New Strategies to Improve the Quality of Life for Normal Aging versus Pathological Aging
Abstract
:1. Introduction
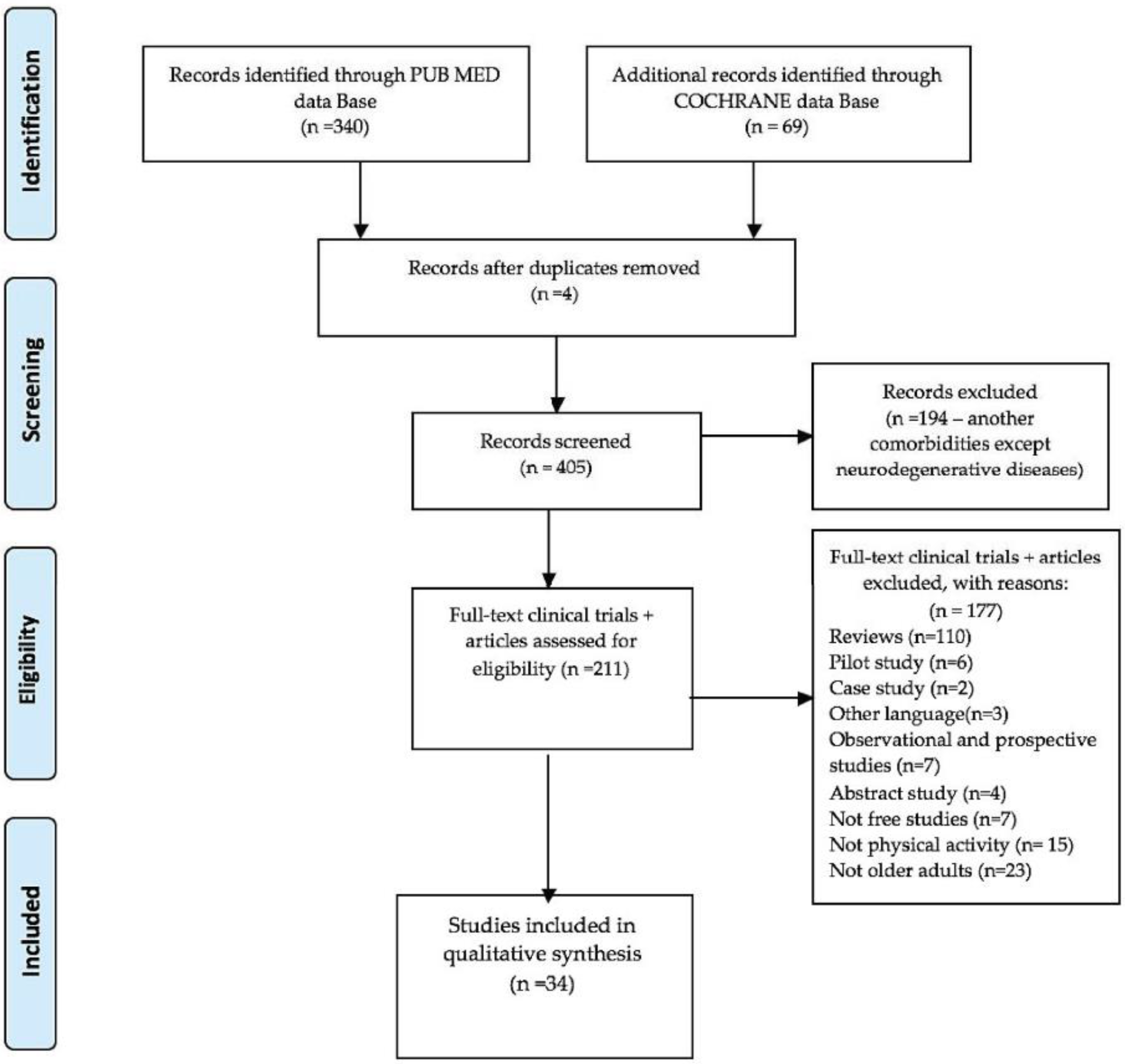
2. Materials and Methods
2.1. Search Criteria
2.2. Selection Strategy
2.3. Dynamics of Extracting Significant Data
2.4. Model Quality Synthesis Assessment
3. Results
3.1. Tools/Instruments—Determinants of Well-Being and Quality of Life in Seemingly Healthy Elderly and Older Adults with Neurodegenerative Diseases
3.1.1. Quantitative General Tools/Instruments
3.1.2. Qualitative Specific Tools/Instruments
3.1.3. Socio-Economics Tools/Instruments
3.1.4. Physical Tools/Instruments
3.1.5. Falls Tools/Instruments
3.1.6. Cognitive Tools/Instruments
3.2. The Impact of Recovery Strategies through Physical Activity and the Use of Assisted Devices on the Well-Being and Quality of Life for Normal Aging
3.3. The Impact of Telerehabilitation through Physical Activity with the Use of Assistive Devices for Apparently Healthy Adults and Seniors with Neurodegenerative Diseases
3.3.1. Telerehabilitation Sustained by Assisted Devices for Efficient Physical Activities at Normal Aging
3.3.2. Telerehabilitation through Physical Therapy Sustained by Assisted Devices at Older Adults with Neurodegenerative Disorders
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Tom, S.E.; Adachi, J.D.; Anderson, J.F.A.; Boonen, S.; Chapurlat, R.D.; Compston, J.E.; Cooper, C.; Gehlbach, S.H.; Greenspan, S.L.; Hooven, F.H.; et al. Frailty and fracture, disability, and falls: A multiple country study from the global longitudinal study of osteoporosis in women. J. Am. Geriatr. Soc. 2013, 61, 327–334. [Google Scholar] [CrossRef] [PubMed]
- Rebelo-Marques, A.; De Sousa, L.A.; Andrade, R.; Ribeiro, C.F.; Mota-Pinto, A.; Carrilho, F.; Espregueira-Mendes, J. Aging hall-marks: The benefits of physical exercise. Front. Endocrinol. 2018, 9, 258. [Google Scholar] [CrossRef] [PubMed]
- Important Facts About Falls. Available online: https://www.cdc.gov/homeandrecreationalsafety/falls/adultfalls.html (accessed on 7 August 2019).
- Mora Pinzon, M.; Myers, S.; Jacobs, E.A.; Ohly, S.; Bonet-Vázquez, M.; Villa, M.; Castro, A.; Mahoney, J. ”Pisando Fuerte”: An evidence-based falls prevention program for Hispanic/Latinos older adults: Results of an implementation trial. BMC Geriatr. 2019, 19, 258. [Google Scholar] [CrossRef] [PubMed]
- Rantz, M.; Phillips, L.J.; Galambos, C.; Lane, K.; Alexander, G.L.; Despins, L.; Koopman, R.J.; Skubic, M.; Hicks, L.; Miller, S.; et al. Randomized trial of intelligent sensor system for early illness alerts in senior housing. J. Am. Med. Dir. Assoc. 2017, 18, 860–870. [Google Scholar] [CrossRef]
- Deidda, M.; Coll-Planas, L.; Giné-Garriga, M.; Guerra-Balic, M.; Roque i Figuls, M.; Tully, M.A.; Caserotti, P.; Rothenbacher, D.; Casanovas, A.S.; McIntosh, E.; et al. Cost-effectiveness of exercise referral schemes enhanced by self-management strategies to battle sedentary behaviour in older adults: Protocol for an economic evaluation alongside the SITLESS three-armed pragmatic randomised controlled trial. BMJ Open 2018, 8, e022266. [Google Scholar] [CrossRef] [Green Version]
- Siegert, C.; Hauptmann, B.; Jochems, N.; Schrader, A.; Deck, R. ParkProTrain: An individualized, tablet-based physiotherapy training programme aimed at improving quality of life and participation restrictions in PD patients—A study protocol for a quasi-randomized, longitudinal and sequential multi-method study. BMC Neurol. 2019, 19, 143. [Google Scholar]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [Green Version]
- EQ-5D User Guides. Available online: https://euroqol.org/publications/user-guides/ (accessed on 27 May 2022).
- Gibbs, J.; McArthur, C.; Wark, J.D.; Thabane, L.; Scherer, S.C.; Prasad, S.; Papaioannou, A.; Mittmann, N.; Laprade, J.; Kim, S.; et al. The effects of home exercise in older women with vertebral fractures: A pilot randomized controlled trial. Phys. Ther. 2020, 100, 662–676. [Google Scholar] [CrossRef]
- Vilpunaho, T.; Kröger, H.; Honkanen, R.; Koivumaa-Honkanen, H.; Sirola, J.; Kuvaja-Köllner, V.; Sund, R.; Rikkonen, T. Randomised controlled trial (RCT) study design for a large-scale municipal fall prevention exercise progarmme in community-living older women: Study protocol for the Kuopio Fall Prevention Study (KFPS). BMJ Open 2019, 9, e028716. [Google Scholar] [CrossRef]
- Li, F.; Harmer, P.; Eckstrom, E.; Fitzgerald, K.; Akers, L.; Chou, L.S.; Pidgeon, D.; Voit, J.; Winters-Stone, K. Cost-effectiveness of a therapheutic Tai Ji Quan fall prevention intervention for older adults at high risk of falling. J. Am. Med. Dir. Assoc. 2017, 18, 860–870. [Google Scholar]
- Delbaere, K.; Valenzuela, T.; Lord, S.R.; Clemson, L.; Zijlstra, G.A.R.; Close, J.C.T.; Lung, T.; Woodbury, A.; Chow, J.; McInerney, G.; et al. E-health standing tall balance exercise for fall prevention in older people: Results of a two year randomised controlled trial. BMJ 2021, 373, n740. [Google Scholar] [CrossRef] [PubMed]
- Stanmore, E.K.; Mavroeidi, A.; de Jong, L.D.; Skelton, D.A.; Sutton, C.J.; Benedetto, V.; Munford, L.A.; Meekes, W.; Bell, V.; Todd, C. The effectiveness and cost-effectiveness of strength and balance Exergames to reduce falls risk for people aged 55 years and older in UK assisted living facilities: A multi-centre, cluster randomised controlled trial. BMC Med. 2019, 17, 49. [Google Scholar] [CrossRef] [PubMed]
- Borges, P.R.T.; Resende, R.A.; Dias, J.F.; Mancini, M.C.; Sampaio, R.F. Additional file 1 of Telerehabilitation program for older adults on a waiting list for physical therapy after hospital discharge: Study protocol for a pragmatic randomized trial protocol. Trials 2021, 22, 445. [Google Scholar] [CrossRef] [PubMed]
- Hill, A.M.; Etherton-Beer, C.; McPhail, S.M.; Morris, M.E.; Flicker, L.; Shorr, R.; Bulsara, M.; Lee, D.C.; Fran-cis-Coad, J.; Waldron, N.; et al. Reducing falls after hospital discharge: A protocol for a ran-domised controlled trial evaluating an individualised multimodal falls education programme for older adults. BMJ Open 2017, 7, e013931. [Google Scholar] [CrossRef] [Green Version]
- EuroQol Group. EQ-5D Instruments. About EQ-5D. 2018. Available online: https://euroqol.org/eq-5d-instruments/eq-5d-3l-about/ (accessed on 27 May 2022).
- Giné-Garriga, M.; Coll-Planas, L.; Guerra, M.; Domingo, À.; Roqué, M.; Caserotti, P.; Denkinger, M.; Rothenbacher, D.; Tully, M.A.; Kee, F.; et al. The SITLESS project: Exercise referral schemes enhanced by self-management strategies to battle sedentary behaviour in older adults: Study protocol for a randomised controlled trial. Trials 2017, 18, 221. [Google Scholar] [CrossRef] [Green Version]
- Jones, C.A.; Siever, J.; Knuff, K.; Van Bergen, C.; Mick, P.; Little, J.; Jones, G.; Murphy, M.A.; Kurtz, D.; Miller, H. Walk, Talk, and Listen: A pilot randomized controlled trial targeting functional fitness and loneliness in older adults with hearing loss. BMJ Open 2019, 9, e026169. [Google Scholar] [CrossRef] [Green Version]
- Yuan, R.-Y.; Chen, S.-C.; Peng, C.-W.; Lin, Y.-N.; Chang, Y.-T.; Lai, C.-H. Effects of interactive video-game-based exercise on balance in older adults with mild-to-moderate Parkinson’s disease. J. Neuroeng. Rehabil. 2020, 17, 91. [Google Scholar] [CrossRef]
- Ward, R.E.; Orkaby, A.R.; Chen, J.; Hshieh, T.T.; Driver, J.A.; Gaziano, J.M.; Djousse, L. Association between diet quality and frately prevalence in the physicians’ health study. J. Am. Geriatr. Soc. 2020, 68, 770–776. [Google Scholar] [CrossRef]
- Fabbri, L.; Mosca, I.E.; Gerli, F.; Martini, L.; Pancani, S.; Lucidi, G.; Savazzi, F.; Baglio, F.; Vannetti, F.; Macchi, C.; et al. The Games for Older Adults Active Life (GOAL) project for people with mild cognitive impairment and vascular cognitive impairment: A study protocol for a randomized controlled trial. Front. Neurol. 2019, 9, 1040. [Google Scholar] [CrossRef] [Green Version]
- Yamada, K.; Muranaga, S.; Shinozaki, T.; Nakamura, K.; Tanaka, S.; Ogata, T. Age independency of mobility decrease assessed using the locomotive syndrome risk test in elderly with disability: A cross-sectional study. BMC Geriatr. 2018, 18, 28. [Google Scholar] [CrossRef]
- Pebole, M.M.; Hall, K.S. Insights following implementation of an exercise intervention in older veterans with PTSD. Int. J. Environ. Res. Public Health 2019, 16, 2630. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shahar, S.; Vanoh, D.; Mat Ludin, A.F.; Singh, D.K.A.; Hamid, T.A. Factors associated poor socioeconomic status among Malaysian older adults: An analysis according urban and rural settings. BMC Public Health 2019, 19, 549. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rønnow, S.S.; Lind, V.M.; Bechshøft, R.L.; Højfeldt, G.; Reitelseder, S.; Jensen, T.; Pernille Jespersen, A.; Sandris Nielsen, D.; Holm, L.; Tetens, I. Investigating risk of suboptimal macro and micronutrient intake and their determinats in older Danish adults with specific focus on protein intake—A cross-sectional study. Nutrients 2019, 11, 795. [Google Scholar] [CrossRef] [Green Version]
- Djuric, Z.; Segar, M.; Orizondo, C.; Mann, J.; Faison, M.; Peddireddy, N.; Paletta, M.; Locke, A. Delivery of health coaching by medical assistants in primary care. J. Am. Board Fam. Med. 2017, 30, 362–370. [Google Scholar] [CrossRef] [Green Version]
- Van Schooten, K.S.; Callisaya, M.L.; O’Dea, B.; Lung, T.; Anstey, K.; Lord, S.R.; Christensen, H.; Brown, A.; Chow, J.; McInerney, G.; et al. Protocol of a 12-month multifactorial eHealth programme targeting balance, dual-tasking and mood to prevent falls in older people: Standing Tall+ randomised controlled trial. BMJ Open. 2021, 11, e051085. [Google Scholar] [CrossRef]
- Sansano-Nadal, O.; Giné-Garriga, M.; Rodríguez-Roca, B.; Guerra-Balic, M.; Ferri, K.; Wilson, J.J.; Caserotti, P.; Olsen, P.Ø.; Blackburn, N.E.; Rothenbacher, D.; et al. Association of self-reported and device-measured sedentary behaviour and physical activity with health-related quality of life among european older adults. Int. J. Environ. Res. Public Health 2021, 18, 13252. [Google Scholar] [CrossRef] [PubMed]
- Realdon, O.; Rossetto, F.; Nalin, M.; Baroni, I.; Cabinio, M.; Fioravanti, R.; Saibene, F.L.; Alberoni, M.; Mantovani, F.; Romano, M.; et al. Technology-enhanced multi-domain at home continuum of care program with respect to usual care for people with cognitive impairment: The Ability-Telerehabilitation study protocol for a randomized controlled trial. BMC Psychiatry 2016, 16, 42. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brinke, L.F.T.; Best, J.R.; Crockett, R.A.; Liu-Ambrose, T. The effects of an 8-week computerized cognitive training program in older adults: A study protocol for a randomized controlled trial. BMC Geriatr. 2018, 18, 31. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wagner, L.; Hauptmann, B.; Hoffmann, A.K.; Jochems, N.; Schmeier, B.; Schrader, A.; Kohlmann, T.; Deck, R. Evaluation of an individualized, tablet-based physiotherapy training programme for patients with Parkinson’s disease: The ParkProTrain study, a quasi-randomised controlled trial. BMC Neurol. 2022, 22, 176. [Google Scholar] [CrossRef]
- Gandolfi, M.; Geroin, C.; Dimitrova, E.; Boldrini, P.; Waldner, A.; Bonadiman, S.; Picelli, A.; Regazzo, S.; Stirbu, E.; Primon, D.; et al. Virtual reality telerehabilitation for postural instability in parkinson’s disease: A multicenter, single-blind, randomized, controlled trial. Biomed. Res. Int. 2017, 2017, 7962826. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Klein, D.; Jeejeebhoy, K.; Tremblay, A.; Kallio, M.; Rheaume, C.; Humphries, S.; Royall, D.; Brauer, P.; Heyland, D.; Dhaliwal, R.; et al. The CHANGE program: Exercise intervention in primary care. Can. Fam. Phys. 2017, 63, 546–552. [Google Scholar]
- Falvey, J.R.; Gustavson, A.M.; Price, L.; Papazian, L.; Stevens-Lapsley, J.E.J. Dementia, comorbidity, and physical function in the Program of the all inclusive care for the elderly. Geriatr. Phys. Ther. 2019, 42, E1–E6. [Google Scholar] [CrossRef] [PubMed]
- Harris, D.M.; Rantalainen, T.; Muthalib, M.; Johnson, L.; Duckham, R.L.; Smith, S.T.; Daly, R.M.; Teo, W.-P. Concurrent exergaming and transcranial direct current stimulation to improve balance in people with Parkinson’s disease: Study protocol for a randomised controlled trial. Trials 2018, 19, 387. [Google Scholar] [CrossRef] [PubMed]
- Rawson, K.S.; Cavanaugh, J.T.; Colon-Semenza, C.; DeAngelis, T.; Duncan, R.P.; Fulford, D.; LaValley, M.P.; Mazzoni, P.; Nordahl, T.; Quintiliani, L.M.; et al. Design of the WHIP-PD study: A phase II, twelve-month, dual-site, randomized controlled trial evaluating the effects of a cognitive-behavioral approach for promoting enhanced walking activity using mobile health technology in people with Parkinson-disease. BMC Neurol. 2020, 20, 146. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Piccinini, G.; Imbimbo, I.; Ricciardi, D.; Coraci, D.; Santilli, C.; Lo Monaco, M.R.; Loreti, C.; Vulpiani, M.C.; Silveri, M.C.; Padua, L. The impact of cognitive reserve on the effectiveness of balance rehabilitation in Parkinson’s disease. Eur. J. Phys. Rehabil. Med. 2018, 54, 554–559. [Google Scholar] [CrossRef]
- Naseri, C.; McPhail, S.M.; Netto, J.; Haines, T.P.; Morris, M.E.; Etherton-Beer, C.; Flicker, L.; Lee, D.A.; Fran-cis-Coad, J.; Hill, A.M. The SITLESS project: Exercise referral schemes enhanced by self-management strategies to battle sedentary behaviour in older adults: Study protocolfor a randomised controlled trial. BMJ Open 2018, 8, e020726. [Google Scholar] [CrossRef]
- Duckham, R.L.; Tait, J.L.; Nowson, C.A.; Sanders, K.M.; Taaffe, D.R.; Hill, K.D.; Daly, R.M. Strategies and challenges associated with recruiting retirement village communities and residents into a group exercise intervention. BMC Med. Res. Methodol. 2018, 18, 173. [Google Scholar] [CrossRef] [Green Version]
- Lei, H.; Toosizadeh, N.; Schwenk, M.; Sherman, S.; Karp, S.; Sternberg, E.; Najafi, B. A pilot clinical trial to objectively assess the efficacy of electroacupuncture on gait in patients with Parkinson’s Disease using body worn sensor. PLoS ONE 2016, 11, e0155613. [Google Scholar] [CrossRef] [Green Version]
- Oliveira, A.; Nossa, P.; Mota-Pinto, A. Assessing functional capacity and factors determining functional decline in the elderly: A cross-sectionional study. Acta Med. Port. 2019, 32, 654–660. [Google Scholar] [CrossRef] [Green Version]
- Rantz, M.; Phillips, L.J.; Galambos, C.; Lane, K.; Alexander, G.L.; Despins, L.; Koopman, R.J.; Skubic, M.; Hicks, L.; Miller, S.; et al. Randomized clinical trial of technology to automatically detect early signs illness in senior housing. J. Gerontol. A Biol. Sci. Med. Sci. 2019, 74, 1504–1510. [Google Scholar]
- Burke, K.; Ellrodt, A.S.; Levine, J.; Adams, T.; Allis, R.; Macmurdie, I.; Paganoni, S. Exploring the use of educa-tional material about shoulder dysfunction a quality improvement project in people with amyotrophic lateral sclerosis. Am. J. Phys. Med. Rehabil. 2018, 97, 379–382. [Google Scholar] [CrossRef] [PubMed]
- Meloni, M.; Saibene, F.L.; Di Tella, S.; Di Cesare, M.; Borgnis, F.; Nemni, R.; Baglio, F. Functional and cognitive improvement after an intensive inpatient multidisciplinary rehabilitation program in mild to severe Parkinson’s disease: A retrospective and observational Study. Front. Neurol. 2021, 12, 626041. [Google Scholar] [CrossRef]
- Baglio, F.; Pirastru, A.; Bergsland, N.; Cazzoli, M.; Tavazzi, E. Neuroplasticity mediated by motor rehabilitation in Parkinson’s disease: A systematic review on structural and functional MRI markers. Rev. Neurosci. 2021, 33, 213–226. [Google Scholar] [CrossRef] [PubMed]
- Rossetto, F.; Borgnis, F.; Blasi, V.; Banfi, P.I.; Tavanelli, M.; Realdon, O.; Baglio, F. System integrated digital empowerment and rehabilitation to promote patient activation and well-Being (SIDERA^ B): Protocol for a randomized crossover trial on effectiveness and implementation. medRxiv 2022. [Google Scholar] [CrossRef]

| Quantitative General Tools | Qualitative Specific Tools | Socio-Economics Tools | Physical Tools | Falls Tools | Cognitive Tools |
|---|---|---|---|---|---|
| EuroQoL-5D-3L HRQoL AQoL-6D/NeuroQoL SWB QUALY Mini-OQLQ SF-36 FCI PSS FAP GLFS PTSD RPE WHODAS SNAQ DRV MUFA PUFA RIR RI FI mSOF aHEI MED DASH FFQ PROMIS COMPAS-W | ICEpop/ICECAP-O SUS LQS LSS SRSE MRSE RAVLT MSEQ HHIE IOI-AI BRCS PEG PDQ-8 HPQ-4 COSI | CEA CCA CCWBA ICER VIF COPM | SPPB TUG Chair sit to stand Test/5TSTST 6 min Walk test One foot balance test Grip strength Back scratch BBS PASE VAS Fatigue 4, 10, 400 m WT BOOMER TLS PFS DT-FPT ABC SOT FRT TMT MCST ROM IPAQ SIBT MDC DGI BARSE SEW-D MDTR MSL UPDRS H&Y ALF-FRS-R COP | BADL IADL FRAT ShortFES FES-I PROFANE Fab FRM FSST Mini Best-28 SEE | Jong Loneliness MMSE GDS DSMV PHQ-9/4 PPA MoCA FCSRT CES-D CRIq PDSS-2 D-QoL |
| References | Design | Physical Activity | Primary Outcomes | Secondary Outcomes | Assistive Devices | Conclusions |
|---|---|---|---|---|---|---|
| Deida M., et al. (2018) [29] | SITLESS study 1338 participants > 65 years | 30 min/daily times 5/week walking training | ERS-exercise referral scheme, SB-sedentary behavior PA-promoting physical activity | EQ-5D-5L ICECAP-O, ICEpop CEA CCA CCWBA | Actigraphy, Dumbbells Bike ergometer Elastic bands Grip dynamometer | Developing health economic model of older adults on long term, Evaluation healthcare and news orientation for promoting healthy programs with a rate of decreasing expenditures. |
| Duckham R.L., et al. (2018) [40] | PACE-IT 398 participants > 65 years 110-male 288-female | 26 weeks exercise training 45–60 min/session: motion exercises, balance training, HV-PRT | Falls rate Risk rate | Changes in lower limb motricity, Grip strength, Dynamic balance, Quality of life, Gait, Cognitive functions Short FES | Hand grip dynamometer, Handheld weights, Tubing, Sands bags, Thera-bands, Weighted vests | Improving balance, gait pattern, Decreasing trend falls, Enhancing strength and velocity motions, Increasing skills in knee motility, dorsiflexion and grip strength. |
| Gibbs J.C., et al. (2019) [10] | Osteoporosis Number of falls in past year >75 years 71-intervention group female 70-control group female | Physical exercises training from to moderate and high intensity 6–16 min/week | SPPB 4 m Walk Test 5-TSTS-5 TUG TLS BOOMER | EQ-5D-3L Mini OQLQ FES-I | Dumbbells | Developing the new strategies for performing physical activities which improve strength, joint mobility and the possibility of delaying the onset of osteoporosis in postmenopausal, Improving performance gait and upper limbs motricity, Early assessment and prevention of bone aging as well as postural outcomes at women elderly. |
| Giné-Garriga, M., et al. (2017) [18] | SITLESS study 1338 participants > 65 years | 16 weeks walking training 45–60 min/session 32 sessions times two/week | ERS—exercise referral scheme, SB—sedentary behavior PA—promoting physical activity | SPPB Muscle functions Health economic factors QUALYs EQ-5D-5L ICECAP-O Anthroponomy items Cognitive functions MSEQ Questionnaire Fear of falling Fear of falling Physical fatigue PFS | Hip work Actigraphy accelerometer Weights Grip dynamometer | Promoting strategies to combat sedentary behavior for the elderly population by implementing exercise schemes and supporting exciting learning programs capable rehabilitating physical and cognitive functions, Decreasing in the costs of institutionalized or assisted home care for the elderly. |
| Jones C.A., et al. (2019) [19] | Hearing loss 35-intervention group GAR+ 31-control group GAR >65 years 57%—male 43%—female | 10 weeks—SHE strengthening exercises 60 min strength, resistance, walking and coordination training | Functional outcomes: Chair sit to stand Test 6 min Walk test TUG One foot balance test Grip strength Back scratch | Psycho-social outcomes: HHIE SF-36 GDS IOI-AI COSI | Hearing aids Pedometer | WTL (walk, talk, listen) Improving communication strategies, Health education, Major benefits through fitness exercises for integration in society, GAR represents the first confidence the decreasing loneliness, Improving functional (gait speed, strength, resistance, health education) and emotional conditions, Increasing social contacts, Improving emotional and social loneliness. |
| Klein D., et al. (2017) [34] | CHANGE Canadian health advanced by nutrition and graded exercises Metabolic syndrome 307 participants 40–76 years | Physical aerobic exercises 3 sessions/week 20–30 min/session | Change to fitness Flexibility Strength | COPM | Treadmill | Improving capacity and mobility of motion, Enhancing intensity of muscular exercises further with a nutrition healthy, Increasing aerobic response and strength of motility, Decreasing risk cardiovascular for older adults. |
| Li F., et al. (2017) [12] | TJQMBB 218-multimodal exercises 363-stretching exercises >70 years Impairments mobility History of falling | 24 weeks twice training/weekly Tai Ji Quan intervention-moving for better balance Multimodal exercises Stretching physical activity | Number of falls | EQ-5D-5L QUALYs ICER | Weights Resistance tubing | Streamlining mobility through TJQMBB intervention, Decreasing the tendency to falls in the elderly and reducing the costs of therapeutic intervention and aging delay through different degrees of physical activity. |
| Mora Pinzon M., et al. (2019) [4] | PISANDO FUERTE Living independently History of falls 24 participants ≥ 65 years 13%—male 87%—female | Physical exercises for balance and strength Session learning workshop 2 h in 8 weeks | FaB (p ˂ 0.0001) TUG (p = 0.07) | Fidelity performing in learning program Upgrading exercises (regular exercises) Safe walking behaviors Safer stand-up from sitting position Change footwear | Assistive devices- weights using for physical activity | Decreasing tendency to falls 6 months training, Improving stance and strength of motility, Discussions with physicians for medication, Environmental changes which decreasing falls risk, Maintenance and continuation of physical exercises. |
| Oliveira A., et al. (2019) [42] | HCS-home care services (Portugal) ADHC-adult day care services Income Hospitalization institutional affiliation falls 95-healthy diet 15-poor diet 65–98 years 22%—male 78%—female | ADL Guided exercises Walking 3 times/week 20 min | BADL (p = 0.042) | IADL (p = 0.047) | Questionnaires: Social and demographic questions health status information | Increasing quality of life of life through care-givers family, Decreasing decline for elderly participants through emotional support, Preventing risk of falls or falls related disorders, sequels with or without change in joints mobility, gait and other motor functions Delaying decline of elderly through physical activity Adopting strategies which stimulate activities daily for older adults. |
| Pebole M.M., et al. (2019) [24] | Warrior wellness intervention sedentary 60–76 years 41-male 4-female | 12 weeks 30 min/session Aerobic exercise Training (recumbent stepper, treadmill, stationary cycle | Weight loss rate | PHQ 9 BMI DSMV PTSD RPE | Bike Treadmill | Improving physical health, mental health, Promoting strategy health with major impact in older adults, Decreasing of weight. |
| Shahar S., et al. (2019) [25] | SES-socio-economic status Nutritional status 2237 urban and rural group >60 years | ADL Physical fitness | BMI TUG Chair stand test Chair sit test 2 min step test Back scratch test Grip test | MMSE GDS WHODAS Dietary intake (Proteins, fiber, fruits, vitamins) | RAVLT PASW | The need to promote program to improving of health and nutrition for the elderly, Improving physical program interventions in both urban and rural areas for people with low incomes and residents in rural areas, Promoting the care of the elderly by launching new health policies that provide a functional diet for those with poor SES. |
| Vilpunaho T., et al. (2019) [11] | Osteoporosis 457-intervention group 457-control group >60 years female | 6 months training with weekly exercises gym and Taiji session 6 months slowly Exercises 12 months physical activity with low cost 60 min/session 2 times/week | Falls rate Falls risk | EQ-5D-5L LQS LSS GDS PSS BRCS MMSE QoL SWB | Stack weight device Biweekly SMS Questions phone | Reducing falls and fair of falls through Taiji program, Enhancing coordination balance and level motricity, Increasing cost-effectiveness for rehabilitation intervention, Delaying the installation Of mobility impairments the appearance of pathological fractures as well as The subsequent institutionalization or the use of caregivers at home. |
| Yamada K., et al. (2018) [23] | Locomotive syndrome risk test 1469 participants 76–88 years 1009-male 460-female | Exercises walking strength two steps while maintaining balance at different weights:10, 20,30, 40, cm.) | Two step score (Ratio of length of two steps and elderly height) Stand-up test score | GLFS | Weights | Early identification of ways to delay the decrease of mobility the lower extremity in the elderly population, Delaying the aggravation of the motor functional deficiencies who already have difficulties in the motor skills of the lower limbs, Delaying the institutionalization of the elderly with progressive motor deficit. |
| References | Design | Physical Exercises | Primary Outcomes | Secondary Outcomes | Assistive Devices | Conclusions |
|---|---|---|---|---|---|---|
| Borges P.R.T., et al. (2021) [15] | Public health care Discharged from hospitals | Physical therapy for resistance and balance home based 3–4 high intensity session/week | TUG 30-CST-30 | SF-36 VAS EuroQol-5D COPM | Smartphone app. | Effectiveness and cost-effectiveness through training telerehabilitation at discharged older adults, Improving strength and resistance for upper and lower limbs, Enhancing balance, Improving gait pattern and skills of motricity. |
| 115-participants telerehabilitation group 115-control group | ||||||
| >60 years | ||||||
| Delbaere K., et al. (2021) [13] | Standing Tall 114 -participants intervention group 112-control group >70 years | ADL Physical activity training | Rate of falls at 12 months | At 24 months EQ-5D-5L AQol-6 D PPA TMT Icon FES SPPB WHODAS COMPAS-W | Tablet with health education intervention McRoberts Move Monitor | Preventing falls in older adults through E-health program which improving executive and cognitive functions, Decreasing injuries associated falls. |
| Djuric Z., et al. (2017) [27] | Physicians’ Health Study 82 participants | ADL Vigorous exercises weekly | Frailty index (FI) | mSOF aHEI MED DASH FFQ | Well-coaches training program Mas-Medical assistants virtually program | Evaluating diet factors and implementation vigorous physical activity Decreasing risk of frailty for physician older adults with motors impairments and cognitive disorders. |
| Pre-frail group Frail group >60 years | ||||||
| Falvey J.R., et al. (2019) [35] | PACE program 525 participants >65 years | ADL | SPPB TUG F-CI VIF | Gait speed (m/s) Balance Strength | Stopwatch | Preventing the decrease of physical abilities in elderly adults with different degrees of impairments. |
| Hill A.M., et al. (2017) [16] | “Back to My Best” Hospital discharge AMT 390 participants >60 years | ADL 45 min/session times 2 sessions of education in hospital 15–30 min/session at phone for 3 months consecutive after for hospitalization | Rate of falls for the first 6 months | Percent of participants with falls Rate of injuries falls Katz index IADL AQOL-6 D | Phone Pre -made Video for 10 min | Decreasing rate of falls about 30%, with educational program “Back to my Best” after hospital discharge. |
| Naseri C., et al. (2017) [39] | Semi-structured interviews at phone Hospital discharge AMT 390 participants 195- intervention group 195-control group >60 years | ADL IADL Strength training Balance exercises Walking training | Rate of falls Katz index Lawton index | Falls prevention after 6 months Discharging Likert Scale SEE | Phone | Changing of physical behavior in order to prevent falls, Learning patterns educational which falls prevention. |
| Rantz M., et al. (2017) [43] | Senior housing Hospitalizations Physicians visit 86-intervention group 85-control group >83 years 23-male 62-female | ADL | SF-12 GDS MMSE ADL-IADL Gait Rite FRM FAP Hand grips | Walking speed in 10 s. Velocity (Gait Rite) Stride length right Stride length left Stride length right and left | Gait Rite Digital Dynamometer Motion system sensor non-wearable | Delaying the functional decline by using the warning system through environmental sensors installed at home, Monitoring behavioral activities tendency of falls and parameters gait, Extension of time for institutionalization of the elderly in nursing houses. |
| Rønnow, Schacht, S., et al. (2019) [26] | CALM 184 participants 65–81 years 79 -male 78-female | Exercises training 400 m walking | DRV MUFA PUFA 400 WT | AR RIR RI | VITAKOST dietary MADLOG app. | Improving the balance in the consumption of foods that bring adequate energy intake such as protein intake, vitamin D and thiamine intake and the application of a constant physical program to the detriment of the use of mono- and polyunsaturated fatty acids, alcohol consumption to increase well-being and prevention early aging. |
| Stanmore E.K., et al. (2019) [26] | Sheltered housing Good mental capacity Able to TV watch, gaming, technology, speaking English 56-exergame group 50-control group >55 years or older 22%—male 78%—female | 12 weeks 30 min/3 times/week Exercises for strength and balance | BBS FRAT VAS | PASE VAS fatigue HR Qol SUS TAM ProFANE QUALY | Kinect sensor ONTAGO-FaME Exergames app. | Improving balance, strength, Decreasing falls and fear falling, Increasing quality of life, Enhancing cost-effectiveness strategies against falling. |
| van Schooten K.S., et al. (2021) [28] | Standing Tall eHealth intervention CBT-cognitive behavioral training CMT-cognitive motor training 259-health education group 259-intervention group ≥65 years | 52 weeks 2–3 h/week Balance cognitive motor training | Rate of falls in the 12 months/person | EQ-5D-5L COMPAS-W WKODAS Exercise training Psychological well-being Balance ability in motricity Health literacy GDS QoL PPA Icon FES ICE pop | Tablets with MyCompas app., CBT program | Improving quality of life through decreasing rate of falls, Enhancing physical activity which promoting balance safety, motor skills, safe walking, but also improving of cognitive functions, Increasing well-being and tomorrow’s safety. |
| Ward R.E., et al. (2020) [21] | Self-care weekly program regarding diet, Sleep and physical activity | 8–12 weeks 136 min/week Physical training | Neuro QoL FSF PROMIS | Confidence to carry out physical activity PSS | Smart phone planning | Improving mobility and cognitive functions, Losing in weight without efforts, Changing of lifestyle for older adults through tele-assistive intervention and learning self-care program household on diet, behavioral sleeping and exercise training. |
| 39 participants >51 years or older |
| References | Design | Physical Exercises | Primary Outcomes | Secondary Outcomes | Assistive Devices | Conclusions |
|---|---|---|---|---|---|---|
| Fabbri L., et al. (2019) [22] | Randomized controlled trial study protocol (AD) experimental group 60 participants | 8 weeks 3 days/week cognitive Activity 2 days/week APA (adapted physical activity) 1 day/week social activities | Cognitive domain: MoCA FCSRT IFR TMT Stroop Test | Physical and social domains: ADCS/ADL CES-D SF-36 CRIq SPPB HAAS IPAQ | GENEA actigraph GOAL app. Architecture Brian HQ app. | Decreasing cognitive functions, Increasing skills in ADL. |
| Gandolfi M., et al. (2017) [33] | Randomized (PD) single blind 38—VR group 38-SIBT group | 50 min/session 21 sessions 3 days/week 7 weeks | BBS MDC | ABC 10-MWT DGI MCID PDQ-8 5 points Likert Scale | Tele Wii Nintendo protocol (exergaming) SIBT protocol (self- and external destabilization exercises) | Improving balance, gait and postural control, Decreasing number of falls, Reducing postural instability, Declining Impairments cognitive functions. |
| Harris D. M., et al. (2018) [36] | Randomized controlled trial (PD) 5-exergaming group 19-control group | 2 sessions/week 12 weeks Walking training | Limits of stability test | UPDRS H&Y COP mBEST 5TSTST 10 MWT FST PDQ-39 | Jintronix Software with a-t DCS (anodal-transcranial direct current stimulation) | Stimulating neuroplasticity, Improving static balance, Facilitating motor learning, Decreasing risk of falls. |
| Lei H., et al. (2016) [41] | Randomized pilot study (PD) 10-EA-experimental group 5-sham EA-control group | 30 min/session 3 sessions 1 day/week training walking | Gait speed | Spatio-temporal gait parameters UPDRS H&Y FES-I VAS MMSE | LEG Sys SEIRIN-stainless steel acupuncture needles ITO-ES-electric stimulators | Performing gait analysis: improving for STHW and DTHW, enhancing cadence, swinging angular velocity. |
| Rawson K.S., et al. (2020) [41] | Randomized controlled trial (PD) 140-experimental group 8-control group | 30–60 min/ session 6 sessions 12 months Walking training Strengthening exercises | Mean number of steps/day Mean number of minutes/day with >100 steps | 6MKT 10MKT BARSE SEW-D | mHealth software Step Watch TM 4 activity monitor (SAM) | Increasing walking ability. |
| Realdon O., et al. (2016) [30] | Randomized controlled trial (AD) ability-group usual care-group | Physical exercises for 6 weeks and 8 weeks follow up 12 months 5 days/week with tablet cognitive activity 7 days/week aerobic activity | SUS D-QoL | MMSE MoCA FCSRT IFR TMT DCS/ADL | Tablet ACG Sphyngo-manometer Pulse oximeter Heart Rate (HR) Fit Bit | Improving motor and non-motor functions. |
| Siegert S., et al. (2019) [32] | Quasi-randomized prospective longitudinal study (PD) | 9 months Physical training MKT | PDQ-8 | IMET FES-I PDSS-2 PHQ-4 Questionnaire Shanga | Tablet performed training program app (MKT) | Improving motor skills, Enhancing cognitive functions. |
| Yuan R.Y., et al. (2020) [20] | Cross-over trial (PD) intervention group-IVGB control group | 12 weeks Balance training | BBS | FES-M MDRT MSL SF-36 | XaviX entertainment system with IVGB (inter-active video games-based) | Reducing incidence of falls, Enhancing postural stability, Improving static and dynamic balance. |
| Piccinini G., et al. (2018) [38] | Idiopathic PD UPDRS (III) H&Y CR: cognitive reserve >64 years 28-male 25-female | 32 sessions for 4 months 2 times/week 50 min/session Rehabilitation protocol | BBS MMSE | CR level CRI score | CRIq: cognitive reserve index questionnaire education, working activity, leisure time BIT: Brief intelligence Test | Improving gait, balance and reducing risk of falls which undergo a conventional rehabilitation training against with patients who had higher CR. |
| Burke K., et al. (2018) [44] | Educational material(brochure) regarding shoulder health in ALS 16 participants | Stretching Exercises Strengthening training Sprinting Position strategies with arm on pillow | ROM | Five-point Likert scale | RedCap software app | Improving motion, Strengthening muscle shoulders, Decreasing pain and dysfunction of upper limbs. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bacanoiu, M.V.; Danoiu, M. New Strategies to Improve the Quality of Life for Normal Aging versus Pathological Aging. J. Clin. Med. 2022, 11, 4207. https://doi.org/10.3390/jcm11144207
Bacanoiu MV, Danoiu M. New Strategies to Improve the Quality of Life for Normal Aging versus Pathological Aging. Journal of Clinical Medicine. 2022; 11(14):4207. https://doi.org/10.3390/jcm11144207
Chicago/Turabian StyleBacanoiu, Manuela Violeta, and Mircea Danoiu. 2022. "New Strategies to Improve the Quality of Life for Normal Aging versus Pathological Aging" Journal of Clinical Medicine 11, no. 14: 4207. https://doi.org/10.3390/jcm11144207
APA StyleBacanoiu, M. V., & Danoiu, M. (2022). New Strategies to Improve the Quality of Life for Normal Aging versus Pathological Aging. Journal of Clinical Medicine, 11(14), 4207. https://doi.org/10.3390/jcm11144207






