Factors Associated with Traumatic Diaphragmatic Rupture among Patients with Chest or Abdominal Injury: A Nationwide Study from Japan
Abstract
:1. Introduction
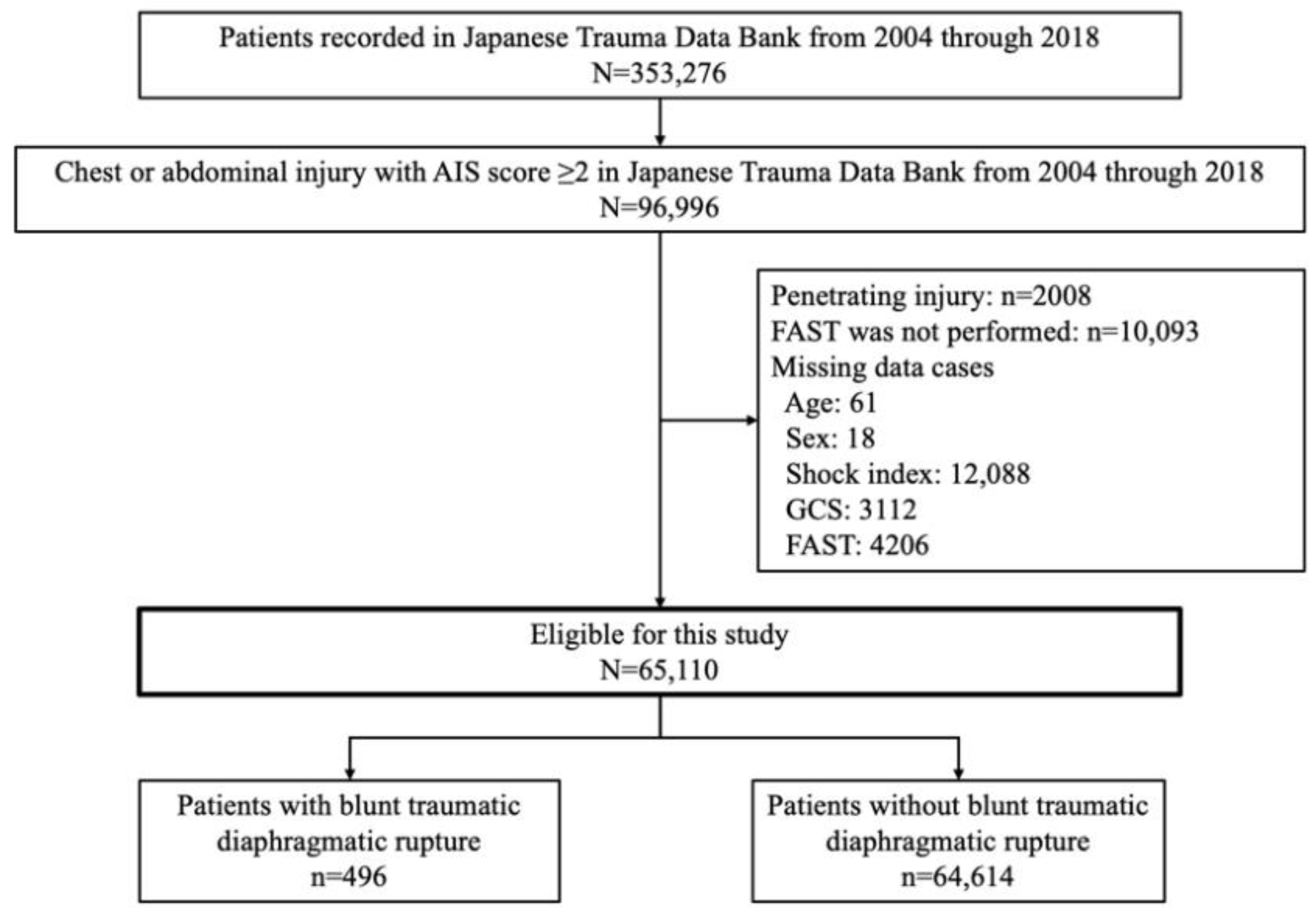
2. Materials and Methods
2.1. Study Design and Settings
2.2. Japanese Trauma Data Bank
2.3. Main Outcome
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Meyers, B.F.; McCabe, C.J. Traumatic diaphragmatic hernia. Occult marker of serious injury. Ann. Surg. 1993, 218, 783–790. [Google Scholar] [CrossRef]
- Haciibrahimoglu, G.; Solak, O.; Olcmen, A.; Bedirhan, M.A.; Solmazer, N.; Gurses, A. Management of traumatic diaphragmatic rupture. Surg. Today 2004, 34, 111–114. [Google Scholar] [CrossRef]
- Stewart, R.M.; Myers, J.G.; Dent, D.L.; Ermis, P.; Gray, G.A.; Villarreal, R.; Blow, O.; Woods, B.; McFarland, M.; Garavaglia, J.; et al. Seven hundred fifty-three consecutive deaths in a level I trauma center: The argument for injury prevention. J. Trauma 2003, 54, 66–70. [Google Scholar] [CrossRef]
- Zarour, A.M.; El-Menyar, A.; Al-Thani, H.; Scalea, T.M.; Chiu, W.C. Presentations and outcomes in patients with traumatic diaphragmatic injury: A 15-year experience. J. Trauma Acute Care Surg. 2013, 74, 1392–1398. [Google Scholar] [CrossRef] [PubMed]
- Fair, K.A.; Gordon, N.T.; Barbosa, R.R.; Rowell, S.E.; Watters, J.M.; Schreiber, M.A. Traumatic diaphragmatic injury in the American College of Surgeons National Trauma Data Bank: A new examination of a rare diagnosis. Am. J. Surg. 2015, 209, 864–868. [Google Scholar] [CrossRef] [PubMed]
- Shah, R.; Sabanathan, S.; Mearns, A.J.; Choudhury, A.K. Traumatic rupture of diaphragm. Ann. Thorac. Surg. 1995, 60, 1444–1449. [Google Scholar] [CrossRef]
- Japan Trauma Care and Research. Japan Trauma Data Bank Annual Report 2013–2017. 2018. Available online: https://www.jtcr-jatec.org/traumabank/dataroom/data/JTDB2018e.pdf (accessed on 22 June 2022).
- Reiff, D.A.; McGwin, G., Jr.; Metzger, J.; Windham, S.T.; Doss, M.; Rue, L.W., 3rd. Identifying injuries and motor vehicle collision characteristics that together are suggestive of diaphragmatic rupture. J. Trauma 2002, 53, 1139–1145. [Google Scholar] [CrossRef]
- Von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P.; STROBE Initiative. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. Lancet 2007, 370, 1453–1457. [Google Scholar] [CrossRef]
- Katayama, Y.; Kitamura, T.; Hirose, T.; Kiguchi, T.; Matsuyama, T.; Takahashi, H.; Kiyohara, K.; Sado, J.; Adachi, S.; Noda, T.; et al. Pelvic angiography is effective for emergency pediatric patients with pelvic fractures: A propensity-score-matching study with a nationwide trauma registry in Japan. Eur. J. Trauma Emerg. Surg. 2021, 47, 515–521. [Google Scholar] [CrossRef] [Green Version]
- Japan Trauma Care and Research. JTDB Annual Report 2021. Available online: https://www.jtcr-jatec.org/traumabank/dataroom/data/JTDB2021e.pdf (accessed on 22 June 2022).
- Nakada, T.A.; Nakao, S.; Mizushima, Y.; Matsuoka, T. Association between male sex and increased mortality after falls. Acad. Emerg. Med. 2015, 22, 708–713. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lim, K.H.; Park, J. Blunt traumatic diaphragmatic rupture: Single-center experience with 38 patients. Medicine 2018, 97, e12849. [Google Scholar] [CrossRef] [PubMed]
- Abe, T.; Takahashi, O.; Saitoh, D.; Tokuda, Y. Association between helicopter with physician versus ground emergency medical services and survival of adults with major trauma in Japan. Crit. Care 2014, 18, R146. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Characteristic | Total | Blunt TDR (+) | Blunt TDR (−) | |||
|---|---|---|---|---|---|---|
| (n = 65,110) | (n = 496) | (n = 64,614) | ||||
| Age, years, median (IQR) | 54 | (33–70) | 58 | (40–71) | 54 | (32–70) |
| Age group, years, n (%) | ||||||
| 0–14 | 2704 | (4.2) | 6 | (1.2) | 2698 | (4.2) |
| 15–29 | 11,708 | (18.0) | 12 | (12.3) | 11,647 | (18.0) |
| 30–44 | 10,686 | (16.4) | 83 | (16.7) | 10,603 | (16.4) |
| 45–59 | 12,672 | (19.5) | 110 | (22.2) | 12,562 | (19.4) |
| 60–74 | 15,922 | (24.5) | 145 | (29.2) | 15,777 | (24.4) |
| ≥75 | 11,418 | (17.5) | 91 | (18.3) | 11,327 | (17.5) |
| Male, n (%) | 46,586 | (71.5) | 323 | (65.1) | 46,263 | (71.6) |
| Disturbance of consciousness (GCS < 8), n (%) | 9708 | (14.9) | 151 | (30.4) | 9557 | (14.8) |
| Shock, n (%) | 53,173 | (81.7) | 279 | (56.3) | 52,894 | (81.9) |
| FAST positive, n (%) | 12,213 | (18.8) | 193 | (38.9) | 12,020 | (18.6) |
| Mechanism of injury, n (%) | ||||||
| Traffic accident | ||||||
| Car driver | 10,913 | (16.8) | 94 | (19.0) | 10,819 | (16.8) |
| Front seat passenger | 2304 | (3.5) | 31 | (6.3) | 2304 | (3.5) |
| Back seat passenger | 1367 | (2.1) | 16 | (3.2) | 1351 | (2.1) |
| Motorcycle rider | 11,235 | (17.3) | 79 | (15.9) | 11,156 | (17.3) |
| Pillion passenger | 383 | (0.6) | 0 | (0) | 383 | (0.6) |
| Cyclist | 5131 | (7.9) | 31 | (6.3) | 5100 | (7.9) |
| Pedestrian | 7224 | (11.1) | 94 | (19.0) | 7130 | (11.1) |
| Injury from height | 10,024 | (15.4) | 54 | (10.9) | 9970 | (15.4) |
| Fall injury from stairs, etc. | 6968 | (10.7) | 15 | (3.0) | 6953 | (10.7) |
| Falling down injury | 2544 | (3.9) | 12 | (2.4) | 2532 | (3.9) |
| Compression injury by press machine | 75 | (0.1) | 1 | (0.2) | 74 | (0.1) |
| Compression injury by heavy object | 1332 | (2.0) | 20 | (4.0) | 1312 | (2.0) |
| Injury by falling or flying object | 510 | (0.8) | 4 | (0.8) | 506 | (0.8) |
| Others | 5100 | (7.8) | 45 | (9.1) | 5055 | (7.8) |
| Chest AIS, n (%) | ||||||
| 1 | 851 | (1.3) | 0 | (0) | 851 | (1.3) |
| 2 | 6149 | (9.4) | 12 | (2.4) | 6137 | (9.5) |
| 3 | 25,625 | (39.4) | 85 | (17.1) | 25,540 | (39.5) |
| 4 | 20,102 | (30.9) | 337 | (67.9) | 20 | (30.6) |
| 5 | 3636 | (5.6) | 59 | (11.9) | 3577 | (5.5) |
| 6 | 149 | (0.2) | 3 | (0.6) | 146 | (0.2) |
| None/unknown | 8598 | (13.2) | 0 | (0) | 8598 | (13.3) |
| Abdominal AIS, n (%) | ||||||
| 1 | 1076 | (1.7) | 14 | (2.8) | 1062 | (1.6) |
| 2 | 9280 | (14.3) | 108 | (21.8) | 9172 | (14.2) |
| 3 | 8299 | (12.7) | 92 | (18.5) | 8207 | (12.7) |
| 4 | 3493 | (5.4) | 71 | (14.3) | 3422 | (5.3) |
| 5 | 741 | (1.1) | 30 | (6.0) | 711 | (1.1) |
| 6 | 21 | (0.0) | 1 | (0.2) | 20 | (0.0) |
| None/unknown | 42,200 | (64.8) | 180 | (36.3) | 42,020 | (65.0) |
| ISS, median (IQR) | 21 | (14–29) | 32 | (24–41) | 21 | (14–29) |
| In-hospital mortality, n (%) | 6823 | (10.9) | 122 | (26.2) | 6701 | (10.7) |
| Proportion % (n/N) | Adjusted OR (95% CI) | p Value | |||
|---|---|---|---|---|---|
| Age group, years | |||||
| 0–14 | 0.2 | (6/2704) | 0.307 | (0.132–0.715) | 0.006 |
| 15–29 | 0.5 | (61/11,708) | 0.668 | (0.476–0.936) | 0.019 |
| 30–44 | 0.8 | (83/10,686) | Reference | ||
| 45–59 | 0.9 | (110/12,672) | 1.212 | (0.905–1.623) | 0.197 |
| 60–74 | 0.9 | (145/15,922) | 1.258 | (0.950–1.666) | 0.110 |
| ≥75 | 0.8 | (91/11,418) | 0.989 | (0.720–1.358) | 0.944 |
| Sex | |||||
| Male | 0.7 | (323/46,586) | Reference | ||
| Female | 0.9 | (173/18,524) | 1.177 | (0.961–1.442) | 0.115 |
| Disturbance of consciousness | |||||
| GCS < 8 | 1.6 | (151/9708) | 1.362 | (1.099–1.686) | 0.005 |
| GCS ≥ 8 | 0.6 | (345/55,402) | Reference | ||
| Shock | |||||
| Shock (+) | 0.5 | (279/53,173) | 0.630 | (0.512–0.776) | <0.001 |
| Shock (−) | 1.8 | (217/11,937) | Reference | ||
| FAST | |||||
| Positive | 1.6 | (193/12,213) | 1.233 | (0.994–1.529) | 0.057 |
| Negative | 0.6 | (303/52,897) | Reference | ||
| Chest AIS (every one score up) | 2.079 | (1.896–2.278) | <0.001 | ||
| Abdominal AIS (every one score up) | 1.520 | (1.431–1.615) | <0.001 | ||
| Mechanism of injury | |||||
| Traffic accident | |||||
| Car driver | 0.9 | (94/10,913) | 1.184 | (0.869–1.615) | 0.285 |
| Front seat passenger | 1.3 | (31/2304) | 1.728 | (1.107–2.698) | 0.016 |
| Back seat passenger | 1.2 | (16/1367) | 1.476 | (0.840–2.593) | 0.176 |
| Motorcycle rider | 0.7 | (79/11,235) | Reference | ||
| Pillion passenger | 0.0 | (0/383) | - | - | - |
| Cyclist | 0.6 | (31/5131) | 1.355 | (0.974–1.885) | 0.071 |
| Pedestrian | 1.3 | (94/7224) | 0.955 | (0.620–1.470) | 0.835 |
| Injury from height | 0.5 | (54/10,024) | 0.590 | (0.413–0.842) | 0.004 |
| Fall injury from stairs, etc. | 0.2 | (15/6968) | 0.401 | (0.228–0.705) | 0.002 |
| Falling down injury | 0.5 | (12/2544) | 1.055 | (0.563–1.975) | 0.868 |
| Compression injury by press machine | 1.3 | (1/75) | 2.084 | (0.282–15.419) | 0.472 |
| Compression injury by heavy object | 1.5 | (20/1332) | 1.626 | (0.978–2.702) | 0.061 |
| Injury by falling or flying object | 0.8 | (4/510) | 0.935 | (0.336–2.606) | 0.898 |
| Others | 0.9 | (45/5100) | 1.193 | (0.819–1.737) | 0.358 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Katayama, Y.; Tanaka, K.; Ishida, K.; Hirose, T.; Tachino, J.; Nakao, S.; Umemura, Y.; Kiyohara, K.; Ojima, M.; Kiguchi, T.; et al. Factors Associated with Traumatic Diaphragmatic Rupture among Patients with Chest or Abdominal Injury: A Nationwide Study from Japan. J. Clin. Med. 2022, 11, 4462. https://doi.org/10.3390/jcm11154462
Katayama Y, Tanaka K, Ishida K, Hirose T, Tachino J, Nakao S, Umemura Y, Kiyohara K, Ojima M, Kiguchi T, et al. Factors Associated with Traumatic Diaphragmatic Rupture among Patients with Chest or Abdominal Injury: A Nationwide Study from Japan. Journal of Clinical Medicine. 2022; 11(15):4462. https://doi.org/10.3390/jcm11154462
Chicago/Turabian StyleKatayama, Yusuke, Kenta Tanaka, Kenichiro Ishida, Tomoya Hirose, Jotaro Tachino, Shunichiro Nakao, Yutaka Umemura, Kosuke Kiyohara, Masahiro Ojima, Takeyuki Kiguchi, and et al. 2022. "Factors Associated with Traumatic Diaphragmatic Rupture among Patients with Chest or Abdominal Injury: A Nationwide Study from Japan" Journal of Clinical Medicine 11, no. 15: 4462. https://doi.org/10.3390/jcm11154462
APA StyleKatayama, Y., Tanaka, K., Ishida, K., Hirose, T., Tachino, J., Nakao, S., Umemura, Y., Kiyohara, K., Ojima, M., Kiguchi, T., Kitamura, T., & Oda, J. (2022). Factors Associated with Traumatic Diaphragmatic Rupture among Patients with Chest or Abdominal Injury: A Nationwide Study from Japan. Journal of Clinical Medicine, 11(15), 4462. https://doi.org/10.3390/jcm11154462







