Key Components, Current Practice and Clinical Outcomes of ERAS Programs in Patients Undergoing Orthopedic Surgery: A Systematic Review
Abstract
1. Introduction
1.1. ERAS in Orthopedic Surgery
1.2. ERAS Protocols
2. Materials and Methods
2.1. Eligibility Criteria
2.2. Information Source and Search Strategies
2.3. Selection Process
2.4. Assessment of Methodological Quality
2.5. Data Collection Process and Synthesis Methods
3. Results
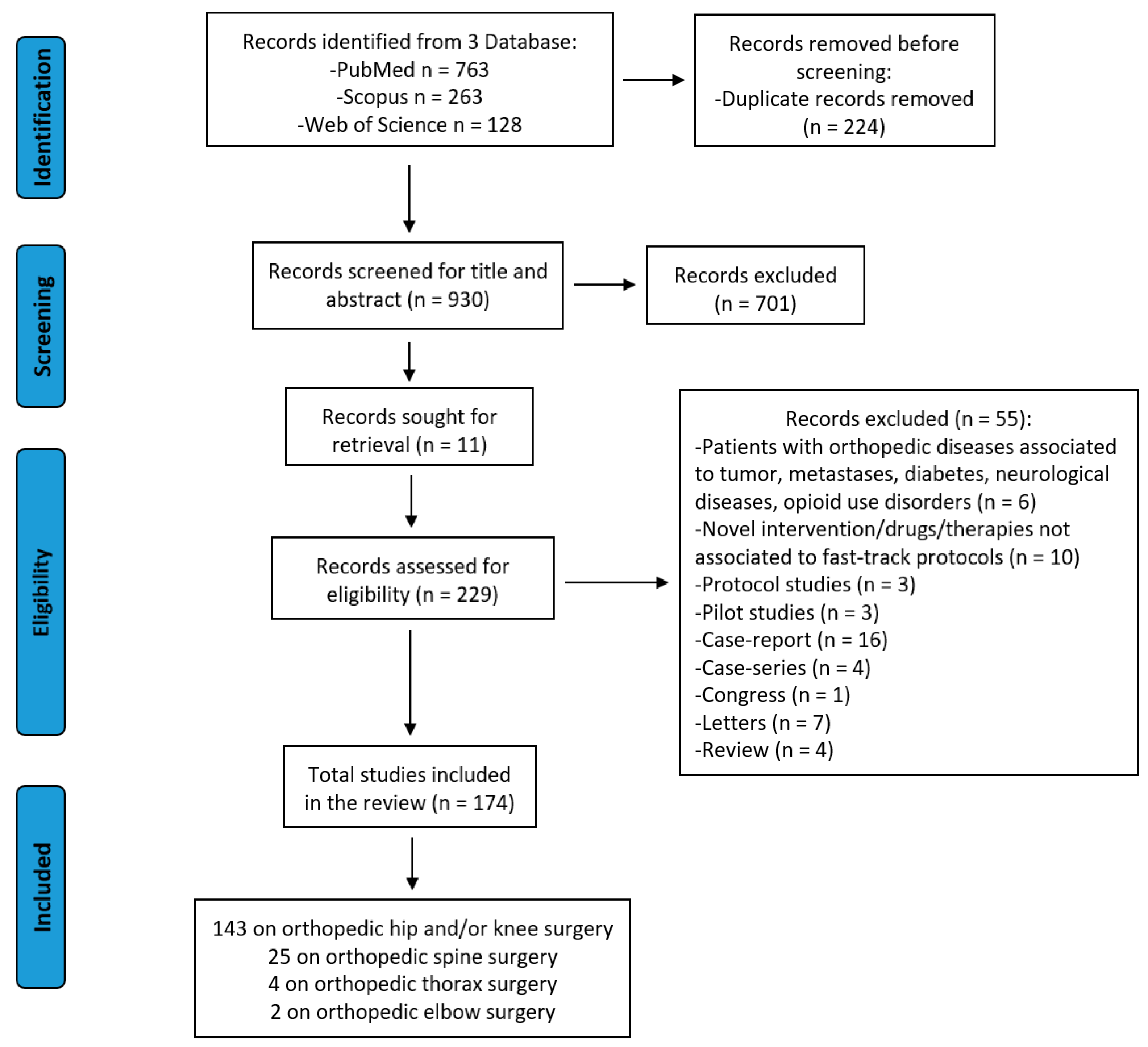
3.1. Study Selection and Characteristics
3.2. Assessment of Methodological Quality
3.3. Study Results and Synthesis
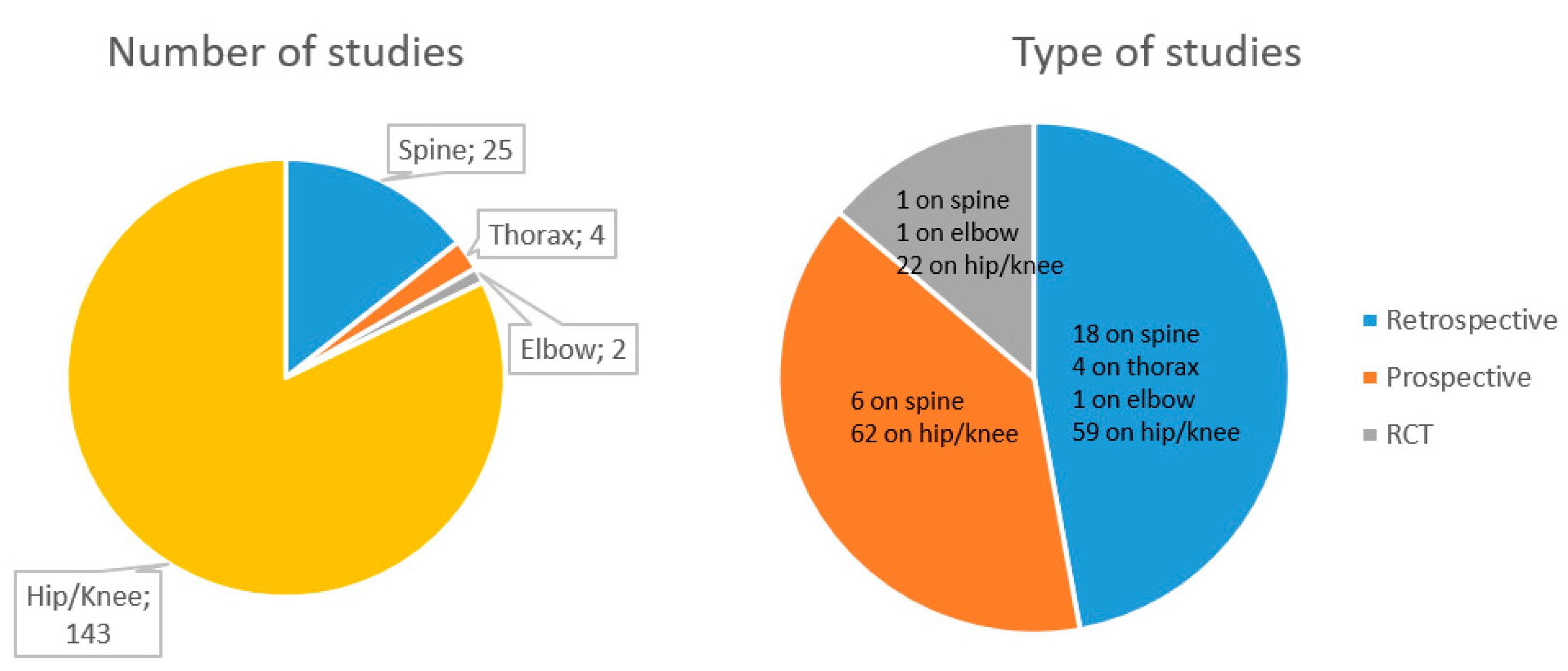
3.3.1. Types of Orthopedic Surgery in ERAS Protocols
3.3.2. Key Components in ERAS Protocols
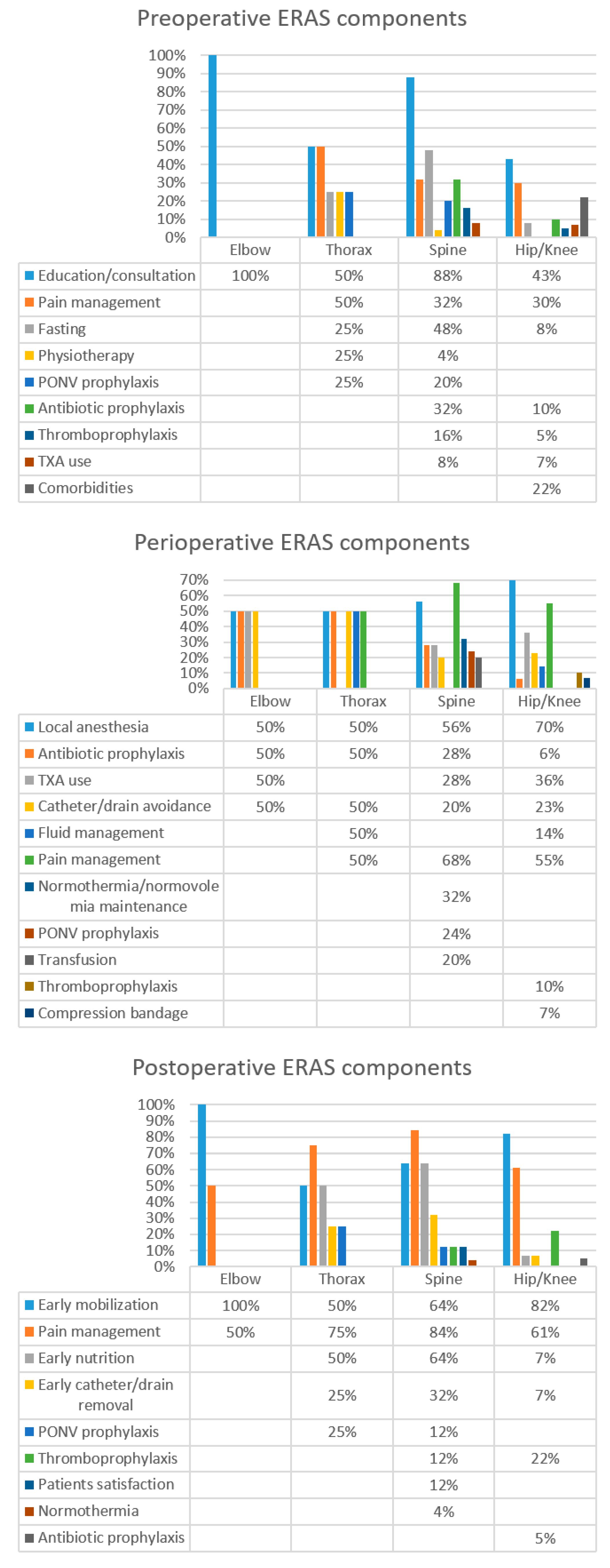
Preoperative
- -
- Elbow: In elbow orthopedic surgery, the most common preoperative interventions were patient education and the provision of information (on the surgical procedure, analgesia, anesthesia, LOS, and physiotherapy) (100%).
- -
- Thorax: The most common preoperative interventions reported in thorax orthopedic surgery were patient education and the provision of information (50%). Supplementary pre-emptive interventions were analgesia and multimodal pain management (50%) (defined as the use of one or more analgesic modes, such as acetaminophen, pregabalin, gabapentin, ketamine, non-steroidal anti-inflammatory drugs (NSAIDs), and cyclooxygenase (COX)-2 inhibitors)), clear fluid fasting (25%), physiotherapy (25%) and nausea and vomiting prophylaxis (25%).
- -
- Spine: In spine orthopedic surgery, among the principal interventions of ERAS protocol were patient education and the provision of information associated with a multidisciplinary consultation (geriatric, psychological, nutritional, behavioral health) (88%). Clear fluid and solid fluid fasting for 2–6 h before surgery (48%), pre-emptive analgesia and multimodal pain management (32%), antimicrobial/antibiotic prophylaxis (32%), nausea and vomiting prevention (20%), thromboprophylaxis (16%), tranexamic acid (TXA) (including oral or parenteral formulations) used to minimize bleeding (8%) and physiotherapy (4%) were other key interventions in spine orthopedic surgery.
- -
- Hip and/or knee: For hip and/or knee orthopedic surgery, the most common pre-operative interventions were patient education, the provision of information, and multidisciplinary consultation (43.3%), followed by pre-emptive analgesia and multimodal pain management (30%), comorbidities assessment (21.7%), antimicrobial/antibiotic prophylaxis (9.7%), clear fluid and solid fluid fasting for 2–6 h before surgery (8.3%), TXA use (7%) and thromboprophylaxis (4.9%).
Perioperative
- -
- Elbow: In elbow orthopedic surgery frequent perioperative interventions were local anesthesia (50%), antimicrobial/antibiotic prophylaxis (50%), TXA use (50%) and avoidance of catheter/drain (50%).
- -
- Thorax: The most common perioperative interventions in thorax surgery included local anesthesia (50%), avoidance of catheter/drain (50%), antibiotic/antimicrobial prophylaxis (50%), fluid management (50%) and multimodal pain management (50%).
- -
- Spine: For spine surgery, perioperative components were multimodal analgesia and pain management (68%), local anesthesia (56%), normothermia/normovolemia maintenance (32%), TXA use (28%), antimicrobial/antibiotic prophylaxis (28%), postoperative nausea and vomiting prophylaxis (24%), transfusion control (20%) and avoidance of catheter/drain (20%).
- -
- Hip and/or knee: For hip and/or knee orthopedic surgery, the most common perioperative elements were local anesthesia (70%), multimodal pain management (55.2%), TXA use (36%), avoidance of catheter/drain (23%), intraoperative fluid management (14%), thromboprophylaxis (10.4%), compression bandage use (7%) and antimicrobial/antibiotic prophylaxis (5.6%).
Postoperative
- -
- Elbow: The principal postoperative elements were early mobilization and rehabilitation/physiotherapy within 24 h (100% of studies) and multimodal analgesia and pain management (50%).
- -
- Thorax: In thorax surgery, key postoperative elements were represented by multimodal analgesia and pain management (75% of studies), early mobilization and rehabilitation/physiotherapy (50%), early nutrition (50%), catheter/drain removal within 24 h after surgery (25%) and nausea and vomiting prophylaxis (25%)
- -
- Spine: In spine surgery, postoperative elements were multimodal analgesia and pain management (84% of studies), early mobilization and rehabilitation/physiotherapy (64%), early nutrition (64%), catheter/drain removal within 24 h after surgery (32%), nausea and vomiting prophylaxis (12% in spine), thromboprophylaxis (12% spine), patient satisfaction survey (12%) and normothermia (4%).
- -
- Hip and/or knee: Principal postoperative elements were early mobilization and rehabilitation/physiotherapy (82% of studies), multimodal analgesia and pain management (61%), thromboprophylaxis (22.3%), early nutrition (7%), catheter/drain removal within 24 h after surgery (7%) and antimicrobial/antibiotic prophylaxis (5%).
3.4. Outcomes and Clinical Evidence of ERAS Protocols
4. Discussion
4.1. Limitation and Strengths
4.2. Future Prospects
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Global Orthopedic Surgery Market Report, 2017 to 2022—Procedure Volume Trends by Type, Country, and Region (2019). Available online: https://www.globenewswire.com/news-release/2019/08/13/1901268/0/en/Global-Orthopedic-Surgery-Market-Report-2017-to-2022-Procedure-Volume-Trends-by-Type-Country-and-Region.html (accessed on 1 August 2021).
- Capone, A.; Congia, S.; Civinini, R.; Marongiu, G. Periprosthetic fractures: Epidemiology and current treatment. Rev. Clin Cases Min. Bone Metab. 2017, 14, 189–196. [Google Scholar] [CrossRef] [PubMed]
- Jiang, M.; Liu, S.; Deng, H.; Liang, X.; Bo, Z. The efficacy and safety of fast track surgery (FTS) in patients after hip fracture surgery: A meta-analysis. J. Orthop. Surg. Res. 2021, 16, 162. [Google Scholar] [CrossRef] [PubMed]
- Pennestrì, F.; Maffulli, N.; Sirtori, P.; Perazzo, P.; Negrini, F.; Banfi, G.; Peretti, G.M. Blood management in ERAS orthopedic surgery: An evidence-based narrative review. J. Orthop. Surg. Res. 2019, 14, 263. [Google Scholar] [CrossRef]
- Kehlet, H. Multimodal approach to control postoperative pathophysiology and rehabilitation. Br. J. Anaesth. 1997, 78, 606–617. [Google Scholar] [CrossRef]
- Kehlet, H.; Wilmore, D.W. Evidence-based surgical care and the evolution of ERAS surgery. Ann. Surg. 2008, 248, 189–198. [Google Scholar] [CrossRef] [PubMed]
- Kehlet, H. Future perspectives and research initiatives in ERAS surgery. Langenbecks Arch. Surg. 2006, 391, 495–498. [Google Scholar] [CrossRef] [PubMed]
- Husted, H. ERAS hip and knee arthroplasty: Clinical and organizational aspects. Acta Orthop. Suppl. 2012, 83, 1–39. [Google Scholar] [CrossRef] [PubMed]
- McDonald, S.; Page, M.J.; Beringer, K.; Wasiak, J.; Sprowson, A. Preoperative education for hip or knee replacement. Cochrane Database Syst. Rev. 2014, 5, CD003526. [Google Scholar] [CrossRef]
- Specht, K.; Kjaersgaard-Andersen, P.; Pedersen, B.D. Patient experience in ERAS hip and knee arthroplasty—A qualitative study. J. Clin. Nurs. 2016, 25, 836–845. [Google Scholar] [CrossRef]
- Kennedy, D.; Wainwright, A.; Pereira, L.; Robarts, S.; Dickson, P.; Christian, J.; Webster, F. A qualitative study of patient education needs for hip and knee replacement. BMC Musculoskelet. Disord. 2017, 18, 413. [Google Scholar] [CrossRef]
- Husted, H.; Lunn, T.H.; Troelsen, A.; Gaarn-Larsen, L.; Kristensen, B.B.; Kehlet, H. Why still in hospital after ERAS hip and knee arthroplasty? Acta Orthop. 2011, 82, 679–684. [Google Scholar] [CrossRef] [PubMed]
- Reay, P.A.; Horner, B.; Duggan, R. The patient’s experience of early discharge following total hip replacement. Int. J. Orthop. Trauma Nurs. 2015, 19, 131–139. [Google Scholar] [CrossRef] [PubMed]
- Kaye, A.D.; Urman, R.D.; Cornett, E.M.; Hart, B.M.; Chami, A.; Gayle, J.A.; Fox, C.J. Enhanced recovery pathways in orthopedic surgery. J. Anaesthesiol. Clin. Pharmacol. 2019, 35, S35–S39. [Google Scholar] [PubMed]
- Berg, U.; Berg, M.; Rolfson, O.; Erichsen-Andersson, A. ERAS program of elective joint replacement in hip and knee-patients’ experiences of the clinical pathway and care process. J. Orthop. Surg. Res. 2019, 14, 186. [Google Scholar] [CrossRef]
- Wainwright, T.W.; Memtsoudis, S.G.; Kehlet, H. ERAS hip and knee arthroplasty...how fast? Br. J. Anaesth. 2021, 126, 348–349. [Google Scholar] [CrossRef]
- Centre for reviews and dissemination. Systematic Reviews: CRD’s Guidance for Undertaking Reviews in Health Care; Centre for Reviews and Dissemination, University of York: York, UK, 2006. [Google Scholar]
- Tugwell, P.; Tovey, D. PRISMA 2020. J. Clin. Epidemiol. 2021, 134, A5–A6. [Google Scholar] [CrossRef]
- Study Quality Assessment Tools (2013). Available online: https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools (accessed on 1 August 2021).
- Soffin, E.M.; Wetmore, D.S.; Barber, L.A.; Vaishnav, A.S.; Beckman, J.D.; Albert, T.J.; Gang, C.H.; Qureshi, S.A. An enhanced recovery after surgery pathway: Association with rapid discharge and minimal complications after anterior cervical spine surgery. Neurosurg. Focus 2019, 46, E9. [Google Scholar] [CrossRef]
- Wang, D.; Wang, H.Y.; Luo, Z.Y.; Meng, W.K.; Pei, F.X.; Li, Q.; Zhou, Z.K.; Zeng, W.N. Blood-conserving efficacy of multiple doses of oral tranexamic acid associated with an enhanced-recovery programme in primary total knee arthroplasty: A randomized controlled trial. Bone Jt. J. 2018, 100-B, 1025–1032. [Google Scholar] [CrossRef]
- Wang, D.; Zhu, H.; Meng, W.K.; Wang, H.Y.; Luo, Z.Y.; Pei, F.X.; Li, Q.; Zhou, Z.K. Comparison of oral versus intra-articular tranexamic acid in enhanced-recovery primary total knee arthroplasty without tourniquet application: A randomized controlled trial. BMC Musculoskelet. Disord. 2018, 19, 85. [Google Scholar] [CrossRef]
- Wang, H.Y.; Wang, L.; Luo, Z.Y.; Wang, D.; Tang, X.; Zhou, Z.K.; Pei, F.X. Intravenous and subsequent long-term oral tranexamic acid in enhanced-recovery primary total knee arthroplasty without the application of a tourniquet: A randomized placebo-controlled trial. BMC Musculoskelet Disord 2019, 20, 478. [Google Scholar] [CrossRef]
- Jørgensen, C.C.; Kehlet, H.; Lundbeck Foundation Centre for ERAS Hip and Knee Replacement Collaborative Group. Fall-related admissions after ERAS total hip and knee arthroplasty—Cause of concern or consequence of success? Clin. Interv. Aging 2013, 8, 1569–1577. [Google Scholar] [CrossRef] [PubMed]
- Aasvang, E.K.; Lunn, T.H.; Hansen, T.B.; Kristensen, P.W.; Solgaard, S.; Kehlet, H. Chronic pre-operative opioid use and acute pain after ERAS total knee arthroplasty. Acta. Anaesthesiol. Scand. 2016, 60, 529–536. [Google Scholar] [CrossRef] [PubMed]
- Adams, C.T.; O’Connor, C.M.; Young, J.R.; Anoushiravani, A.A.; Doherty, B.S.; Congiusta, F. Outcomes of a Total Joint Arthroplasty Enhanced Recovery Program in a Community Hospital Setting. J. Arthroplast. 2021, 36, S173–S178. [Google Scholar] [CrossRef] [PubMed]
- Adeyemo, E.A.; Aoun, S.G.; Barrie, U.; Nguyen, M.L.; Badejo, O.; Pernik, M.N.; Christian, Z.; Dosselman, L.J.; El Ahmadieh, T.Y.; Hall, K.; et al. Enhanced Recovery After Surgery Reduces Postoperative Opioid Use and 90-Day Readmission Rates After Open Thoracolumbar Fusion for Adult Degenerative Deformity. Neurosurgery 2021, 88, 295–300. [Google Scholar] [CrossRef]
- Alvis, B.D.; Amsler, R.G.; Leisy, P.J.; Feng, X.; Shotwell, M.S.; Pandharipande, P.P.; Ajmal, M.; McHugh, M.; Walia, A.; Hughes, C.G. Effects of an anesthesia perioperative surgical home for total knee and hip arthroplasty at a Veterans Affairs Hospital: A quality improvement before-and-after cohort study. Can. J. Anaesth. 2021, 68, 367–375. [Google Scholar] [CrossRef] [PubMed]
- Andreasen, S.E.; Holm, H.B.; Jørgensen, M.; Gromov, K.; Kjærsgaard-Andersen, P.; Husted, H. Time-driven Activity-based Cost of ERAS Total Hip and Knee Arthroplasty. J. Arthroplast. 2017, 32, 1747–1755. [Google Scholar] [CrossRef]
- Ascione, F.; Braile, A.; Romano, A.M.; di Giunta, A.; Masciangelo, M.; Senorsky, E.H.; Samuelsson, K.; Marzano, N. Experience-optimised fast track improves outcomes and decreases complications in total knee arthroplasty. Knee 2020, 27, 500–508. [Google Scholar] [CrossRef]
- Auyong, D.B.; Allen, C.J.; Pahang, J.A.; Clabeaux, J.J.; MacDonald, K.M.; Hanson, N.A. Reduced Length of Hospitalization in Primary Total Knee Arthroplasty Patients Using an Updated Enhanced Recovery After Orthopedic Surgery (ERAS) Pathway. J. Arthroplast. 2015, 30, 1705–1709. [Google Scholar] [CrossRef]
- Awada, H.N.; Luna, I.E.; Kehlet, H.; Wede, H.R.; Hoevsgaard, S.J.; Aasvang, E.K. Postoperative cognitive dysfunction is rare after ERAS hip- and knee arthroplasty—But potentially related to opioid use. J. Clin. Anesth. 2019, 57, 80–86. [Google Scholar] [CrossRef]
- Bandholm, T.; Thorborg, K.; Lunn, T.H.; Kehlet, H.; Jakobsen, T.L. Knee pain during strength training shortly following ERAS total knee arthroplasty: A cross-sectional study. PLoS ONE 2014, 9, e91107. [Google Scholar] [CrossRef]
- Berg, U.; BüLow, E.; Sundberg, M.; Rolfson, O. No increase in readmissions or adverse events after implementation of ERAS program in total hip and knee replacement at 8 Swedish hospitals: An observational before-and-after study of 14,148 total joint replacements 2011–2015. Acta Orthop. 2018, 89, 522–527. [Google Scholar] [CrossRef] [PubMed]
- Berg, U.; W-Dahl, A.; Rolfson, O.; Nauclér, E.; Sundberg, M.; Nilsdotter, A. Influence of ERAS programs on patient-reported outcomes in total hip and knee replacement (THR/TKR) at Swedish hospitals 2011–2015: An observational study including 51,169 THR and 8393 TKR operations. Acta Orthop. 2020, 91, 306–312. [Google Scholar] [CrossRef] [PubMed]
- Berg, U.; W-Dahl, A.; Nilsdotter, A.; Nauclér, E.; Sundberg, M.; Rolfson, O. ERAS Programs in Total Hip and Knee Replacement at Swedish Hospitals-Influence on 2-Year Risk of Revision and Mortality. J. Clin. Med. 2021, 10, 1680. [Google Scholar] [CrossRef]
- Bernaus, M.; Novellas, M.; Bartra, A.; Núñez, J.H.; Anglès, F. Local infiltration analgesia does not have benefits in ERAS hip arthroplasty programmes: A double-blind, randomised, placebo-controlled, clinical trial. Hip Int. 2021. [Google Scholar] [CrossRef] [PubMed]
- Berthelsen, C.B.; Kristensson, J. The SICAM-trial: Evaluating the effect of spouses’ involvement through case management in older patients’ ERAS programmes during and after total hip replacement. J. Adv. Nurs. 2017, 73, 112–126. [Google Scholar] [CrossRef]
- Birznieks, M.; Golubovska, I.; Repða, L.; Èeròavska, I.; Âbols, J.; Muste, A.; Ļu, I.; Miščuks, A. ERAS surgery and early rehabilitation for total hip replacement in hospital of traumatology and orthopaedics. Proc. Latv. Acad. Sci. 2019, 73, 419–424. [Google Scholar] [CrossRef]
- Bjerregaard, L.S.; Bogø, S.; Raaschou, S.; Troldborg, C.; Hornum, U.; Poulsen, A.M.; Bagi, P.; Kehlet, H. Incidence of and risk factors for postoperative urinary retention in ERAS hip and knee arthroplasty. Acta Orthop. 2015, 86, 183–188. [Google Scholar] [CrossRef]
- Bjerregaard, L.S.; Hornum, U.; Troldborg, C.; Bogoe, S.; Bagi, P.; Kehlet, H. Postoperative Urinary Catheterization Thresholds of 500 versus 800 ml after ERAS Total Hip and Knee Arthroplasty: A Randomized, Open-label, Controlled Trial. Anesthesiology 2016, 124, 1256–1264. [Google Scholar] [CrossRef]
- Cao, Q.; He, Z.; Fan, Y.; Meng, J.; Yuan, T.; Zhao, J.; Bao, N. Effects of tourniquet application on enhanced recovery after surgery (ERAS) and ischemia-reperfusion post-total knee arthroplasty: Full- versus second half-course application. J. Orthop. Surg. 2020, 28, 2309499019896026. [Google Scholar] [CrossRef]
- Castle, H.; Dragovic, M.; Waterreus, A. Mobilization after joint arthroplasty surgery: Who benefits from standing within 12 hours? ANZ J. Surg. 2021, 91, 1271–1276. [Google Scholar] [CrossRef]
- Castorina, S.; Guglielmino, C.; Castrogiovanni, P.; Szychlinska, M.A.; Ioppolo, F.; Massimino, P.; Leonardi, P.; Maci, C.; Iannuzzi, M.; Di Giunta, A.; et al. Clinical evidence of traditional vs fast track recovery methodologies after total arthroplasty for osteoarthritic knee treatment. A retrospective observational study. Muscles Ligaments Tendons J. 2018, 7, 504–513. [Google Scholar] [CrossRef] [PubMed]
- Christelis, N.; Wallace, S.; Sage, C.E.; Babitu, U.; Liew, S.; Dugal, J.; Nyulasi, I.; Mutalima, N.; Tran, T.; Myles, P.S. An enhanced recovery after surgery program for hip and knee arthroplasty. Med. J. Aust. 2015, 202, 363–368. [Google Scholar] [CrossRef] [PubMed]
- Concina, C.; Crucil, M.; Fabbro, S.; Gherlinzoni, F. Do tourniquet and drainage influence fast track in total knee arthroplasty? Our results on 151 cases. Acta Biomed. 2019, 90, 123–129. [Google Scholar] [CrossRef] [PubMed]
- Collett, G.; Insley, A.P.; Michaelis, S.; Shaji, S.; Feierstein, B.; Martell, J.R. Reduction of Opioid Use with Enhanced Recovery Program for Total Knee Arthroplasty. Fed. Pract. 2021, 38, 212–219. [Google Scholar] [CrossRef]
- Cui, H.; Sun, Z.; Ruan, J.; Yu, Y.; Fan, C. Effect of enhanced recovery after surgery (ERAS) pathway on the postoperative outcomes of elbow arthrolysis: A randomized controlled trial. Int. J. Surg. 2019, 68, 78–84. [Google Scholar] [CrossRef]
- D’Amato, T.; Martorelli, F.; Fenocchio, G.; Simili, V.; Kon, E.; Di Matteo, B.; Scardino, M. Tapentadol vs oxycodone/naloxone in the management of pain after total hip arthroplasty in the fast track setting: An observational study. J. Exp. Orthop. 2019, 6, 36. [Google Scholar] [CrossRef]
- d’Astorg, H.; Fière, V.; Dupasquier, M.; Vieira, T.D.; Szadkowski, M. Enhanced recovery after surgery (ERAS) protocol reduces LOS without additional adverse events in spine surgery. Orthop. Traumatol. Surg. Res. 2020, 106, 1167–1173. [Google Scholar] [CrossRef]
- Dagal, A.; Bellabarba, C.; Bransford, R.; Zhang, F.; Chesnut, R.M.; O’Keefe, G.E.; Wright, D.R.; Dellit, T.H.; Painter, I.; Souter, M.J. Enhanced Perioperative Care for Major Spine Surgery. Spine 2019, 44, 959–966. [Google Scholar] [CrossRef]
- Davies, L.; Bainton, K.; Milne, R.; Lewis, P. Primary lower limb joint replacement and tranexamic acid: An observational cohort study. Arthroplast. Today 2018, 4, 330–334. [Google Scholar] [CrossRef]
- Dawson-Bowling, S.J.; Jha, S.; Chettiar, K.K.; East, D.J.; Gould, G.C.; Apthorp, H.D. A multidisciplinary enhanced recovery programme allows discharge within two days of total hip replacement; three- to five-year results of 100 patients. Hip Int. 2014, 24, 167–174. [Google Scholar] [CrossRef]
- De Ladoucette, A.; Mertl, P.; Henry, M.P.; Bonin, N.; Tracol, P.; Courtin, C.; Jenny, J.Y.; French Society of Orthopaedic Surgery and Traumatology (SoFCOT). Fast track protocol for primary total hip arthroplasty in non-trauma cases reduces the length of hospital stay: Prospective French multicenter study. Orthop. Traumatol. Surg. Res. 2020, 106, 1527–1531. [Google Scholar] [CrossRef] [PubMed]
- Debono, B.; Corniola, M.V.; Pietton, R.; Sabatier, P.; Hamel, O.; Tessitore, E. Benefits of Enhanced Recovery After Surgery for fusion in degenerative spine surgery: Impact on outcome, length of stay, and patient satisfaction. Neurosurg. Focus 2019, 46, E6. [Google Scholar] [CrossRef]
- Debono, B.; Sabatier, P.; Boniface, G.; Bousquet, P.; Lescure, J.P.; Garnaud, V.; Hamel, O.; Lonjon, G. Implementation of enhanced recovery after surgery (ERAS) protocol for anterior cervical discectomy and fusion: A propensity score-matched analysis. Eur. Spine J. 2021, 30, 560–567. [Google Scholar] [CrossRef] [PubMed]
- Deiter, J.; Ponzio, D.; Grau, L.; Griffiths, S.; Ong, A.; Post, Z.; Doucette, D.; Orozco, F. Efficacy of adductor canal block protocol implementation in a multimodal pain management protocol for total knee arthroplasty. J. Clin. Orthop. Trauma 2020, 11, 118–121. [Google Scholar] [CrossRef]
- den Hartog, Y.M.; Mathijssen, N.M.C.; Hannink, G.; Vehmeijer, S.B.W. Which patient characteristics influence length of hospital stay after primary total hip arthroplasty in a ‘ERAS’ setting? Bone Jt. J. 2015, 97-B, 19–23. [Google Scholar] [CrossRef] [PubMed]
- den Hartog, Y.M.; Hannink, G.; van Dasselaar, N.T.; Mathijssen, N.M.; Vehmeijer, S.B. Which patient-specific and surgical characteristics influence postoperative pain after THA in a ERAS setting? BMC Musculoskelet. Disord. 2017, 18, 363. [Google Scholar] [CrossRef]
- Didden, A.G.M.; Punt, I.M.; Feczko, P.Z.; Lenssen, A.F. Enhanced recovery in usual health care improves functional recovery after total knee arthroplasty. Int. J. Orthop. Trauma. Nurs. 2019, 34, 9–15. [Google Scholar] [CrossRef]
- Ding, Z.C.; Xu, B.; Liang, Z.M.; Wang, H.Y.; Luo, Z.Y.; Zhou, Z.K. Limited Influence of Comorbidities on Length of Stay after Total Hip Arthroplasty: Experience of Enhanced Recovery after Surgery. Orthop. Surg. 2020, 12, 153–161. [Google Scholar] [CrossRef]
- Drosos, G.I.; Ververidis, A.; Valkanis, C.; Tripsianis, G.; Stavroulakis, E.; Vogiatzaki, T.; Kazakos, K. A randomized comparative study of topical versus intravenous tranexamic acid administration in enhanced recovery after surgery (ERAS) total knee replacement. J. Orthop. 2016, 13, 127–131. [Google Scholar] [CrossRef][Green Version]
- Drosos, G.I.; Kougioumtzis, I.E.; Tottas, S.; Ververidis, A.; Chatzipapas, C.; Tripsianis, G.; Tilkeridis, K. The results of a stepwise implementation of a ERAS program in total hip and knee replacement patients. J. Orthop. 2020, 21, 100–108. [Google Scholar] [CrossRef]
- Dwyer, A.J.; Tarassoli, P.; Thomas, W.; Porter, P. Enhanced recovery program in total hip arthroplasty. Indian J. Orthop. 2012, 46, 407–412. [Google Scholar] [CrossRef] [PubMed]
- Dwyer, A.J.; Thomas, W.; Humphry, S.; Porter, P. Enhanced recovery programme for total knee replacement to reduce the length of hospital stay. J. Orthop. Surg. 2014, 22, 150–154. [Google Scholar] [CrossRef]
- Fenelon, C.; Galbraith, J.G.; Kearsley, R.; Motherway, C.; Condon, F.; Lenehan, B. Saving Blood and Reducing Costs: Updating Blood Transfusion Practice in Lower Limb Arthroplasty. Ir. Med J. 2018, 111, 730. [Google Scholar] [PubMed]
- Feng, C.; Zhang, Y.; Chong, F.; Yang, M.; Liu, C.; Liu, L.; Huang, C.; Huang, C.; Feng, X.; Wang, X.; et al. Establishment and Implementation of an Enhanced Recovery After Surgery (ERAS) Pathway Tailored for Minimally Invasive Transforaminal Lumbar Interbody Fusion Surgery. World Neurosurg. 2019, 129, e317–e323. [Google Scholar] [CrossRef] [PubMed]
- Fletcher, N.D.; Bellaire, L.L.; Dilbone, E.S.; Ward, L.A.; Bruce, R.W.J. Variability in length of stay following neuromuscular spinal fusion. Spine Deform. 2020, 8, 725–732. [Google Scholar] [CrossRef] [PubMed]
- Fletcher, N.D.; Murphy, J.S.; Austin, T.M.; Bruce, R.W.J.; Harris, H.; Bush, P.; Yu, A.; Kusumoto, H.; Schmitz, M.L.; Devito, D.P.; et al. Short term outcomes of an enhanced recovery after surgery (ERAS) pathway versus a traditional discharge pathway after posterior spinal fusion for adolescent idiopathic scoliosis. Spine Deform. 2021, 9, 1013–1019. [Google Scholar] [CrossRef]
- Fransen, B.L.; Hoozemans, M.J.M.; Argelo, K.D.S.; Keijser, L.C.M.; Burger, B.J. ERAS total knee arthroplasty improved clinical and functional outcome in the first 7 days after surgery: A randomized controlled pilot study with 5-year follow-up. Arch. Orthop. Trauma. Surg. 2018, 138, 1305–1316. [Google Scholar] [CrossRef]
- Frassanito, L.; Vergari, A.; Nestorini, R.; Cerulli, G.; Placella, G.; Pace, V.; Rossi, M. Enhanced recovery after surgery (ERAS) in hip and knee replacement surgery: Description of a multidisciplinary program to improve management of the patients undergoing major orthopedic surgery. Musculoskelet. Surg. 2020, 104, 87–92. [Google Scholar] [CrossRef]
- Füssenich, W.; Gerhardt, D.M.; Pauly, T.; Lorenz, F.; Olieslagers, M.; Braun, C.; van Susante, J.L. A comparative health care inventory for primary hip arthroplasty between Germany versus the Netherlands. Is there a downside effect to ERAS surgery with regard to patient satisfaction and functional outcome? Hip Int. 2020, 30, 423–430. [Google Scholar] [CrossRef]
- Galbraith, J.G.; Fenelon, C.; Gibbons, J.; Kelly, G.A.; Bennett, D. Enhanced recovery in lower limb arthroplasty in the Irish setting. Ir. J. Med. Sci. 2017, 186, 687–691. [Google Scholar] [CrossRef]
- Glassou, E.N.; Pedersen, A.B.; Hansen, T.B. Risk of re-admission, reoperation, and mortality within 90 days of total hip and knee arthroplasty in ERAS departments in Denmark from 2005 to 2011. Acta Orthop. 2014, 85, 493–500. [Google Scholar] [CrossRef] [PubMed]
- Gomez, M.; Marc, C.; Talha, A.; Ruiz, N.; Noublanche, S.; Gillibert, A.; Bergman, S.; Rony, L.; Maynard, V.; Hubert, L.; et al. Fast track care for pertrochanteric hip fractures: How does it impact length of stay and complications? Orthop. Traumatol. Surg. Res. 2019, 105, 979–984. [Google Scholar] [CrossRef] [PubMed]
- Gomez, M.; Rony, L.; Marc, C.; Talha, A.; Ruiz, N.; Noublanche, S.; Gillibert, A.; Bergman, S.; Maynard, V.; Hubert, L. ERAS care for pertrochanteric hip fracture: What impact on function and autonomy after discharge? Orthop. Traumatol. Surg. Res. 2020, 106, 633–637. [Google Scholar] [CrossRef] [PubMed]
- Götz, J.S.; Leiss, F.; Maderbacher, G.; Meyer, M.; Reinhard, J.; Zeman, F.; Grifka, J.; Greimel, F. Implementing ERAS in total hip arthroplasty: Rapid mobilization with low need for pain medication and low pain values: Retrospective analysis of 102 consecutive patients. Zeitschrift für Rheumatologie 2021. online ahead of print. [Google Scholar] [CrossRef]
- Gromov, K.; Willendrup, F.; Palm, H.; Troelsen, A.; Husted, H. ERAS pathway for reduction of dislocated hip arthroplasty reduces surgical delay and length of stay. Acta Orthop. 2015, 86, 335–338. [Google Scholar] [CrossRef] [PubMed]
- Gromov, K.; Troelsen, A.; Raaschou, S.; Sandhold, H.; Nielsen, C.S.; Kehlet, H.; Husted, H. Tissue Adhesive for Wound Closure Reduces Immediate Postoperative Wound Dressing Changes After Primary TKA: A Randomized Controlled Study in Simultaneous Bilateral TKA. Clin. Orthop. Relat. Res. 2019, 477, 2032–2038. [Google Scholar] [CrossRef]
- Gromov, K.; Petersen, P.B.; Jørgensen, C.C.; Troelsen, A.; Kehlet, H.; Lundbeck Foundation Centre for ERAS Hip and Knee Replacement Collaborative Group. Unicompartmental knee arthroplasty undertaken using a ERAS protocol. Bone Jt. J. 2020, 102-B, 1167–1175. [Google Scholar] [CrossRef]
- Gupta, A. The effectiveness of geriatrician-led comprehensive hip fracture collaborative care in a new acute hip unit based in a general hospital setting in the UK. J. R. Coll. Physicians Edinb. 2014, 44, 20–26. [Google Scholar] [CrossRef]
- Halawi, M.J.; Caminiti, N.; Cote, M.P.; Lindsay, A.D.; Williams, V.J. The Most Significant Risk Factors for Urinary Retention in ERAS Total Joint Arthroplasty are Iatrogenic. J. Arthroplast. 2019, 34, 136–139. [Google Scholar] [CrossRef]
- Hansson, S.; Rolfson, O.; Åkesson, K.; Nemes, S.; Leonardsson, O.; Rogmark, C. Complications and patient-reported outcome after hip fracture. A consecutive annual cohort study of 664 patients. Injury 2015, 46, 2206–2211. [Google Scholar] [CrossRef]
- den Hartog, Y.M.; Mathijssen, N.M.C.; Vehmeijer, S.B.W. Total hip arthroplasty in an outpatient setting in 27 selected patients. Acta Orthop. 2015, 86, 667–670. [Google Scholar] [CrossRef] [PubMed]
- He, B.; Li, Y.; Xu, S.; Ou, Y.; Zhao, J. Tranexamic Acid for Blood Loss after Transforaminal Posterior Lumbar Interbody Fusion Surgery: A Double-Blind, Placebo-Controlled, Randomized Study. BioMed Res. Int. 2020, 2020, 8516504. [Google Scholar] [CrossRef] [PubMed]
- Heo, D.H.; Park, C.K. Clinical results of percutaneous biportal endoscopic lumbar interbody fusion with application of enhanced recovery after surgery. Neurosurg. Focus 2019, 46, E18. [Google Scholar] [CrossRef]
- Herndon, C.L.; Martinez, R.; Sarpong, N.O.; Geller, J.A.; Shah, R.P.; Cooper, H.J. Spinal Anesthesia Using Chloroprocaine is Safe, Effective, and Facilitates Earlier Discharge in Selected ERAS Total Hip Arthroplasty. Arthroplast. Today 2020, 6, 305–308. [Google Scholar] [CrossRef] [PubMed]
- Higgins, M.; Jayakumar, P.; Kortlever, J.T.P.; Rijk, L.; Galvain, T.; Drury, G.; Dekker, A.P.; Westbrook, A. Improving resource utilisation and outcomes after total knee arthroplasty through technology-enabled patient engagement. Knee 2020, 27, 469–476. [Google Scholar] [CrossRef]
- Holm, B.; Bandholm, T.; Lunn, T.H.; Husted, H.; Aalund, P.K.; Hansen, T.B.; Kehlet, H. Role of preoperative pain, muscle function, and activity level in discharge readiness after ERAS hip and knee arthroplasty. Acta Orthop. 2014, 85, 488–492. [Google Scholar] [CrossRef]
- Holmes, D.M.; Polites, S.F.; Roskos, P.L.; Moir, C.R. Opioid use and length of stay following minimally invasive pectus excavatum repair in 436 patients—Benefits of an enhanced recovery pathway. J. Pediatr. Surg. 2019, 54, 1976–1983. [Google Scholar] [CrossRef]
- Hoorntje, A.; Koenraadt, K.L.M.; Boevé, M.G.; van Geenen, R.C.I. Outpatient unicompartmental knee arthroplasty: Who is afraid of outpatient surgery? Knee Surg. Sports Traumatol. Arthrosc. 2017, 25, 759–766. [Google Scholar] [CrossRef]
- Huang, Z.; Zhang, J.; Di, Z.; Zeng, Z. A comprehensive program for enhanced management of femoral neck fractures including an enhanced recovery after surgery program: A retrospective study. Medicine 2021, 100, e24331. [Google Scholar] [CrossRef]
- Husted, H.; Otte, K.S.; Kristensen, B.B.; Kehlet, H. ERAS revision knee arthroplasty. A feasibility study. Acta Orthop. 2011, 82, 438–440. [Google Scholar] [CrossRef]
- Husted, H.; Jensen, C.M.; Solgaard, S.; Kehlet, H. Reduced length of stay following hip and knee arthroplasty in Denmark 2000–2009: From research to implementation. Arch. Orthop. Trauma. Surg. 2012, 132, 101–104. [Google Scholar] [CrossRef] [PubMed]
- Husted, H.; Jørgensen, C.C.; Gromov, K.; Kehlet, H.; Lundbeck Foundation Center for ERAS Hip and Knee Replacement Collaborative Group. Does BMI influence hospital stay and morbidity after ERAS hip and knee arthroplasty? Acta Orthop. 2016, 87, 466–472. [Google Scholar] [CrossRef] [PubMed]
- Imbelloni, L.E.; Gomes, D.; Braga, R.L.; de Morais Filho, G.B.; da Silva, A. Clinical strategies to accelerate recovery after surgery orthopedic femur in elderly patients. Anesth. Essays Res. 2014, 8, 156–161. [Google Scholar] [CrossRef] [PubMed]
- Jenny, J.Y.; Bulaid, Y.; Boisrenoult, P.; Bonin, N.; Henky, P.; Tracol, P.; Chouteau, J.; Courtin, C.; Henry, M.P.; Schwartz, C.; et al. French Society of Orthopaedic Surgery, Traumatology (SofCOT). Bleeding and thromboembolism risk of standard antithrombotic prophylaxis after hip or knee replacement within an enhanced recovery program. Orthop. Traumatol. Surg. Res. 2020, 106, 1533–1538. [Google Scholar] [CrossRef] [PubMed]
- Jensen, C.B.; Troelsen, A.; Nielsen, C.S.; Otte, N.K.S.; Husted, H.; Gromov, K. Why are patients still in hospital after ERAS, unilateral unicompartmental knee arthroplasty. Acta Orthop. 2020, 91, 433–438. [Google Scholar] [CrossRef]
- Jensen, C.B.; Petersen, P.B.; Jørgensen, C.C.; Kehlet, H.; Troelsen, A.; Gromov, K.; Lundbeck Foundation Centre for ERAS Hip and Knee Replacement Collaborative Group. Length of Stay and 90-Day Readmission/Complication Rates in Unicompartmental Versus Total Knee Arthroplasty: A Propensity-Score-Matched Study of 10,494 Procedures Performed in a ERAS Setup. J. Bone Jt. Surg. Am. 2021, 103, 1063–1071. [Google Scholar] [CrossRef]
- Jiang, H.H.; Jian, X.F.; Shangguan, Y.F.; Qing, J.; Chen, L.B. Effects of Enhanced Recovery After Surgery in Total Knee Arthroplasty for Patients Older Than 65 Years. Orthop. Surg. 2019, 11, 229–235. [Google Scholar] [CrossRef]
- Jørgensen, C.C.; Kehlet, H.; Lundbeck Foundation Centre for ERAS Hip and Knee Replacement Collaborative Group. Role of patient characteristics for ERAS hip and knee arthroplasty. Br. J. Anaesth. 2013, 110, 972–980. [Google Scholar] [CrossRef]
- Jørgensen, C.C.; Pitter, F.T.; Kehlet, H.; Lundbeck Foundation Center for ERAS Hip and Knee Replacement Collaborative Group. Safety aspects of preoperative high-dose glucocorticoid in primary total knee replacement. Br. J. Anaesth. 2017, 119, 267–275. [Google Scholar] [CrossRef][Green Version]
- Jørgensen, C.C.; Gromov, K.; Petersen, P.B.; Kehlet, H.; Lundbeck Foundation Centre for ERAS Hip and Knee Replacement Collaborative Group. Influence of day of surgery and prediction of LOS > 2 days after ERAS hip and knee replacement. Acta Orthop. 2021, 92, 170–175. [Google Scholar] [CrossRef]
- Julien-Marsollier, F.; Michelet, D.; Assaker, R.; Doval, A.; Louisy, S.; Madre, C.; Simon, A.L.; Ilharreborde, B.; Brasher, C.; Dahmani, S. Enhanced recovery after surgical correction of adolescent idiopathic scoliosis. Paediatr. Anaesth. 2020, 30, 1068–1076. [Google Scholar] [CrossRef] [PubMed]
- Kang, Y.; Liu, J.; Chen, H.; Ding, W.; Chen, J.; Zhao, B.; Yin, X. Enhanced recovery after surgery (ERAS) in elective intertrochanteric fracture patients result in reduced length of hospital stay (LOS) without compromising functional outcome. J. Orthop. Surg. Res. 2019, 14, 209. [Google Scholar] [CrossRef] [PubMed]
- Kerr, H.L.; Armstrong, L.A.; Beard, L.; Teichmann, D.; Mutimer, J. Challenges to the orthopaedic arthroplasty enhanced recovery programme. J. Perioper. Pract. 2017, 27, 15–19. [Google Scholar] [CrossRef] [PubMed]
- Kilic, E.T.; Tastan, N.O.; Sarikaya, C.; Naderi, S. The Application of an Enhanced Recovery After Surgery to Spine Instrumentation. Turk. Neurosurg. 2020, 30, 707–713. [Google Scholar] [CrossRef] [PubMed]
- Klapwijk, L.C.M.; Mathijssen, N.M.C.; Van Egmond, J.C.; Verbeek, B.M.; Vehmeijer, S.B.W. The first 6 weeks of recovery after primary total hip arthroplasty with fast track. Acta Orthop. 2017, 88, 140–144. [Google Scholar] [CrossRef] [PubMed]
- Klement, M.R.; Bullock, W.M.; Nickel, B.T.; Lampley, A.J.; Seyler, T.M.; Green, C.L.; Wellman, S.S.; Bolognesi, M.P.; Grant, S.A. Continuous adductor canal blockade facilitates increased home discharge and decreased opioid consumption after total knee arthroplasty. Knee 2019, 26, 679–686. [Google Scholar] [CrossRef]
- Kolodziej, L.; Bohatyrewicz, A.; Jurewicz, A.; Szczypiór-Piasecka, K.; Przybył, K. Simultaneous Bilateral Minimally Invasive Direct Anterior Approach Total Hip Arthroplasty with fast track Protocol. Ortop. Traumatol. Rehabil. 2020, 22, 17–24. [Google Scholar] [CrossRef]
- Kort, N.P.; Bemelmans, Y.; Vos, R.; Schotanus, M.G.M. Low incidence of postoperative urinary retention with the use of a nurse-led bladder scan protocol after hip and knee arthroplasty: A retrospective cohort study. Eur. J. Orthop. Surg. Traumatol. 2018, 28, 283–289. [Google Scholar] [CrossRef]
- Krenk, L.; Rasmussen, L.S.; Hansen, T.B.; Bogø, S.; Søballe, K.; Kehlet, H. Delirium after ERAS hip and knee arthroplasty. Br. J. Anaesth. 2012, 108, 607–611. [Google Scholar] [CrossRef]
- Krenk, L.; Kehlet, H.; Hansen, T.B.; Solgaard, S.; Soballe, K.; Rasmussen, L.S. Cognitive dysfunction after ERAS hip and knee replacement. Anesth. Analg. 2014, 118, 1034–1040. [Google Scholar] [CrossRef]
- Lamplot, J.D.; Wagner, E.R.; Manning, D.W. Multimodal pain management in total knee arthroplasty: A prospective randomized controlled trial. J. Arthroplast. 2014, 29, 329–334. [Google Scholar] [CrossRef] [PubMed]
- Larsen, K.; Hansen, T.B.; Søballe, K.; Kehlet, H. Patient-reported outcome after ERAS knee arthroplasty. Knee Surg. Sports Traumatol. Arthrosc. 2012, 20, 1128–1135. [Google Scholar] [CrossRef] [PubMed]
- Larsson, G.; Strömberg, R.U.; Rogmark, C.; Nilsdotter, A. Prehospital fast track care for patients with hip fracture: Impact on time to surgery, hospital stay, post-operative complications and mortality a randomised, controlled trial. Injury 2016, 47, 881–886. [Google Scholar] [CrossRef] [PubMed]
- Leiss, F.; Götz, J.S.; Maderbacher, G.; Meyer, M.; Reinhard, J.; Zeman, F.; Grifka, J.; Greimel, F. Excellent Functional Outcome and Quality of Life after Primary Cementless Total Hip Arthroplasty (THA) Using an Enhanced Recovery Setup. J. Clin. Med. 2021, 10, 621. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Li, H.; Xv, Z.K.; Wang, J.; Yu, Q.F.; Chen, G.; Li, F.C.; Ren, Y.; Chen, Q.X. Enhanced recovery care versus traditional care following laminoplasty: A retrospective case-cohort study. Medicine 2018, 97, e13195. [Google Scholar] [CrossRef]
- Li, Z.E.; Lu, S.B.; Kong, C.; Sun, W.Z.; Wang, P.; Zhang, S.T. Impact of Compliance with an Enhanced Recovery After Surgery Program on the Outcomes Among Elderly Patients Undergoing Lumbar Fusion Surgery. Clin. Interv. Aging 2020, 15, 2423–2430. [Google Scholar] [CrossRef]
- Li, J.; Rai, S.; Ze, R.; Tang, X.; Liu, R.; Hong, P. Enhanced recovery care versus traditional non-ERAS care following osteotomies in developmental dysplasia of the hip in children: A retrospective case-cohort study. BMC Musculoskelet. Disord. 2020, 21, 234. [Google Scholar] [CrossRef]
- Li, Z.E.; Lu, S.B.; Kong, C.; Sun, W.Z.; Wang, P.; Zhang, S.T. Comparative short-term outcomes of enhanced recovery after surgery (ERAS) program and non-ERAS traditional care in elderly patients undergoing lumbar arthrodesis: A retrospective study. BMC Musculoskelet. Disord. 2021, 22, 283. [Google Scholar] [CrossRef]
- Li, Z.; Li, B.; Wang, G.; Wang, K.; Chen, J.; Liang, Y.; Tang, X.; Yang, Y. Impact of enhanced recovery nursing combined with limb training on knee joint function and neurological function after total knee arthroplasty in patients with knee osteoarthritis. Am. J. Transl. Res. 2021, 13, 6864–6872. [Google Scholar]
- Lindberg-Larsen, V.; Bandholm, T.Q.; Zilmer, C.K.; Bagger, J.; Hornsleth, M.; Kehlet, H. Preoperative methylprednisolone does not reduce loss of knee-extension strength after total knee arthroplasty A randomized, double-blind, placebo-controlled trial of 61 patients. Acta Orthop. 2017, 88, 543–549. [Google Scholar] [CrossRef]
- Lindberg-Larsen, V.; Petersen, P.B.; Jans, Ø.; Beck, T.; Kehlet, H. Effect of pre-operative methylprednisolone on orthostatic hypotension during early mobilization after total hip arthroplasty. Acta Anaesthesiol. Scand. 2018, 62, 882–892. [Google Scholar] [CrossRef]
- Lindberg-Larsen, V.; Kehlet, H.; Bagger, J.; Madsbad, S. Preoperative High-Dose Methylprednisolone and Glycemic Control Early After Total Hip and Knee Arthroplasty: A Randomized, Double-Blind, Placebo-Controlled Trial. Anesth. Analg. 2018, 127, 906–913. [Google Scholar] [CrossRef]
- Lindberg-Larsen, M.; Pitter, F.T.; Husted, H.; Kehlet, H.; Jørgensen, C.C.; Lundbeck Foundation Centre for ERAS Hip and Knee Replacement Collaborative Group. Simultaneous vs staged bilateral total knee arthroplasty: A propensity-matched case-control study from nine ERAS centres. Arch. Orthop. Trauma. Surg. 2019, 139, 709–716. [Google Scholar] [CrossRef] [PubMed]
- Lovecchio, F.; Alvi, H.; Sahota, S.; Beal, M.; Manning, D. Is Outpatient Arthroplasty as Safe as ERAS Inpatient Arthroplasty? A Propensity Score Matched Analysis. J. Arthroplast. 2016, 31, 197–201. [Google Scholar] [CrossRef] [PubMed]
- Machin, J.T.; Phillips, S.; Parker, M.; Carrannante, J.; Hearth, M.W. Patient satisfaction with the use of an enhanced recovery programme for primary arthroplasty. Ann. R. Coll. Surg. Engl. 2013, 95, 577–581. [Google Scholar] [CrossRef] [PubMed]
- Maempel, J.F.; Walmsley, P.J. Enhanced recovery programmes can reduce length of stay after total knee replacement without sacrificing functional outcome at one year. Ann. R. Coll. Surg. Engl. 2015, 97, 563–567. [Google Scholar] [CrossRef]
- Mangat, S.; Hance, L.; Ricketts, K.J.; Phillips, M.R.; Mclean, S.E. The impact of an enhanced recovery perioperative pathway for pediatric pectus deformity repair. Pediatr. Surg. Int. 2020, 36, 1035–1045. [Google Scholar] [CrossRef]
- McDonald, D.A.; Siegmeth, R.; Deakin, A.H.; Kinninmonth, A.W.G.; Scott, N.B. An enhanced recovery programme for primary total knee arthroplasty in the United Kingdom—Follow up at one year. Knee 2012, 19, 525–529. [Google Scholar] [CrossRef]
- Memtsoudis, S.G.; Fiasconaro, M.; Soffin, E.M.; Liu, J.; Wilson, L.A.; Poeran, J.; Bekeris, J.; Kehlet, H. Enhanced recovery after surgery components and perioperative outcomes: A nationwide observational study. Br. J. Anaesth. 2020, 124, 638–647. [Google Scholar] [CrossRef]
- Mikkelsen, L.R.; Mechlenburg, I.; Søballe, K.; Jørgensen, L.B.; Mikkelsen, S.; Bandholm, T.; Petersen, A.K. Effect of early supervised progressive resistance training compared to unsupervised home-based exercise after ERAS total hip replacement applied to patients with preoperative functional limitations. A single-blinded randomised controlled trial. Osteoarthr. Cartil. 2014, 22, 2051–2058. [Google Scholar] [CrossRef]
- Munk, S.; Dalsgaard, J.; Bjerggaard, K.; Andersen, I.; Hansen, T.B.; Kehlet, H. Early recovery after ERAS Oxford unicompartmental knee arthroplasty. 35 patients with minimal invasive surgery. Acta Orthop. 2012, 83, 41–45. [Google Scholar] [CrossRef] [PubMed]
- Nazarenko, A.G.; Konovalov, N.A.; Krut’ko, A.V.; Zamiro, T.N.; Geroeva, I.B.; Gubaydullin, R.R.; Khoreva, N.E.; Komarov, A.N.; Stepanyan, M.A.; Konstantinova, M.V.; et al. Postoperative applications of the fast track technology in patients with herniated intervertebral discs of the lumbosacral spine. Zhurnal Voprosy Neirokhirurgii Imeni NN Burdenko 2016, 80, 5–12. [Google Scholar] [CrossRef] [PubMed]
- Nicolaiciuc, S.; Probst, P.; von Eisenhart-Rothe, R.; Burgkart, R.; Hube, R. Modern Total Knee Arthroplasty (TKA): With or without a Tourniquet? Surg. Technol. Int. 2019, 35, 336–340. [Google Scholar] [PubMed]
- Noel, E.; Miglionico, L.; Leclercq, M.; Jennart, H.; Fils, J.F.; Van Rompaey, N. Sufentanil sublingual tablet system versus oral oxycodone for management of postoperative pain in enhanced recovery after surgery pathway for total knee arthroplasty: A randomized controlled study. J. Exp. Orthop. 2020, 7, 92. [Google Scholar] [CrossRef]
- Okamoto, T.; Ridley, R.J.; Edmondston, S.J.; Visser, M.; Headford, J.; Yates, P.J. Day-of-Surgery Mobilization Reduces the Length of Stay After Elective Hip Arthroplasty. J. Arthroplast. 2016, 31, 2227–2230. [Google Scholar] [CrossRef]
- Otte, K.S.; Husted, H.; Ørsnes, T.; Kehlet, H. Bilateral simultaneous total hip arthroplasty in a fast track setting. Hip Int. 2011, 21, 336–339. [Google Scholar] [CrossRef] [PubMed]
- Pamilo, K.J.; Torkki, P.; Peltola, M.; Pesola, M.; Remes, V.; Paloneva, J. ERASing for total knee replacement reduces use of institutional care without compromising quality. Acta Orthop. 2018, 89, 184–189. [Google Scholar] [CrossRef]
- Petersen, P.B.; Jørgensen, C.C.; Kehlet, H. Lundbeck Foundation Centre for ERAS Hip and Knee Replacement Collaborative Group. Delirium after ERAS hip and knee arthroplasty—A cohort study of 6331 elderly patients. Acta Anaesthesiol. Scand. 2017, 61, 767–772. [Google Scholar] [CrossRef]
- Petersen, P.B.; Jørgensen, C.C.; Kehlet, H. Lundbeck Foundation Center for ERAS Hip and Knee Replacement collaborative group. Temporal trends in length of stay and readmissions after ERAS hip and knee arthroplasty. Dan Med. J. 2019, 66, A5553. [Google Scholar]
- Petersen, P.B.; Jørgensen, C.C.; Kehlet, H. Lundbeck Foundation Centre for ERAS Hip and Knee Replacement Collaborative Group. ERAS hip and knee arthroplasty in older adults-a prospective cohort of 1,427 procedures in patients ≥85 years. Age Ageing 2020, 49, 425–431. [Google Scholar] [CrossRef]
- Petersen, P.B.; Jørgensen, C.C.; Gromov, K.; Kehlet, H.; Lundbeck Foundation Centre for ERAS Hip and Knee Replacement Collaborative Group. Venous thromboembolism after ERAS unicompartmental knee arthroplasty—A prospective multicentre cohort study of 3927 procedures. Thromb. Res. 2020, 195, 81–86. [Google Scholar] [CrossRef] [PubMed]
- Petersen, P.B.; Lindberg-Larsen, M.; Jørgensen, C.C.; Kehlet, H.; Lundbeck Foundation Centre for ERAS Hip and Knee Arthroplasty collaborating group. Venous thromboembolism after ERAS elective revision hip and knee arthroplasty—A multicentre cohort study of 2814 unselected consecutive procedures. Thromb. Res. 2021, 199, 101–105. [Google Scholar] [CrossRef] [PubMed]
- Pirsaharkhiz, N.; Comolli, K.; Fujiwara, W.; Stasiewicz, S.; Boyer, J.M.; Begin, E.V.; Rubinstein, A.J.; Henderson, H.R.; Lazar, J.F.; Watson, T.J.; et al. Utility of erector spinae plane block in thoracic surgery. J. Cardiothorac. Surg. 2020, 15, 91. [Google Scholar] [CrossRef] [PubMed]
- Pitter, F.T.; Jørgensen, C.C.; Lindberg-Larsen, M.; Kehlet, H.; Lundbeck Foundation Center for ERAS Hip and Knee Replacement Collaborative Group. Postoperative Morbidity and Discharge Destinations After ERAS Hip and Knee Arthroplasty in Patients Older Than 85 Years. Anesth. Analg. 2016, 122, 1807–1815. [Google Scholar] [CrossRef]
- Plenge, U.; Parker, R.; Davids, S.; Davies, G.L.; Fullerton, Z.; Gray, L.; Groenewald, P.; Isaacs, R.; Kauta, N.; Louw, F.M.; et al. Quality of recovery after total hip and knee arthroplasty in South Africa: A national prospective observational cohort study. BMC Musculoskelet. Disord. 2020, 21, 721. [Google Scholar] [CrossRef]
- Plessl, D.; Salomon, B.; Haydel, A.; Leonardi, C.; Bronstone, A.; Dasa, V. Rapid Versus Standard Recovery Protocol Is Associated with Improved Recovery of Range of Motion 12 Weeks After Total Knee Arthroplasty. J. Am. Acad. Orthop. Surg. 2020, 28, e962–e968. [Google Scholar] [CrossRef]
- Pollmann, C.T.; Røtterud, J.H.; Gjertsen, J.E.; Dahl, F.A.; Lenvik, O.; Årøen, A. Fast track hip fracture care and mortality—An observational study of 2230 patients. BMC Musculoskelet. Disord. 2019, 20, 248. [Google Scholar] [CrossRef]
- Porsius, J.T.; Mathijssen, N.M.C.; Klapwijk-Van Heijningen, L.C.M.; Van Egmond, J.C.; Melles, M.; Vehmeijer, S.B.W. Early recovery trajectories after ERAS primary total hip arthroplasty: The role of patient characteristics. Acta Orthop. 2018, 89, 597–602. [Google Scholar] [CrossRef]
- PrkiĆ, A.; Viveen, J.; The, B.; Koenraadt, K.L.M.; Eygendaal, D. Early Mobilization and Functional Discharge Criteria Affecting Length of Stay after Total Elbow Arthroplasty. Acta Chir. Orthop. Traumatol. Cech. 2020, 87, 197–202. [Google Scholar]
- Robinson, K.P.; Wagstaff, K.J.; Sanghera, S.; Kerry, R.M. Postoperative pain following primary lower limb arthroplasty and enhanced recovery pathway. Ann. R. Coll. Surg. Engl. 2014, 96, 302–306. [Google Scholar] [CrossRef]
- Romano, L.U.; Rigoni, M.; Torri, E.; Nella, M.; Morandi, M.; Casetti, P.; Nollo, G. A Propensity Score-Matched Analysis to Assess the Outcomes in Pre- and Post-ERAS Hip and Knee Elective Prosthesis Patients. J. Clin. Med. 2021, 10, 741. [Google Scholar] [CrossRef] [PubMed]
- Ruiz, N.; Buisson, X.; Filippi, G.; Roulet, M.; Robert, H.; Orthopedics and Traumatology Society of Western France (SOO). Ambulatory unicompartmental knee arthroplasty: Short outcome of 50 first cases. Orthop. Traumatol. Surg. Res. 2018, 104, 961–966. [Google Scholar] [CrossRef]
- Rytter, S.; Stilling, M.; Munk, S.; Hansen, T.B. Methylprednisolone reduces pain and decreases knee swelling in the first 24 h after ERAS unicompartmental knee arthroplasty. Knee Surg. Sports Traumatol. Arthrosc. 2017, 25, 284–290. [Google Scholar] [CrossRef] [PubMed]
- Saku, S.A.; Mäkinen, T.J.; Madanat, R. Reasons and Risk Factors for Delayed Discharge After Total Knee Arthroplasty Using an Opioid-Sparing Discharge Protocol. J. Arthroplast. 2019, 34, 2365–2370. [Google Scholar] [CrossRef]
- Savaridas, T.; Serrano-Pedraza, I.; Khan, S.K.; Martin, K.; Malviya, A.; Reed, M.R. Reduced medium-term mortality following primary total hip and knee arthroplasty with an enhanced recovery program. A study of 4,500 consecutive procedures. Acta Orthop. 2013, 84, 40–43. [Google Scholar] [CrossRef] [PubMed]
- Schotanus, M.G.M.; Bemelmans, Y.F.L.; Grimm, B.; Heyligers, I.C.; Kort, N.P. Physical activity after outpatient surgery and enhanced recovery for total knee arthroplasty. Knee Surg. Sports Traumatol. Arthrosc. 2017, 25, 3366–3371. [Google Scholar] [CrossRef]
- Shaw, K.A.; Fletcher, N.D.; Devito, D.P.; Schmitz, M.L.; Fabregas, J.; Gidwani, S.; Chhatbar, P.; Murphy, J.S. In-hospital opioid usage following posterior spinal fusion for adolescent idiopathic scoliosis: Does methadone offer an advantage when used with an ERAS pathway? Spine Deform. 2021; online ahead of print. [Google Scholar] [CrossRef]
- Skovgaard, C.; Holm, B.; Troelsen, A.; Lunn, T.H.; Gaarn-Larsen, L.; Kehlet, H.; Husted, H. No effect of fibrin sealant on drain output or functional recovery following simultaneous bilateral total knee arthroplasty: A randomized, double-blind, placebo-controlled study. Acta Orthop. 2013, 84, 153–158. [Google Scholar] [CrossRef]
- Soffin, E.M.; Vaishnav, A.S.; Wetmore, D.S.; Barber, L.; Hill, P.; Gang, C.H.; Beckman, J.D.; Albert, T.J.; Qureshi, S.A. Design and Implementation of an Enhanced Recovery After Surgery (ERAS) Program for Minimally Invasive Lumbar Decompression Spine Surgery: Initial Experience. Spine 2019, 44, E561–E570. [Google Scholar] [CrossRef]
- Soffin, E.M.; Wetmore, D.S.; Beckman, J.D.; Sheha, E.D.; Vaishnav, A.S.; Albert, T.J.; Gang, C.H.; Qureshi, S.A. Opioid-free anesthesia within an enhanced recovery after surgery pathway for minimally invasive lumbar spine surgery: A retrospective matched cohort study. Neurosurg. Focus 2019, 46, E8. [Google Scholar] [CrossRef]
- Soffin, E.M.; Beckman, J.D.; Tseng, A.; Zhong, H.; Huang, R.C.; Urban, M.; Guheen, C.R.; Kim, H.J.; Cammisa, F.P.; Nejim, J.A.; et al. Enhanced Recovery after Lumbar Spine Fusion: A Randomized Controlled Trial to Assess the Quality of Patient Recovery. Anesthesiology 2020, 133, 350–363. [Google Scholar] [CrossRef] [PubMed]
- Specht, K.; Leonhardt, J.S.; Revald, P.; Mandøe, H.; Andresen, E.B.; Brodersen, J.; Kreiner, S.; Kjaersgaard-Andersen, P. No evidence of a clinically important effect of adding local infusion analgesia administrated through a catheter in pain treatment after total hip arthroplasty. Acta Orthop. 2011, 82, 315–320. [Google Scholar] [CrossRef] [PubMed]
- Staartjes, V.E.; de Wispelaere, M.P.; Schröder, M.L. Improving recovery after elective degenerative spine surgery: 5-year experience with an enhanced recovery after surgery (ERAS) protocol. Neurosurg. Focus 2019, 46, E7. [Google Scholar] [CrossRef] [PubMed]
- Stambough, J.B.; Bloom, G.B.; Edwards, P.K.; Mehaffey, G.R.; Barnes, C.L.; Mears, S.C. Rapid Recovery After Total Joint Arthroplasty Using General Anesthesia. J. Arthroplast. 2019, 34, 1889–1896. [Google Scholar] [CrossRef] [PubMed]
- Starks, I.; Wainwright, T.W.; Lewis, J.; Lloyd, J.; Middleton, R.G. Older patients have the most to gain from orthopaedic enhanced recovery programmes. Age Ageing 2014, 43, 642–648. [Google Scholar] [CrossRef]
- Stowers, M.D.J.; Manuopangai, L.; Hill, A.G.; Gray, J.R.; Coleman, B.; Munro, J.T. Enhanced Recovery After Surgery in elective hip and knee arthroplasty reduces length of hospital stay. ANZ J. Surg. 2016, 86, 475–479. [Google Scholar] [CrossRef]
- Talboys, R.; Mak, M.; Modi, N.; Fanous, N.; Cutts, S. Enhanced recovery programme reduces opiate consumption in hip hemiarthroplasty. Eur. J. Orthop. Surg. Traumatol. 2016, 26, 177–181. [Google Scholar] [CrossRef]
- Tan, N.L.T.; Hunt, J.L.; Gwini, S.M. Does implementation of an enhanced recovery after surgery program for hip replacement improve quality of recovery in an Australian private hospital: A quality improvement study. BMC Anesth. 2018, 18, 64. [Google Scholar] [CrossRef]
- Temporiti, F.; Draghici, I.; Fusi, S.; Traverso, F.; Ruggeri, R.; Grappiolo, G.; Gatti, R. Does walking the day of total hip arthroplasty speed up functional independence? A non-randomized controlled study. Arch. Physiother. 2020, 10, 8. [Google Scholar] [CrossRef]
- Tucker, A.; McCusker, D.; Gupta, N.; Bunn, J.; Murnaghan, M. Orthopaedic Enhanced Recovery Programme for Elective Hip and Knee Arthroplasty—Could a Regional Programme be Beneficial? Ulst. Med. J. 2016, 85, 86–91. [Google Scholar]
- van den Belt, L.; van Essen, P.; Heesterbeek, P.J.C.; Defoort, K.C. Predictive factors of length of hospital stay after primary total knee arthroplasty. Knee Surg. Sports Traumatol. Arthrosc. 2015, 23, 1856–1862. [Google Scholar] [CrossRef] [PubMed]
- Van Egmond, J.C.; Verburg, H.; Mathijssen, N.M.C. The first 6 weeks of recovery after total knee arthroplasty with fast track. Acta Orthop. 2015, 86, 708–713. [Google Scholar] [CrossRef] [PubMed]
- Van Horne, A.; Van Horne, J. Patient-optimizing enhanced recovery pathways for total knee and hip arthroplasty in Medicare patients: Implication for transition to ambulatory surgery centers. Arthroplast. Today 2019, 5, 497–502. [Google Scholar] [CrossRef] [PubMed]
- Van Horne, A.; Van Horne, J. Presurgical optimization and opioid-minimizing enhanced recovery pathway for ambulatory knee and hip arthroplasty: Postsurgical opioid use and clinical outcomes. Arthroplast. Today 2019, 6, 71–76. [Google Scholar] [CrossRef]
- Venkata, H.K.; van Dellen, J.R. A perspective on the use of an enhanced recovery program in open, non-instrumented day surgery for degenerative lumbar and cervical spinal conditions. J. Neurosurg. Sci. 2018, 62, 245–254. [Google Scholar] [CrossRef]
- Vesterby, M.S.; Pedersen, P.U.; Laursen, M.; Mikkelsen, S.; Larsen, J.; Søballe, K.; Jørgensen, L.B. Telemedicine support shortens length of stay after ERAS hip replacement. Acta Orthop. 2017, 88, 41–47. [Google Scholar] [CrossRef]
- Wang, P.; Wang, Q.; Kong, C.; Teng, Z.; Li, Z.; Zhang, S.; Sun, W.; Feng, M.; Lu, S. Enhanced recovery after surgery (ERAS) program for elderly patients with short-level lumbar fusion. J. Orthop. Surg. Res. 2020, 15, 299. [Google Scholar] [CrossRef]
- Wharton, K.; Chun, Y.; Hunsberger, J.; Jelin, E.; Garcia, A.; Stewart, D. Successful use of an enhanced recovery after surgery (ERAS) pathway to improve outcomes following the Nuss procedure for pectus excavatum. J. Pediatr. Surg. 2020, 55, 1065–1071. [Google Scholar] [CrossRef]
- Wied, C.; Thomsen, M.G.; Kallemose, T.; Myhrmann, L.; Jensen, L.S.; Husted, H.; Troelsen, A. The risk of manipulation under anesthesia due to unsatisfactory knee flexion after ERAS total knee arthroplasty. Knee 2015, 22, 419–423. [Google Scholar] [CrossRef]
- Winther, S.B.; Foss, O.A.; Wik, T.S.; Davis, S.P.; Engdal, M.; Jessen, V.; Husby, O.S. 1-year follow-up of 920 hip and knee arthroplasty patients after implementing ERAS. Acta Orthop. 2015, 86, 78–85. [Google Scholar] [CrossRef]
- Wynell-Mayow, W.; Saeed, M.Z. Much ado about nothing: The effect of tourniquet time on an accelerated rehabilitation programme following total knee replacement (TKR). Eur. J. Orthop. Surg. Traumatol. 2018, 28, 1177–1182. [Google Scholar] [CrossRef] [PubMed]
- Xie, J.; Hu, Q.; Huang, Q.; Chen, G.; Zhou, Z.; Pei, F. Efficacy and safety of tranexamic acid in geriatric hip fracture with hemiarthroplasty: A retrospective cohort study. BMC Musculoskelet. Disord. 2019, 20, 304. [Google Scholar] [CrossRef]
- Xu, H.; Xie, J.; Lei, Y.; Huang, Q.; Huang, Z.; Pei, F. Closed suction drainage following routine primary total joint arthroplasty is associated with a higher transfusion rate and longer postoperative length of stay: A retrospective cohort study. J. Orthop. Surg. Res. 2019, 14, 163. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.; Skaggs, D.L.; Chan, P.; Villamor, G.A.; Choi, P.D.; Tolo, V.T.; Kissinger, C.; Lehman, A.; Andras, L.M. High Satisfaction in Adolescent Idiopathic Scoliosis Patients on Enhanced Discharge Pathway. J. Pediatr. Orthop. 2020, 40, e166–e170. [Google Scholar] [CrossRef] [PubMed]
- Yanik, J.M.; Bedard, N.A.; Hanley, J.M.; Otero, J.E.; Callaghan, J.J.; Marsh, J.L. Rapid Recovery Total Joint Arthroplasty is Safe, Efficient, and Cost-Effective in the Veterans Administration Setting. J. Arthroplast. 2018, 33, 3138–3142. [Google Scholar] [CrossRef]
- Yu, H.; Wang, H.; Zhou, K.; Rong, X.; Yao, S.; Pei, F.; Zhou, Z. Modified Robert Jones bandage can not reduce postoperative swelling in enhanced-recovery after primary total knee arthroplasty without intraoperative tourniquet: A randomized controlled trial. BMC Musculoskelet. Disord. 2018, 19, 357. [Google Scholar] [CrossRef] [PubMed]
- Zhang, C.; Xiao, J. Application of ERAS surgery combined with a clinical nursing pathway in the rehabilitation of patients undergoing total hip arthroplasty. J. Int. Med. Res. 2020, 48, 300060519889718. [Google Scholar] [CrossRef]
- Zietek, P.; Zietek, J.; Szczypior, K.; Safranow, K. Effect of adding one 15-minute-walk on the day of surgery to ERAS rehabilitation after total knee arthroplasty: A randomized, single-blind study. Eur. J. Phys. Rehabil. Med. 2015, 51, 245–252. [Google Scholar]
- Zietek, P.; Dziedziejko, V.; Safranow, K.; Zietek, J.; Stępień-Słodkowska, M.; Bialecka, M.; Zietek, M.; Kotrych, D.; Kamiński, A.; Kowalska, A. TNF-α concentrations in pre-operative synovial fluid for predicting early post-operative function and pain after ERAS total knee arthroplasty. Knee 2016, 23, 1044–1048. [Google Scholar] [CrossRef]
- Scott, N.B.; McDonald, D.; Campbell, J.; Smith, R.D.; Carey, A.K.; Johnston, I.G.; James, K.R.; Breusch, S.J. The use of enhanced recovery after surgery (ERAS) principles in Scottish orthopaedic units—An implementation and follow-up at 1 year, 2010–2011: A report from the musculoskeletal Audit, Scotland. Arch. Orthop. Trauma. Surg. 2013, 133, 117–124. [Google Scholar] [CrossRef]
- Zhu, S.; Qian, W.; Jiang, C.; Ye, C.; Chen, X. Enhanced recovery after surgery for hip and knee arthroplasty: A systematic review and meta-analysis. Postgrad. Med. J. 2017, 93, 736–742. [Google Scholar] [CrossRef] [PubMed]
- Jansen, J.A.; Kruidenier, J.; Spek, B.; Snoeker, B.A.M. A cost-effectiveness analysis after implementation of a ERAS protocol for total knee arthroplasty. Knee 2020, 27, 451–458. [Google Scholar] [CrossRef] [PubMed]
- Choi, Y.S.; Kim, T.W.; Chang, M.J.; Kang, S.B.; Chang, C.B. Enhanced recovery after surgery for major orthopedic surgery: A narrative review. Knee Surg. Relat. Res. 2022, 34, 8. [Google Scholar] [CrossRef] [PubMed]
- Debono, B.; Wainwright, T.W.; Wang, M.Y.; Sigmundsson, F.G.; Yang, M.M.H.; Smid-Nanninga, H.; Bonnal, A.; Le Huec, J.C.; Fawcett, W.J.; Ljungqvist, O.; et al. Consensus statement for perioperative care in lumbar spinal fusion: Enhanced Recovery After Surgery (ERAS®) Society recommendations. Spine J. 2021, 21, 729–752. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Salamanna, F.; Contartese, D.; Brogini, S.; Visani, A.; Martikos, K.; Griffoni, C.; Ricci, A.; Gasbarrini, A.; Fini, M. Key Components, Current Practice and Clinical Outcomes of ERAS Programs in Patients Undergoing Orthopedic Surgery: A Systematic Review. J. Clin. Med. 2022, 11, 4222. https://doi.org/10.3390/jcm11144222
Salamanna F, Contartese D, Brogini S, Visani A, Martikos K, Griffoni C, Ricci A, Gasbarrini A, Fini M. Key Components, Current Practice and Clinical Outcomes of ERAS Programs in Patients Undergoing Orthopedic Surgery: A Systematic Review. Journal of Clinical Medicine. 2022; 11(14):4222. https://doi.org/10.3390/jcm11144222
Chicago/Turabian StyleSalamanna, Francesca, Deyanira Contartese, Silvia Brogini, Andrea Visani, Konstantinos Martikos, Cristiana Griffoni, Alessandro Ricci, Alessandro Gasbarrini, and Milena Fini. 2022. "Key Components, Current Practice and Clinical Outcomes of ERAS Programs in Patients Undergoing Orthopedic Surgery: A Systematic Review" Journal of Clinical Medicine 11, no. 14: 4222. https://doi.org/10.3390/jcm11144222
APA StyleSalamanna, F., Contartese, D., Brogini, S., Visani, A., Martikos, K., Griffoni, C., Ricci, A., Gasbarrini, A., & Fini, M. (2022). Key Components, Current Practice and Clinical Outcomes of ERAS Programs in Patients Undergoing Orthopedic Surgery: A Systematic Review. Journal of Clinical Medicine, 11(14), 4222. https://doi.org/10.3390/jcm11144222








