Proadrenomedullin in the Management of COVID-19 Critically Ill Patients in Intensive Care Unit: A Systematic Review and Meta-Analysis of Evidence and Uncertainties in Existing Literature
Abstract
:1. Introduction
2. Materials and Methods
2.1. Eligibility Criteria
2.2. Information Sources
2.3. Search Strategy
- PubMed: “proADM” [All Fields] AND (“COVID-19” [All Fields] OR “COVID-19” [MeSH Terms] OR “COVID-19 vaccines” [All Fields] OR “COVID-19 vaccines” [MeSH Terms] OR “COVID-19 serotherapy” [All Fields] OR “COVID-19 serotherapy” [Supplementary Concept] OR “COVID-19 nucleic acid testing” [All Fields] OR “COVID-19 nucleic acid testing” [MeSH Terms] OR “COVID-19 serological testing” [All Fields] OR “COVID-19 serological testing” [MeSH Terms] OR “COVID-19 testing” [All Fields] OR “COVID-19 testing” [MeSH Terms] OR “SARS-CoV-2” [All Fields] OR “SARS-CoV-2” [MeSH Terms] OR “severe acute respiratory syndrome coronavirus 2” [All Fields] OR “ncov” [All Fields] OR “2019 ncov” [All Fields] OR ((“coronavirus” [MeSH Terms] OR “coronavirus” [All Fields] OR “cov” [All Fields]) AND 1 November 2019:3000/12/31 [Date—Publication])); Embase, Scopus, clinicaltrials.gov, and greylit.org: (‘proadrenomedullin’/exp OR proadrenomedullin) AND (‘coronavirus disease 2019’/exp OR ‘coronavirus disease 2019’).
2.4. Selection and Data Collection Process
2.5. Study Risk of Bias Assessment
2.6. Synthesis Methods
3. Results
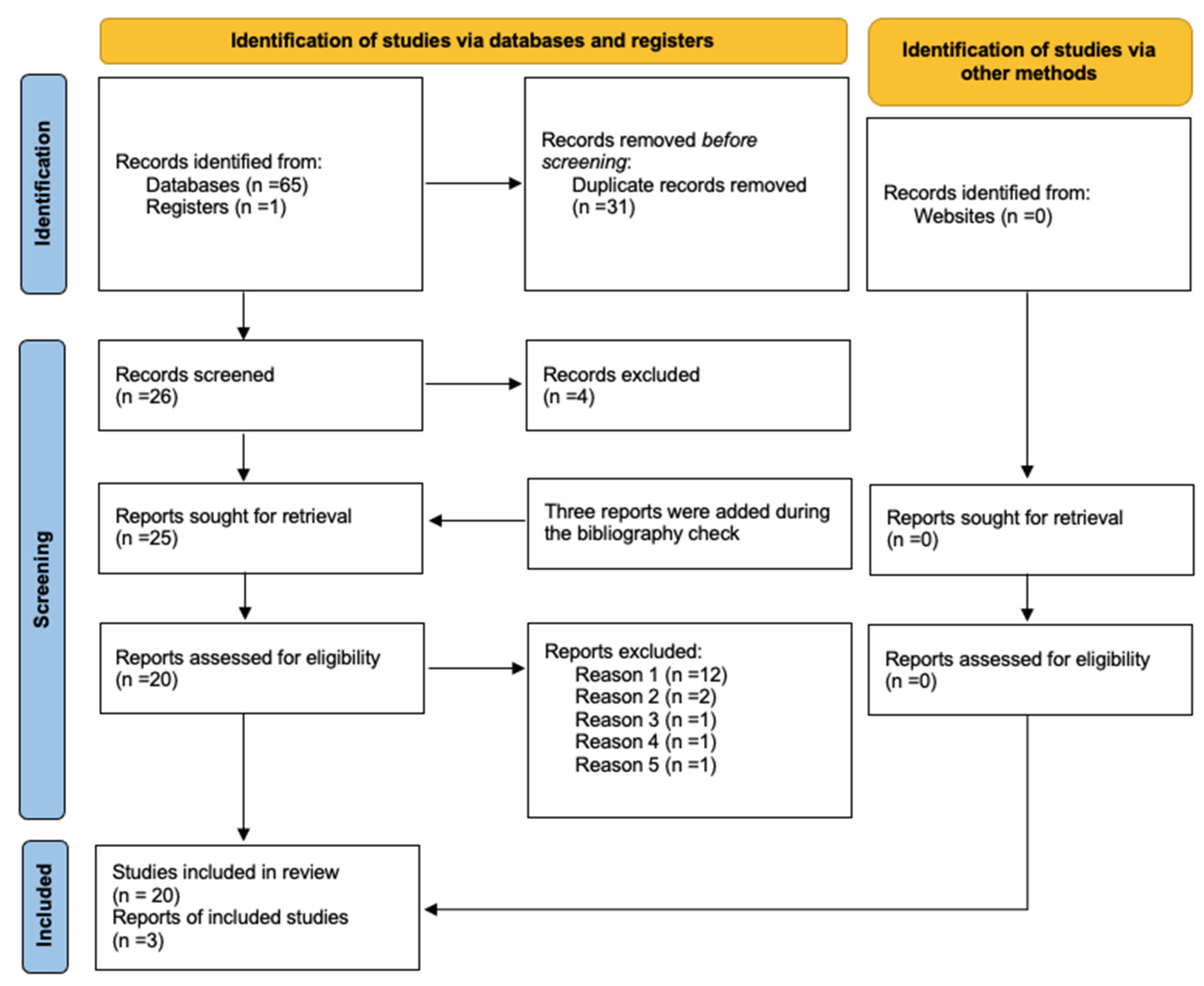
3.1. Study Selection
3.2. Systematic Review
Study Characteristics
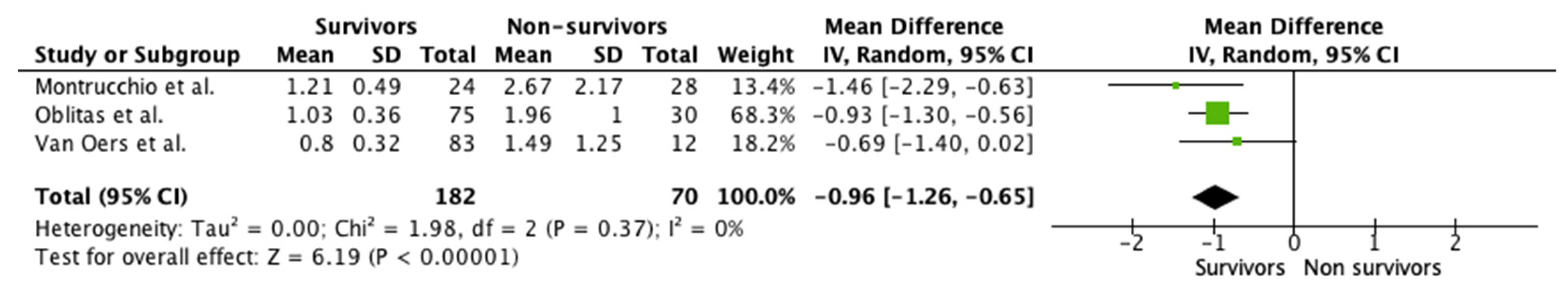
3.3. Meta-Analysis
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Saeed, K.; Legramante, J.M.; Angeletti, S.; Curcio, F.; Miguens, I.; Poole, S.; Tascini, C.; Sozio, E.; Del Castillo, J.G. Mid-regional pro-adrenomedullin as a supplementary tool to clinical parameters in cases of suspicion of infection in the emergency department. Expert Rev. Mol. Diagn. 2021, 21, 397–404. [Google Scholar] [CrossRef]
- Saeed, K.; Wilson, D.C.; Bloos, F.; Schuetz, P.; van der Does, Y.; Melander, O.; Hausfater, P.; Legramante, J.M.; Claessens, Y.-E.; Amin, D.; et al. The early identification of disease progression in patients with suspected infection presenting to the emergency department: A multi-centre derivation and validation study. Crit. Care 2019, 23, 40. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Elke, G.; Bloos, F.; Wilson, D.C.; Brunkhorst, F.M.; Briegel, J.; Reinhart, K.; Loeffler, M.; Kluge, S.; Nierhaus, A.; Jaschinski, U.; et al. The use of mid-regional proadrenomedullin to identify disease severity and treatment response to sepsis-a secondary analysis of a large randomised controlled trial. Crit. Care 2018, 22, 79. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wilson, D.C.; Schefold, J.C.; Baldirà, J.; Spinetti, T.; Saeed, K.; Elke, G. Adrenomedullin in COVID-19 induced endotheliitis. Crit. Care 2020, 24, 411. [Google Scholar] [CrossRef]
- Varga, Z.; Flammer, A.J.; Steiger, P.; Haberecker, M.; Andermatt, R.; Zinkernagel, A.S.; Mehra, M.R.; Schuepbach, R.A.; Ruschitzka, F.; Moch, H. Endothelial cell infection and endotheliitis in COVID-19. Lancet 2020, 395, 1417–1418. [Google Scholar] [CrossRef]
- Renaud, B.; Schuetz, P.; Claessens, Y.E.; Labarère, J.; Albrich, W.; Mueller, B. Proadrenomedullin improves Risk of Early Admission to ICU score for predicting early severe community-acquired pneumonia. Chest 2012, 142, 1447–1454. [Google Scholar] [CrossRef]
- Van Paassen, J.; Van Dissel, J.T.; Hiemstra, P.S.; Zwaginga, J.J.; Cobbaert, C.M.; Juffermans, N.P.; De Wilde, R.B.; Stijnen, T.; De Jonge, E.; Klautz, R.J.; et al. Perioperative proADM-change is associated with the development of acute respiratory distress syndrome in critically ill cardiac surgery patients: A prospective cohort study. Biomark. Med. 2019, 13, 1081–1091. [Google Scholar] [CrossRef] [PubMed]
- Sterne, J.A.; Hernán, M.A.; Reeves, B.C.; Savović, J.; Berkman, N.D.; Viswanathan, M.; Henry, D.; Altman, D.G.; Ansari, M.T.; Boutron, I.; et al. ROBINS-I: A tool for assessing risk of bias in non-randomised studies of interventions. BMJ 2016, 355, i4919. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sterne, J.A.C.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ 2019, 366, l4898. [Google Scholar] [CrossRef] [Green Version]
- Luo, D.; Wan, X.; Liu, J.; Tong, T. Optimally estimating the sample mean from the sample size, median, mid-range, and/or mid-quartile range. Stat. Methods Med. Res. 2018, 27, 1785–1805. [Google Scholar] [CrossRef] [Green Version]
- Revman Cp. Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager 5 (RevMan 5); Version 5.4; Nordic Cochrane Centre, The Cochrane Collaboration: Copenhagen, Denmark, 2020. [Google Scholar]
- Higgins, J.P.T.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.J.; Welch, V.A. Cochrane Handbook for Systematic Reviews of Interventions; John Wiley & Sons: Hoboken, NJ, USA, 2019. [Google Scholar]
- Lippi, G.; Henry, B.M. Pooled analysis of mid-regional pro-adrenomedullin values in COVID-19 patients with critical illness. Intern. Emerg. Med. 2021, 16, 1723–1725. [Google Scholar] [CrossRef] [PubMed]
- Oblitas, C.-M.; Galeano-Valle, F.; Ramírez-Navarro, J.; López-Cano, J.; Monterrubio-Manrique, Á.; García-Gámiz, M.; Sancho-González, M.; Arenal-López, S.; Walther, L.-A.-S.; Demelo-Rodríguez, P. Mid-Regional Pro-Adrenomedullin, Methemoglobin and Carboxyhemoglobin as Prognosis Biomarkers in Critically Ill Patients with COVID-19: An Observational Prospective Study. Viruses 2021, 13, 2445. [Google Scholar] [CrossRef]
- Malinina, D.A.; Shlyk, I.V.; Polushin, Y.S.; Afanasiev, A.A.; Stanevich, O.V.; Bakin, E.A. The informative value of proadrenomedullin in patients with severe COVID-19. Messenger Anesthesiol. Resusc. 2020, 17, 31–38. [Google Scholar] [CrossRef]
- Roedl, K.; Jarczak, D.; Fischer, M.; Haddad, M.; Boenisch, O.; de Heer, G.; Burdelski, C.; Frings, D.; Sensen, B.; Karakas, M.; et al. MR-proAdrenomedullin as a predictor of renal replacement therapy in a cohort of critically ill patients with COVID-19. Biomarkers 2021, 26, 417–424. [Google Scholar] [CrossRef]
- Girona-Alarcon, M.; Bobillo-Perez, S.; Sole-Ribalta, A.; Hernandez, L.; Guitart, C.; Suarez, R.; Balaguer, M.; Cambra, F.J.; Jordan, I. The different manifestations of COVID-19 in adults and children: A cohort study in an intensive care unit. BMC Infect. Dis. 2021, 21, 87. [Google Scholar] [CrossRef]
- Simon, T.P.; Stoppe, C.; Breuer, T.; Stiehler, L.; Dreher, M.; Kersten, A.; Kluge, S.; Karakas, M.; Zechendorf, E.; Marx, G.; et al. Prognostic Value of Bioactive Adrenomedullin in Critically Ill Patients with COVID-19 in Germany: An Observational Cohort Study. J. Clin. Med. 2021, 10, 1667. [Google Scholar] [CrossRef] [PubMed]
- Oblitas, C.M.; Galeano-Valle, F.; Lopez-Cano, J.; Monterrubio-Manrique, A.; Garcia-Gamiz, M.; Ramirez-Navarro, J.; Sancho-Gonzalez, M.; Arenal-Lopez, S.; Alvarez-Sala Walther, L.; Demelo-Rodriguez, P. Potential prognostic biomarkers in COVID19: Role of mid-regional pro-adrenomedullin, methemoglobin and carboxyhemoglobin. Intensive Care Med. Exp. 2021, 9, 50. [Google Scholar] [CrossRef]
- Lhote, S.; Van Grunderbeeck, N.; Colling, D.; Verchain, S.; Varillon, C.; Floch, P.; Vinsonneau, C.; Caulier, T.; Granier, M.; Mallat, J. Proadrenomedullin assessment of multi-organ failure in COVID-19 sepsis (PAMOCOS): A prospective, multicentric observational study. Crit. Care 2021, 25, 383. [Google Scholar] [CrossRef]
- Benedetti, I.; Spinelli, D.; Callegari, T.; Bonometti, R.; Molinaro, E.; Novara, E.; Cassinari, M.; Frino, C.; Guaschino, R.; Boverio, R.; et al. High levels of mid-regional proadrenomedullin in ARDS COVID-19 patients: The experience of a single, italian center. Eur. Rev. Med. Pharmacol. Sci. 2021, 25, 1743–1751. [Google Scholar] [CrossRef]
- García de Guadiana-Romualdo, L.; Martínez Martínez, M.; Rodríguez Mulero, M.D.; Esteban-Torrella, P.; Hernández Olivo, M.; Alcaraz García, M.J.; Campos-Rodríguez, V.; Sancho-Rodríguez, N.; Galindo Martínez, M.; Alcaraz, A.; et al. Circulating MR-proADM levels, as an indicator of endothelial dysfunction, for early risk stratification of mid-term mortality in COVID-19 patients. Int. J. Infect. Dis. 2021, 111, 211–218. [Google Scholar] [CrossRef] [PubMed]
- Gregoriano, C.; Koch, D.; Kutz, A.; Haubitz, S.; Conen, A.; Bernasconi, L.; Hammerer-Lercher, A.; Saeed, K.; Mueller, B.; Schuetz, P. The vasoactive peptide MR-pro-adrenomedullin in COVID-19 patients: An observational study. Clin. Chem. Lab. Med. 2021, 59, 995–1004. [Google Scholar] [CrossRef] [PubMed]
- Indirli, R.; Bandera, A.; Valenti, L.; Ceriotti, F.; Di Modugno, A.; Tettamanti, M.; Gualtierotti, R.; Peyvandi, F.; Montano, N.; Blasi, F.; et al. Prognostic value of copeptin and mid-regional proadrenomedullin in COVID-19-hospitalized patients. Eur. J. Clin. Investig. 2022, 52, e13753. [Google Scholar] [CrossRef] [PubMed]
- Lo Sasso, B.; Gambino, C.M.; Scichilone, N.; Giglio, R.V.; Bivona, G.; Scazzone, C.; Muratore, R.; Milano, S.; Barbagallo, M.; Agnello, L.; et al. Clinical Utility of Midregional Proadrenomedullin in Patients with COVID-19. Lab. Med. 2021, 52, 493–498. [Google Scholar] [CrossRef]
- Méndez, R.; González-Jiménez, P.; Latorre, A.; Piqueras, M.; Bouzas, L.; Yépez, K.; Ferrando, A.; Zaldívar-Olmeda, E.; Moscardó, A.; Alonso, R.; et al. Acute and sustained increase in endothelial biomarkers in COVID-19. Thorax 2022, 77, 400–403. [Google Scholar] [CrossRef] [PubMed]
- Minieri, M.; Di Lecce, V.N.; Lia, M.S.; Maurici, M.; Bernardini, S.; Legramante, J.M. Role of MR-proADM in the risk stratification of COVID-19 patients assessed at the triage of the Emergency Department. Crit. Care 2021, 25, 407. [Google Scholar] [CrossRef] [PubMed]
- Montrucchio, G.; Sales, G.; Rumbolo, F.; Palmesino, F.; Fanelli, V.; Urbino, R.; Filippini, C.; Mengozzi, G.; Brazzi, L. Effectiveness of mid-regional pro-adrenomedullin (MR-proADM) as prognostic marker in COVID-19 critically ill patients: An observational prospective study. PLoS ONE 2021, 16, e0246771. [Google Scholar] [CrossRef]
- Moore, N.; Williams, R.; Mori, M.; Bertolusso, B.; Vernet, G.; Lynch, J.; Philipson, P.; Ledgerwood, T.; Kidd, S.P.; Thomas, C.; et al. Mid-regional proadrenomedullin (MR-proADM), C-reactive protein (CRP) and other biomarkers in the early identification of disease progression in patients with COVID-19 in the acute NHS setting. J. Clin. Pathol. 2022; in press. [Google Scholar] [CrossRef]
- Popov, D.A.; Borovkova, U.L.; Rybka, M.M.; Ramnenok, T.V.; Golukhova, E.Z. Predictive value of proadrenomedullin in patients with COVID-19. Russ. J. Anesthesiol. Reanimatol. 2020, 6, 6–12. [Google Scholar] [CrossRef]
- Sozio, E.; Tascini, C.; Fabris, M.; D’Aurizio, F.; De Carlo, C.; Graziano, E.; Bassi, F.; Sbrana, F.; Ripoli, A.; Pagotto, A.; et al. MR-proADM as prognostic factor of outcome in COVID-19 patients. Sci. Rep. 2021, 11, 5121. [Google Scholar] [CrossRef] [PubMed]
- Spoto, S.; Agrò, F.E.; Sambuco, F.; Travaglino, F.; Valeriani, E.; Fogolari, M.; Mangiacapra, F.; Costantino, S.; Ciccozzi, M.; Angeletti, S. High value of mid-regional proadrenomedullin in COVID-19: A marker of widespread endothelial damage, disease severity, and mortality. J. Med. Virol. 2021, 93, 2820–2827. [Google Scholar] [CrossRef]
- van Oers, J.A.H.; Kluiters, Y.; Bons, J.A.P.; de Jongh, M.; Pouwels, S.; Ramnarain, D.; de Lange, D.W.; de Grooth, H.J.; Girbes, A.R.J. Endothelium-associated biomarkers mid-regional proadrenomedullin and C-terminal proendothelin-1 have good ability to predict 28-day mortality in critically ill patients with SARS-CoV-2 pneumonia: A prospective cohort study. J. Crit. Care 2021, 66, 173–180. [Google Scholar] [CrossRef]
- Zaninotto, M.; Maria Mion, M.; Marchioro, L.; Padoan, A.; Plebani, M. Endothelial dysfunction and Mid-Regional proAdrenomedullin: What role in SARS-CoV-2 infected Patients? Clin. Chim. Acta 2021, 523, 185–190. [Google Scholar] [CrossRef]
- Agnello, L.; Bellia, C.; Iacolino, G.; Gambino, C.M.; Petrancosta, R.; Lo Sasso, B.; Ciaccio, M. Mid-regional pro-adrenomedullin predicts poor outcome in non-selected patients admitted to intensive care unit. Biochim. Clin. 2018, 42, S171. [Google Scholar]
- Piccioni, A.; Saviano, A.; Cicchinelli, S.; Valletta, F.; Santoro, M.C.; de Cunzo, T.; Zanza, C.; Longhitano, Y.; Tullo, G.; Tilli, P.; et al. Proadrenomedullin in Sepsis and Septic Shock: A Role in the Emergency Department. Med. Kaunas 2021, 57, 920. [Google Scholar] [CrossRef] [PubMed]
- Bima, P.; Montrucchio, G.; Caramello, V.; Rumbolo, F.; Dutto, S.; Boasso, S.; Ferraro, A.; Brazzi, L.; Lupia, E.; Boccuzzi, A.; et al. Prognostic Value of Mid-Regional Proadrenomedullin Sampled at Presentation and after 72 Hours in Septic Patients Presenting to the Emergency Department: An Observational Two-Center Study. Biomedicines 2022, 10, 719. [Google Scholar] [CrossRef] [PubMed]
- Marino, R.; Struck, J.; Maisel, A.S.; Magrini, L.; Bergmann, A.; Di Somma, S. Plasma adrenomedullin is associated with short-term mortality and vasopressor requirement in patients admitted with sepsis. Crit. Care 2014, 18, R34. [Google Scholar] [CrossRef] [Green Version]
- Laterre, P.F.; Pickkers, P.; Marx, G.; Wittebole, X.; Meziani, F.; Dugernier, T.; Huberlant, V.; Schuerholz, T.; François, B.; Lascarrou, J.B.; et al. Safety and tolerability of non-neutralizing adrenomedullin antibody adrecizumab (HAM8101) in septic shock patients: The AdrenOSS-2 phase 2a biomarker-guided trial. Intensive Care Med. 2021, 47, 1284–1294. [Google Scholar] [CrossRef]
| Author | Year | Type of Study | Country | Period | Number of Patient | Clinical Setting | Timing | Outcome | Findings | AUC | Cut Off |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Benedetti et al. [21] | 2021 | prospective observational | Italy | March–April 2020 | 21 | IMCU | admission (T0), 24 h (T1), T3 e 5 | severe disease |
| 0.81 | 1.07 nmol/L |
| García de Guadiana-Romualdo et al. [22] | 2021 | prospective observational | Spain | March–April 2021 | 99 | ED | T0 | mortality/severe disease progression |
| 0.871 | 0.80 nmol/L |
| Girona-Alarcon et al. [17] | 2021 | prospective observational cohort | Spain | March–June 2020 | 20 | ICU | hospitalization | pediatric vs. adult population |
| ||
| Gregoriano et al. [23] | 2021 | prospective observational | Switzerland | February–April 2020 | 89 | mixed population | T0, T1, T2, T3 | in-hospital mortality |
| 0.78 | 0.93 nmol/L |
| Indirli et al. [24] | 2022 | retrospective | Italy | March–June 2020 | 116 | IMCU | At admission | in-hospital mortality |
| 0.79 | >1 |
| Lhote et al. * | 2021 | prospective multicentric | France | July 2020 to February 2021 | 170 | ICU | T0 | SOFA at day 3 |
| NA | NA |
| Lo Sasso et al. [25] | 2021 | retrospective observational | Italy | September–October 2020 | 110 | mixed population | hospitalization | Inhospital mortality |
| 0.95 | 1.73 nmol/L |
| Malinina et al. ** [15] | 2020 | retrospective observational | Russia | 37 | ICU | Bacterial superinfection |
| ||||
| Mendez et al. [26] | 2021 | longitudinal | Spain | March–June 2020 | 210 | ED | T0 | in-hospital mortality |
| NA | 1.16 |
| Minieri et al. [27] | 2021 | not specified | Italy | not specified | 321 | ED | ED-triage | overall in-hospital mortality |
| 0.85 | 1.105 |
| Montrucchio et al. [28] | 2021 | prospective observational | Italy | March–June 2020 | 57 | ICU | T0–1, T3, T7, T14 | ICU mortality—trend |
| 0.85 | >1.8 nmol/L * |
| Moore et al. [29] | 2022 | prospective | UK | April–June 2020 | 135 | ED | at the admission | 30-days mortality |
| 0.8441 | 1.54 |
| Oblitas et al. [19] | 2021 | prospective | Spain | August–November 2020 | 95 | ICU | once within 72 h of ICU admission | 30-day mortality and 30-day combined event |
| 0.73 and 0.72 | ≥1 |
| Popov et al. [30] | 2021 | prospective observational | Russia | 97 | mixed population | mortality |
| 0.75 | 0.895 nmol/L | ||
| Roedl et al. [16] | 2021 | observational | Germany | March–September 2020 | 64 | ICU | ICU admission | RRT versus no-RRT |
| 0.69 | |
| Simon et al. [18] | 2021 | prospective observational | Germany | March–April 2020 | 53 | ICU | Daily, T1–7 | ARDS, ECMO, MV, RRT |
| bio-ADM: 70 pg/mL * | |
| Sozio et al. [31] | 2021 | retrospective | Italy | March–May 2020 | 111 | mixed population | ED admission | severe disease |
| 0.85 | Mortality 0.895 nmol/L |
| Spoto et al. [32] | 2020 | prospective observational | Italy | April–June 2020 | 69 | mixed population | hospitalization | endothelial damage, MOF, severe disease |
| 0.78 | ARDS 3.04; mortality 2 nmol/L |
| Van Oers et al. [33] | 2021 | prospective | the Netherlands | March–May 2020 | 105 | ICU | on a daily basis, during the first 7 days | 28-day mortalit |
| 0.84 | 1.57 |
| Zaninotto et al. [34] | 2021 | retrospective | Italy | November | 135 | mixed population | 7 days | clinical outcomes |
| 0.900 | 1.50 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Montrucchio, G.; Balzani, E.; Lombardo, D.; Giaccone, A.; Vaninetti, A.; D’Antonio, G.; Rumbolo, F.; Mengozzi, G.; Brazzi, L. Proadrenomedullin in the Management of COVID-19 Critically Ill Patients in Intensive Care Unit: A Systematic Review and Meta-Analysis of Evidence and Uncertainties in Existing Literature. J. Clin. Med. 2022, 11, 4543. https://doi.org/10.3390/jcm11154543
Montrucchio G, Balzani E, Lombardo D, Giaccone A, Vaninetti A, D’Antonio G, Rumbolo F, Mengozzi G, Brazzi L. Proadrenomedullin in the Management of COVID-19 Critically Ill Patients in Intensive Care Unit: A Systematic Review and Meta-Analysis of Evidence and Uncertainties in Existing Literature. Journal of Clinical Medicine. 2022; 11(15):4543. https://doi.org/10.3390/jcm11154543
Chicago/Turabian StyleMontrucchio, Giorgia, Eleonora Balzani, Davide Lombardo, Alice Giaccone, Anna Vaninetti, Giulia D’Antonio, Francesca Rumbolo, Giulio Mengozzi, and Luca Brazzi. 2022. "Proadrenomedullin in the Management of COVID-19 Critically Ill Patients in Intensive Care Unit: A Systematic Review and Meta-Analysis of Evidence and Uncertainties in Existing Literature" Journal of Clinical Medicine 11, no. 15: 4543. https://doi.org/10.3390/jcm11154543
APA StyleMontrucchio, G., Balzani, E., Lombardo, D., Giaccone, A., Vaninetti, A., D’Antonio, G., Rumbolo, F., Mengozzi, G., & Brazzi, L. (2022). Proadrenomedullin in the Management of COVID-19 Critically Ill Patients in Intensive Care Unit: A Systematic Review and Meta-Analysis of Evidence and Uncertainties in Existing Literature. Journal of Clinical Medicine, 11(15), 4543. https://doi.org/10.3390/jcm11154543







