Central Giant Cell Granuloma in the Mandibular Condyle in a Teenager. A Case Report with Literature Review
Abstract
1. Introduction
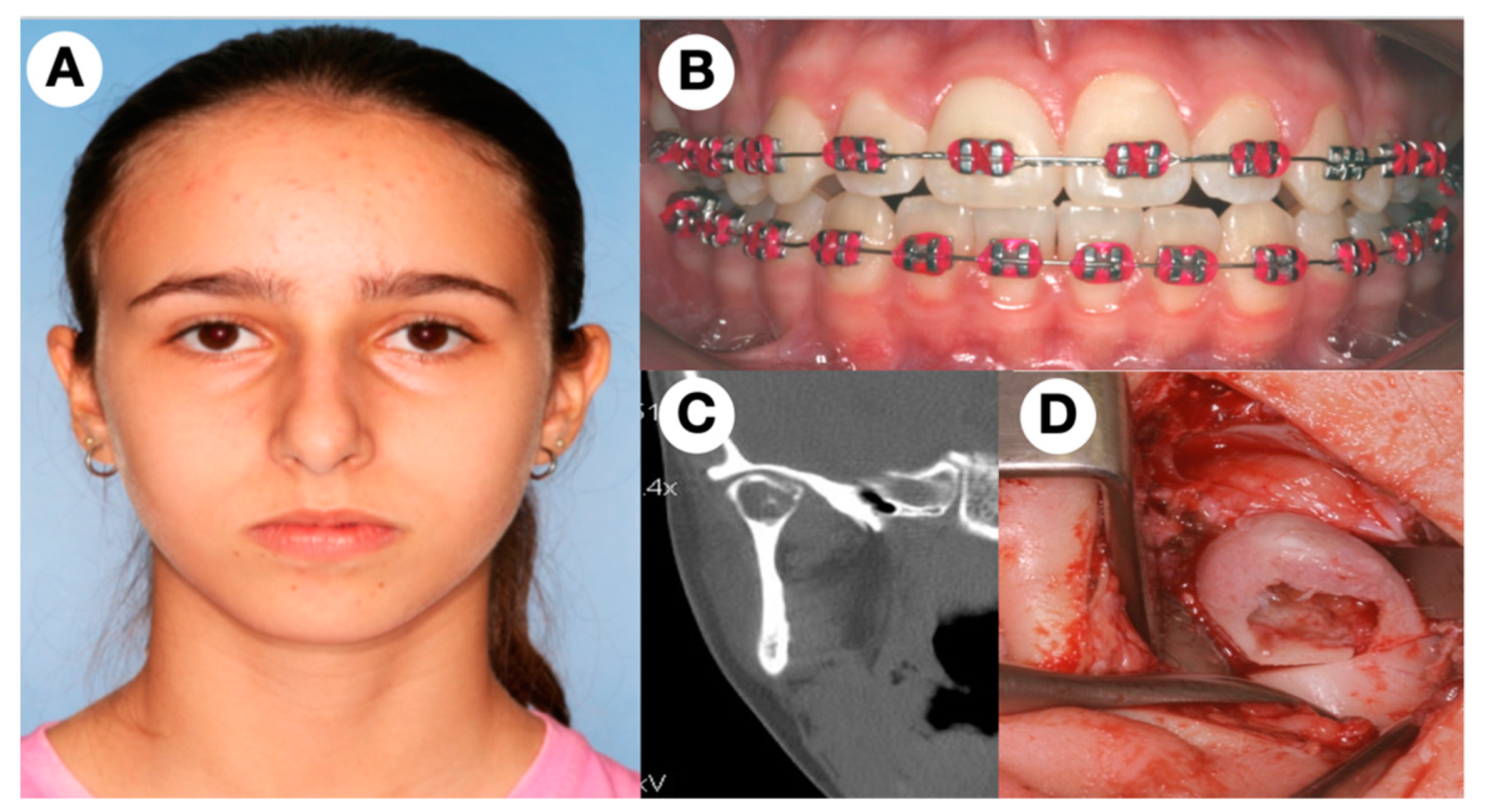
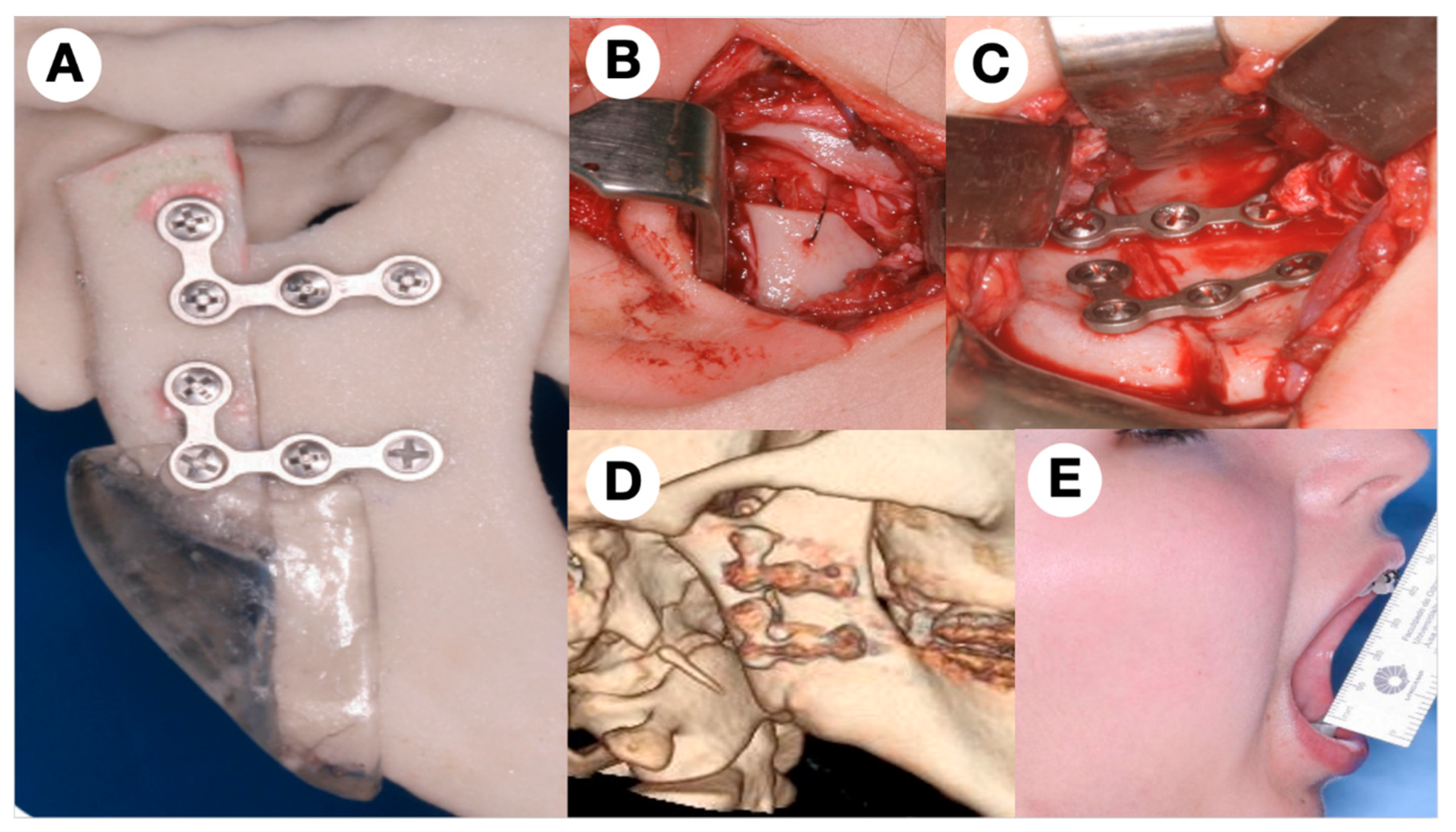
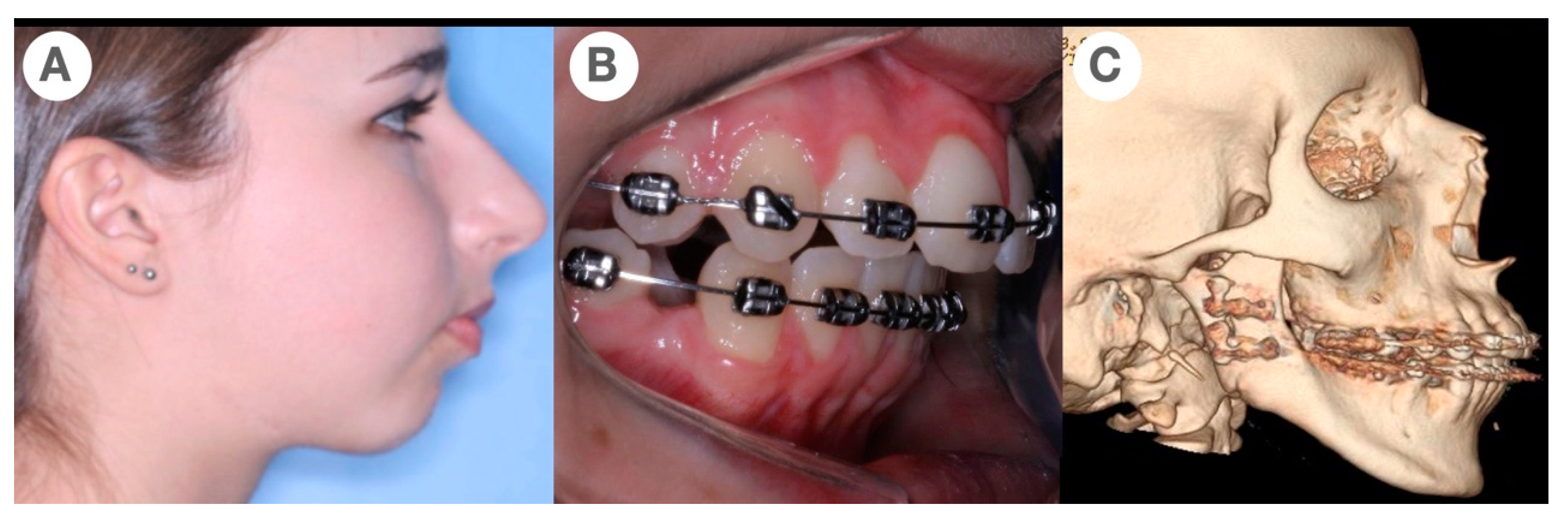
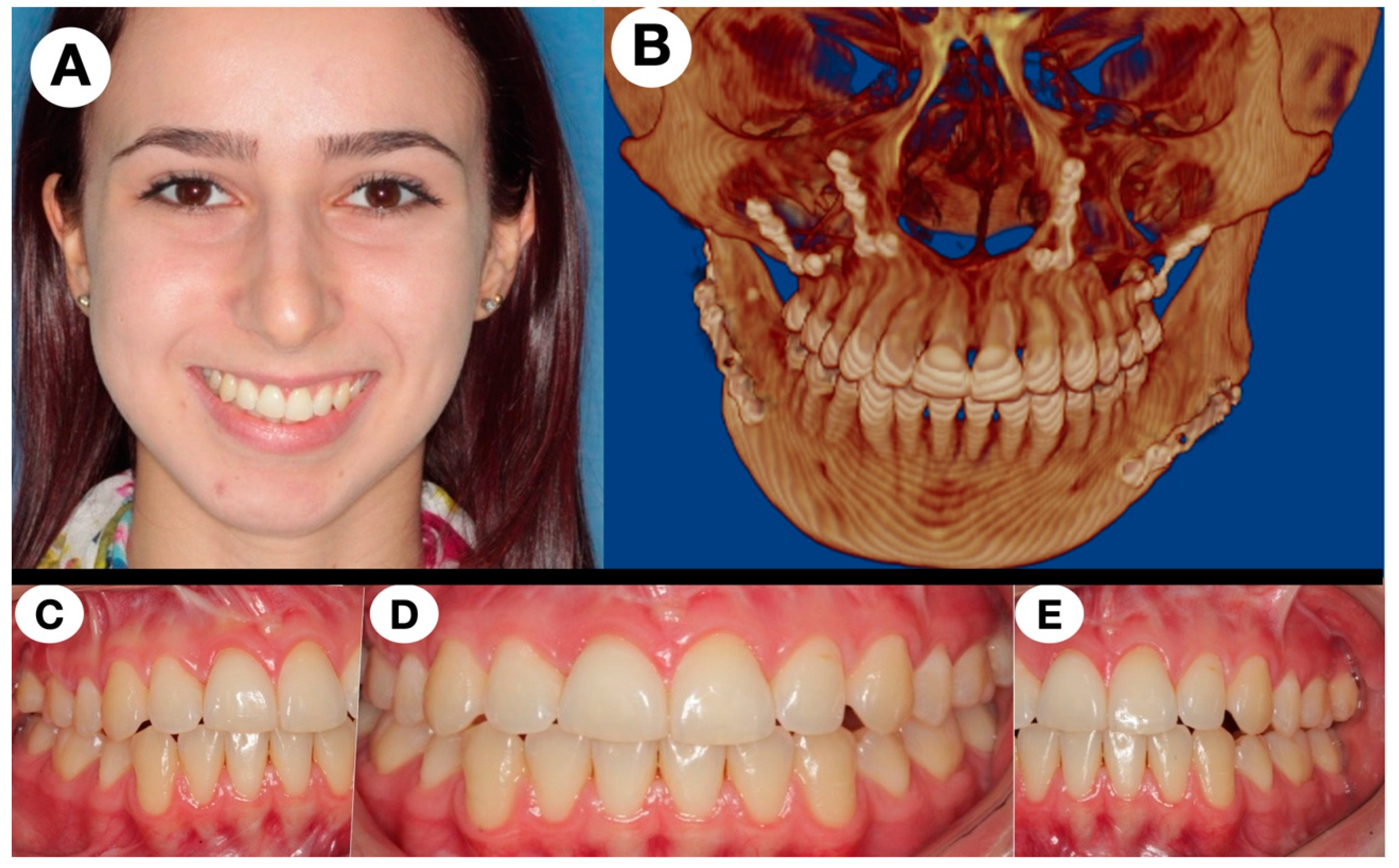
2. The Subject
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ozcan, C.; Apaydın, F.D.; Gorur, K.; Apa, D.D. Peripheral giant cell granuloma of the mandibular condyle presenting as a preauricular mass. Eur. Arch. Otorhinolaryngol. 2005, 262, 178–181. [Google Scholar] [CrossRef] [PubMed]
- Jadu, F.M.; Pharoah, M.J.; Lee, L.; Baker, G.I.; Allidina, A. Central giant cell granuloma of the mandibular condyle: A case report and review of the literature. Dentomaxillofac. Radiol. 2011, 40, 60–64. [Google Scholar] [CrossRef] [PubMed]
- Khanna, J.N.; Ramaswami, R.; Shah, M. Giant cell reparative granuloma of mandibular condyle—A case report. J. Oral Maxillofac. Surg. Med. Pathol. 2018, 30, 515–518. [Google Scholar] [CrossRef]
- Bocchialini, G.; Salvagni, L.; Guerini, A.; Castellani, A. Central giant cell granuloma of the mandibular condyle: A rare case and a literature review. Heliyon 2020, 6, e03085. [Google Scholar] [CrossRef]
- Abu-El-Naaj, I.; Ardekian, L.; Liberman, R.; Peled, M. Central giant cell granuloma of the mandibular condyle: A rare presentation. J. Oral. Maxillofac. Surg. 2002, 60, 939–941. [Google Scholar] [CrossRef]
- Munzenmayer, J.; Tapia, P.; Zeballos, J.; Martínez, A.; Compan, Á.; Urra, A.; Spencer, M.L. Central giant cell granuloma of the mandibular condyle. Case-report. Rev. Clin. Periodoncia Implantol. Rehabil. Oral. 2013, 6, 83–86. [Google Scholar]
- Chang, C.S.; Hsiao, Y.C.; Huang, F.; Chen, P.K.T.; Chen, J.P.; Noordhoff, M.S. Giant cell reparative granuloma of the mandibular condyle: A long-term case report and review of the literature. Plast. Surg. Case Stud. 2016, 2, 44–46. [Google Scholar] [CrossRef]
- Pai, D.; Kamath, A.T.; Kudva, A.; Solomon, M.M.C.; Kumar, S.; Sasikumar, P. Concomitant central giant cell granuloma and Aneurismal Bone Cyst in a Young Child. Case reports in dentistry. Case Rep. Dent. 2017, 2017, 6545848. [Google Scholar] [CrossRef]
- Chuong, R.; Kaban, L.B.; Kozakewich, H.; Perez-Atayde, A. Central Giant Cell Lesions of the Jaws: A Clinicopathologic Study. J. Oral. Maxillofac. Surg. 1986, 44, 708–713. [Google Scholar] [CrossRef]
- Tasanen, A.; von Konow, L.; Nordling, S. Central giant cell lesion in the mandibular condyle: Report of a case. Oral. Surg. Oral. Med. Oral. Pathol. 1978, 45, 532. [Google Scholar] [CrossRef]
- Shensa, D.R.; Nasseri, S. Centeral giant cell reparative granuloma of the mandibular condyle. J. Oral. Surg. 1978, 36, 642. [Google Scholar]
- Sun, Z.J.; Cai, Y.; Zwahlen, R.A.; Zheng, Y.F.; Wang, S.P.; Zhao, Y.Z. Central giant cell granuloma of the jaws: Clinical and radiological evaluation of 22 cases. Skeletal Radiol. 2009, 38, 903–909. [Google Scholar] [CrossRef] [PubMed]
- Gigliotti, J.; Alghamdi, O.; El-Hakim, M.; Makhoul, N. Central giant cell granuloma of the mandibular condyle: A case report, literature review, and discussion of treatment. Oral. Maxillofac. Surg. Cases 2015, 1, 42–46. [Google Scholar] [CrossRef][Green Version]
- Camarini, C.; Tolentino, E. Non-surgical treatment as an alternative for the management of central giant cell granuloma: A systematic review. Clin. Oral. Investig. 2022, 26, 2111–2132. [Google Scholar] [CrossRef] [PubMed]
- Lin, J.; Mecham, J.C.; Ryan Hall, S.; Oh, C.; Lettieri, S. Padiatric mandibular central giant cell granuloma: Neoadjuvant immunotherapy to minimize surgical resection. J. Craniofac. Surg. 2021, 32, e267–e269. [Google Scholar] [CrossRef]
- Nilesh, K.; Dadhich, A.; Patil, R. Management of recurrent central giant cell granuloma of mandible using intralesional corticosteroid with long-term follow-up. BMJ Case Rep. 2020, 14, e237200. [Google Scholar] [CrossRef]
- Lipplaa, A.; Dijkstra, S.; Gelderblom, H. Challenge of denosumab in giant cell tumor of bone, and other giant cell-rich tumors of bone. Curr. Opin. Oncol. 2019, 31, 329–335. [Google Scholar] [CrossRef]
- Dolanmaz, D.; Esen, A.; Mihmanll, A.; Isik, K. Management of central giant cell granuloma of the jaws with intralesional steroid injection and review of the literature. Oral. Maxillofac. Surg. 2016, 20, 203–209. [Google Scholar] [CrossRef]
- Rasband-Lindquist, A.N.; Lindquist, J.D.; Larsen, C.; Thiessen, A.; Girod, D. Nonsurgical options to treat giant-cell tumors of the head and neck: A case report and brief review of the literature. Ear Nose Throat J. 2016, 95, E29–E34. [Google Scholar]
- Costello, B.J.; Rivera, R.; Shand, J.; Mooney, M. Growth and development considerations for craniomaxillofacial surgery. Oral Maxillofac. Surg. Clin. N. Am. 2012, 24, 377–396. [Google Scholar] [CrossRef]
- Resnick, C. Temporomandibular joint reconstruction in growing child. Oral Maxillofac. Surg. Clin. N. Am. 2018, 30, 109–121. [Google Scholar] [CrossRef] [PubMed]
- Parmar, B.S.; Garg, B.; Mehta, R.D.; Midha, A.; Thakkar, D. Ramus condyle unit reconstruction using vertical ramus osteotomy in the temporomandibular joint ankylosis. J. Maxillofac. Oral Surg. 2015, 14, 630–636. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Al-Moraissi, E.A.; El-Sharkawy, T.M.; Mounair, R.M.; El-Ghareeb, T.I. A systematic review and meta-analysis of the clinical outcomes for various surgical modalities in the management of temporomandibular joint ankylosis. Int. J. Oral Maxillofac. Surg. 2015, 44, 470–482. [Google Scholar] [CrossRef] [PubMed]
- De Meurechy, N.; Mommaerts, M.Y. Alloplastic temporomandibular joint replacement systems: A systematic review of their history. Int. J. Oral. Maxillofac. Surg. 2018, 47, 743–754. [Google Scholar] [CrossRef] [PubMed]
- Mercuri, L.G. Patient-fitted (“custom”) alloplastic temporomandibular joint replacement technique. Atlas Oral Maxillofac. Surg. Clin. N. Am. 2011, 19, 233–242. [Google Scholar] [CrossRef]
- Bach, E.; Sigaux, N.; Fauvernier, M.; Cousin, A.-S. Reason for failure of total temporomandibular joint replacement: A systematic review and meta-analysis. Int. J. Oral Maxillofac. Surg. 2022, in press. [Google Scholar] [CrossRef]
- Sidebottom, A. Alloplastic or autogenous reconstruction of the TMJ. J. Oral Biol. Craniofac. Res. 2013, 3, 135–139. [Google Scholar] [CrossRef]
| Author/Year | Age/Sex | Clinical Findings | Imaging | Treatment | Follow-Up |
|---|---|---|---|---|---|
| Tasanen et al. (1978) [10] | 59/M | Right painless slow-growing pre-auricular swelling. Mouth-opening limitation | Well-defined multilocular radiolucency—25 mm (right condyle) | Resection + reconstruction with CCG | 21 months NRD |
| Shensa/Nasseri, (1978) [11] | 15/M | Expansive mass. Asymptomatic | Well-defined radiolucency | Enucleation | NI |
| Abu-El-Naaj et al. (2002) [5] | 15/F | Left preauricular swelling (2 months). Asymptomatic. Normal mandibular motion | Well-defined unilocular radiolucency (3 × 2 cm), left condyle | Enucleation | 6 months NRD |
| Özcan et al. (2005) [1] | 44/F | Right preauricular swelling (2-year evolution). Pain | CT—hypodense 2 × 2 cm. MRI rim-like hypodense T1. Peripheral calcification | Curettage | 1 year NRD |
| Sun et al. (2009) [12] | NI (1 out of 22 cases) | Pain and tenderness | Well-defined radiolucency. Extending to the coronoid process | Curettage | NI |
| Jadu et al. (2011) [2] | 31/M | Painful slow-growing left pre-auricular swelling (2 years). Limited mouth opening | CT—Well defined, expansile (3.5 cm), with a granular bone pattern | Enucleation then resection after recurrence | 4 years NRD |
| Munzenmayer et al. (2013) [6] | 19/F | Asymptomatic. No occlusal or mandibular movement disorders | Well-defined multilocular radiolucency (4 × 2.2 × 1.5 cm), with granular bone pattern (left condyle) | Resection + reconstruction with NVFF | 2 years NRD |
| Gigliotti et al. (2015) [13] | 29/M | Firm and nodular left pre-auricular swelling (6 months). No occlusal changes. Discomfort during the mandibular function. | Left multilocular radiolucency with thin cortices 5.5 × 3.8 × 3.4 cm | Resection + reconstruction with CCG | 1 year NRD |
| Chang et al. (2016) [7] | 37/F | Hardened left pre-auricular mass 4 × 3 cm. Asymptomatic | Well-defined radiolucent and radiopaque areas involving two cortical in left condyle + ramus | Resection + reconstruction with CCG | 10 years NRD |
| Pai et al. (2017) [8] | 2/M | Progressive and firm increase in the right preauricular region. Painless. (4 months) | Expansive multinucleated radiolucent lesion (4.2 × 3.5 × 4 cm) with cortical perforation. | Resection + reconstruction with CCG | 18 months NRD |
| Khanna et al. (2018) [3] | 22/M | Right preauricular swelling (4 months). Pain and TMJ movements restricted | Large lesion extending to the coronoid with areas of cortical perforation at multiple places. | Resection + 2.4 mm reconstruction plate with condylar head | 1 year NRD |
| Bocchialini et al. (2020) [4] | 60/F | Right preauricular pain (1 year). Mouth-opening limitation. | A large radiolucent lesion with distortion of the right condyle | Enucleation | 1 year NRD |
| Present case | 11/F | No swellings, joint pain during mandibular motion (1 year) | Well-defined radiolucent lesion on the right mandible head | Resection + sliding vertical ramus osteotomy + later orthognathic surgery | 13 years NRD |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cantanhede, A.L.C.; Olate, S.; de Assis, A.F.; de Moraes, M. Central Giant Cell Granuloma in the Mandibular Condyle in a Teenager. A Case Report with Literature Review. J. Clin. Med. 2022, 11, 4239. https://doi.org/10.3390/jcm11144239
Cantanhede ALC, Olate S, de Assis AF, de Moraes M. Central Giant Cell Granuloma in the Mandibular Condyle in a Teenager. A Case Report with Literature Review. Journal of Clinical Medicine. 2022; 11(14):4239. https://doi.org/10.3390/jcm11144239
Chicago/Turabian StyleCantanhede, André Luís Costa, Sergio Olate, Adriano Freitas de Assis, and Márcio de Moraes. 2022. "Central Giant Cell Granuloma in the Mandibular Condyle in a Teenager. A Case Report with Literature Review" Journal of Clinical Medicine 11, no. 14: 4239. https://doi.org/10.3390/jcm11144239
APA StyleCantanhede, A. L. C., Olate, S., de Assis, A. F., & de Moraes, M. (2022). Central Giant Cell Granuloma in the Mandibular Condyle in a Teenager. A Case Report with Literature Review. Journal of Clinical Medicine, 11(14), 4239. https://doi.org/10.3390/jcm11144239







