Post-Bariatric Plastic Surgery: Abdominoplasty, the State of the Art in Body Contouring
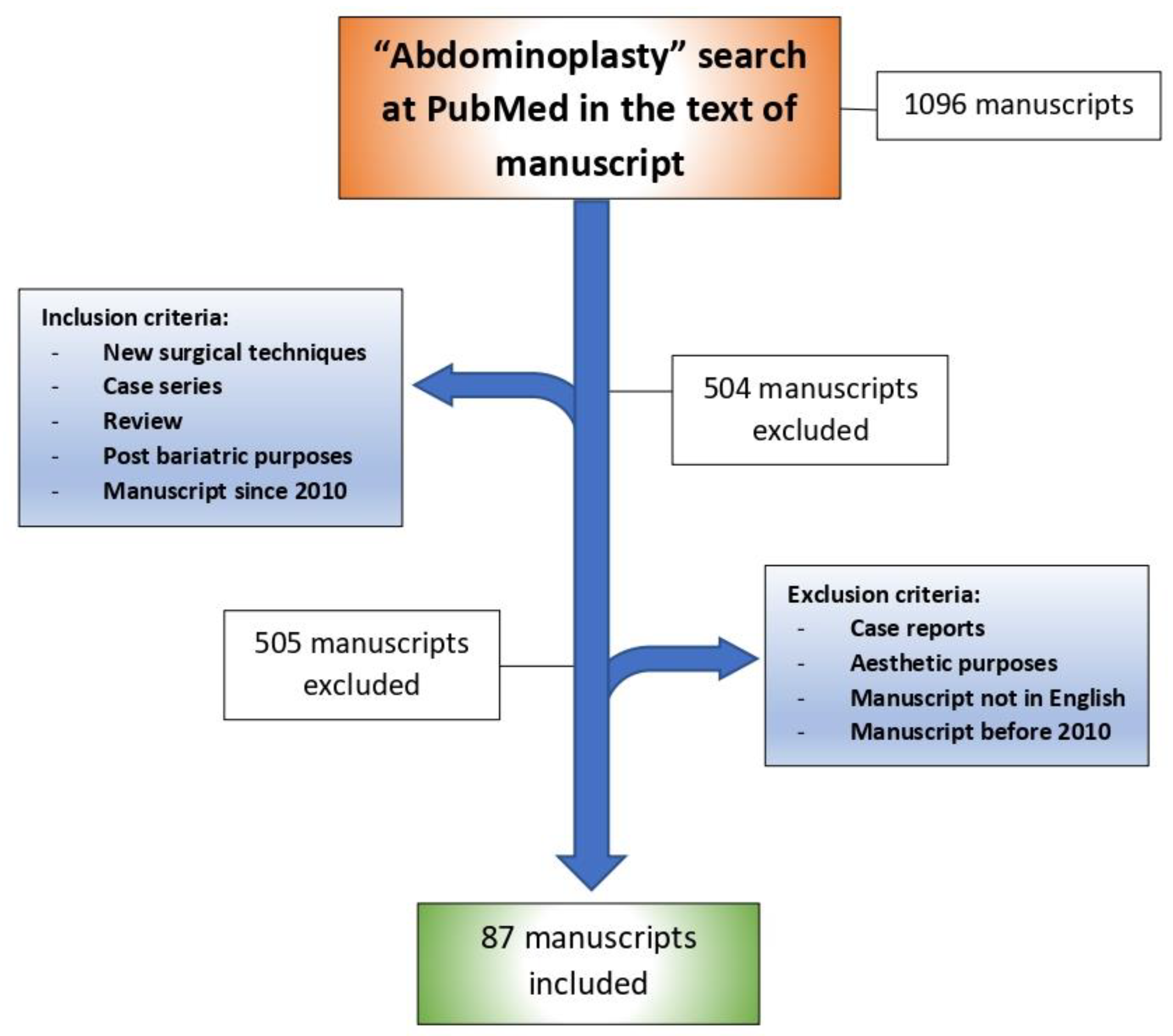
Abstract
:1. Introduction
2. Ethical Approval
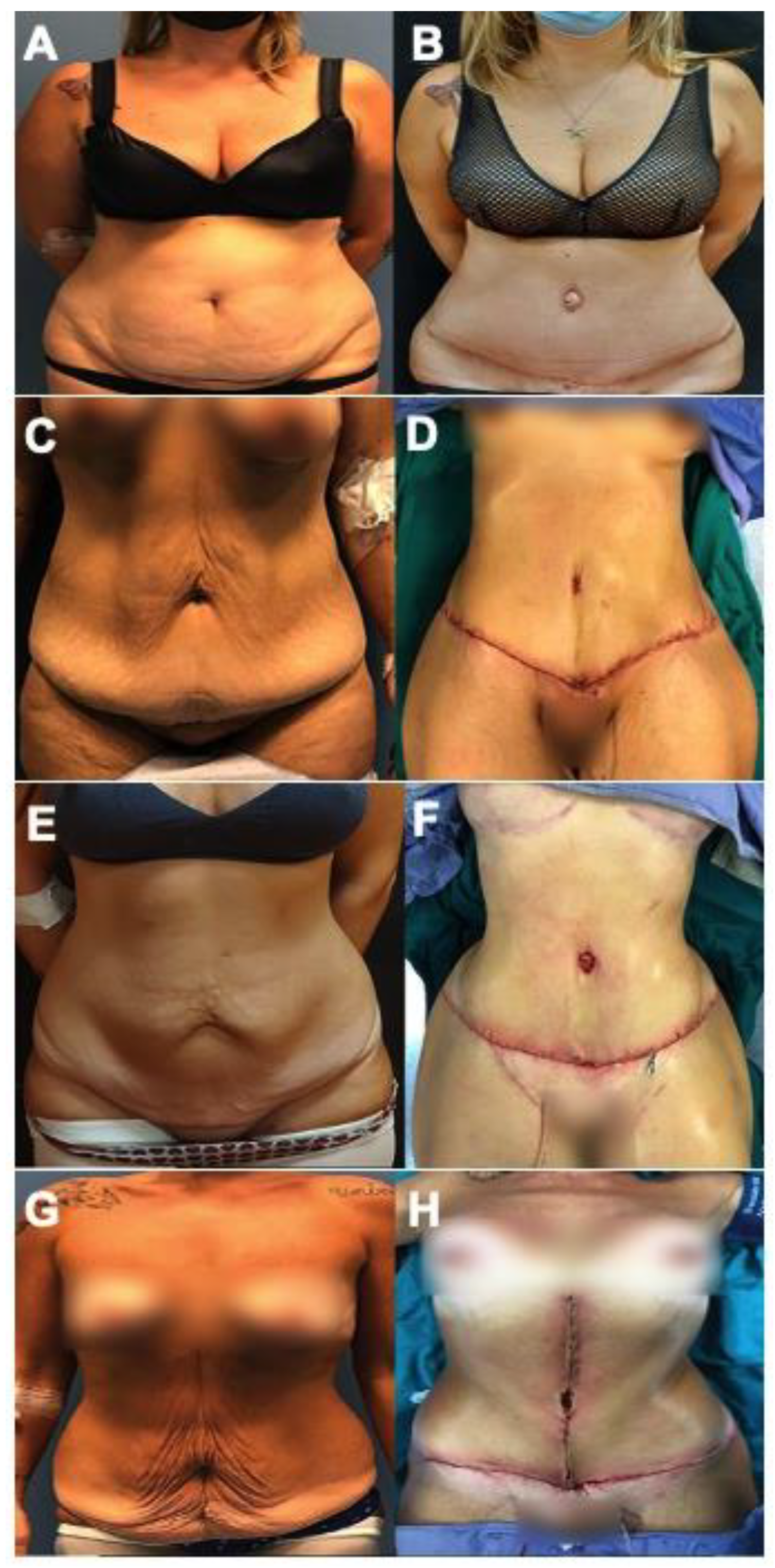
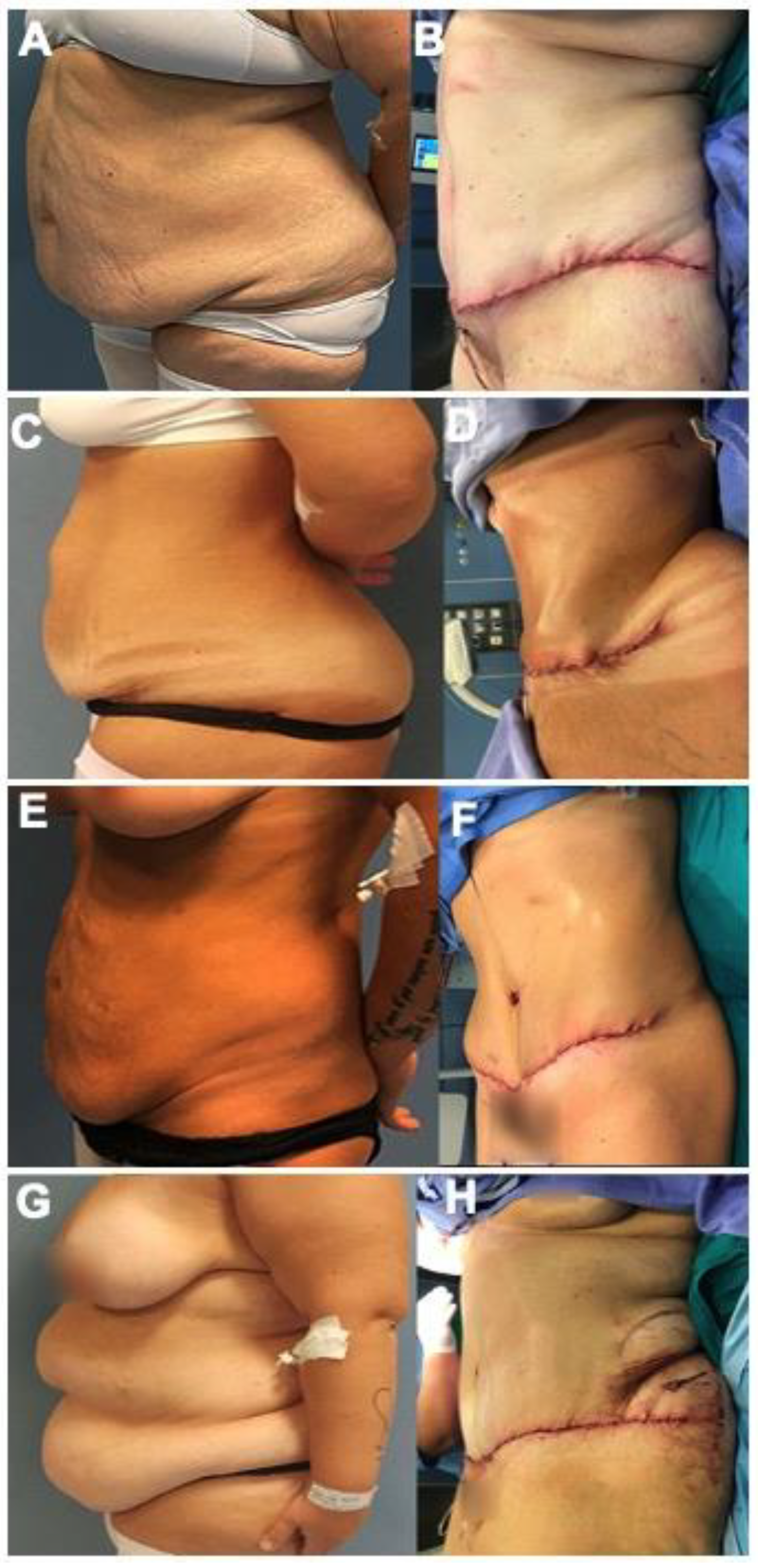
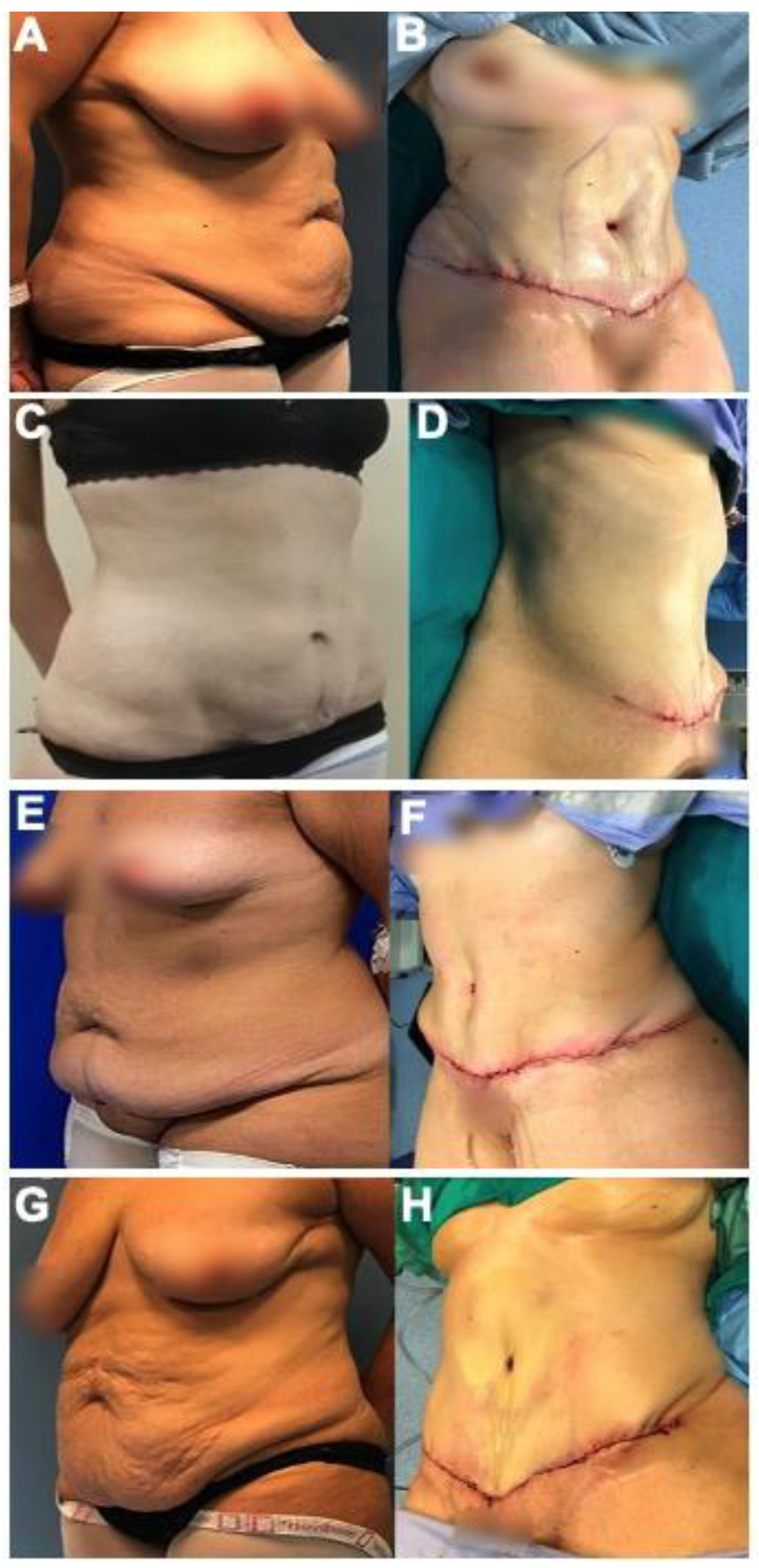
3. Abdominoplasty in Post-Bariatric Patients
4. Different Techniques in Abdominoplasty
5. Complications in Abdominoplasty
| Authors. | Benefits | Complications | Study Design | Number of Participants |
|---|---|---|---|---|
| Gilmartin et al. [22] | Excess skin limits mobility and exercise, causes difficulty performing personal hygiene, skin irritation and infections, psychological and emotional distress, and social discomfort. Body contouring surgery such as abdominoplasty can improve self-esteem and mood. | Long-lasting scarring | Retrospective | 20 |
| De Paep et al. [21] | Restores musculofascial integrity and skin elasticity. | 29.8% complication rate: minor wound problems, complications require medical intervention, seroma, umbilical necrosis, bleeding, DVT/PE | Retrospective | 898 |
| Schlosshauer et al. [33] | N/A | 42% complication rate. Increased risk of wound healing problems. Increased complications associated with age, male gender, resection weight. | Retrospective | 406 |
| Donato et al. [28] | N/A | Male gender is risk factor for complications | Retrospective | 4369 |
| Lievain et al. [34] | N/A | Complication rate significantly higher in post-bariatric patients, mainly healing problems | Retrospective | 238 |
| Vastine et al. [31] | N/A | 80% obese patients had complications vs 33% in nonobese. No effect of gastric bypass on complications. | Retrospective | 90 |
| Greco et al. [49] | N/A | Significant increase in wound complications for post-bariatric patients | Retrospective | 89 |
| Staalesen el al [50] | N/A | Significant increase in wound complications for post-bariatric patients | Retrospective | 161 |
| Chetta et al. [51] | N/A | No difference in complication rate | Retrospective | 307 |
| Pajula et al. [52] | N/A | No difference in complication rate | Retrospective | 158 |
| Neaman and Hansen [46] | N/A | Variable complication rates | Retrospective | 206 |
| de Kerviler et al. [53] | N/A | Variable complication rates | Retrospective | 104 |
| Brito et al. [54] | N/A | Variable complication rates | Retrospective | 191 |
| Sirota et al. [55] | N/A | Variable complication rates | Retrospective | 144 |
| Marouf and Mortada [45] | N/A | Most common complications in post-bariatric patients: seroma, wound dehiscence, infection, necrosis, DVT, PE | Systematic review and meta-analysis | 522 |
| Authors | Current Techniques | Complications |
|---|---|---|
| Gonzalez-Ulloa [38] | Circumferential abdominoplasty | N/A |
| Hunstad [39] | Circumferential abdominoplasty | N/A |
| Friedman and Michaels [41] | Fleur-de-lis | Complication rate comparable to traditional abdominoplasty. |
| Shestak [43] | Belt lipectomy modification | N/A |
6. Recent Technologies in Post-Bariatric Body Contouring
| Authors | Assistive Technologies | Complications |
|---|---|---|
| Vidal et al. [42] | Liposuction | Does not put patients at additional risk. |
| Herman et al. [37] | Liposuction | Could introduce excess ptotic skin. |
| Zocchi [65] | Ultrasonic-assisted lipoplasty | N/A |
| Irvine Duncan [66] | Radiofrequency-assisted liposuction | N/A |
| Jewell et al. [67] | VASER | No major complications |
| Hoyos and Millard [68] | VASER-assisted high definition liposculpture | 6.5% incidence of seromas, 2.94% incidence of port skin burns |
| Cook et al. [69] | Bipolar RF | Minimal adverse events |
| Pierazzi et al. [71] | Ligasure Impact | Reduction in seroma and bleeding risk |
| Kinney and Lozanova [72] | High-Intensity Focused Electro-Magnetic (HIFEM) | Muscle growth, fat reduction, reduced abdominal separation |
| Rohrich et al. [73] | Ultrasound-assisted lipoplasty | N/A |
| Schlosshauer et al. [74] | Pulsed electron avalanche knife (PEAK) | Less tissue damage, lower complication rate, fewer seroma |
7. Impact of Abdominoplasty on Health-Related Quality of Life (HRQoL)
8. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- WHO. Obesity and Overweight; WHO: Geneva, Switzerland, 2017. [Google Scholar]
- Vasileva, L.V.; Marchev, A.S.; Georgiev, M.I. Causes and solutions to “globesity”: The new fa(s)t alarming global epidemic. Food Chem. Toxicol. 2018, 121, 173–193. [Google Scholar] [CrossRef] [PubMed]
- GBD 2015 Obesity Collaborators; Afshin, A.; Forouzanfar, M.H.; Reitsma, M.B.; Sur, P.; Estep, K.; Lee, A.; Marczak, L.; Mokdad, A.H.; Moradi-Lakeh, M.; et al. Health Effects of Overweight and Obesity in 195 Countries over 25 Years. N. Engl. J. Med. 2017, 377, 13–27. [Google Scholar] [CrossRef] [PubMed]
- Sarma, S.; Sockalingam, S.; Dash, S. Obesity as a multisystem disease: Trends in obesity rates and obesity-related complications. Diabetes Obes. Metab. 2021, 23 (Suppl. S1), 3–16. [Google Scholar] [CrossRef] [PubMed]
- Finkelstein, E.A.; Khavjou, O.A.; Thompson, H.; Trogdon, J.G.; Pan, L.; Sherry, B.; Dietz, W. Obesity and severe obesity forecasts through 2030. Am. J. Prev. Med. 2012, 42, 563–570. [Google Scholar] [CrossRef] [PubMed]
- Arterburn, D.E.; Telem, D.A.; Kushner, R.F.; Courcoulas, A.P. Benefits and risks of bariatric surgery in adults: A review. JAMA 2020, 324, 879–887. [Google Scholar] [CrossRef]
- Sundbom, M.; Hedberg, J.; Marsk, R.; Boman, L.; Bylund, A.; Hedenbro, J.; Laurenius, A.; Lundegårdh, G.; Möller, P.; Olbers, T.; et al. Substantial Decrease in Comorbidity 5 Years After Gastric Bypass: A Population-based Study From the Scandinavian Obesity Surgery Registry. Ann. Surg. 2017, 265, 1166–1171. [Google Scholar] [CrossRef] [Green Version]
- Sutanto, A.; Wungu, C.D.K.; Susilo, H.; Sutanto, H. Reduction of Major Adverse Cardiovascular Events (MACE) after Bariatric Surgery in Patients with Obesity and Cardiovascular Diseases: A Systematic Review and Meta-Analysis. Nutrients 2021, 13, 3568. [Google Scholar] [CrossRef]
- Angrisani, L.; Santonicola, A.; Iovino, P.; Ramos, A.; Shikora, S.; Kow, L. Bariatric Surgery Survey 2018: Similarities and Disparities Among the 5 IFSO Chapters. Obes. Surg. 2021, 31, 1937–1948. [Google Scholar] [CrossRef]
- ASMBS. Estimate of Bariatric Surgery Numbers, 2011–2019. Available online: https://asmbs.org/resources/estimate-of-bariatric-surgery-numbers (accessed on 28 May 2022).
- O’Brien, P.E.; Hindle, A.; Brennan, L.; Skinner, S.; Burton, P.; Smith, A.; Crosthwaite, G.; Brown, W. Long-term outcomes after bariatric surgery: A systematic review and meta-analysis of weight loss at 10 or more years for all bariatric procedures and a single-centre review of 20-year outcomes after adjustable gastric banding. Obes. Surg. 2019, 29, 3–14. [Google Scholar] [CrossRef] [Green Version]
- Alalwan, A.A.; Friedman, J.; Park, H.; Segal, R.; Brumback, B.A.; Hartzema, A.G. US national trends in bariatric surgery: A decade of study. Surgery 2021, 170, 13–17. [Google Scholar] [CrossRef]
- Maciejewski, M.L.; Arterburn, D.E.; Van Scoyoc, L.; Smith, V.A.; Yancy, W.S., Jr.; Weidenbacher, H.J.; Livingston, E.H.; Olsen, M.K. Bariatric surgery and long-term durability of weight loss. JAMA Surg. 2016, 151, 1046–1055. [Google Scholar] [CrossRef] [PubMed]
- Hegland, P.A.; Aasprang, A.; Kolotkin, R.L.; Tell, G.S.; Andersen, J.R. Overall treatment satisfaction 5 years after bariatric surgery. Obes. Surg. 2020, 30, 206–213. [Google Scholar] [CrossRef] [PubMed]
- Shankar, P.; Boylan, M.; Sriram, K. Micronutrient deficiencies after bariatric surgery. Nutrition 2010, 26, 1031–1037. [Google Scholar] [CrossRef] [PubMed]
- Lamoshi, A.; Chernoguz, A.; Harmon, C.M.; Helmrath, M. Complications of bariatric surgery in adolescents. Semin. Pediatr. Surg. 2020, 29, 150888. [Google Scholar] [CrossRef] [PubMed]
- Baillot, A.; Brais-Dussault, E.; Bastin, A.; Cyr, C.; Brunet, J.; Aimé, A.; Romain, A.J.; Langlois, M.-F.; Bouchard, S.; Tchernof, A.; et al. What is known about the correlates and impact of excess skin after bariatric surgery: A scoping review. Obes. Surg. 2017, 27, 2488–2498. [Google Scholar] [CrossRef] [PubMed]
- Klassen, A.F.; Kaur, M.; Breitkopf, T.; Thoma, A.; Cano, S.; Pusic, A. Using the BODY-Q to understand impact of weight loss, excess skin, and the need for body contouring following bariatric surgery. Plast. Reconstr. Surg. 2018, 142, 77–86. [Google Scholar] [CrossRef]
- ElAbd, R.; Samargandi, O.A.; AlGhanim, K.; Alhamad, S.; Almazeedi, S.; Williams, J.; AlSabah, S.; AlYouha, S. Body contouring surgery improves weight loss after bariatric surgery: A systematic review and meta-analysis. Aesthetic Plast. Surg. 2021, 45, 1064–1075. [Google Scholar] [CrossRef]
- Romano, L.; Zoccali, G.; Orsini, G.; Giuliani, M. Reducing complications in post-bariatric plastic surgery: Our experience and literature review. Acta Bio Med. Atenei Parm. 2019, 90, 475. [Google Scholar]
- De Paep, K.; Van Campenhout, I.; Van Cauwenberge, S.; Dillemans, B. Post-bariatric Abdominoplasty: Identification of Risk Factors for Complications. Obes. Surg. 2021, 31, 3203–3209. [Google Scholar] [CrossRef]
- Gilmartin, J.; Long, A.F.; Soldin, M. Changing body image and well-being: Following the experience of massive weight loss and body contouring surgery. Healthcare 2014, 2, 150–165. [Google Scholar] [CrossRef] [Green Version]
- Plastic Surgery Statistics Report. The American Society of Plastic Surgeons. Available online: https://www.plasticsurgery.org/documents/News/Statistics/2020/plastic-surgery-statistics-full-report-2020.pdf (accessed on 28 May 2022).
- Winocour, J.; Gupta, V.; Ramirez, J.R.; Shack, R.B.; Grotting, J.C.; Higdon, K.K. Abdominoplasty: Risk factors, complication rates, and safety of combined procedures. Plast. Reconstr. Surg. 2015, 136, 597e–606e. [Google Scholar] [CrossRef] [Green Version]
- Momeni, A.; Heier, M.; Bannasch, H.; Stark, G.B. Complications in abdominoplasty: A risk factor analysis. J. Plast. Reconstr. Aesthetic Surg. 2009, 62, 1250–1254. [Google Scholar] [CrossRef] [PubMed]
- Neaman, K.C.; Armstrong, S.D.; Baca, M.E.; Albert, M.; Vander Woude, D.L.; Renucci, J.D. Outcomes of traditional cosmetic abdominoplasty in a community setting: A retrospective analysis of 1008 patients. Plast. Reconstr. Surg. 2013, 131, 403e–410e. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Staalesen, T.; Elander, A.; Strandell, A.; Bergh, C. A systematic review of outcomes of abdominoplasty. J. Plast. Surg. Hand Surg. 2012, 46, 139–144. [Google Scholar] [CrossRef]
- Donato, D.P.; Simpson, A.M.; Garlick, J.W.; Kwok, A.C.; Crombie, C.; Agarwal, J.P. Abdominal contouring and male gender: Analysis of complications using the national quality improvement program database. Ann. Plast. Surg. 2019, 83, 481–487. [Google Scholar] [CrossRef]
- Kim, J.; Stevenson, T.R. Abdominoplasty, liposuction of the flanks, and obesity: Analyzing risk factors for seroma formation. Plast. Reconstr. Surg. 2006, 117, 773–779. [Google Scholar] [CrossRef] [PubMed]
- Rogliani, M.; Silvi, E.; Labardi, L.; Maggiulli, F.; Cervelli, V. Obese and nonobese patients: Complications of abdominoplasty. Ann. Plast. Surg. 2006, 57, 336–338. [Google Scholar] [CrossRef]
- Vastine, V.L.; Morgan, R.F.; Williams, G.S.; Gampper, T.J.; Drake, D.B.; Knox, L.K.; Lin, K.Y. Wound complications of abdominoplasty in obese patients. Ann. Plast. Surg. 1999, 42, 34–39. [Google Scholar] [CrossRef]
- Schlosshauer, T.; Kiehlmann, M.; Jung, D.; Sader, R.; Rieger, U.M. Post-bariatric abdominoplasty: Analysis of 406 cases with focus on risk factors and complications. Aesthetic Surg. J. 2021, 41, 59–71. [Google Scholar] [CrossRef] [PubMed]
- Schlosshauer, T.; Kiehlmann, M.; Jung, D.; Sader, R.; Rieger, U.M. Response to “Comments on ‘Post-Bariatric Abdominoplasty: Analysis of 406 Cases With Focus on Risk Factors and Complications’”. Aesthetic Surg. J. 2020, 40, NP580–NP581. [Google Scholar] [CrossRef] [PubMed]
- Lievain, L.; Aktouf, A.; Auquit-Auckbur, I.; Coquerel-Beghin, D.; Scotte, M.; Milliez, P.Y. Abdominoplasty complications: Particularities of the post-bariatric patients within a 238 patients series. Ann. Chir. Plast. Esthet. 2015, 60, 26–34. (In French) [Google Scholar] [CrossRef] [PubMed]
- Fernandes, J.W.; Damin, R.; Holzmann, M.V.N.; Ribas, G.G.O. Use of an algorithm in choosing abdominoplasty techniques. Rev. Col. Bras. Cir. 2018, 45, e1394. (In Portuguese) [Google Scholar] [CrossRef] [Green Version]
- Mirrafati, S. Abdominoplasty history and techniques. In Aesthetic Surgery of the Abdominal Wall; Springer: Berlin/Heidelberg, Germany, 2005; pp. 62–66. [Google Scholar]
- Herman, C.K.; Hoschander, A.S.; Wong, A. Post-bariatric body contouring. Aesthetic Surg. J. 2015, 35, 672–687. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- González-Ulloa, M. Belt lipectomy. Br. J. Plast. Surg. 1960, 13, 179–186. [Google Scholar] [CrossRef]
- Hunstad, J.P. Body contouring in the obese patient. Clin. Plast. Surg. 1996, 23, 647–670. [Google Scholar] [CrossRef]
- Strauch, B.; Herman, C.; Rohde, C.; Baum, T. Mid-body contouring in the post–bariatric surgery patient. Plast. Reconstr. Surg. 2006, 117, 2200–2211. [Google Scholar] [CrossRef]
- Friedman, T.; Coon, D.O.; Michaels, J.M.; Purnell, C.; Hur, S.; Harris, D.N.; Rubin, J.P. Fleur-de-Lis abdominoplasty: A safe alternative to traditional abdominoplasty for the massive weight loss patient. Plast. Reconstr. Surg. 2010, 125, 1525–1535. [Google Scholar] [CrossRef]
- Vidal, P.; Berner, J.E.; Will, P.A. Managing complications in abdominoplasty: A literature review. Arch. Plast. Surg. 2017, 44, 457. [Google Scholar] [CrossRef] [Green Version]
- Shestak, K.C. 14 Halfway to a Body Lift. In Encyclopedia of Body Sculpting after Massive Weight Loss. 2011. Available online: https://plasticsurgerykey.com/14-halfway-to-a-body-lift/ (accessed on 28 May 2022).
- Matarasso, A.; Schneider, L.F.; Barr, J. The incidence and management of secondary abdominoplasty and secondary abdominal contour surgery. Plast. Reconstr. Surg. 2014, 133, 40–50. [Google Scholar] [CrossRef]
- Marouf, A.; Mortada, H. Complications of Body Contouring Surgery in Postbariatric Patients: A Systematic Review and Meta-Analysis. Aesthetic Plast. Surg. 2021, 45, 2810–2820. [Google Scholar] [CrossRef]
- Neaman, K.C.; Hansen, J.E. Analysis of Complications From Abdominoplasty: A Review of 206 Cases at a University Hospital. Ann. Plast. Surg. 2007, 58, 292–298. Available online: https://journals.lww.com/annalsplasticsurgery/Fulltext/2007/03000/Analysis_of_Complications_From_Abdominoplasty__A.12.aspx (accessed on 28 May 2022). [CrossRef] [PubMed]
- Hensel, J.M.; Lehman, J.A., Jr.; Tantri, M.P.; Parker, M.G.; Wagner, D.S.; Topham, N.S. An Outcomes Analysis and Satisfaction Survey of 199 Consecutive Abdominoplasties. Ann. Plast. Surg. 2001, 46, 357–363. Available online: https://journals.lww.com/annalsplasticsurgery/Fulltext/2001/04000/An_Outcomes_Analysis_and_Satisfaction_Survey_of.1.aspx (accessed on 28 May 2022). [CrossRef] [PubMed]
- Lesko, R.P.; Cheah, M.A.; Sarmiento, S.; Cooney, C.M.; Cooney, D.S. Postoperative Complications of Panniculectomy and Abdominoplasty: A Retrospective Review. Ann. Plast. Surg. 2020, 85, 285–289. [Google Scholar] [CrossRef] [PubMed]
- Greco, J.A.; Castaldo, E.T.; Nanney, L.B.; Wendel, J.J.; Summitt, J.B.; Kelly, K.J.; Braun, S.A.; Hagan, K.F.; Shack, R.B. The effect of weight loss surgery and body mass index on wound complications after abdominal contouring operations. Ann. Plast. Surg. 2008, 61, 235–242. [Google Scholar] [CrossRef] [PubMed]
- Staalesen, T.; Olsén, M.F.; Elander, A. Complications of abdominoplasty after weight loss as a result of bariatric surgery or dieting/postpregnancy. J. Plast. Surg. Hand Surg. 2012, 46, 416–420. [Google Scholar] [CrossRef] [PubMed]
- Chetta, M.D.; Aliu, O.; Tran, B.A.; Abdulghani, M.; Kidwell, K.M.; Momoh, A.O. Complications in body contouring stratified according to weight loss method. Plast. Surg. 2016, 24, 103–106. [Google Scholar] [CrossRef] [Green Version]
- Pajula, S.; Jyränki, J.; Tukiainen, E.; Koljonen, V. Complications after lower body contouring surgery due to massive weight loss unaffected by weight loss method. J. Plast. Reconstr. Aesthetic Surg. JPRAS 2019, 72, 649–655. [Google Scholar] [CrossRef] [Green Version]
- De Kerviler, S.; Hüsler, R.; Banic, A.; Constantinescu, M.A. Body Contouring Surgery Following Bariatric Surgery and Dietetically Induced Massive Weight Reduction: A Risk Analysis. Obes. Surg. 2009, 19, 553–559. [Google Scholar] [CrossRef] [Green Version]
- Brito, Í.M.; Meireles, R.; Baltazar, J.; Brandão, C.; Sanches, F.; Freire-Santos, M.J. Abdominoplasty and Patient Safety: The Impact of Body Mass Index and Bariatric Surgery on Complications Profile. Aesthetic Plast. Surg. 2020, 44, 1615–1624. [Google Scholar] [CrossRef]
- Sirota, M.; Weiss, A.; Billig, A.; Hassidim, A.; Zaga, J.; Adler, N. Abdominoplasty complications—What additional risks do postbariatric patients carry? J. Plast. Reconstr. Aesthetic Surg. JPRAS 2021, 74, 3415–3420. [Google Scholar] [CrossRef]
- Love, A.L.; Billett, H.H. Obesity, bariatric surgery, and iron deficiency: True, true, true and related. Am. J. Hematol. 2008, 83, 403–409. [Google Scholar] [CrossRef] [PubMed]
- Slater, G.H.; Ren, C.J.; Siegel, N.; Williams, T.; Barr, D.; Wolfe, B.; Fielding, G.A. Serum fat-soluble vitamin deficiency and abnormal calcium metabolism after malabsorptive bariatric surgery. J. Gastrointest. Surg. 2004, 8, 48–55; discussion 54–55. [Google Scholar] [CrossRef] [PubMed]
- Shermak, M.A. Body contouring. Plast. Reconstr. Surg. 2012, 129, 963e–978e. [Google Scholar] [CrossRef] [PubMed]
- Shermak, M.A.; Mallalieu, J.; Chang, D. Do preexisting abdominal scars threaten wound healing in abdominoplasty? Eplasty 2010, 10, e14. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2808056/ (accessed on 28 May 2022). [PubMed]
- Parvizi, D.; Friedl, H.; Wurzer, P.; Kamolz, L.; Lebo, P.; Tuca, A.; Rappl, T.; Wiedner, M.; Kuess, K.; Grohmann, M.; et al. A Multiple Regression Analysis of Postoperative Complications after Body-Contouring Surgery: A Retrospective Analysis of 205 Patients: Regression Analysis of Complications. Obes. Surg. 2015, 25, 1482–1490. [Google Scholar] [CrossRef] [PubMed]
- Vasilakis, V.; Lisiecki, J.L.; Kortesis, B.G.; Bharti, G.; Hunstad, J.P. The Effect of Obesity, Bariatric Surgery, and Operative Time on Abdominal Body Contouring Outcomes. Aesthetic Surg. J. 2021, 41, Np1044–Np1052. [Google Scholar] [CrossRef]
- Van der Beek, E.S.; van der Molen, A.M.; van Ramshorst, B. Complications after body contouring surgery in post-bariatric patients: The importance of a stable weight close to normal. Obes. Facts 2011, 4, 61–66. [Google Scholar] [CrossRef]
- Coon, D.; Michaels, J.; Gusenoff, J.A.; Purnell, C.; Friedman, T.; Rubin, J.P. Multiple procedures and staging in the massive weight loss population. Plast. Reconstr. Surg. 2010, 125, 691–698. [Google Scholar] [CrossRef]
- Hurwitz, D.J.; Wright, L. Noninvasive Abdominoplasty. Clin. Plast. Surg. 2020, 47, 379–388. [Google Scholar] [CrossRef]
- Zocchi, M.L. Ultrasonic assisted lipoplasty. Technical refinements and clinical evaluations. Clin. Plast. Surg. 1996, 23, 575–598. Available online: https://www.ncbi.nlm.nih.gov/pubmed/8906391 (accessed on 28 May 2022).
- Irvine Duncan, D. Nonexcisional tissue tightening: Creating skin surface area reduction during abdominal liposuction by adding radiofrequency heating. Aesthetic Surg. J. 2013, 33, 1154–1166. [Google Scholar] [CrossRef] [Green Version]
- Jewell, M.L.; Fodor, P.B.; de Souza Pinto, E.B.; Al Shammari, M.A. Clinical application of VASER--assisted lipoplasty: A pilot clinical study. Aesthetic Surg. J. 2002, 22, 131–146. [Google Scholar] [CrossRef] [PubMed]
- Hoyos, A.E.; Millard, J.A. VASER-assisted high-definition liposculpture. Aesthetic Surg. J. 2007, 27, 594–604. [Google Scholar] [CrossRef] [Green Version]
- Cook, J.; DiBernardo, B.E.; Pozner, J.N. Bipolar Radiofrequency as an Adjunct to Face and Body Contouring: A 745-Patient Clinical Experience. Aesthetic Surg. J. 2021, 41, 685–694. [Google Scholar] [CrossRef]
- Hernandez Zendejas, G.; Reavie, D.W.; Azabache, R.; Guerrerosantos, J. Lipoplasty Combined with Percutaneous Radiofrequency Dermaplasty: A New Strategy for Body Contouring. Aesthetic Plast. Surg. 2020, 44, 455–463. [Google Scholar] [CrossRef]
- Pierazzi, D.M.; Alfieri, E.P.; Cuomo, R.; Bocchiotti, M.A.; Grimaldi, L.; Donniacuo, A.; Zerini, I.; Nisi, G. Ligasure™ Impact and Ligasure™ Small Jaw in Body Contouring after Massive Weight Loss: A New Perspective. J. Investig. Surg. 2022, 35, 659–666. [Google Scholar] [CrossRef] [PubMed]
- Kinney, B.M.; Lozanova, P. High intensity focused electromagnetic therapy evaluated by magnetic resonance imaging: Safety and efficacy study of a dual tissue effect based non-invasive abdominal body shaping. Lasers Surg. Med. 2019, 51, 40–46. [Google Scholar] [CrossRef] [Green Version]
- Rohrich, R.J.; Beran, S.J.; Kenkel, J.M.; Adams, W.P., Jr.; DiSpaltro, F. Extending the role of liposuction in body contouring with ultrasound-assisted liposuction. Plast. Reconstr. Surg. 1998, 101, 1090–1102; discussion 1117–1119. [Google Scholar] [CrossRef]
- Schlosshauer, T.; Kiehlmann, M.; Ramirez, P.; Riener, M.O.; Djedovic, G.; Rieger, U.M. Comparative analysis on the effect of low-thermal plasma dissection device (PEAK PlasmaBlade) versus conventional electro surgery in post-bariatric body-contouring procedures: A retrospective randomised clinical study. Int. Wound J. 2019, 16, 932–939. [Google Scholar] [CrossRef]
- Schlosshauer, T.; Kiehlmann, M.; Riener, M.O.; Sader, R.; Rieger, U.M. Comparative analysis on the effect of low-thermal plasma dissection device (PEAK PlasmaBlade) vs. conventional electrosurgery in post-bariatric abdominoplasty: A retrospective randomised clinical study. Int. Wound J. 2019, 16, 1494–1502. [Google Scholar] [CrossRef]
- Jiang, Z.; Zhang, G.; Huang, J.; Shen, C.; Cai, Z.; Yin, X.; Yin, Y.; Zhang, B. A systematic review of body contouring surgery in post-bariatric patients to determine its prevalence, effects on quality of life, desire, and barriers. Obes. Rev. 2021, 22, e13201. [Google Scholar] [CrossRef]
- Toma, T.; Harling, L.; Athanasiou, T.; Darzi, A.; Ashrafian, H. Does body contouring after bariatric weight loss enhance quality of life? A systematic review of QOL studies. Obes. Surg. 2018, 28, 3333–3341. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Derderian, S.C.; Dewberry, L.C.; Patten, L.; Sitzman, T.J.; Kaizer, A.M.; Jenkins, T.M.; Michalsky, M.P.; Xie, C.; Mitchell, J.E.; Inge, T. Excess skin problems among adolescents after bariatric surgery. Surg. Obes. Relat. Dis. 2020, 16, 993–998. [Google Scholar] [CrossRef] [PubMed]
- Sandvik, J.; Hole, T.; Klockner, C.; Kulseng, B.; Wibe, A. The Impact of Post-bariatric Abdominoplasty on Secondary Weight Regain After Roux-en-Y Gastric Bypass. Front. Endocrinol. 2020, 11, 459. [Google Scholar] [CrossRef] [PubMed]
- Sailon, A.M.; Wasserburg, J.R.; Kling, R.R.; Pasick, C.M.; Taub, P.J. Influence of Large-Volume Liposuction on Metabolic and Cardiovascular Health: A Systematic Review. Ann. Plast. Surg. 2017, 79, 623–630. [Google Scholar] [CrossRef] [PubMed]
- Stapel, B.; Jelinic, M.; Drummond, G.R.; Hartung, D.; Kahl, K.G. Adipose Tissue Compartments, Inflammation, and Cardiovascular Risk in the Context of Depression. Front. Psychiatry 2022, 13, 831358. [Google Scholar] [CrossRef]
- Cai, A.; Maringa, L.; Hauck, T.; Boos, A.M.; Schmitz, M.; Arkudas, A.; Horch, R.E.; Ludolph, I. Body Contouring Surgery Improves Physical Activity in Patients After Massive Weight Loss-a Retrospective Study. Obes. Surg. 2020, 30, 146–153. [Google Scholar] [CrossRef]
- Nielsen, C.; Elander, A.; Staalesen, T.; Al Nouh, M.; Fagevik Olsen, M. Depressive symptoms before and after abdominoplasty among post-bariatric patients—A cohort study. J. Plast. Surg. Hand Surg. 2022, 1–6. [Google Scholar] [CrossRef]
- Paul, M.A.; Opyrchał, J.; Knakiewicz, M.; Jaremków, P.; Duda-Barcik, Ł.; Ibrahim, A.M.S.; Lin, S. J The long-term effect of body contouring procedures on the quality of life in morbidly obese patients after bariatric surgery. PLoS ONE 2020, 15, e0229138. [Google Scholar] [CrossRef] [Green Version]
- Ngaage, L.; Wasicek, P.J.; Puthumana, J.; Kambouris, A.R.; Tannouri, S.; Rada, E.M.; Kligman, M.D.; Rasko, Y.M. A Cross-sectional Analysis of Insurance Coverage of Extremity Contouring After Massive Weight Loss. Ann. Plast. Surg. 2020, 84, 253–256. [Google Scholar] [CrossRef]
- Warner, J.P.; Stacey, D.H.; Sillah, N.M.; Gould, J.C.; Garren, M.J.; Gutowski, K.A. National bariatric surgery and massive weight loss body contouring survey. Plast. Reconstr. Surg. 2009, 124, 926–933. [Google Scholar] [CrossRef]
- Ellison, J.M.; Steffen, K.J.; Sarwer, D.B. Body contouring after bariatric surgery. Eur. Eat. Disord. Rev. 2015, 23, 479–487. [Google Scholar] [CrossRef] [PubMed]
- Al-Hadithy, N.; Aditya, H.; Stewart, K. Does the degree of ptosis predict the degree of psychological morbidity in bariatric patients undergoing reconstruction? Plast. Reconstr. Surg. 2014, 134, 942–950. [Google Scholar] [CrossRef] [PubMed]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sadeghi, P.; Duarte-Bateman, D.; Ma, W.; Khalaf, R.; Fodor, R.; Pieretti, G.; Ciccarelli, F.; Harandi, H.; Cuomo, R. Post-Bariatric Plastic Surgery: Abdominoplasty, the State of the Art in Body Contouring. J. Clin. Med. 2022, 11, 4315. https://doi.org/10.3390/jcm11154315
Sadeghi P, Duarte-Bateman D, Ma W, Khalaf R, Fodor R, Pieretti G, Ciccarelli F, Harandi H, Cuomo R. Post-Bariatric Plastic Surgery: Abdominoplasty, the State of the Art in Body Contouring. Journal of Clinical Medicine. 2022; 11(15):4315. https://doi.org/10.3390/jcm11154315
Chicago/Turabian StyleSadeghi, Payam, Daniela Duarte-Bateman, Wanyan Ma, Ryan Khalaf, R’ay Fodor, Gorizio Pieretti, Feliciano Ciccarelli, Hamed Harandi, and Roberto Cuomo. 2022. "Post-Bariatric Plastic Surgery: Abdominoplasty, the State of the Art in Body Contouring" Journal of Clinical Medicine 11, no. 15: 4315. https://doi.org/10.3390/jcm11154315
APA StyleSadeghi, P., Duarte-Bateman, D., Ma, W., Khalaf, R., Fodor, R., Pieretti, G., Ciccarelli, F., Harandi, H., & Cuomo, R. (2022). Post-Bariatric Plastic Surgery: Abdominoplasty, the State of the Art in Body Contouring. Journal of Clinical Medicine, 11(15), 4315. https://doi.org/10.3390/jcm11154315








