Lung Ultrasound in Adults and Children with COVID-19: From First Discoveries to Recent Advances
- (a)
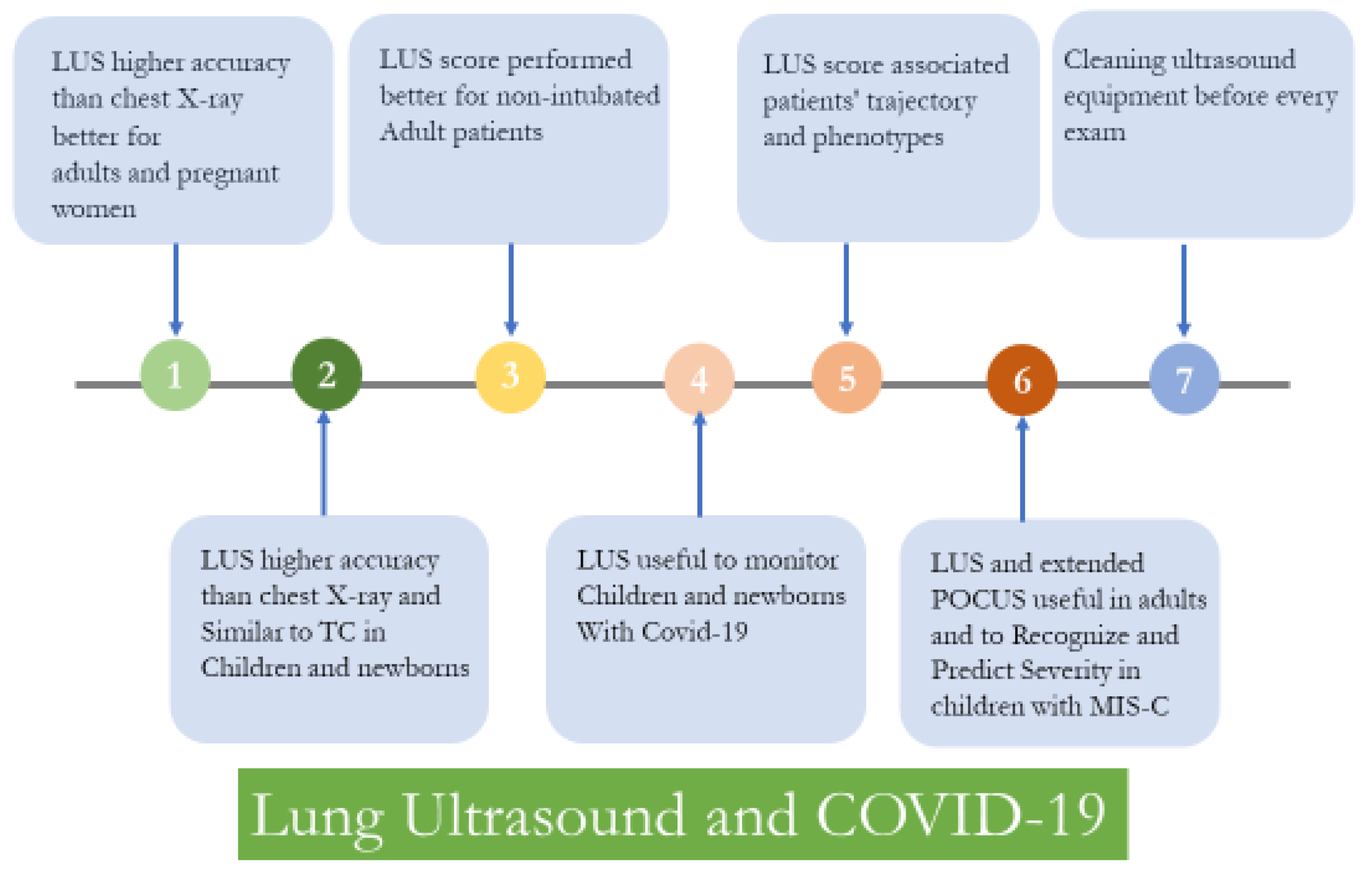
- Phenotype 1: patients with clinical improvement independent from the LUS evolution;
- (b)
- Phenotype 2: patients who presented a moderate improvement in their ultrasound imaging;
- (c)
- Phenotype 3: patients who responded very clearly, with a significant reduction in pulmonary involvement and LUS score;
- (d)
- Phenotype 4: patients who, while improving their clinical conditions, did not show an evident improvement from an ultrasound point of view, or presented an apparent worsening in LUS.
- -
- Confirmation that LUS was able to detect peripheral lung consolidations in children, independent from disease severity [28];
- -
- The optimum correlation between LUS and CT findings, making LUS a safe option to assess children with COVID-19 and spare them from unnecessary radiation, at least in asymptomatic, mild and moderate disease [31];
- -
- Equal or better sensitivity than chest X-ray in detecting lung involvement during SARS-CoV-2 infection [32];
- -
- Usefulness in monitoring lung involvement during follow-up, shown in small studies and supported by previous experience from other viral pediatric respiratory infections [33];
- -
- Application in children with Multisystem Inflammatory Syndrome, one of the most severe post-infective complications of SARS-CoV-2 infection [34,35]. This finding is in agreement with previous pediatric studies that showed how lung ultrasound can detect cardiopulmonary interactions during acute systemic diseases [36]. LUS has also been successfully used in MIS-C. Specifically, a team from Rome described the first findings of vertical artifacts and simple pleural effusions, and a team from Northern Italy detected a cutoff of severity, predicting the need for intensive care admission, as well as inotropic or respiratory support [34,35]. Importantly, as MIS-C is a systemic condition, a wider application of point-of-care ultrasound that also assesses free abdominal fluids, the thickening of intestinal walls, and ventricular contraction would allow a better recognition and characterization of a child with suspected MIS-C, as described by two independent teams [37,38].
- -
- The possibility of using linear high-frequency probes in the majority of cases;
- -
- Rare chronic respiratory comorbidities that make the interpretation of LUS findings more difficult;
- -
- A well-established lower risk of developing severe COVID-19, including thromboembolic events, which may be more difficult to recognize with the exclusive use of LUS.
Author Contributions
Funding
Conflicts of Interest
References
- Vetrugno, L.; Bove, T.; Orso, D.; Barbariol, F.; Bassi, F.; Boero, E.; Ferrari, G.; Kong, R. Our Italian experience using lung ultrasound for identification, grading and serial follow-up of severity of lung involvement for management of patients with COVID-19. Echocardiography 2020, 37, 625–627. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Haaksma, M.E.; Heldeweg, M.L.A.; Lopez Matta, J.E.; Smit, J.M.; van Trigt, J.D.; Nooitgedacht, J.S.; Elzo Kraemer, C.V.; van de Wiel, M.; Girbes, A.R.J.; Heunks, L.; et al. Lung ultrasound findings in patients with novel SARS-CoV-2. ERJ Open Res. 2020, 6, 00238-2020. [Google Scholar] [CrossRef] [PubMed]
- Pivetta, E.; Goffi, A.; Tizzani, M.; Locatelli, S.M.; Porrino, G.; Losano, I.; Leone, D.; Calzolari, G.; Vesan, M.; Steri, F.; et al. Lung Ultrasonography for the Diagnosis of SARS-CoV-2 Pneumonia in the Emergency Department. Ann. Emerg. Med. 2021, 77, 385–394. [Google Scholar] [CrossRef] [PubMed]
- Volpicelli, G.; Gargani, L.; Perlini, S.; Spinelli, S.; Barbieri, G.; Lanotte, A.; Casasola, G.G.; Nogué-Bou, R.; Lamorte, A.; Agricola, E.; et al. Lung ultrasound for the early diagnosis of COVID-19 pneumonia: An international multicenter study. Intensive Care Med. 2021, 47, 444–454. [Google Scholar] [CrossRef] [PubMed]
- Ma, I.W.Y.; Steinmetz, P.; Weerdenburg, K.; Woo, M.Y.; Olszynski, P.; Heslop, C.L.; Miller, S.; Sheppard, G.; Daniels, V.; Desy, J.; et al. The Canadian Medical Student Ultrasound Curriculum: A Statement From the Canadian Ultrasound Consensus for Undergraduate Medical Education Group. J. Ultrasound Med. 2020, 39, 1279–1287. [Google Scholar] [CrossRef] [Green Version]
- Vetrugno, L.; Mojoli, F.; Cortegiani, A.; Bignami, E.G.; Ippolito, M.; Orso, D.; Corradi, F.; Cammarota, G.; Mongodi, S.; Boero, E.; et al. Italian Society of Anesthesia, Analgesia, Resuscitation, and Intensive Care expert consensus statement on the use of lung ultrasound in critically ill patients with coronavirus disease 2019 (ITACO). J. Anesth. Analg. Crit. Care 2021, 1, 16. [Google Scholar] [CrossRef]
- Soldati, G.; Smargiassi, A.; Inchingolo, R.; Buonsenso, D.; Perrone, T.; Briganti, D.F.; Perlini, S.; Torri, E.; Mariani, A.; Mossolani, E.E.; et al. Proposal for International Standardization of the Use of Lung Ultrasound for Patients With COVID-19: A Simple, Quantitative, Reproducible Method. J. Ultrasound Med. 2020, 39, 1413–1419. [Google Scholar] [CrossRef] [Green Version]
- Smargiassi, A.; Soldati, G.; Borghetti, A.; Scoppettuolo, G.; Tamburrini, E.; Testa, A.C.; Moro, F.; Natale, L.; Larici, A.R.; Buonsenso, D.; et al. Lung ultrasonography for early management of patients with respiratory symptoms during COVID-19 pandemic. J. Ultrasound 2020, 23, 449–456. [Google Scholar] [CrossRef]
- Vetrugno, L.; Mojoli, F.; Boero, E.; Berchialla, P.; Bignami, E.G.; Orso, D.; Cortegiani, A.; Forfori, F.; Corradi, F.; Cammarota, G.; et al. Level of Diffusion and Training of Lung Ultrasound during the COVID-19 Pandemic—A National Online Italian Survey (ITALUS) from the Lung Ultrasound Working Group of the Italian Society of Anesthesia, Analgesia, Resuscitation, and Intensive Care (SIAARTI). Ultraschall Med. 2021. [Google Scholar] [CrossRef]
- Tung-Chen, Y.; Martí de Gracia, M.; Díez-Tascón, A.; Alonso-González, R.; Agudo-Fernández, S.; Parra-Gordo, M.L.; Ossaba-Vélez, S.; Rodríguez-Fuertes, P.; Llamas-Fuentes, R. Correlation between Chest Computed Tomography and Lung Ultrasonography in Patients with Coronavirus Disease 2019 (COVID-19). Ultrasound Med. Biol. 2020, 46, 2918–2926. [Google Scholar] [CrossRef]
- Islam, N.; Ebrahimzadeh, S.; Salameh, J.-P.; Kazi, S.; Fabiano, N.; Treanor, L.; Absi, M.; Hallgrimson, Z.; Leeflang, M.M.G.; Hooft, L.; et al. Thoracic imaging tests for the diagnosis of COVID-19. Cochrane Database Syst. Rev. 2021, CD013639. [Google Scholar] [CrossRef]
- Vetrugno, L.; Sala, A.; Orso, D.; Meroi, F.; Fabbro, S.; Boero, E.; Valent, F.; Cammarota, G.; Restaino, S.; Vizzielli, G.; et al. Lung Ultrasound Signs and Their Correlation With Clinical Symptoms in COVID-19 Pregnant Women: The “PINK-CO” Observational Study. Front. Med. 2022, 8, 768261. [Google Scholar] [CrossRef]
- Lichter, Y.; Topilsky, Y.; Taieb, P.; Banai, A.; Hochstadt, A.; Merdler, I.; Gal Oz, A.; Vine, J.; Goren, O.; Cohen, B.; et al. Lung ultrasound predicts clinical course and outcomes in COVID-19 patients. Intensive Care Med. 2020, 46, 1873–1883. [Google Scholar] [CrossRef] [PubMed]
- Duclos, G.; Bazalguette, F.; Allaouchiche, B.; Mohammedi, N.; Lopez, A.; Gazon, M.; Besch, G.; Bouvet, L.; Muller, L.; Mathon, G.; et al. Can Thoracic Ultrasound on Admission Predict the Outcome of Critically Ill Patients with SARS-CoV-2? A French Multi-Centric Ancillary Retrospective Study. Adv Ther. 2021, 38, 2599–2612. [Google Scholar] [CrossRef] [PubMed]
- Bonadia, N.; Carnicelli, A.; Piano, A.; Buonsenso, D.; Gilardi, E.; Kadhim, C.; Torelli, E.; Petrucci, M.; Di Maurizio, L.; Biasucci, D.G.; et al. Lung Ultrasound Findings Are Associated with Mortality and Need for Intensive Care Admission in COVID-19 Patients Evaluated in the Emergency Department. Ultrasound Med. Biol. 2020, 46, 2927–2937. [Google Scholar] [CrossRef] [PubMed]
- Biasucci, D.G.; Buonsenso, D.; Piano, A.; Bonadia, N.; Vargas, J.; Settanni, D.; Bocci, M.G.; Grieco, D.L.; Carnicelli, A.; Scoppettuolo, G.; et al. Lung ultrasound predicts non-invasive ventilation outcome in COVID-19 acute respiratory failure: A pilot study. Minerva Anestesiol. 2021, 87, 1006–1016. [Google Scholar] [CrossRef] [PubMed]
- Baciarello, M.; Bonetti, A.; Vetrugno, L.; Saturno, F.; Nouvenne, A.; Bellini, V.; Meschi, T.; Bignami, E. Is lung ultrasound score a useful tool to monitoring and handling moderate and severe COVID-19 patients in the general ward? An observational pilot study. J. Clin. Monit. Comput. 2022, 36, 785–793. [Google Scholar] [CrossRef]
- Meroi, F.; Orso, D.; Vetrugno, L.; Bove, T. Lung Ultrasound Score in Critically Ill COVID-19 Patients: A Waste of Time or a Time-Saving Tool? Acad. Radiol. 2021, 28, 1323–1324. [Google Scholar] [CrossRef]
- Rouby, J.J.; Arbelot, C.; Gao, Y.; Zhang, M.; Lv, J.; An, Y.; Chunyao, W.; Bin, D.; Valente Barbas, C.S.; Dexheimer Neto, F.L.; et al. Training for Lung Ultrasound Score Measurement in Critically Ill Patients. Am. J. Respir. Crit. Care Med. 2018, 198, 398–401. [Google Scholar] [CrossRef]
- Fumagalli, J.; Panigada, M.; Klompas, M.; Berra, L. Ventilator-associated pneumonia among SARS-CoV-2 acute respiratory distress syndrome patients. Curr. Opin. Crit. Care 2022, 28, 74–82. [Google Scholar] [CrossRef]
- Vetrugno, L.; Meroi, F.; Orso, D.; D’Andrea, N.; Marin, M.; Cammarota, G.; Mattuzzi, L.; Delrio, S.; Furlan, D.; Foschiani, J.; et al. Can Lung Ultrasound Be the Ideal Monitoring Tool to Predict the Clinical Outcome of Mechanically Ventilated COVID-19 Patients? An Observational Study. Healthcare 2022, 10, 568. [Google Scholar] [CrossRef] [PubMed]
- Karagodin, I.; Carvalho Singulane, C.; Woodward, G.M.; Xie, M.; Tucay, E.S.; Tude Rodrigues, A.C.; Vasquez-Ortiz, Z.Y.; Alizadehasl, A.; Monaghan, M.J.; Ordonez Salazar, B.A.; et al. Echocardiographic Correlates of In-Hospital Death in Patients with Acute COVID-19 Infection: The World Alliance Societies of Echocardiography (WASE-COVID) Study. J. Am. Soc. Echocardiogr. 2021, 34, 819–830. [Google Scholar] [CrossRef] [PubMed]
- Corradi, F.; Vetrugno, L.; Orso, D.; Bove, T.; Schreiber, A.; Boero, E.; Santori, G.; Isirdi, A.; Barbieri, G.; Forfori, F. Diaphragmatic thickening fraction as a potential predictor of response to continuous positive airway pressure ventilation in COVID-19 pneumonia: A single-center pilot study. Respir. Physiol. Neurobiol. 2021, 284, 103585. [Google Scholar] [CrossRef]
- Leote, J.; Judas, T.; Broa, A.L.; Lopes, M.; Abecasis, F.; Pintassilgo, I.; Goncalves, A.; Gonzalez, F. Time Course of Lung Ultrasound Findings in Patients with COVID-19 Pneumonia and Cardiac Dysfunction. Ultrasound J. 2022, 14, 28. [Google Scholar] [CrossRef] [PubMed]
- Dell’Aquila, P.; Raimondo, P.; Racanelli, V.; De Luca, P.; De Matteis, S.; Pistone, A.; Melodia, R.; Crudele, L.; Lomazzo, D.; Solimando, A.G.; et al. Integrated lung ultrasound score for early clinical decision-making in patients with COVID-19: Results and implications. Ultrasound J. 2022, 14, 21. [Google Scholar] [CrossRef] [PubMed]
- Musolino, A.M.; Tomà, P.; De Rose, C.; Pitaro, E.; Boccuzzi, E.; De Santis, R.; Morello, R.; Supino, M.C.; Villani, A.; Valentini, P.; et al. Ten Years of Pediatric Lung Ultrasound: A Narrative Review. Front Physiol. 2022, 12, 721951. [Google Scholar] [CrossRef]
- Amendolea, A.; Gori, L.; Adamoli, P.; Limoli, G.; Supino, M.C.; Coco, A.D.; Trobia, G.L.; Tursi, F.; Soldati, G.; Buonsenso, D.; et al. Pleuropulmonary Ultrasound in Pediatrics: Proposal of a Reporting Model From the Academy of Thoracic Ultrasound. J. Ultrasound Med. 2021. [Google Scholar] [CrossRef]
- Caro-Dominguez, P.; Shelmerdine, S.C.; Toso, S.; Secinaro, A.; Toma, P.; Damasio, M.B.; Navallas, M.; Riaza-Martin, L.; Gomez-Pastrana, D.; Ghadimi Mahani, M.; et al. Thoracic imaging of coronavirus disease 2019 (COVID-19) in children: A series of 91 cases. Pediatr. Radiol. 2020, 50, 1354–1368. [Google Scholar] [CrossRef]
- Musolino, A.M.; Supino, M.C.; Buonsenso, D.; Ferro, V.; Valentini, P.; Magistrelli, A.; Lombardi, M.H.; Romani, L.; D’Argenio, P.; Campana, A.; et al. Lung Ultrasound in Children with COVID-19: Preliminary Findings. Ultrasound Med. Biol. 2020, 46, 2094–2098. [Google Scholar] [CrossRef]
- Gregorio-Hernández, R.; Escobar-Izquierdo, A.B.; Cobas-Pazos, J.; Martínez-Gimeno, A. Point-of-care lung ultrasound in three neonates with COVID-19. Eur. J. Pediatr. 2020, 179, 1279–1285. [Google Scholar] [CrossRef]
- Hizal, M.; Aykac, K.; Yayla, B.C.C.; Yilmaz, A.; Altun, D.; Akkaya, H.E.; Bayhan, G.I.; Kurt, A.N.C.; Karakaya, J.; Ozsurekci, Y.; et al. Diagnostic value of lung ultrasonography in children with COVID-19. Pediatr. Pulmonol. 2021, 56, 1018–1025. [Google Scholar] [CrossRef]
- Türe, E.; Korkmaz, M.F.; Aksoy, F.D.; Ceylan Demirbaş, B.; Menekşe, B.; Çiftçi, M.; Korkmaz, M. Point-of-care lung ultrasound findings in the pediatric emergency clinic during the COVID-19 pandemic. J. Clin. Ultrasound 2021, 49, 85–90. [Google Scholar] [CrossRef]
- Musolino, A.M.; Supino, M.C.; Buonsenso, D.; Papa, R.E.; Chiurchiù, S.; Magistrelli, A.; Barbieri, M.A.; Raponi, M.; D’Argenio, P.; Villani, A.; et al. Lung ultrasound in the diagnosis and monitoring of 30 children with coronavirus disease 2019. Pediatr. Pulmonol. 2021, 56, 1045–1052. [Google Scholar] [CrossRef] [PubMed]
- Musolino, A.M.; Boccuzzi, E.; Buonsenso, D.; Supino, M.C.; Mesturino, M.A.; Pitaro, E.; Ferro, V.; Nacca, R.; Sinibaldi, S.; Palma, P.; et al. The Role of Lung Ultrasound in Diagnosing COVID-19-Related Multisystemic Inflammatory Disease: A Preliminary Experience. J. Clin. Med. 2022, 11, 234. [Google Scholar] [CrossRef] [PubMed]
- Camporesi, A.; Gemma, M.; Buonsenso, D.; Ferrario, S.; Mandelli, A.; Pessina, M.; Diotto, V.; Rota, E.; Raso, I.; Fiori, L.; et al. Lung Ultrasound Patterns in Multisystem Inflammatory Syndrome in Children (MIS-C)-Characteristics and Prognostic Value. Children 2022, 9, 931. [Google Scholar] [CrossRef]
- De Rose, C.; Pierantoni, L.; Buonsenso, D. COVID-19 and lung ultrasound: Reasons why paediatricians can support adult COVID-19 units during critical epidemiologic periods. J. Ultrasound 2022, 25, 413–417. [Google Scholar] [CrossRef]
- Delmonaco, A.G.; Carpino, A.; Raffaldi, I.; Pruccoli, G.; Garrone, E.; Del Monte, F.; Riboldi, L.; Licciardi, F.; Urbino, A.F.; Parodi, E. First diagnosis of multisystem inflammatory syndrome in children (MIS-C): An analysis of PoCUS findings in the ED. Ultrasound J. 2021, 13, 41. [Google Scholar] [CrossRef]
- Kennedy, T.M.; Dessie, A.; Kessler, D.O.; Malia, L.; Rabiner, J.E.; Firnberg, M.T.; Ng, L. Point-of-Care Ultrasound Findings in Multisystem Inflammatory Syndrome in Children: A Cross-Sectional Study. Pediatr. Emerg. Care 2021, 37, 334–339. [Google Scholar] [CrossRef]
- Buonsenso, D.; Musolino, A.; Ferro, V.; De Rose, C.; Morello, R.; Ventola, C.; Liotti, F.M.; De Sanctis, R.; Chiaretti, A.; Biasucci, D.G.; et al. Role of lung ultrasound for the etiological diagnosis of acute lower respiratory tract infection (ALRTI) in children: A prospective study. J. Ultrasound 2022, 25, 185–197. [Google Scholar] [CrossRef]
- Berce, V.; Tomazin, M.; Gorenjak, M.; Berce, T.; Lovrenčič, B. The Usefulness of Lung Ultrasound for the Aetiological Diagnosis of Community-Acquired Pneumonia in Children. Sci. Rep. 2019, 9, 17957. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Buonsenso, D.; Vetrugno, L. Lung Ultrasound in Adults and Children with COVID-19: From First Discoveries to Recent Advances. J. Clin. Med. 2022, 11, 4340. https://doi.org/10.3390/jcm11154340
Buonsenso D, Vetrugno L. Lung Ultrasound in Adults and Children with COVID-19: From First Discoveries to Recent Advances. Journal of Clinical Medicine. 2022; 11(15):4340. https://doi.org/10.3390/jcm11154340
Chicago/Turabian StyleBuonsenso, Danilo, and Luigi Vetrugno. 2022. "Lung Ultrasound in Adults and Children with COVID-19: From First Discoveries to Recent Advances" Journal of Clinical Medicine 11, no. 15: 4340. https://doi.org/10.3390/jcm11154340
APA StyleBuonsenso, D., & Vetrugno, L. (2022). Lung Ultrasound in Adults and Children with COVID-19: From First Discoveries to Recent Advances. Journal of Clinical Medicine, 11(15), 4340. https://doi.org/10.3390/jcm11154340





