Diagnostic, Therapy and Complications in Acute Appendicitis of 19,749 Cases Based on Routine Data: A Retrospective Multicenter Observational Study
Abstract
:1. Introduction
2. Methods
2.1. CLINOTEL Hospital Association Germany
2.2. Patients and Data
2.3. Statistical Analysis
3. Results
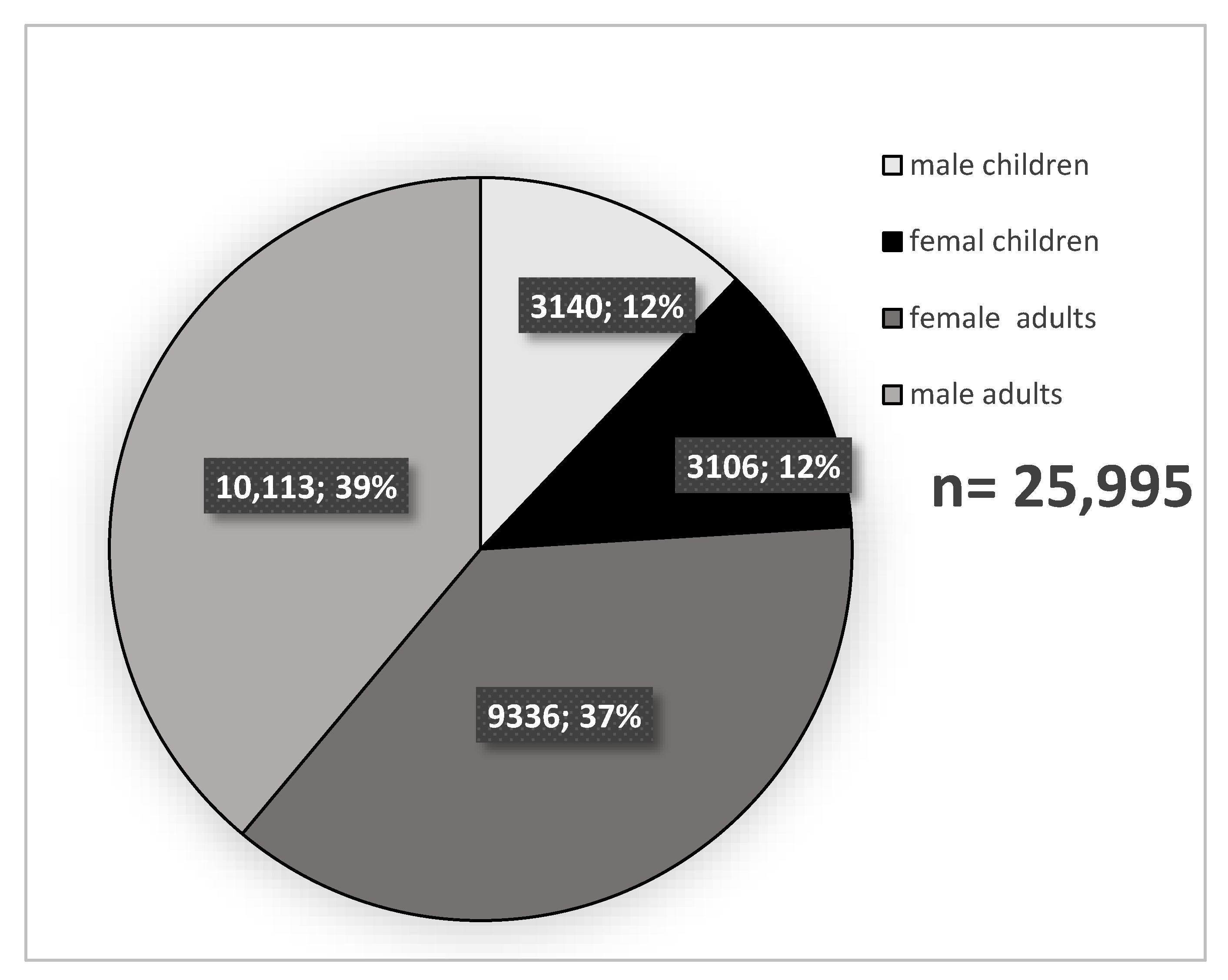
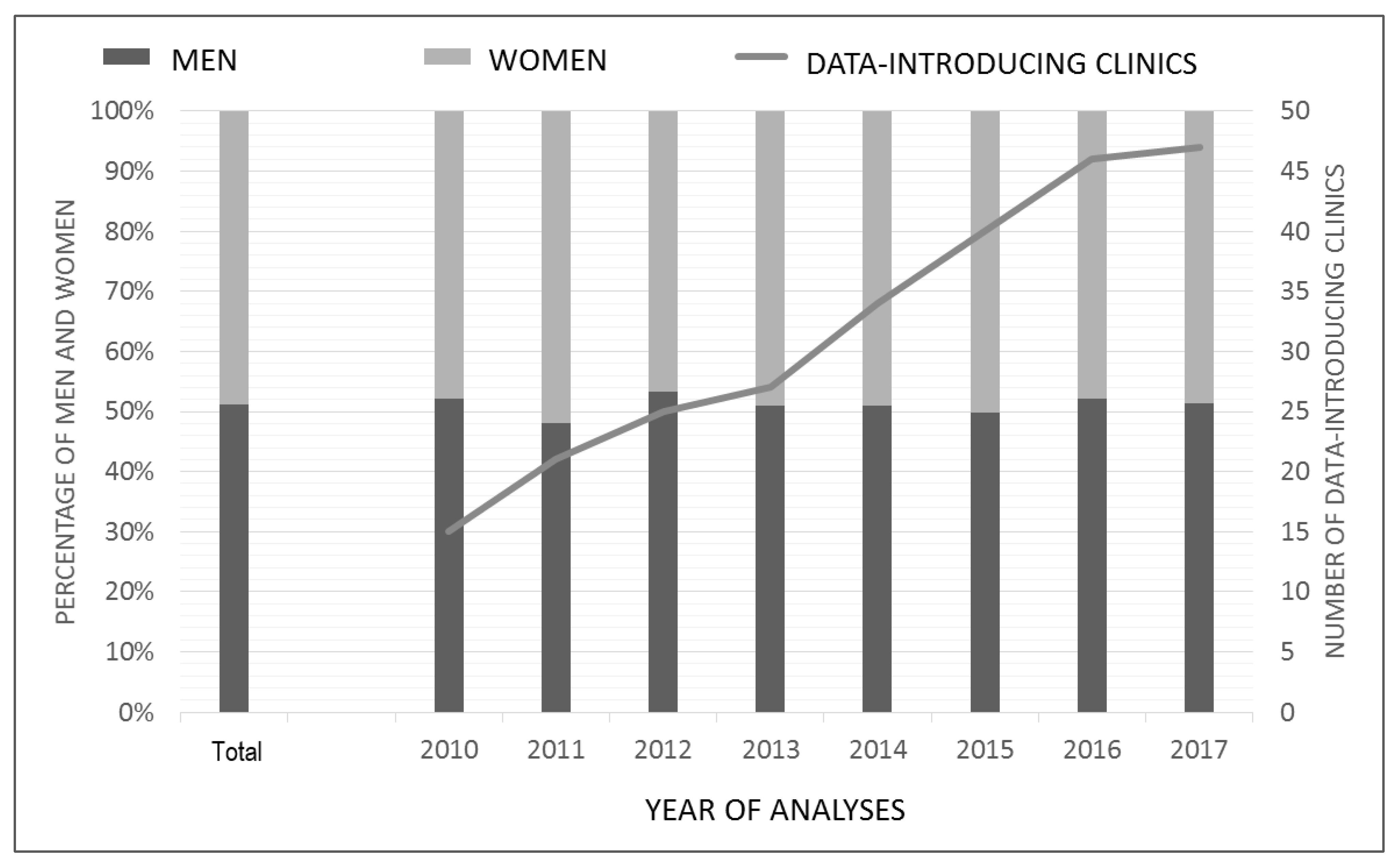
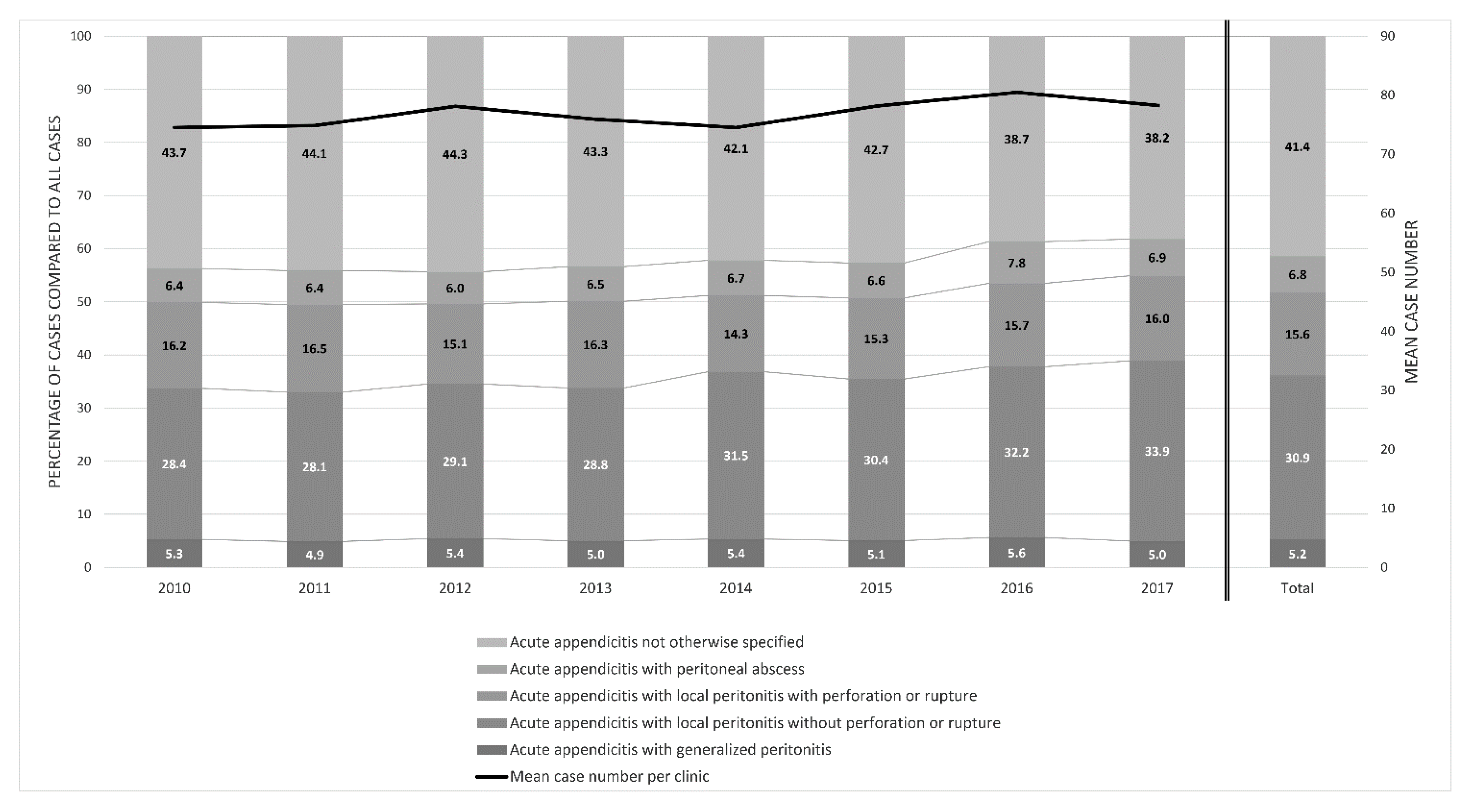
3.1. Study Population
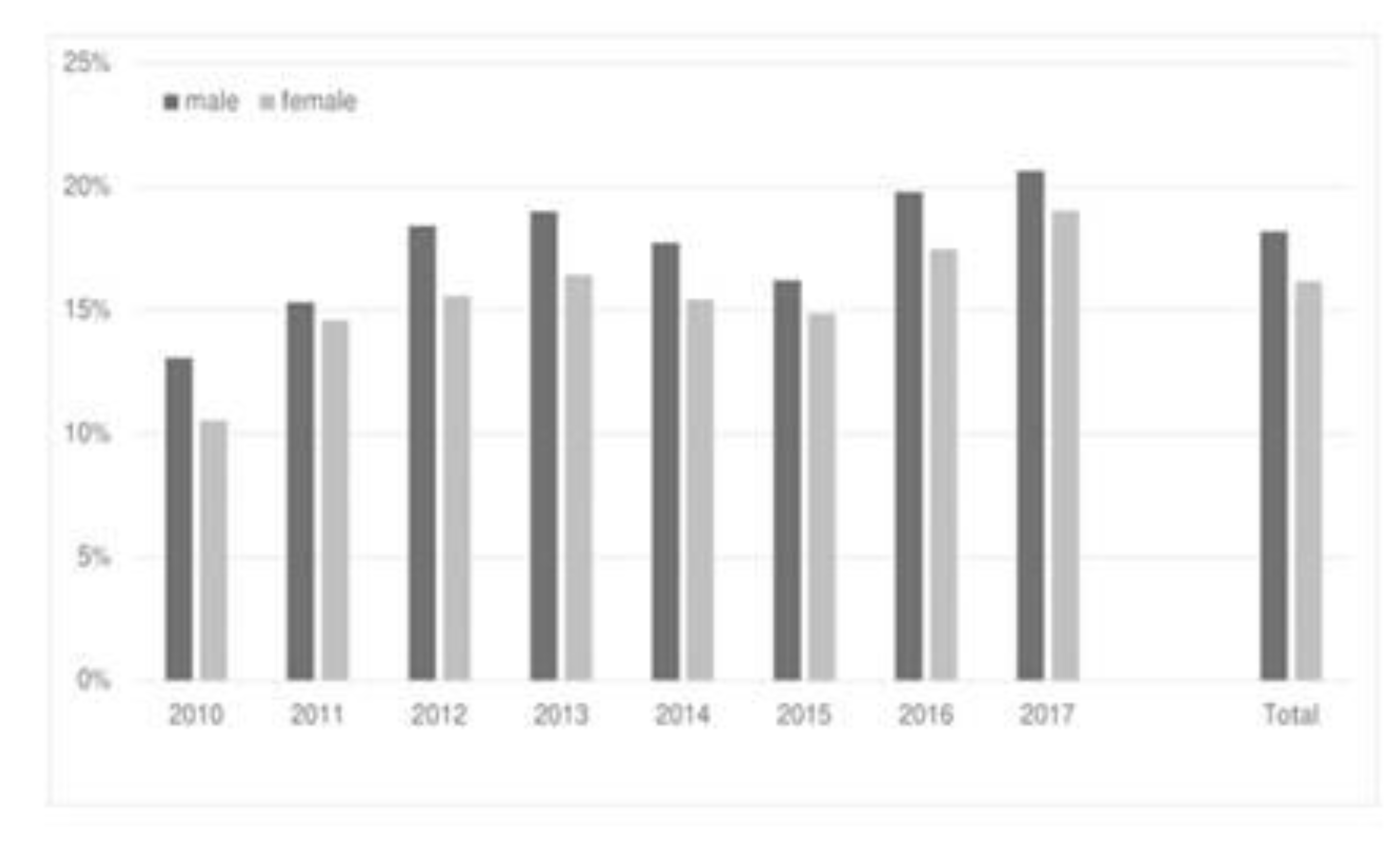
3.2. Diagnostic and Clinical Presentation
3.3. Therapy
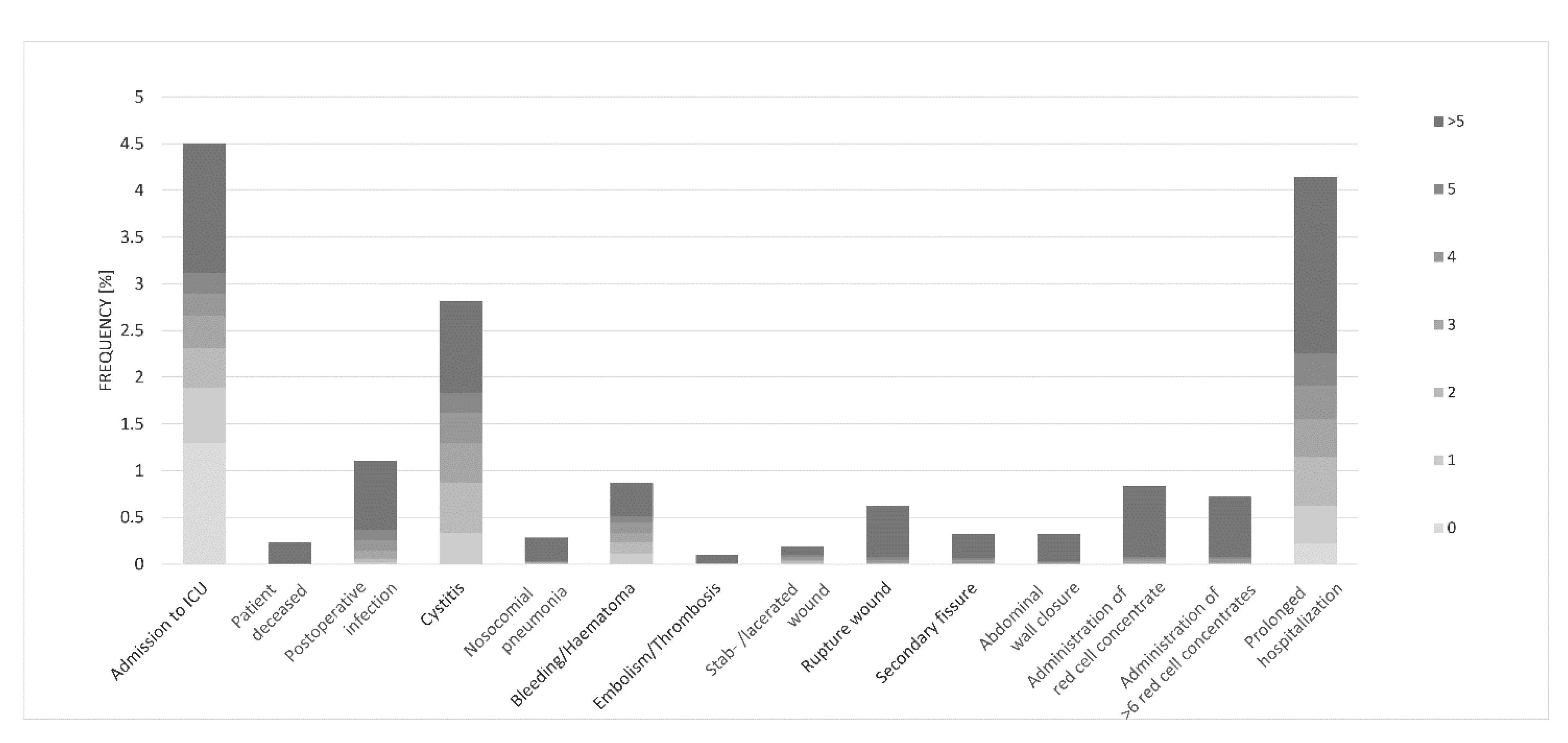
3.4. Complications
4. Discussion
4.1. Population and Diagnostic
4.2. Therapy and Complications
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Rolle, U.; Maneck, M. Versorgungstrends, regionale Variation und Qualität der Versorgung bei Appendektomien. Versorg. Rep. 2016, 10, 218–228. [Google Scholar]
- Jaschinski, T.; Christoph, G.; Mosch, M.; Eikermann, M.; Edmund, N.A.M.; Sauerland, S.; Cochrane Colorectal Cancer Group. Laparoscopic versus open surgery for suspected appendicitis. Cochrane Database Syst. Rev. 2018, 11. [Google Scholar] [CrossRef] [PubMed]
- Busch, M.; Gutzwiller, F.S.; Aellig, S.; Kuettel, R.; Metzger, U.; Zing, U. In-hospital delay increases the risk of perforation in adults with appendicitis. World J. Surg. 2011, 35, 1626–1633. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Harnoss, J.C.; Zelienka, I.; Probst, P.; Grummich, K.; Müller-Lantzsch, C.; Harnoss, J.M.; Ulrich, A.; Büchler, M.W.; Diener, M.K. Antibiotics Versus Surgical Therapy for Uncomplicated Appendicitis: Systematic Review and Meta-analysis of Controlled Trials (PROSPERO 2015: CRD42015016882). Ann. Surg. 2017, 265, 889–900. [Google Scholar] [CrossRef] [PubMed]
- Braun, M. Akute Appendizitis: Moderne Diagnostik und Therapie. HEABL 2016, 1, 17–22. [Google Scholar]
- Andert, A.; Alizai, H.P.; Klink, C.D.; Neitzke, N.; Fitzner, C.; Heidenhain, C.; Kroh, A.; Neumann, U.P.; Binnebösel, M. Risk factors for morbidity after appendectomy. Langenbecks Arch Surg. 2017, 402, 987–993. [Google Scholar] [CrossRef]
- Jaschinski, T.; Mosch, C.; Eikermann, M.; Neugebauer, E.A. Laparoscopic versus open appendectomy in patients with suspected appendicitis: A systematic review of meta-analyses of randomised controlled trials. BMC Gastroenterol. 2015, 15, 1–10. [Google Scholar] [CrossRef] [Green Version]
- Available online: https://www.dimdi.de/static/de/klassifikationen/icd/icd-10-gm/kode-suche/htmlgm2013/ (accessed on 14 April 2022).
- Available online: https://www.dimdi.de/static/de/klassifikationen/ops/kode-suche/opshtml2019/ (accessed on 14 April 2022).
- Agha, R.; Mathew, G.; STROCSS Group. STROCSS 2021 Guideline: Strengthening the reporting of cohort studies in surgery. Int. J. Surg. 2021, 96, 106–165. [Google Scholar]
- Téoule, P.; Laffolie, J.; Rolle, U.; Reissfelder, C. Acute Appendicitis in Childhood and Adulthood. Dtsch. Arztebl. Int. 2020, 117, 764–774. [Google Scholar]
- Hoffmann, J.C.; Trimborn, C.P.; Hoffmann, M.; Schröder, R.; Förster, S.; Dirks, K.; Tannapfel, A.; Anthuber, M.; Hollerweger, A. Classification of acute appendicitis (CAA): Treatment directed new classification based on imaging (ultrasound, computed tomography) and pathology. Int. J. Colorectal. Dis. 2021, 36, 2347–2360. [Google Scholar] [CrossRef]
- Sahm, M.; Pross, M.; Otto, R.; Koch, A.; Gastinger, I.; Lippert, H. Clinical Health Service Research on the Surgical Therapy of Acute Appendicitis: Comparison of Outcomes Based on 3 German Multicenter Quality Assurance Studies Over 21 Years. Ann. Surg. 2015, 262, 338–346. [Google Scholar] [CrossRef] [PubMed]
- Kotaluoto, S.; Ukkonen, M.L.; Pauniaho, S.; Helminen, M.; Sand, J.; Rantanen, T. Mortality Related to Appendectomy; a Population Based Analysis over Two Decades in Finland. World J. Surg. 2017, 41, 64–69. [Google Scholar] [CrossRef] [PubMed]
- Blomqvist, P.; Ljung, H.; Nyrén, O.; Ekbom, A. Appendectomy in Sweden 1989-1993 assessed by the Inpatient Registry. J. Clin. Epidemiol. 1998, 51, 859–865. [Google Scholar] [CrossRef]
- Sartelli, M.; Baiocchi, G.L.; Di Saverio, S.; Ferrara, F.; Labricciosa, F.M.; Ansaloni, L.; Catena, F. Prospective Observational Study on acute Appendicitis Worldwide (POSAW). World J. Emerg. Surg. 2018, 16, 13. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Andersson, R.E. Short and long-term mortality after appendectomy in Sweden 1987 to 2006, Influence of appendectomy diagnosis, sex, age, co-morbidity, surgical method, hospital volume, and time period. A national population-based cohort study. World J. Surg. 2013, 37, 974–981. [Google Scholar] [CrossRef]
- Oguntola, A.S.; Adeoti, M.L.; Oyemolade, T.A. Appendicitis: Trends in incidence, age, sex, and seasonal variations in South-Western Nigeria. Ann. Afr. Med. 2010, 9, 213–217. [Google Scholar] [CrossRef] [Green Version]
- Noudeh, N.; Sadigh, Y.J.; Ahmadnia, A.Y. Epidemiologic features, seasonal variations and false positive rate of acute appendicitis in Shahr-e-Rey, Tehran. Int. J. Surg. 2007, 5, 95–98. [Google Scholar] [CrossRef] [Green Version]
- Gorter, R.R.; Eker, H.H.; Gorter-Stam, M.A.; Abis, G.S.; Acharya, A.; Ankersmit, M.; Bonjer, J. Diagnosis and management of acute appendicitis. EAES consensus development conference 2015. Surg. Endosc. 2016, 30, 4668–4690. [Google Scholar] [CrossRef] [Green Version]
- Yun, S.J.; Ryu, C.W.; Choi, N.Y.; Kim, H.C.; Oh, J.Y.; Yang, D.M. Comparison of Low- and Standard-Dose CT for the Diagnosis of Acute Appendicitis: A Meta-Analysis. AJR Am. J. Roentgenol. 2017, 208, 198–207. [Google Scholar] [CrossRef]
- Nelson, D.W.; Causey, M.W.; Porta, C.R.; McVay, D.P.; Carnes, A.M.; Johnson, E.K.; Steele, S.R. Examining the relevance of the physician’s clinical assessment and the reliance on computed tomography in diagnosing acute appendicitis. Am. J. Surg. 2013, 205, 452–456. [Google Scholar] [CrossRef]
- Duda, J.B.; Lynch, M.L.; Bhatt, S.; Dogra, V.S. Computed tomography mimics of acute appendicitis: Predictors of appendiceal disease confirmed at pathology. J. Clin. Imaging. Sci. 2012, 2, 73. [Google Scholar] [CrossRef] [PubMed]
- Rud, B.; Olafsson, L.; Vejborg, T.S.; Wilhelmsen, M.; Reitsma, J.B.; Rappeport, E.D.; Wille-Jørgensen, P. Diagnostic accuracy of computed tomography for appendicitis in adults. Cochrane Database Syst. Rev. 2019, 7, 19. [Google Scholar] [CrossRef]
- Leite, N.P.; Pereira, J.M.; Cunha, R.; Pinto, P.; Sirlin, C. CT evaluation of appendicitis and its complications: Imaging techniques and key diagnostic findings. AJR Am. J. Roentgenol. 2005, 185, 406–417. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.J.; Jeon, B.G.; Hong, C.K.; Kwon, K.W.; Han, S.B.; Paik, S.; Kang, G.H. Low-dose CT for the diagnosis of appendicitis in adolescents and young adults (LOCAT): A pragmatic, multicenter, randomized controlled non-inferiority trial. Lancet Gastroenterol. Hepatol. 2017, 2, 793–804. [Google Scholar] [CrossRef]
- Gaskill, C.E.; Simianu, V.V.; Carnell, J.; Hippe, D.S.; Bhargava, P.; Flum, D.R.; Davidson, G.H. Use of computed tomography to determine perforation in patients with acute appendicitis. Curr. Prob. Diagnostic Radiol. 2018, 47, 6–9. [Google Scholar] [CrossRef]
- Garcia, E.M.; Camacho, M.A.; Karolyi, D.R.; Kim, D.H.; Cash, B.D.; Chang, K.J.; Carucci, L.R. ACR Appropriateness Criteria® Right Lower Quadrant Pain-Suspected Appendicitis. J. Am. Coll. Radiol. 2018, 15, 373–387. [Google Scholar] [CrossRef] [Green Version]
- Kundiona, I.; Chihaka, O.B.; Muguti, G.I. Negative appendectomy: Evaluation of ultrasonography and Alvarado score. Cent Afr. J. Med. 2015, 61, 66–73. [Google Scholar]
- Bretagnol, F.; Zappa, M.; Panis, Y. Ultrasound and CT imaging in the diagnosis of acute appendicitis. J. Chir. 2009, 1, 8–11. [Google Scholar] [CrossRef] [PubMed]
- Schildberg, C.W.; Skibbe, J.; Croner, R.; Schellerer, V.; Hohenberger, W.; Horbach, T. Rational diagnostics of acute abdomen. Chirurg 2010, 81, 1013–1019. [Google Scholar] [CrossRef] [PubMed]
- Hoffmann, M.; Anthuber, M. Rational diagnostics of acute appendicitis. Chirurg 2019, 90, 173–177. [Google Scholar] [CrossRef]
- Sahm, M.; Pross, M.; Lippert, H. Acute appendicitis-changes in epidemiology, diagnosis and therapy. Zentralbl. Chir. 2011, 36, 18–24. [Google Scholar] [CrossRef] [PubMed]
- Khan, M.A.B.; Abu-Zidan, F.M. Point-of-care ultrasound for the acute abdomen in the primary health care. Turk J. Emerg. Med. 2020, 20, 1–11. [Google Scholar] [PubMed]
- Andric, M.; Kalff, J.C.; Schwenk, W.; Farkas, S.; Hartwig, W.; Türler, A.; Croner, R. Recommendations on treatment of acute appendicitis: Recommendations of an expert group based on the current literature. Chirurg 2020, 9, 700–711. [Google Scholar] [CrossRef] [PubMed]
- Lapsa, S.; Ozolins, A.; Strumfa, I.; Gardovskis, J. Acute Appendicitis in the Elderly: A Literature Review on an Increasingly Frequent Surgical Problem. Geriatrics 2021, 6, 93. [Google Scholar] [CrossRef] [PubMed]
- Yeh, D.D.; Eid, A.I.; Young, K.A.; Wild, J.; Kaafarani, H.M.A.; Ray-Zack, M.; Kana’an, T.; Lawless, R.; Cralley, A.L.; Crandall, M. EAST Appendicitis Study Group. Multicenter Study of the Treatment of Appendicitis in America: Acute, Perforated, and Gangrenous (MUSTANG), an EAST Multicenter Study. Ann. Surg. 2021, 273, 548–556. [Google Scholar] [CrossRef] [PubMed]
- Mowbray, N.G.; Hurt, L.; Powell-Chandler, A.; Reeves, N.; Chandler, S.; Walters, E.; Cornish, J. Where have all the appendectomies gone? Ann. R Coll. Surg. Engl. 2021, 103, 250–254. [Google Scholar] [CrossRef]
- Kabir, S.A.; Kabir, S.I.; Sun, R.; Jafferbhoy, S.; Karim, A. How to diagnose an acutely inflamed appendix; a systematic review of the latest evidence. Int. J. Surg. 2017, 40, 155–162. [Google Scholar] [CrossRef] [PubMed]
- Di Saverio, S.; Podda, M.; De Simoneet, B.; Ceresoli, M.; Augustin, G.; Gori, A.; Catena, F. Diagnosis and treatment of acute appendicitis: 2020 update of the WSES Jerusalem Guidelines. World J. Emerg. Surg. 2020, 15, 27. [Google Scholar] [CrossRef]
- Park, J.H.; Salminen, P.; Tannaphai, P.; Lee, K.H. Low-Dose Abdominal CT for Evaluating Suspected Appendicitis in Adolescents and Young Adults: Review of Evidence. Korean J. Radiol. 2022, ahead of print.
- D’Souza, N.; Hicks, G.; Beable, R.; Higginson, A.; Rud, B. Magnetic resonance imaging (MRI) for diagnosis of acute appendicitis. Cochrane Database Syst. Rev. 2021, 12. [Google Scholar] [CrossRef]
- MERCY Study Collaborating Group. Predictors of surgical outcomes of minimally invasive right colectomy: The MERCY study. Int. J. Colorectal. Dis. 2022, 37, 907–918. [Google Scholar] [CrossRef]
- van Dongen, J.C.; van der Geest, L.G.M.; de Meijer, V.E.; van Santvoort, H.C.; de Vos-Geelen, J.; Besselink, M.G.; Groot Koerkamp, B.; Wilmink, J.W.; van Eijck, C.H.J. Dutch Pancreatic Cancer Group. Age and prognosis in patients with pancreatic cancer: A population-based study. Acta Oncol. 2022, 61, 286–293. [Google Scholar] [CrossRef] [PubMed]
- Dumas, R.P.; Subramanian, M.; Hodgman, E.; Arevalo, M.; Nguyen, G.; Li, K.; Aijwe, T.; Williams, B.; Eastman, A.; Luk, S.; et al. Laparoscopic Appendectomy: A Report on 1164 Operations at a Single-Institution, Safety-Net Hospital. Am. Surg. 2018, 84, 1110–1116. [Google Scholar] [CrossRef] [PubMed]
- Minutolo, V.; Licciardello, A.; Di Stefano, B.; Arena, M.; Arena, G.; Antonacci, V. Outcomes and cost analysis of laparoscopic versus open appendectomy for treatment of acute appendicitis: 4-years’ experience in a district hospital. BMC Surg. 2014, 14, 14. [Google Scholar] [CrossRef] [Green Version]
- Balogun, O.S.; Osinowo, A.; Afolayan, M.; Olajide, T.; Lawal, A.; Adesanyam, A. Acute perforated appendicitis in adults: Management and complications in Lagos, Nigeria. Ann. Afr. Med. 2019, 18, 36–41. [Google Scholar] [CrossRef]
- Wei, B.; Qi, C.L.; Chen, T.F.; Zheng, Z.H.; Huang, J.L.; Hu, B.G.; Wie, H.B. Laparoscopic versus open appendectomy for acute appendicitis: A metaanalysis. Surg. Endosc. 2011, 25, 1199–1208. [Google Scholar] [CrossRef]
- Ohtani, H.; Tamamori, Y.; Arimoto, Y.; Nishiguchi, Y.; Maeda, K.; Hirakawa, K. Meta-analysis of the results of randomized controlled trials that compared laparoscopic and open surgery for acute appendicitis. J. Gastrointest. Surg. 2012, 16, 1929–1939. [Google Scholar] [CrossRef]
- Woodham, B.L.; Cox, M.R.; Eslick, G.D. Evidence to support the use of laparoscopic over open appendectomy for obese individuals: A meta-analysis. Surg. Endosc. 2012, 26, 2566–2570. [Google Scholar] [CrossRef] [PubMed]
- Liu, Z.; Zhang, P.; Ma, Y.; Chen, H.; Zhou, Y.; Zhang, M.; Qin, H. Laparoscopy or not: A meta-analysis of the surgical effects of laparoscopic versus open appendectomy. Surg. Laparosc. Endosc. Percutan. Tech. 2010, 20, 362–370. [Google Scholar] [CrossRef]
- Bennet, J.; Boddy, A.; Rhodes, M. Choice of approach for appendectomy: A meta-analysis of open versus laparoscopic appendectomy. Surg. Laparosc. Endosc. Percutan. Tech. 2007, 17, 245–255. [Google Scholar] [CrossRef]
- Li, X.; Zhang, J.; Sang, L.; Zhang, W.; Chu, Z.; Li, X.; Liu, Y. Laparoscopic versus conventional appendectomy—A meta-analysis of randomized controlled trials. BMC Gastroenterol. 2010, 3, 129. [Google Scholar] [CrossRef] [Green Version]
- Ferris, M.; Quan, S.; Kaplan, B.S.; Molodecky, N.; Ball, C.G.; Chernoff, G.W.; Bhala, N.; Ghosh, S.; Dixon, E.; Ng, S.; et al. The Global Incidence of Appendicitis: A Systematic Review of Population-based Studies. Ann. Surg. 2017, 266, 237–241. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- van Rossem, C.C.; Bolmers, M.D.; Schreinemacher, M.H.; van Geloven, A.A.; Bemelman, W.A. Snapshot Appendicitis Collaborative Study Group. Prospective nationwide outcome audit of surgery for suspected acute appendicitis. Br. J. Surg. 2016, 103, 144–151. [Google Scholar] [CrossRef] [PubMed]
- Gurrado, A.; Faillace, G.; Bottero, L.; Frola, C.; Stefanini, P.; Piccinni, G.; Longoni, M. Laparoscopic appendectomies: Experience of a surgical unit. Minim. Invasive Ther. Allied. Techno. 2009, 18, 242–247. [Google Scholar] [CrossRef] [PubMed]
- Andersson, R.E. Short-term complications and long-term morbidity of laparoscopic and open appendectomy in a national cohort. Br. J. Surg. 2014, 101, 1135–1142. [Google Scholar] [CrossRef] [PubMed]
- Calis, H. Morbidity and Mortality in Appendicitis in the Elderly. J. Coll. Phys. Surg. Pak. 2018, 28, 875–878. [Google Scholar] [CrossRef]
- Weinandt, M.; Godiris-Petit, G.; Menegaux, F.; Chereau, N.; Lupinacci, R.M. Appendicitis is a Severe Disease in Elderly Patients: A Twenty-Year Audit. JSLS 2020, 24, e2020. [Google Scholar] [CrossRef]
- Masoomi, H.; Mills, S.; Dolich, M.O.; Ketana, N.; Carmichael, J.C.; Nguyen, N.T.; Stamos, M.J. Does laparoscopic appendectomy impart an advantage over open appendectomy in elderly patients? World J. Surg. 2012, 36, 1534–1539. [Google Scholar] [CrossRef]



| Age | n | % |
|---|---|---|
| 18–29 | 8270 | 41.9 |
| 30–39 | 3292 | 16.7 |
| 40–49 | 2655 | 13.4 |
| 50–59 | 2564 | 13 |
| 60–69 | 1474 | 7.5 |
| 70–79 | 1053 | 5.3 |
| 80–89 | 400 | 2 |
| 90–99 | 41 | 0.2 |
| 19,749 | 100 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Schildberg, C.W.; Reissig, K.; Hunger, R.; Paasch, C.; Stillger, R.; Mantke, R. Diagnostic, Therapy and Complications in Acute Appendicitis of 19,749 Cases Based on Routine Data: A Retrospective Multicenter Observational Study. J. Clin. Med. 2022, 11, 4495. https://doi.org/10.3390/jcm11154495
Schildberg CW, Reissig K, Hunger R, Paasch C, Stillger R, Mantke R. Diagnostic, Therapy and Complications in Acute Appendicitis of 19,749 Cases Based on Routine Data: A Retrospective Multicenter Observational Study. Journal of Clinical Medicine. 2022; 11(15):4495. https://doi.org/10.3390/jcm11154495
Chicago/Turabian StyleSchildberg, Claus W., Kathrin Reissig, Richard Hunger, Christoph Paasch, Rosi Stillger, and René Mantke. 2022. "Diagnostic, Therapy and Complications in Acute Appendicitis of 19,749 Cases Based on Routine Data: A Retrospective Multicenter Observational Study" Journal of Clinical Medicine 11, no. 15: 4495. https://doi.org/10.3390/jcm11154495
APA StyleSchildberg, C. W., Reissig, K., Hunger, R., Paasch, C., Stillger, R., & Mantke, R. (2022). Diagnostic, Therapy and Complications in Acute Appendicitis of 19,749 Cases Based on Routine Data: A Retrospective Multicenter Observational Study. Journal of Clinical Medicine, 11(15), 4495. https://doi.org/10.3390/jcm11154495





