Self-Injury: A Cross-National Study of Community Samples from Italy, the Netherlands and the United States. Psychiatry Res. 2012, 197, 66–72. [Google Scholar] [CrossRef] [PubMed]
- Gatta, M.; Rago, A.; Dal Santo, F.; Spoto, A.; Battistella, P.A. Non-Suicidal Self-Injury among Northern Italian High School Students: Emotional, Interpersonal and Psychopathological Correlates. J. Psychopathol. 2016, 22, 185–190. [Google Scholar]
- Zetterqvist, M.; Jonsson, L.S.; Landberg, Å.; Svedin, C.G. A Potential Increase in Adolescent Nonsuicidal Self-Injury during COVID-19: A Comparison of Data from Three Different Time Points during 2011–2021. Psychiatry Res. 2021, 305, 114208. [Google Scholar] [CrossRef]
- Arbuthnott, A.E.; Lewis, S.P. Parents of Youth Who Self-Injure: A Review of the Literature and Implications for Mental Health Professionals. Child Adolesc. Psychiatry Ment. Health 2015, 9, 35. [Google Scholar] [CrossRef] [PubMed]
- Benzi, I.M.A.; Sarno, I.; Di Pierro, R. Maladaptive Personality Functioning and Non-Suicidal Self Injury in Adolescence. Clin. Neuropsychiatry 2018, 15, 215–221. [Google Scholar]
- Fischer-Kern, M.; Buchheim, A.; Hörz, S.; Schuster, P.; Doering, S.; Kapusta, N.D.; Taubner, S.; Tmej, A.; Rentrop, M.; Buchheim, P.; et al. The Relationship between Personality Organization, Reflective Functioning, and Psychiatric Classification in Borderline Personality Disorder. Psychoanal. Psychol. 2010, 27, 395–409. [Google Scholar] [CrossRef]
- Serafini, G.; Canepa, G.; Adavastro, G.; Nebbia, J.; Belvederi Murri, M.; Erbuto, D.; Pocai, B.; Fiorillo, A.; Pompili, M.; Flouri, E.; et al. The Relationship between Childhood Maltreatment and Non-Suicidal Self-Injury: A Systematic Review. Front. Psychiatry 2017, 8, 149. [Google Scholar] [CrossRef] [PubMed]
- Brunstein Klomek, A.; Snir, A.; Apter, A.; Carli, V.; Wasserman, C.; Hadlaczky, G.; Hoven, C.W.; Sarchiapone, M.; Balazs, J.; Bobes, J.; et al. Association between Victimization by Bullying and Direct Self Injurious Behavior among Adolescence in Europe: A Ten-Country Study. Eur. Child Adolesc. Psychiatry 2016, 25, 1183–1193. [Google Scholar] [CrossRef] [PubMed]
- Baetens, I.; Greene, D.; Van Hove, L.; Van Leeuwen, K.; Wiersema, J.R.; Desoete, A.; Roelants, M. Predictors and Consequences of Non-suicidal Self-injury in Relation to Life, Peer, and School Factors. J. Adolesc. 2021, 90, 100–108. [Google Scholar] [CrossRef] [PubMed]
- Jarvi, S.M.; Swenson, L.P. The Role of Positive Expectancies in Risk Behavior: An Exploration of Alcohol Use and Nonsuicidal Self-Injury. Crisis J. Crisis Interv. Suicide Prev. 2017, 38, 115–122. [Google Scholar] [CrossRef] [PubMed]
- Victor, S.E.; Hipwell, A.E.; Stepp, S.D.; Scott, L.N. Parent and Peer Relationships as Longitudinal Predictors of Adolescent Non-Suicidal Self-Injury Onset. Child Adolesc. Psychiatry Ment. Health 2019, 13, 1. [Google Scholar] [CrossRef]
- Gatta, M.; Sisti, M.; Sudati, L.; Miscioscia, M.; Simonelli, A. The Lausanne Trilogue Play within the Outcome Evaluation in Infant Mental Health: A Preliminary Report. Res. Psychother. Psychopathol. Process Outcome 2016, 19. [Google Scholar] [CrossRef][Green Version]
- Gatta, M.; Miscioscia, M.; Sisti, M.; Comis, I.; Battistella, P.A. Interactive Family Dynamics and Non-Suicidal Self-Injury in Psychiatric Adolescent Patients: A Single Case Study. Front. Psychol. 2017, 8, 46. [Google Scholar] [CrossRef] [PubMed]
- You, J.; Leung, F. The Role of Depressive Symptoms, Family Invalidation and Behavioral Impulsivity in the Occurrence and Repetition of Non-Suicidal Self-Injury in Chinese Adolescents: A 2-Year Follow-up Study. J. Adolesc. 2012, 35, 389–395. [Google Scholar] [CrossRef]
- Wang, B.; You, J.; Lin, M.-P.; Xu, S.; Leung, F. Developmental Trajectories of Nonsuicidal Self-Injury in Adolescence and Intrapersonal/Interpersonal Risk Factors. J. Res. Adolesc. 2016, 27, 1–15. [Google Scholar] [CrossRef] [PubMed]
- You, J.; Leung, F.; Fu, K.; Lai, C.M. The Prevalence of Nonsuicidal Self-Injury and Different Subgroups of Self-Injurers in Chinese Adolescents. Arch. Suicide Res. 2011, 15, 75–86. [Google Scholar] [CrossRef]
- Hankin, B.L.; Abela, J.R.Z. Nonsuicidal Self-Injury in Adolescence: Prospective Rates and Risk Factors in a 2 ½year Longitudinal Study. Psychiatry Res. 2011, 186, 65–70. [Google Scholar] [CrossRef]
- Liu, R.T. Characterizing the Course of Non-Suicidal Self-Injury: A Cognitive Neuroscience Perspective. Neurosci. Biobehav. Rev. 2017, 80, 159–165. [Google Scholar] [CrossRef] [PubMed]
- Selby, E.A.; Kranzler, A.; Fehling, K.B.; Panza, E. Nonsuicidal Self-Injury Disorder: The Path to Diagnostic Validity and Final Obstacles. Clin. Psychol. Rev. 2015, 38, 79–91. [Google Scholar] [CrossRef]
- Victor, S.E.; Styer, D.; Washburn, J.J. Functions of Nonsuicidal Self-Injury (NSSI): Cross-Sectional Associations with NSSI Duration and Longitudinal Changes over Time and Following Treatment. Psychiatry Res. 2016, 241, 83–90. [Google Scholar] [CrossRef] [PubMed]
- Fox, K.R.; Franklin, J.C.; Ribeiro, J.D.; Kleiman, E.M.; Bentley, K.H.; Nock, M.K. Meta-Analysis of Risk Factors for Nonsuicidal Self-Injury. Clin. Psychol. Rev. 2015, 42, 156–167. [Google Scholar] [CrossRef]
- Glenn, C.R.; Klonsky, E.D. Prospective Prediction of Nonsuicidal Self-Injury: A 1-Year Longitudinal Study in Young Adults. Behav. Ther. 2011, 42, 751–762. [Google Scholar] [CrossRef]
- Chapman, A.L.; Gratz, K.L.; Brown, M.Z. Solving the Puzzle of Deliberate Self-Harm: The Experiential Avoidance Model. Behav. Res. Ther. 2006, 44, 371–394. [Google Scholar] [CrossRef] [PubMed]
- Nock, M.K.; Prinstein, M.J. A Functional Approach to the Assessment of Self-Mutilative Behavior. J. Consult. Clin. Psychol. 2004, 72, 885–890. [Google Scholar] [CrossRef] [PubMed]
- Andrews, T.; Martin, G.; Hasking, P.; Page, A. Predictors of Continuation and Cessation of Nonsuicidal Self-Injury. J. Adolesc. Health 2013, 53, 40–46. [Google Scholar] [CrossRef] [PubMed]
- Kiekens, G.; Hasking, P.; Bruffaerts, R.; Claes, L.; Baetens, I.; Boyes, M.; Mortier, P.; Demyttenaere, K.; Whitlock, J. What Predicts Ongoing Nonsuicidal Self-Injury?: A Comparison Between Persistent and Ceased Self-Injury in Emerging Adults. J. Nerv. Ment. Dis. 2017, 205, 762–770. [Google Scholar] [CrossRef]
- Lockwood, J.; Townsend, E.; Daley, D.; Sayal, K. Impulsivity as a Predictor of Self-Harm Onset and Maintenance in Young Adolescents: A Longitudinal Prospective Study. J. Affect. Disord. 2020, 274, 583–592. [Google Scholar] [CrossRef]
- Asarnow, J.R.; Porta, G.; Spirito, A.; Emslie, G.; Clarke, G.; Wagner, K.D.; Vitiello, B.; Keller, M.; Birmaher, B.; McCracken, J.; et al. Suicide Attempts and Nonsuicidal Self-Injury in the Treatment of Resistant Depression in Adolescents: Findings from the TORDIA Study. Adolesc Psychiatry 2011, 50, 10. [Google Scholar] [CrossRef]
- Hamza, C.A.; Stewart, S.L.; Willoughby, T. Examining the Link between Nonsuicidal Self-Injury and Suicidal Behavior: A Review of the Literature and an Integrated Model. Clin. Psychol. Rev. 2012, 32, 482–495. [Google Scholar] [CrossRef]
- Jacobson, C.M.; Muehlenkamp, J.J.; Miller, A.L.; Turner, J.B. Psychiatric Impairment Among Adolescents Engaging in Different Types of Deliberate Self-Harm. J. Clin. Child Adolesc. Psychol. 2008, 37, 363–375. [Google Scholar] [CrossRef]
- Muehlenkamp, J.; Brausch, A.; Quigley, K.; Whitlock, J. Interpersonal Features and Functions of Nonsuicidal Self-Injury. Suicide Life Threat. Behav. 2013, 43, 67–80. [Google Scholar] [CrossRef]
- Nock, M.K. Why Do People Hurt Themselves?: New Insights Into the Nature and Functions of Self-Injury. Curr. Dir. Psychol. Sci. 2009, 18, 78–83. [Google Scholar] [CrossRef] [PubMed]
- Edmondson, A.J.; Brennan, C.A.; House, A.O. Non-Suicidal Reasons for Self-Harm: A Systematic Review of Self-Reported Accounts. J. Affect. Disord. 2016, 191, 109–117. [Google Scholar] [CrossRef] [PubMed]
- Emery, A.A.; Heath, N.L.; Mills, D.J. The Role of Basic Need Satisfaction in the Onset, Maintenance, and Cessation of Non-Suicidal Self-Injury: An Application of Self-Determination Theory. Arch. Suicide Res. 2017, 21, 413–424. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. The ICD-10 Classification of Mental and Behavioural Disorders; Diagnostic Criteria for Research: Geneva, Switzerland, 1993. [Google Scholar]
- Kernberg, O.F. Disturbi Gravi Della Personalità. Bollati Boringhieri; Bollati Boringhieri: Torino, Italy, 1987. [Google Scholar]
- Achenbach, T.M.; Rescorla, L. Manual for the ASEBA Preschool Forms & Profiles: An Integrated System of Multi-Informant Assessment; Manual for the ASEBA preschool forms and profiles; ASEBA: Burlington, VT, USA, 2001. [Google Scholar]
- Frigerio, A.; Cattaneo, C.; Cataldo, M.; Schiatti, A.; Molteni, M.; Battaglia, M. Behavioral and Emotional Problems Among Italian Children and Adolescents Aged 4 to 18 Years as Reported by Parents and Teachers. Eur. J. Psychol. Assess. 2004, 20, 124–133. [Google Scholar] [CrossRef]
- Frigerio, A.; Vanzin, L.; Pastore, V.; Nobile, M.; Giorda, R.; Marino, C.; Molteni, M.; Rucci, P.; Ammaniti, M.; Lucarelli, L.; et al. The Italian Preadolescent Mental Health Project (PrISMA): Rationale and Methods. Int. J. Methods Psychiatr. Res. 2006, 15, 22–35. [Google Scholar] [CrossRef]
- Biederman, J.; Petty, C.R.; Day, H.; Goldin, R.L.; Spencer, T.; Faraone, S.V.; Surman, C.B.H.; Wozniak, J. Severity of the Aggression/Anxiety-Depression/Attention Child Behavior Checklist Profile Discriminates Between Different Levels of Deficits in Emotional Regulation in Youth With Attention-Deficit Hyperactivity Disorder. J. Dev. Behav. Pediatr. 2012, 33, 236–243. [Google Scholar] [CrossRef]
- Biederman, J.; Petty, C.R.; Monuteaux, M.C.; Evans, M.; Parcell, T.; Faraone, S.V.; Wozniak, J. The Child Behavior Checklist-Pediatric Bipolar Disorder Profile Predicts a Subsequent Diagnosis of Bipolar Disorder and Associated Impairments in ADHD Youth Growing Up: A Longitudinal Analysis. J. Clin. Psychiatry 2009, 70, 732–740. [Google Scholar] [CrossRef]
- Schwarz, G. Estimating the Dimension of a Model. Ann. Stat. 1978, 6, 461–464. [Google Scholar] [CrossRef]
- Fraley, C. How Many Clusters? Which Clustering Method? Answers Via Model-Based Cluster Analysis. Comput. J. 1998, 41, 578–588. [Google Scholar] [CrossRef]
- Akaike, H. Information Theory and an Extension of the Maximum Likelihood Principle. In Proceedings of the Second International Symposium on Information Theory, Tsahkadsor, Armenia, 2–8 September 1971; Adademiai Kiado: Budapest, Hungary, 1973; pp. 267–281. [Google Scholar]
- JASP Team. JASP (Version 0.16.1). Available online: https://jasp-stats.org/previous-versions/ (accessed on 28 June 2022).
- Hawton, K.; Hall, S.; Simkin, S.; Bale, L.; Bond, A.; Codd, S.; Stewart, A. Deliberate Self-Harm in Adolescents: A Study of Characteristics and Trends in Oxford, 1990–2000: Deliberate Self-Harm in Adolescents. J. Child Psychol. Psychiatry 2003, 44, 1191–1198. [Google Scholar] [CrossRef] [PubMed]
- Nock, M.K. Actions Speak Louder than Words: An Elaborated Theoretical Model of the Social Functions of Self-Injury and Other Harmful Behaviors. Appl. Prev. Psychol. 2008, 12, 159–168. [Google Scholar] [CrossRef]
- Cassels, M.; Wilkinson, P. Non-Suicidal Self-Injury in Adolescence. Paediatr. Child Health 2016, 26, 554–558. [Google Scholar] [CrossRef]
- Tatnell, R.; Kelada, L.; Hasking, P.; Martin, G. Longitudinal Analysis of Adolescent NSSI: The Role of Intrapersonal and Interpersonal Factors. J. Abnorm. Child Psychol. 2014, 42, 885–896. [Google Scholar] [CrossRef] [PubMed]
- Parolin, M.; Miscioscia, M.; De Carli, P.; Cristofalo, P.; Gatta, M.; Simonelli, A. Alexithymia in Young Adults With Substance Use Disorders: Critical Issues About Specificity and Treatment Predictivity. Front. Psychol. 2018, 9, 645. [Google Scholar] [CrossRef] [PubMed]
- Raffagnato, A.; Angelico, C.; Valentini, P.; Miscioscia, M.; Gatta, M. Using the Body When There Are No Words for Feelings: Alexithymia and Somatization in Self-Harming Adolescents. Front. Psychiatry 2020, 11, 262. [Google Scholar] [CrossRef]
- Weissman, D.G.; Nook, E.C.; Dews, A.A.; Miller, A.B.; Lambert, H.K.; Sasse, S.F.; Somerville, L.H.; McLaughlin, K.A. Low Emotional Awareness as a Transdiagnostic Mechanism Underlying Psychopathology in Adolescence. Clin. Psychol. Sci. 2020, 8, 971–988. [Google Scholar] [CrossRef]
- Di Tella, M.; Adenzato, M.; Catmur, C.; Miti, F.; Castelli, L.; Ardito, R.B. The Role of Alexithymia in Social Cognition: Evidence from a Non-Clinical Population. J. Affect. Disord. 2020, 273, 482–492. [Google Scholar] [CrossRef]
- Heilbron, N.; Prinstein, M.J. Peer Influence and Adolescent Nonsuicidal Self-Injury: A Theoretical Review of Mechanisms and Moderators. Appl. Prev. Psychol. 2008, 12, 169–177. [Google Scholar] [CrossRef]
- Evans, R.; Hurrell, C. The Role of Schools in Children and Young People’s Self-Harm and Suicide: Systematic Review and Meta-Ethnography of Qualitative Research. BMC Public Health 2016, 16, 401. [Google Scholar] [CrossRef]
- Victor, S.E.; Klonsky, E.D. Correlates of Suicide Attempts among Self-Injurers: A Meta-Analysis. Clin. Psychol. Rev. 2014, 34, 282–297. [Google Scholar] [CrossRef]
- Tuisku, V.; Kiviruusu, O.; Pelkonen, M.; Karlsson, L.; Strandholm, T.; Marttunen, M. Depressed Adolescents as Young Adults –Predictors of Suicide Attempt and Non-Suicidal Self-Injury during an 8-Year Follow-Up. J. Affect. Disord. 2014, 152–154, 313–319. [Google Scholar] [CrossRef] [PubMed]
- Klonsky, E.D.; May, A.M. The Three-Step Theory (3ST): A New Theory of Suicide Rooted in the “Ideation-to-Action” Framework. Int. J. Cogn. Ther. 2015, 8, 114–129. [Google Scholar] [CrossRef]
- Klonsky, E.D.; May, A.M.; Saffer, B.Y. Suicide, Suicide Attempts, and Suicidal Ideation. Annu. Rev. Clin. Psychol. 2016, 12, 307–330. [Google Scholar] [CrossRef]
- Lee, W.K. Psychological Characteristics of Self-Harming Behavior in Korean Adolescents. Asian J. Psychiatry 2016, 23, 119–124. [Google Scholar] [CrossRef]
- Plener, P.L.; Schumacher, T.S.; Munz, L.M.; Groschwitz, R.C. The Longitudinal Course of Non-Suicidal Self-Injury and Deliberate Self-Harm: A Systematic Review of the Literature. Bord. Personal. Disord. Emot. Dysregul. 2015, 2, 2. [Google Scholar] [CrossRef]
- Rodav, O.; Levy, S.; Hamdan, S. Clinical Characteristics and Functions of Non-Suicide Self-Injury in Youth. Eur. Psychiatry 2014, 29, 503–508. [Google Scholar] [CrossRef]
- Brunner, R.; Kaess, M.; Parzer, P.; Fischer, G.; Carli, V.; Hoven, C.W.; Wasserman, C.; Sarchiapone, M.; Resch, F.; Apter, A.; et al. Life-Time Prevalence and Psychosocial Correlates of Adolescent Direct Self-Injurious Behavior: A Comparative Study of Findings in 11 European Countries. J. Child Psychol. Psychiatry 2014, 55, 337–348. [Google Scholar] [CrossRef] [PubMed]
- Franklin, J.C.; Puzia, M.E.; Lee, K.M.; Lee, G.E.; Hanna, E.K.; Spring, V.L.; Prinstein, M.J. The Nature of Pain Offset Relief in Nonsuicidal Self-Injury: A Laboratory Study. Clin. Psychol. Sci. 2013, 1, 110–119. [Google Scholar] [CrossRef]
- Andover, M.S.; Morris, B.W. Expanding and Clarifying the Role of Emotion Regulation in Nonsuicidal Self-Injury. Can. J. Psychiatry 2014, 59, 569–575. [Google Scholar] [CrossRef]
- Kumar, G.; Pepe, D.; Steer, R.A. Adolescent Psychiatric Inpatients’ Self-Reported Reasons for Cutting Themselves. J. Nerv. Ment. Dis. 2004, 192, 830–836. [Google Scholar] [CrossRef]
- Muehlenkamp, J.J.; Gutierrez, P.M. An Investigation of Differences Between Self-Injurious Behavior and Suicide Attempts in a Sample of Adolescents. Suicide Life. Threat. Behav. 2004, 34, 12–23. [Google Scholar] [CrossRef] [PubMed]
- Epstein, S.; Roberts, E.; Sedgwick, R.; Polling, C.; Finning, K.; Ford, T.; Dutta, R.; Downs, J. School Absenteeism as a Risk Factor for Self-Harm and Suicidal Ideation in Children and Adolescents: A Systematic Review and Meta-Analysis. Eur. Child Adolesc. Psychiatry 2019, 29, 1175–1194. [Google Scholar] [CrossRef] [PubMed]
- Nakar, O.; Brunner, R.; Schilling, O.; Chanen, A.; Fischer, G.; Parzer, P.; Carli, V.; Wasserman, D.; Sarchiapone, M.; Wasserman, C.; et al. Developmental Trajectories of Self-Injurious Behavior, Suicidal Behavior and Substance Misuse and Their Association with Adolescent Borderline Personality Pathology. J. Affect. Disord. 2016, 197, 231–238. [Google Scholar] [CrossRef] [PubMed]
- Moggi, F. Etiological Theories on the Relationship of Mental Disorders and Substance Use Disorders. In Dual Diagnosis: The Evolving Conceptual Framework; Bibliotheca Psychiatrica: Basel, Switzerland, 2005; pp. 15–30. [Google Scholar]
- Sarno, I.; Madeddu, F. Comportamenti Di Autoferimento, Uso Di Sostanze e Disturbo Borderline. Personalità/Dipendenze 2007, 13, 117–151. [Google Scholar]
| Past NSSI Onset % | Recent NSSI Onset % | |
|---|---|---|
| Sociodemographic variables | ||
| Female | 84.21 | 90.16 |
| Caucasian | 89.47 | 88.52 |
| Immigration | 18.42 | 21.31 |
| Separated parents | 28.94 | 28.33 |
| Only child | 23.68 | 16.39 |
| High school educational level | 65.78 | 59.01 |
| Maternal unemployment | 10.52 | 14.75 |
| Paternal unemployment | 5.26 | 3.27 |
| Individual variables | ||
| School problems | 83.78 | 62.29 |
| Bullying/cyberbullying | 37.83 | 48.33 |
| Social withdrawal | 10.81 | 21.31 |
| Conflictual peer relationships | 35.13 | 36.06 |
| Intensive use of online social networks | 56.52 | 53.19 |
| Alcohol use/abuse | 34.21 | 15.25 |
| Substance use/abuse | 34.21 | 11.86 |
| Smoking | 47.36 | 16.94 |
| Borderline functioning | 58.33 | 44.82 |
| Traumatic life events | 52.63 | 45.90 |
| Eating disorders | 10.52 | 14.75 |
| Chronic pathology | 23.68 | 37.70 |
| Family variables | ||
| Family health problems | 51.35 | 45.90 |
| Intra-family problems | 73.68 | 67.21 |
| Psychiatric familiarity | 67.64 | 72.41 |
| Variables related to admission to mental health services | ||
| Previous hospitalizations | 39.47 | 29.50 |
| 1-year post-discharge relapse | 10.52 | 31.14 |
| Previous accesses in other mental health services | 89.47 | 75.40 |
| Pharmacological therapy | 89.18 | 83.33 |
| Psychotherapy | 94.28 | 89.65 |
| Self-injurious phenomena variables | ||
| Attempted suicide | 39.47 | 40.98 |
| Suicidal ideation | 81.57 | 85.24 |
| High NSSI frequency | 63.15 | 45.90 |
| Multiple self-injured body parts | 75.75 | 56.36 |
| Intrapersonal function of NSSI | 100 | 93.47 |
| Clustering Solution | R2 | AIC | BIC | Silhouette |
|---|---|---|---|---|
| Two clusters | 0.41 | 174.29 | 189.55 | 0.35 |
| Three clusters | 0.58 | 134.04 | 157.93 | 0.34 |
| Four clusters | 0.68 | 114.36 | 144.88 | 0.34 |
| Five clusters | 0.72 | 109.13 | 147.28 | 0.31 |
| YSR Scales | β | Z | p | χ2 (df) | Odds Ratio (95% CI) |
|---|---|---|---|---|---|
| Social competencies | 0.11 | 3.26 | 0.001 | 13.05 (1) | 1.11 (1.04–1.19) |
| Social problems | −0.07 | −1.75 | 0.08 | 3.44 (1) | 0.93 (0.86–1.01) |
| Affective disorders | 0.09 | 2.81 | 0.005 | 9.47 (1) | 1.09 (1.02–1.16) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Raffagnato, A.; Iannattone, S.; Fasolato, R.; Rossaro, M.P.; Spoto, A.; Gatta, M. Psycho-Behavioral Profiles of Pediatric Inpatients with Past and Recent Onset of Nonsuicidal Self-Injury: A Cluster Analysis Approach. J. Clin. Med. 2022, 11, 4602. https://doi.org/10.3390/jcm11154602
Raffagnato A, Iannattone S, Fasolato R, Rossaro MP, Spoto A, Gatta M. Psycho-Behavioral Profiles of Pediatric Inpatients with Past and Recent Onset of Nonsuicidal Self-Injury: A Cluster Analysis Approach. Journal of Clinical Medicine. 2022; 11(15):4602. https://doi.org/10.3390/jcm11154602
Chicago/Turabian StyleRaffagnato, Alessia, Sara Iannattone, Rachele Fasolato, Maria Paola Rossaro, Andrea Spoto, and Michela Gatta. 2022. "Psycho-Behavioral Profiles of Pediatric Inpatients with Past and Recent Onset of Nonsuicidal Self-Injury: A Cluster Analysis Approach" Journal of Clinical Medicine 11, no. 15: 4602. https://doi.org/10.3390/jcm11154602
APA StyleRaffagnato, A., Iannattone, S., Fasolato, R., Rossaro, M. P., Spoto, A., & Gatta, M. (2022). Psycho-Behavioral Profiles of Pediatric Inpatients with Past and Recent Onset of Nonsuicidal Self-Injury: A Cluster Analysis Approach. Journal of Clinical Medicine, 11(15), 4602. https://doi.org/10.3390/jcm11154602






