Effect of Fetoscopic Laser Photocoagulation on Fetal Growth and Placental Perfusion in Twin–Twin Transfusion Syndrome
Abstract
1. Introduction
2. Materials and Methods
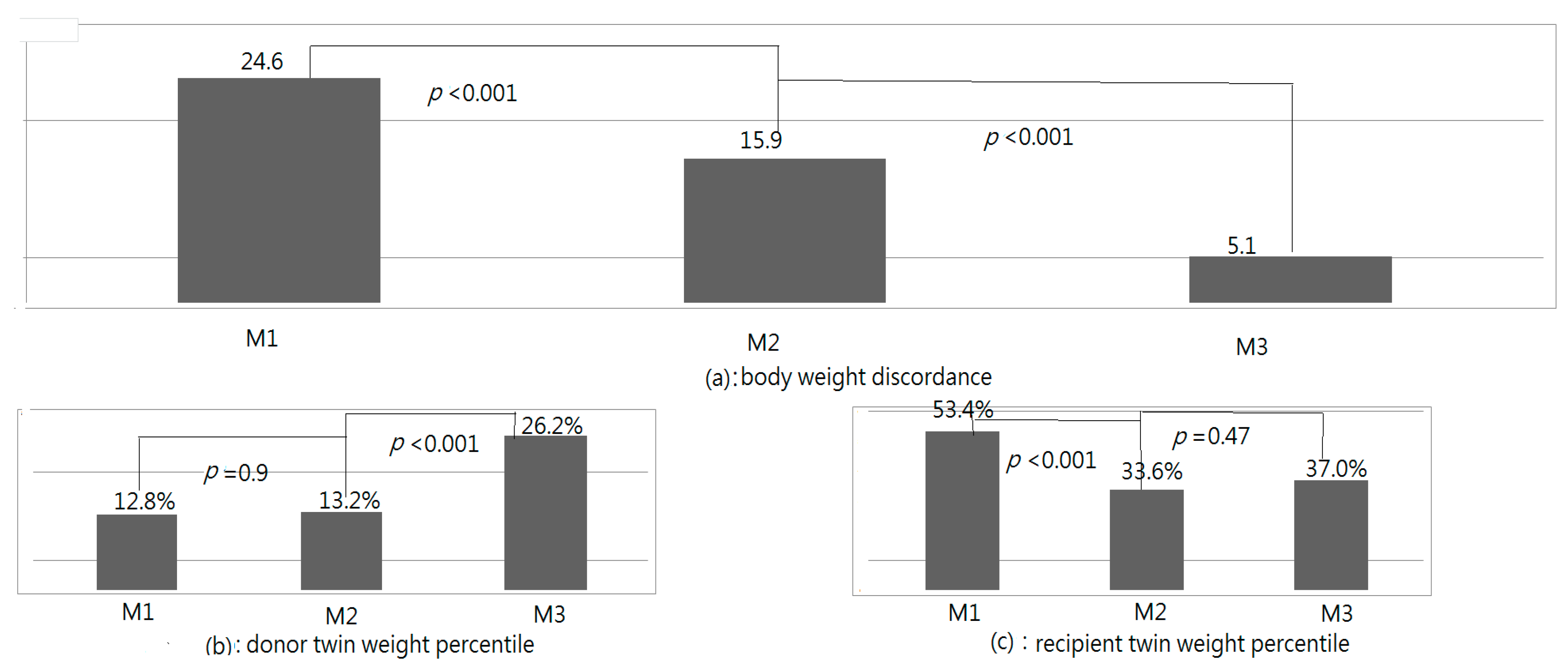
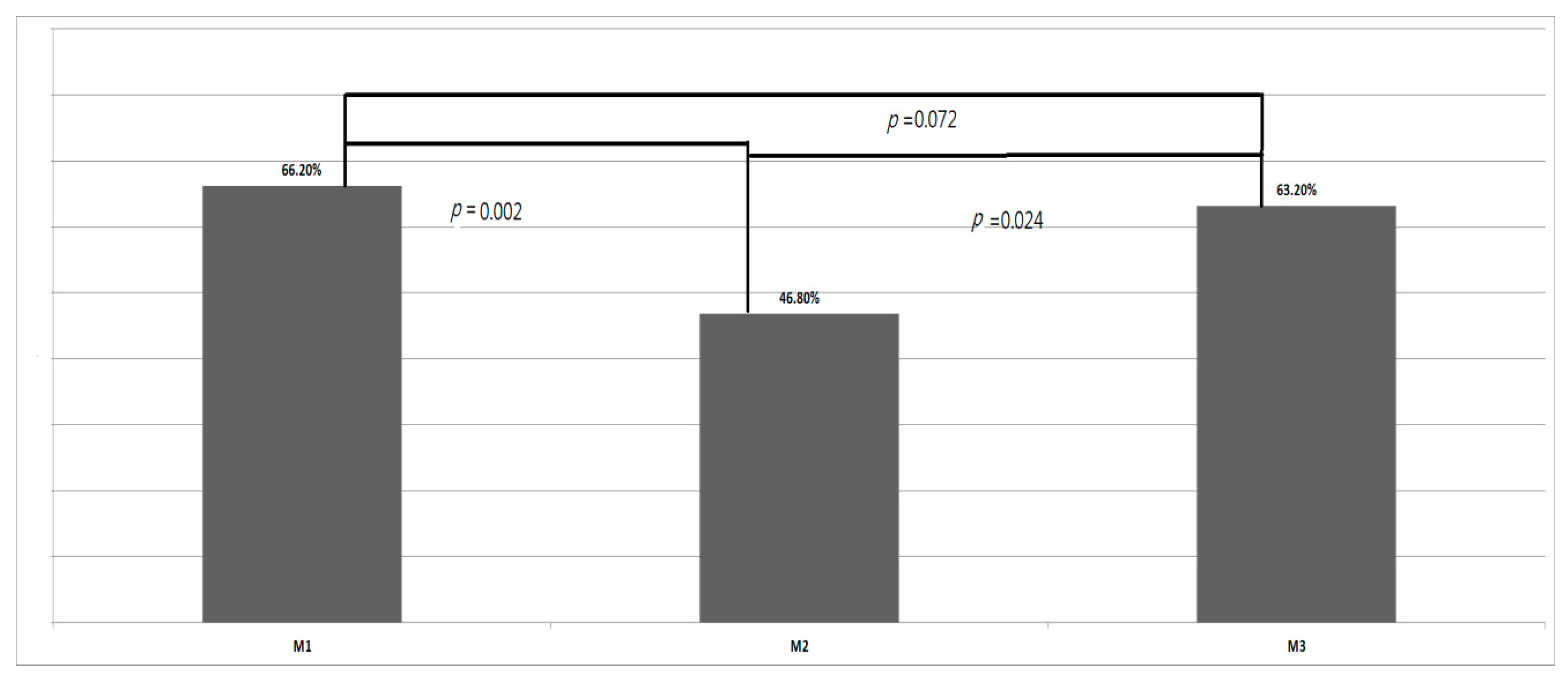
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lewi, L.; Jani, J.; Blickstein, I.; Huber, A.; Gucciardo, L.; Van Mieghem, T.; Done, E.; Boes, A.S.; Hecher, K.; Gratacos, E.; et al. The outcome of monochorionic diamniotic twin gestations in the era of invasive fetal therapy: A prospective cohort study. Am. J. Obstet. Gynecol. 2008, 199, 514.E1–514.E8. [Google Scholar] [CrossRef] [PubMed]
- Roberts, D.; Neilson, J.P.; Kilby, M.D.; Gates, S. Interventions for the treatment of twin-twin transfusion syndrome. Cochrane Database Syst. Rev. 2014, 1, CD002073. [Google Scholar] [CrossRef] [PubMed]
- Emery, S.P.; Hasley, S.K.; Catov, J.M.; Miller, R.S.; Moon-Grady, A.J.; Baschat, A.A.; Johnson, A.; Lim, F.Y.; Gagnon, A.L.; O’Shaughnessy, R.W.; et al. North American Fetal Therapy Network: Intervention vs. expectant management for stage I twin-twin transfusion syndrome. Am. J. Obstet. Gynecol. 2016, 215, 346.E1–346.E7. [Google Scholar] [CrossRef] [PubMed]
- Khalil, A.; Cooper, E.; Townsend, R.; Thilaganathan, B. Evolution of Stage 1 Twin-to-Twin Transfusion Syndrome (TTTS): Systematic Review and Meta-Analysis. Twin Res. Hum. Genet. 2016, 19, 207–216. [Google Scholar] [CrossRef] [PubMed]
- Sutton, D.; Miller, R. Neurologic Outcomes after Prenatal Treatment of Twin-Twin Transfusion Syndrome. Clin. Perinatol. 2020, 47, 719–731. [Google Scholar] [CrossRef]
- Chmait, R.H.; Chon, A.H.; Schrager, S.M.; Kontopoulos, E.V.; Quintero, R.A.; Vanderbilt, D.L. Donor catch-up growth after laser surgery for twin-twin transfusion syndrome. Early Hum. Dev. 2015, 91, 751–754. [Google Scholar] [CrossRef]
- Chmait, R.H.; Korst, L.M.; Bornick, P.W.; Allen, M.H.; Quintero, R.A. Fetal growth after laser therapy for twin-twin transfusion syndrome. Am. J. Obstet. Gynecol. 2008, 199, 47.E6–47.E41. [Google Scholar] [CrossRef]
- Maschke, C.; Franz, A.R.; Ellenrieder, B.; Hecher, K.; Diemert, A.; Bartmann, P. Growth after intrauterine laser coagulation for twin-twin transfusion syndrome. Arch. Dis. Child. Fetal Neonatal Ed. 2010, 95, F115–F117. [Google Scholar] [CrossRef]
- Moreira de Sa, R.A.; Salomon, L.J.; Takahashi, Y.; Yamamoto, M.; Ville, Y. Analysis of fetal growth after laser therapy in twin-to-twin transfusion syndrome. J. Ultrasound Med. 2005, 24, 1213–1219. [Google Scholar] [CrossRef][Green Version]
- Cheetham, C. Perinatal death in twins: Absolute risk: Better basis for decision making. BMJ 2007, 334, 651–652. [Google Scholar] [CrossRef]
- Vogel, J.P.; Torloni, M.R.; Seuc, A.; Betran, A.P.; Widmer, M.; Souza, J.P.; Merialdi, M. Maternal and perinatal outcomes of twin pregnancy in 23 low- and middle-income countries. PLoS ONE 2013, 8, e70549. [Google Scholar] [CrossRef] [PubMed]
- Alexander, G.R.; Kogan, M.; Bader, D.; Carlo, W.; Allen, M.; Mor, J. US birth weight/gestational age-specific neonatal mortality: 1995–1997 rates for whites, hispanics, and blacks. Pediatrics 2003, 111, e61–e66. [Google Scholar] [CrossRef] [PubMed]
- Baschat, A.A. Fetal responses to placental insufficiency: An update. BJOG 2004, 111, 1031–1041. [Google Scholar] [CrossRef] [PubMed]
- Miller, J.; Chauhan, S.P.; Abuhamad, A.Z. Discordant twins: Diagnosis, evaluation and management. Am. J. Obstet. Gynecol. 2012, 206 Pt 1, 10–20. [Google Scholar] [CrossRef] [PubMed]
- Quintero, R.A.; Morales, W.J.; Allen, M.H.; Bornick, P.W.; Johnson, P.K.; Kruger, M. Staging of twin-twin transfusion syndrome. J. Perinatol. 1999, 19, 550–555. [Google Scholar] [CrossRef]
- Quintero, R.A.; Morales, W.J.; Mendoza, G.; Allen, M.; Kalter, C.S.; Giannina, G.; Angel, J.L. Selective photocoagulation of placental vessels in twin-twin transfusion syndrome: Evolution of a surgical technique. Obstet. Gynecol. Surv. 1998, 53 (Suppl. 12), S97–S103. [Google Scholar] [CrossRef]
- Slaghekke, F.; Lopriore, E.; Lewi, L.; Middeldorp, J.M.; van Zwet, E.W.; Weingertner, A.S.; Klumper, F.J.; DeKoninck, P.; Devlieger, R.; Kilby, M.D.; et al. Fetoscopic laser coagulation of the vascular equator versus selective coagulation for twin-to-twin transfusion syndrome: An open-label randomised controlled trial. Lancet 2014, 383, 2144–2151. [Google Scholar] [CrossRef]
- Bamberg, C.; Hecher, K. Update on twin-to-twin transfusion syndrome. Best Pract. Res. Clin. Obstet. Gynaecol. 2019, 58, 55–65. [Google Scholar] [CrossRef]
- Chang, Y.L.; Chao, A.S.; Chang, S.D.; Li, W.F.; Cheng, P.J. Predisposing factors and neonatal outcomes for twin-twin transfusion syndrome cases developing transient donor hydrops after fetoscopic laser coagulation: A case control study. BMC Pregnancy Childbirth 2019, 19, 87. [Google Scholar] [CrossRef]
- Hadlock, F.P.; Harrist, R.B.; Fearneyhough, T.C.; Deter, R.L.; Park, S.K.; Rossavik, I.K. Use of femur length/abdominal circumference ratio in detecting the macrosomic fetus. Radiology 1985, 154, 503–505. [Google Scholar] [CrossRef]
- Kiserud, T.; Benachi, A.; Hecher, K.; Perez, R.G.; Carvalho, J.; Piaggio, G.; Platt, L.D. The World Health Organization fetal growth charts: Concept, findings, interpretation, and application. Am. J. Obstet. Gynecol. 2018, 218, S619–S629. [Google Scholar] [CrossRef] [PubMed]
- Kiserud, T.; Piaggio, G.; Carroli, G.; Widmer, M.; Carvalho, J.; Neerup Jensen, L.; Giordano, D.; Cecatti, J.G.; Abdel Aleem, H.; Talegawkar, S.A.; et al. The World Health Organization Fetal Growth Charts: A Multinational Longitudinal Study of Ultrasound Biometric Measurements and Estimated Fetal Weight. PLoS Med. 2017, 14, e1002220. [Google Scholar] [CrossRef]
- Olsen, I.E.; Groveman, S.A.; Lawson, M.L.; Clark, R.H.; Zemel, B.S. New intrauterine growth curves based on United States data. Pediatrics 2010, 125, e214–e224. [Google Scholar] [CrossRef] [PubMed]
- Bamberg, C.; Diehl, W.; Diemert, A.; Sehner, S.; Hecher, K. Differentiation between TTTS Stages I vs. II and III vs. IV does not affect probability of double survival after laser therapy. Ultrasound Obstet. Gynecol. 2021, 58, 201–206. [Google Scholar] [CrossRef]
- Blickstein, I.; Kalish, R.B. Birthweight discordance in multiple pregnancy. Twin Res. 2003, 6, 526–531. [Google Scholar] [CrossRef]
- Keet, M.P.; Jaroszewicz, A.M.; Lombard, C.J. Follow-up study of physical growth of monozygous twins with discordant within-pair birth weights. Pediatrics 1986, 77, 336–344. [Google Scholar] [CrossRef]
- Monset-Couchard, M.; de Bethmann, O.; Relier, J.P. Long term outcome of small versus appropriate size for gestational age co-twins/triplets. Arch. Dis. Child. Fetal Neonatal Ed. 2004, 89, F310–F314. [Google Scholar] [CrossRef]
- Chang, Y.L.; Yang, C.Y.; Chao, A.S.; Chang, S.D.; Cheng, P.J.; Li, W.F.; You, S.H.; Lee, Y.C.; Peng, H.H.; Chueh, H.Y. Birth Weight Discordance and Neonatal Outcomes in Uncomplicated Twin Pregnancies. J. Reprod. Med. 2021, 66, 155–162. [Google Scholar]
- Quintero, R.A.; Martinez, J.M.; Lopez, J.; Bermudez, C.; Becerra, C.; Morales, W.; Arroyo, J. Individual placental territories after selective laser photocoagulation of communicating vessels in twin-twin transfusion syndrome. Am. J. Obstet. Gynecol. 2005, 192, 1112–1118. [Google Scholar] [CrossRef]
- Chang, Y.L.; Chmait, R.H.; Bornick, P.W.; Allen, M.H.; Quintero, R.A. The role of laser surgery in dissecting the etiology of absent or reverse end-diastolic velocity in the umbilical artery of the donor twin in twin-twin transfusion syndrome. Am. J. Obstet. Gynecol. 2006, 195, 478–483. [Google Scholar] [CrossRef]
- Donepudi, R.; Espinoza, J.; Nassr, A.A.; Belfort, M.A.; Shamshirsaz, A.A.; Sanz Cortes, M. Prediction of post-laser fetal death in selective growth restriction complicating twin-twin transfusion syndrome using standardized definitions. Ultrasound Obstet. Gynecol. 2021, 58, 738–743. [Google Scholar] [CrossRef] [PubMed]
- Donepudi, R.; Krispin, E.; Mustafa, H.; Espinoza, J.; Nassr, A.A.; Belfort, M.A.; Sanz Cortes, M.; Mostafaei, S.; Harman, C.; Turan, O.; et al. Twin twin transfusion syndrome with and without selective fetal growth restriction: Predictors of donor demise. Prenat. Diagn. 2021, 41, 1524–1530. [Google Scholar] [CrossRef] [PubMed]
- Chang, Y.L.; Chang, T.C.; Chang, S.D.; Cheng, P.J.; Chao, A.S.; Hsieh, P.C.; Soong, Y.K. Sonographic prediction of significant intertwin birth weight discordance. Eur. J. Obstet. Gynecol. Reprod. Biol. 2006, 127, 35–40. [Google Scholar] [CrossRef] [PubMed]

| TTTS Receipted FLP with Two Survivals (N = 53) | ||
|---|---|---|
| Maternal age at operation (year-old) | 33.0 ± 5.1 | |
| Gestational age at operation (weeks) | 20.6 ± 2.7 | |
| Gestational age at delivery (weeks) | 33.5 ± 3.4 | |
| Interval from operation to delivery (days) | 92.1 ± 48.7 | |
| Quintero stage (number) | ||
| I | 8 | |
| II | 26 | |
| III | 13 | |
| IV | 6 | |
| Mean interval between delivery to neonatal follow-up (days) | 569 ± 450 | |
| BWD | Quintero Stage I (N = 8) | Quintero Stage II (N = 26) | Quintero Stage III (N = 13) | Quintero Stage IV (N = 9) | p |
|---|---|---|---|---|---|
| M1 | 23.7 ± 12.6 | 18.8 ± 14.6 | 33.3 ± 12.8 | 32.0 ± 12.7 | 0.015 |
| M2 | 10.7 ± 22.3 | 9.7 ± 17.2 | 25.7 ±15.0 | 28.7 ± 20.9 | 0.020 |
| M3 | 2.9 ± 10.0 | 2.4 ± 10.5 | 11.4 ± 14.1 | 5.7 ± 13.1 | 0.157 |
| M2 | M3 | p | |
|---|---|---|---|
| Donor head circumference percentile | 26.3 ± 21.5 | 39.6 ± 30.1 | 0.004 |
| Recipient head circumference percentile | 47.1 ± 25.5 | 49.0 ± 31.0 | 0.66 |
| Donor body height percentile | 8.3 ± 12.2 | 33.6 ± 27.2 | <0.001 |
| Recipient body height percentile | 18.6 ± 15.7 | 40.7 ± 24.6 | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chang, Y.-L.; Hsu, C.-C.; Chao, A.-S.; Chang, S.-D.; Cheng, P.-J.; Li, W.-F. Effect of Fetoscopic Laser Photocoagulation on Fetal Growth and Placental Perfusion in Twin–Twin Transfusion Syndrome. J. Clin. Med. 2022, 11, 4404. https://doi.org/10.3390/jcm11154404
Chang Y-L, Hsu C-C, Chao A-S, Chang S-D, Cheng P-J, Li W-F. Effect of Fetoscopic Laser Photocoagulation on Fetal Growth and Placental Perfusion in Twin–Twin Transfusion Syndrome. Journal of Clinical Medicine. 2022; 11(15):4404. https://doi.org/10.3390/jcm11154404
Chicago/Turabian StyleChang, Yao-Lung, Chin-Chieh Hsu, An-Shine Chao, Shuenn-Dyh Chang, Po-Jen Cheng, and Wen-Fang Li. 2022. "Effect of Fetoscopic Laser Photocoagulation on Fetal Growth and Placental Perfusion in Twin–Twin Transfusion Syndrome" Journal of Clinical Medicine 11, no. 15: 4404. https://doi.org/10.3390/jcm11154404
APA StyleChang, Y.-L., Hsu, C.-C., Chao, A.-S., Chang, S.-D., Cheng, P.-J., & Li, W.-F. (2022). Effect of Fetoscopic Laser Photocoagulation on Fetal Growth and Placental Perfusion in Twin–Twin Transfusion Syndrome. Journal of Clinical Medicine, 11(15), 4404. https://doi.org/10.3390/jcm11154404






