Th17/Regulatory T-Cell Imbalance and Acute Kidney Injury in Patients with Sepsis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Aim, Design and Setting
2.2. Participants
2.3. Data Collection
2.4. Blood Sampling and Measurements
2.5. Group Analysis and Follow-Up
2.6. Statistical Analysis
3. Results
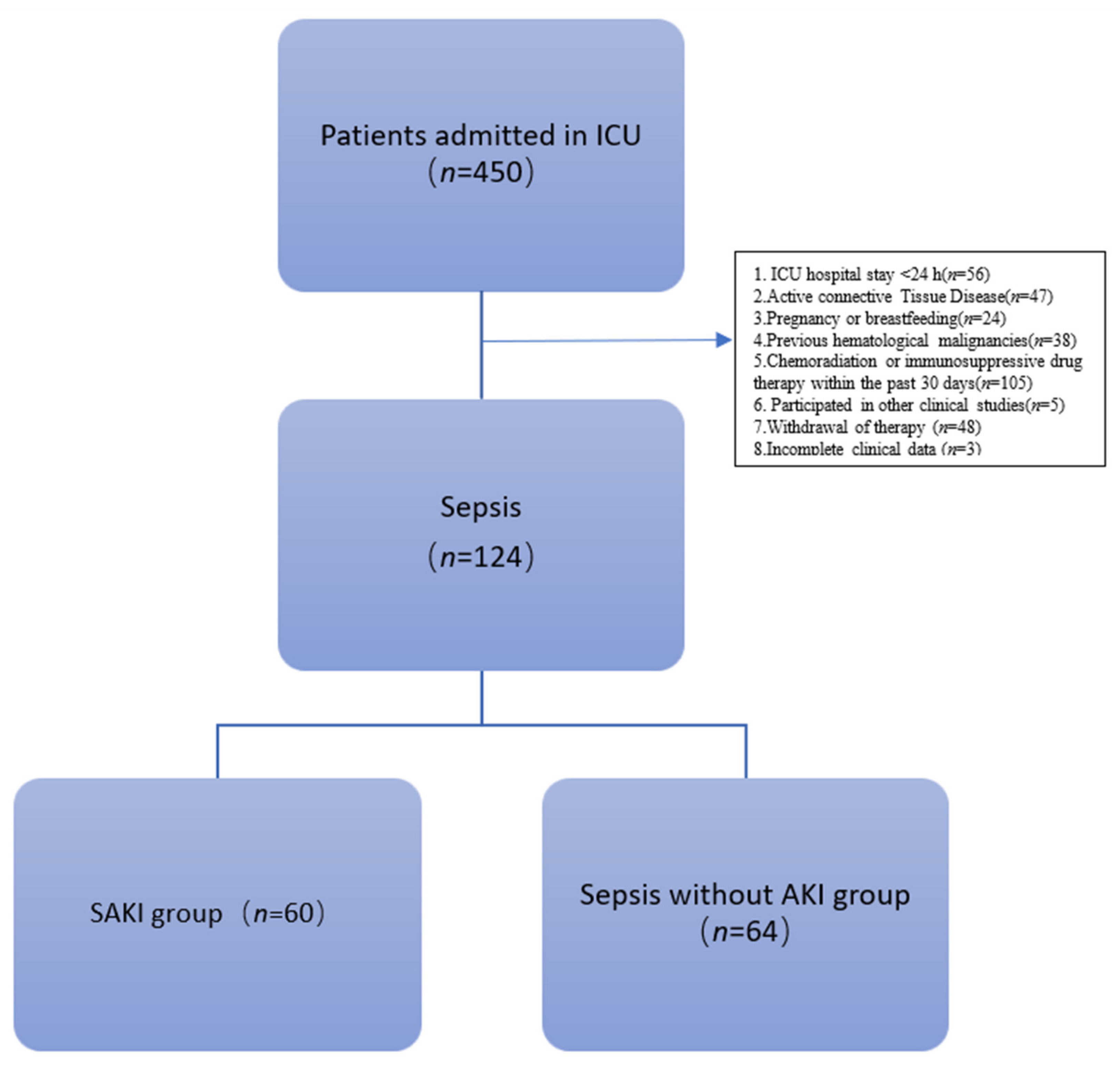
3.1. Enrollment of Patients
3.1.1. Clinical Characteristics of Patients
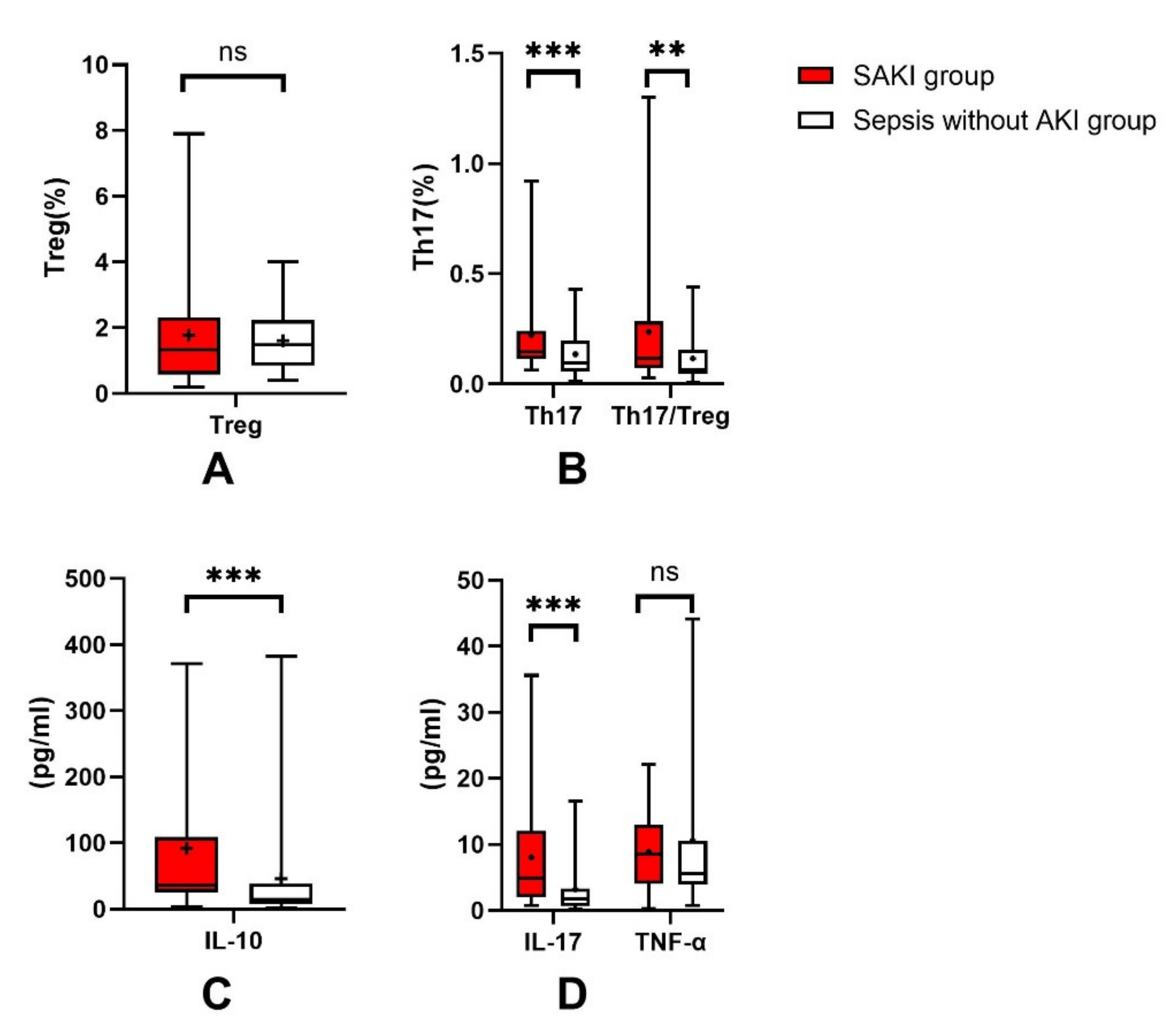
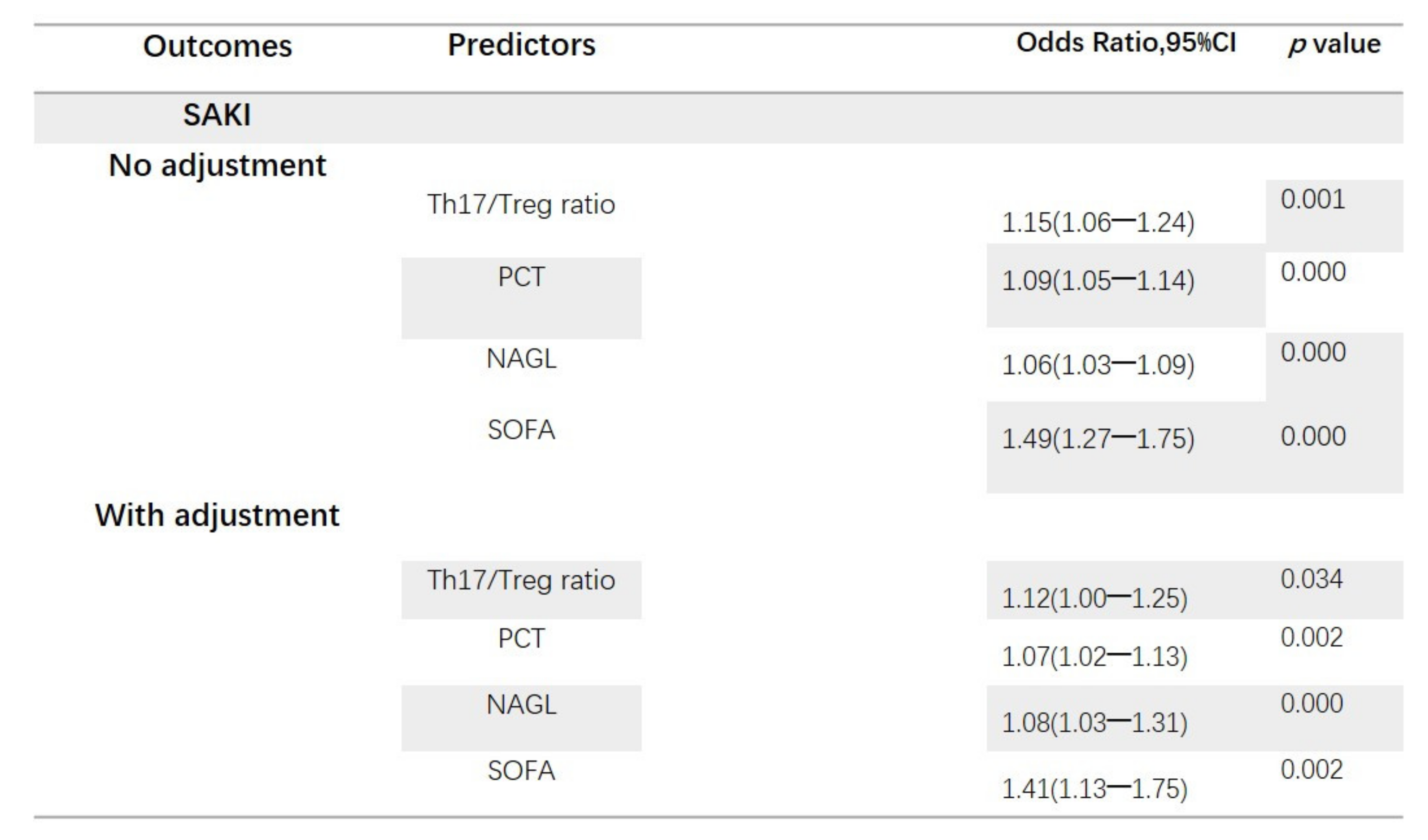
3.1.2. Th17/Treg Ratio Is Associated with the Occurrence of SAKI
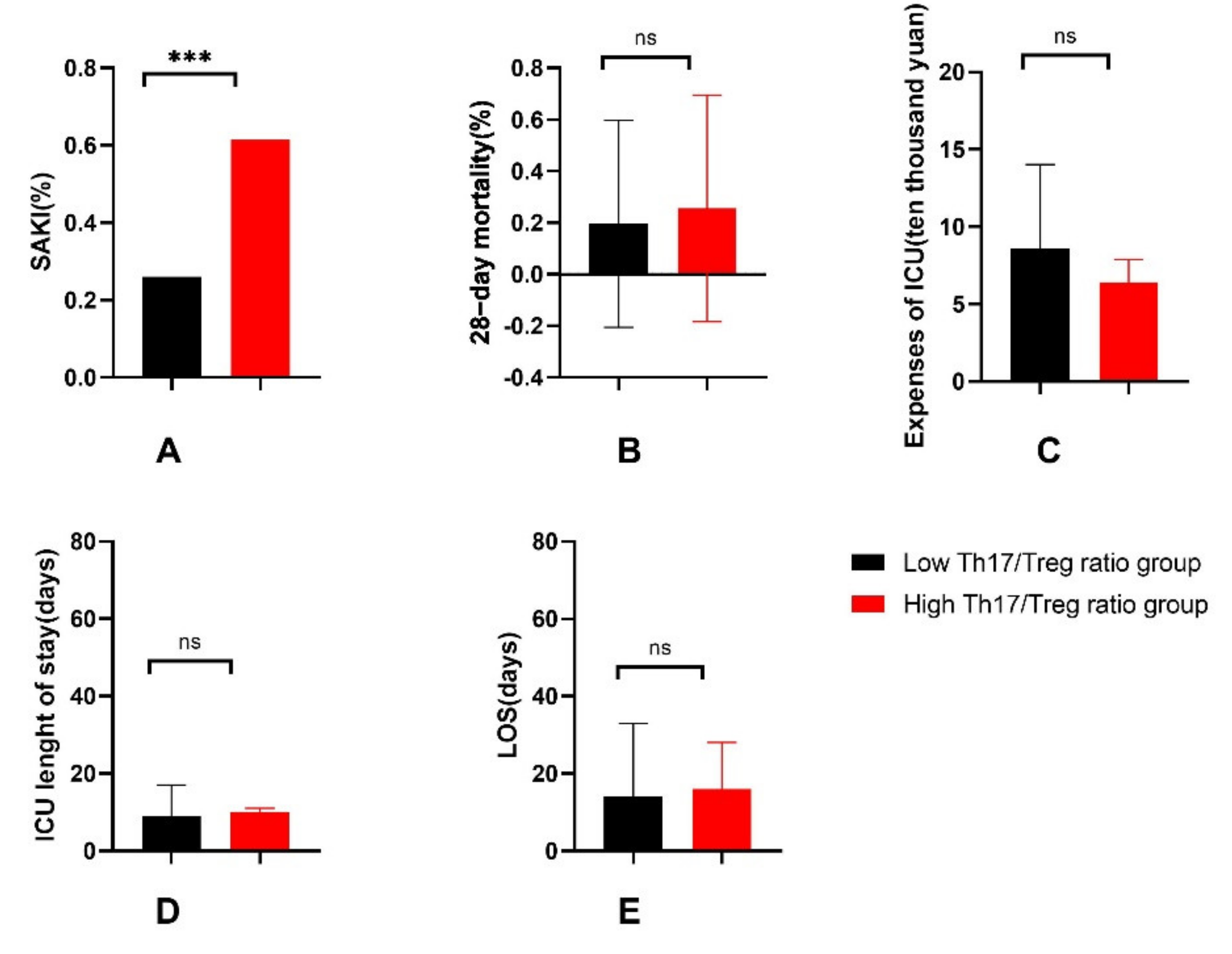
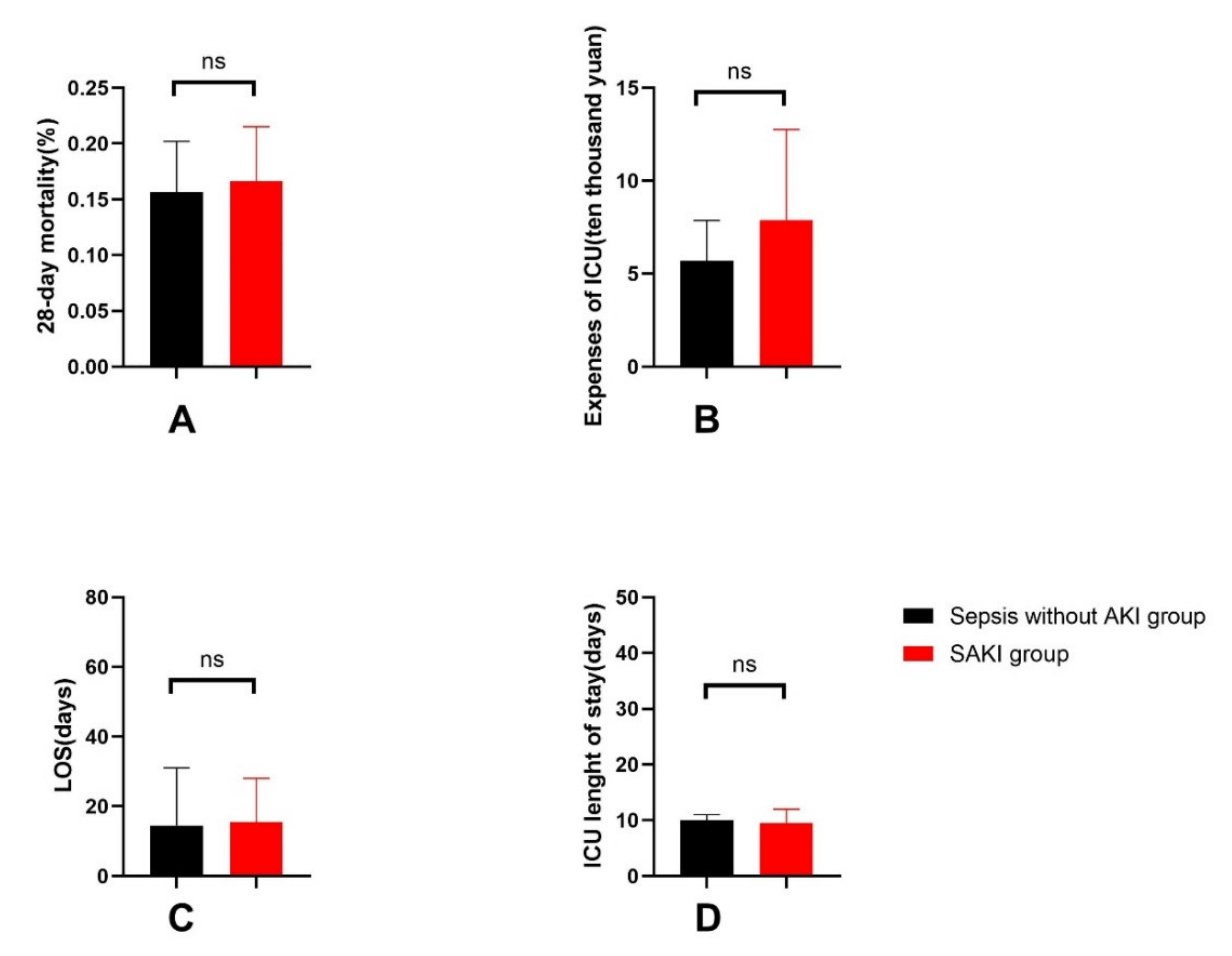
3.1.3. General Outcomes of Patients
3.1.4. Increased Th17/Treg Ratio in Patients with SAKI
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| Th17 | helper T cell 17 |
| Treg | regulatory T cell |
| ICU | intensive care unit |
| AKI | acute kidney injury |
| KDIGO | Kidney Disease: Improving Global Outcomes |
| SAKI | sepsis-induced acute kidney injury |
| BMI | body mass index |
| CKD | chronic kidney disease |
| COPD | chronic obstructive pulmonary disease |
| NAGL | neutrophil gelatinase-associated lipocalin |
| Cr | serum creatinine |
| BUN | blood urea nitrogen |
| WBC | white blood cell |
| GR | neutrophil granulocyte |
| LY | lymphocyte |
| NLR | neutrophil/lymphocyte ratio |
| PCT | procalcitonin |
| Lac | lactic acid |
| OI | oxygenation index |
| APACHE II | Acute Physiology and Chronic Health Evaluation |
| SOFA | Sepsis-Related Organ Failure Assessment |
| LOS | length of hospital stay |
| EDTA | ethylene diamine tetraacetic acid |
| PBMCs | peripheral mononuclear cells |
| IL-10 | Interleukin-10 |
| IL-17 | Interleukin-17 |
| TNF-α | Tumor necrosis factor alpha |
| ELISA | enzyme-linked immunosorbent assay |
| RRT | renal replacement therapy |
| IQRs | interquartile ranges |
| ROC | receiver operating characteristic curve |
| AUC | area under the curve |
| CI | confidence interval |
| IGFBP-7 | Insulin-like growth factor-binding protein-7 |
| TIMP-2 | Tissue inhibitor of metalloproteinase-2 |
References
- Singer, M.; Deutschman, C.S.; Seymour, C.W.; Shankar-Hari, M.; Annane, D.; Bauer, M.; Bellomo, R.; Bernard, G.R.; Chiche, J.-D.; Coopersmith, C.M.; et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA 2016, 315, 801–810. [Google Scholar] [CrossRef] [PubMed]
- Fleischmann, C.; Scherag, A.; Adhikari, N.K.; Hartog, C.S.; Tsaganos, T.; Schlattmann, P.; Angus, D.C.; Reinhart, K.; International Forum of Acute Care Trialists. Assessment of Global Incidence and Mortality of Hospital-treated Sepsis. Current Estimates and Limitations. Am. J. Respir. Crit. Care Med. 2016, 193, 259–272. [Google Scholar] [CrossRef] [PubMed]
- Rudd, K.E.; Johnson, S.C.; Agesa, K.M.; Shackelford, K.A.; Tsoi, D.; Kievlan, D.R.; Colombara, D.V.; Ikuta, K.S.; Kissoon, N.; Finfer, S.; et al. Global, regional, and national sepsis incidence and mortality, 1990–2017: Analysis for the Global Burden of Disease Study. Lancet 2020, 395, 200–211. [Google Scholar] [CrossRef] [Green Version]
- Healthcare Cost and Utilization Project (HCUP). HCUP Facts and Figures, 2006: Statistics on Hospital-Based Care in the United States; Agency for Healthcare Research and Quality: Rockville, MD, USA, 2008. [Google Scholar]
- Cohen, J.; Vincent, J.-L.; Adhikari, N.K.J.; Machado, F.R.; Angus, D.C.; Calandra, T.; Jaton, K.; Giulieri, S.; Delaloye, J.; Opal, S.; et al. Sepsis: A roadmap for future research. Lancet Infect. Dis. 2015, 15, 581–614. [Google Scholar] [CrossRef]
- Zhou, X.; Liu, J.F.; Ji, X.J.; Yang, X.; Duan, M. Predictive value of inflammatory markers for acute kidney injury in sepsis patients: Analysis of 753 cases in 7 years. Zhong Hua Wei Zhong Bing Ji Jiu Yi Xue 2018, 30, 346–350. [Google Scholar] [CrossRef]
- Manrique-Caballero, C.L.; Del Rio-Pertuz, G.; Gomez, H. Sepsis-Associated Acute Kidney Injury. Crit. Care Clin. 2021, 37, 279–301. [Google Scholar] [CrossRef] [PubMed]
- Orieux, A.; Boyer, A.; Dewitte, A.; Combe, C.; Rubin, S. Insuffisance rénale aiguë en soins intensifs-réanimation et ses conséquences: Mise au point. Nephrol. Ther. 2021, 18, 7–20. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.M.; Zhu, Y.; Zhang, J.; Xu, D.X.; Liu, Y.; Liu, F.; Peng, Z.y. Sepsis and acute kidney injury. Zhong Hua Yi Xue Za Zhi. 2021, 101, 1210–1213. [Google Scholar] [CrossRef]
- Kumar, V. T cells and their immunometabolism: A novel way to understanding sepsis immunopathogenesis and future therapeutics. Eur. J. Cell Biol. 2018, 97, 379–392. [Google Scholar] [CrossRef] [Green Version]
- Xia, H.; Wang, F.; Wang, M.; Wang, J.; Sun, S.; Chen, M.; Huang, S.; Chen, X.; Yao, S. Maresin1 ameliorates acute lung injury induced by sepsis through regulating Th17/Treg balance. Life Sci. 2020, 254, 117773. [Google Scholar] [CrossRef]
- Maravitsa, P.; Adamopoulou, M.; Pistiki, A.; Netea, M.G.; Louis, K.; Giamarellos-Bourboulis, E.J. Systemic over-release of interleukin-17 in acute kidney injury after septic shock: Clinical and experimental evidence. Immunol. Lett. 2016, 178, 68–76. [Google Scholar] [CrossRef] [PubMed]
- Yang, X.-Y.; Song, J.; Hou, S.-K.; Fan, H.-J.; Lv, Q.; Liu, Z.-Q.; Ding, H.; Zhang, Y.-Z.; Liu, J.-Y.; Dong, W.-L.; et al. Ulinastatin ameliorates acute kidney injury induced by crush syndrome inflammation by modulating Th17/Treg cells. Int. Immunopharmacol. 2020, 81, 106265. [Google Scholar] [CrossRef] [PubMed]
- Kinsey, G.R.; Sharma, R.; Okusa, M.D. Regulatory T Cells in AKI. J. Am. Soc. Nephrol. 2013, 24, 1720–1726. [Google Scholar] [CrossRef] [PubMed]
- Sharma, R.; Kinsey, G.R. Regulatory T cells in acute and chronic kidney diseases. Am. J. Physiol. Physiol. 2018, 314, F679–F698. [Google Scholar] [CrossRef] [Green Version]
- Lee, S.-Y.; Lee, Y.-S.; Choi, H.-M.; Ko, Y.-S.; Lee, H.-Y.; Jo, S.-K.; Cho, W.-Y.; Kim, H.-K. Distinct pathophysiologic mechanisms of septic acute kidney injury. Crit. Care Med. 2012, 40, 2997–3006. [Google Scholar] [CrossRef]
- Chen, L.; Lu, Y.; Zhao, L.; Hu, L.; Qiu, Q.; Zhang, Z.; Li, M.; Hong, G.; Wu, B.; Zhao, G.; et al. Curcumin attenuates sepsis-induced acute organ dysfunction by preventing inflammation and enhancing the suppressive function of Tregs. Int. Immunopharmacol. 2018, 61, 1–7. [Google Scholar] [CrossRef]
- Kellum, J.A.; Lameire, N.; KDIGO AKI Guideline Work Group. Diagnosis, evaluation, and management of acute kidney injury: A KDIGO summary (Part 1). Crit. Care 2013, 17, 204. [Google Scholar] [CrossRef] [Green Version]
- Yu, Z.-X.; Ji, M.-S.; Yan, J.; Cai, Y.; Liu, J.; Yang, H.-F.; Li, Y.; Jin, Z.-C.; Zheng, J.-X. The ratio of Th17/Treg cells as a risk indicator in early acute respiratory distress syndrome. Crit. Care 2015, 19, 82. [Google Scholar] [CrossRef] [Green Version]
- Imiela, A.M.; Mikołajczyk, T.P.; Siedliński, M.; Dobrowolski, P.; Konior-Rozlachowska, A.; Wróbel, A.; Biernat-Kałuża, E.; Januszewicz, M.; Guzik, B.; Guzik, T.J.; et al. The Th17/Treg imbalance in patients with primary hyperaldosteronism and resistant hypertension. Pol. Arch. Intern. Med. 2022, 132, 16171. [Google Scholar] [CrossRef]
- Zhang, S.; Gang, X.; Yang, S.; Cui, M.; Sun, L.; Li, Z.; Wang, G. The Alterations in and the Role of the Th17/Treg Balance in Metabolic Diseases. Front. Immunol. 2021, 12, 678355. [Google Scholar] [CrossRef]
- Lourenço, J.D.; Ito, J.T.; Martins, M.D.A.; Tibério, I.D.F.L.C.; Lopes, F.D.T.Q.D.S. Th17/Treg Imbalance in Chronic Obstructive Pulmonary Disease: Clinical and Experimental Evidence. Front. Immunol. 2021, 12, 804919. [Google Scholar] [CrossRef] [PubMed]
- Drescher, H.K.; Bartsch, L.M.; Weiskirchen, S.; Weiskirchen, R. Intrahepatic TH17/TReg Cells in Homeostasis and Disease—It’s All About the Balance. Front. Pharmacol. 2020, 11, 588436. [Google Scholar] [CrossRef] [PubMed]
- Luo, S.; Yang, M.; Jin, H.; Xu, Z.-Q.; Li, Y.-F.; Xia, P.; Yang, Y.-R.; Chen, B.-C.; Zhang, Y. The role of sildenafil in the development of transplant arteriosclerosis in rat aortic grafts. Am. J. Transl. Res. 2017, 9, 4914–4924. [Google Scholar] [PubMed]
- Hou, H.; Sun, Y.; Miao, J.; Gao, M.; Guo, L.; Song, X. Ponesimod modulates the Th1/Th17/Treg cell balance and ameliorates disease in experimental autoimmune encephalomyelitis. J. Neuroimmunol. 2021, 356, 577583. [Google Scholar] [CrossRef]
- Devarajan, P. Neutrophil gelatinase-associated lipocalin: A promising biomarker for human acute kidney injury. Biomarkers Med. 2010, 4, 265–280. [Google Scholar] [CrossRef] [Green Version]
- Kashani, K.; Al-Khafaji, A.; Ardiles, T.; Artigas, A.; Bagshaw, S.M.; Bell, M.; Bihorac, A.; Birkhahn, R.; Cely, C.M.; Chawla, L.S.; et al. Discovery and validation of cell cycle arrest biomarkers in human acute kidney injury. Crit. Care 2013, 17, R25. [Google Scholar] [CrossRef] [Green Version]
- Liu, J.; Wang, Z.; Lin, J.; Li, T.; Guo, X.; Pang, R.; Dong, L.; Duan, M. Xuebijing injection in septic rats mitigates kidney injury, reduces cortical microcirculatory disorders, and suppresses activation of local inflammation. J. Ethnopharmacol. 2021, 276, 114199. [Google Scholar] [CrossRef]
- Carney, E. Targeting Treg cells to protect the kidney. Nat. Rev. Nephrol. 2017, 13, 444. [Google Scholar] [CrossRef]
- Jun, C.; Ke, W.; Qingshu, L.; Ping, L.; Jun, D.; Jie, L.; Bo, C.; Su, M. Protective effect of CD4+CD25highCD127low regulatory T cells in renal ischemia–reperfusion injury. Cell. Immunol. 2014, 289, 106–111. [Google Scholar] [CrossRef]
- Gandolfo, M.T.; Jang, H.R.; Bagnasco, S.M.; Ko, G.-J.; Agreda, P.; Satpute, S.R.; Crow, M.T.; King, L.S.; Rabb, H. Foxp3+ regulatory T cells participate in repair of ischemic acute kidney injury. Kidney Int. 2009, 76, 717–729. [Google Scholar] [CrossRef] [Green Version]
- Ramani, K.; Jawale, C.V.; Verma, A.; Coleman, B.M.; Kolls, J.K.; Biswas, P.S. Unexpected kidney-restricted role for IL-17 receptor signaling in defense against systemic Candida albicans infection. JCI Insight 2018, 3, e98241. [Google Scholar] [CrossRef] [PubMed]
- Mehrotra, P.; Collett, J.A.; McKinney, S.D.; Stevens, J.; Ivancic, C.M.; Basile, D.P. IL-17 mediates neutrophil infiltration and renal fibrosis following recovery from ischemia reperfusion: Compensatory role of natural killer cells in athymic rats. Am. J. Physiol. Physiol. 2017, 312, F385–F397. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dolff, S.; Witzke, O.; Wilde, B. Th17 cells in renal inflammation and autoimmunity. Autoimmun. Rev. 2018, 18, 129–136. [Google Scholar] [CrossRef] [PubMed]
- Nakashima, T.; DESIRE Trial Investigators; Miyamoto, K.; Shima, N.; Kato, S.; Kawazoe, Y.; Ohta, Y.; Morimoto, T.; Yamamura, H. Dexmedetomidine improved renal function in patients with severe sepsis: An exploratory analysis of a randomized controlled trial. J. Intensiv. Care 2020, 8, 1. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dewayani, A.; Fauzia, K.; Alfaray, R.; Waskito, L.; Doohan, D.; Rezkitha, Y.; Abdurachman, A.; Kobayashi, T.; I’Tishom, R.; Yamaoka, Y.; et al. The Roles of IL-17, IL-21, and IL-23 in the Helicobacter pylori Infection and Gastrointestinal Inflammation: A Review. Toxins 2021, 13, 315. [Google Scholar] [CrossRef]
- Nalesso, F.; Cattarin, L.; Gobbi, L.; Fragasso, A.; Garzotto, F.; Calò, L.A. Evaluating Nephrocheck® as a Predictive Tool for Acute Kidney Injury. Int. J. Nephrol. Renov. Dis. 2020, 13, 85–96. [Google Scholar] [CrossRef] [Green Version]
- Hahn, R.G.; Yanase, F.; Zdolsek, J.H.; Tosif, S.H.; Bellomo, R.; Weinberg, L. Serum Creatinine Levels and Nephrocheck® Values with and Without Correction for Urine Dilution-A Multicenter Observational Study. Front. Med. 2022, 9, 847129. [Google Scholar] [CrossRef]
- Jia, J.; Gong, X.; Zhao, Y.; Yang, Z.; Ji, K.; Luan, T.; Zang, B.; Li, G. Autophagy Enhancing Contributes to the Organ Protective Effect of Alpha-Lipoic Acid in Septic Rats. Front. Immunol. 2019, 10, 1491. [Google Scholar] [CrossRef]


| Total (n = 124) | SAKI Group (n = 60) | Sepsis-without-AKI Group (n = 64) | Test Value | p Value | |
|---|---|---|---|---|---|
| Male [n (%)] | 70 (56.5) | 38 (63.3) | 32 (50.0) | 2.239 | 0.135 |
| Age—year (median [Q1, Q2]) | 67.50 (55.00, 75.00) | 67.50 (54.00, 76.00) | 67.50 (56.25, 74.50) | −0.130 | 0.896 |
| BMI—kg/m2 (mean ± SD) | 23.70 ± 4.79 | 23.33 ± 4.76 | 23.95 ± 4.84 | 0.586 | 0.559 |
| Comorbidities | |||||
| Hypertension [n (%)] | 74 (59.7) | 40 (66.7) | 34 (53.1) | 2.360 | 0.124 |
| Diabetes [n (%)] | 36 (29.0) | 22 (36.7) | 14 (21.9) | 3.289 | 0.070 |
| CKD [n (%)] | 20 (16.1) | 10 (16.7) | 10 (15.6) | 0.025 | 0.875 |
| Chronic cardiovascular disease [n (%)] | 50 (40.3) | 26 (43.3) | 24 (37.5) | 0.438 | 0.508 |
| Chronic lung disease [n (%)] | 16 (12.9) | 10 (16.7) | 6 (9.4) | 1.465 | 0.226 |
| Chronic liver disease [n (%)] | 8 (6.5) | 2 (3.3) | 6 (9.4) | 1.873 | 0.171 |
| Nervous system disease [n (%)] | 36 (29.0) | 14 (23.3) | 22 (34.4) | 1.832 | 0.176 |
| Rheumatic system disease [n (%)] | 4 (3.2) | 2 (3.3) | 2 (3.1) | 0.004 | 0.948 |
| Malignant tumor [n (%)] | 38 (30.6) | 16 (26.7) | 22 (34.4) | 0.866 | 0.352 |
| Physiological parameters | |||||
| SOFA score (median [Q1, Q2]) | 7.00 (4.00, 8.00) | 8.00 (6.00, 11.00) | 4.50 (3.00, 7.00) | −5.554 | 0.000 *** |
| APACHEII score (median [Q1, Q2]) | 20.00 (15.00, 25.00) | 20.50 (15.00, 25.00) | 20.00 (15.00, 25.00) | −0.271 | 0.787 |
| Septic shock [n (%)] | 84 (67.7) | 46 (76.7) | 38 (59.4) | 4.237 | 0.040 * |
| Numbers of organs with injuries caused by infection (median [Q1, Q2]) | 3 (2, 5) | 4 (3, 5) | 2 (1, 3) | −6.138 | 0.000 *** |
| Site of infection | |||||
| respiratory system [n (%)] | 58 (46.8) | 22 (36.7) | 36 (56.3) | 4.770 | 0.029 * |
| urinary system [n (%)] | 20 (16.1) | 18 (30.0) | 2 (3.1) | 16.534 | 0.000 *** |
| gastrointestinal [n (%)] | 4 (3.2) | 4 (6.7) | 0 (0) | 4.409 | 0.036 * |
| biliary tract [n (%)] | 6 (4.8) | 4 (6.7) | 2 (3.1) | 0.844 | 0.358 |
| Thoracic and abdominal cavity [n (%)] | 84 (67.7) | 32 (53.5) | 52 (81.3) | 11.044 | 0.001 ** |
| bloodstream [n (%)] | 4 (3.2) | 2 (3.3) | 2 (3.1) | 0.004 | 0.948 |
| skin and soft tissue [n (%)] | 2 (1.6) | 0 (0) | 2 (3.1) | 1.906 | 0.167 |
| central nervous system [n (%)] | 4 (3.2) | 0 (0) | 4 (6.3) | 3.875 | 0.049 * |
| NAGL—ng/ mL(median [Q1, Q2]) | 60.021 (53.190, 75.104) | 74.101 (60.013, 80.943) | 54.676 (51.057, 61.933) | −5.161 | 0.000 *** |
| Urine output—L/24 h (median [Q1, Q2]) | 1.81 (1.15, 2.47) | 1.21 (0.38, 2.21) | 2.02 (1.37, 2.67) | −3.120 | 0.002 ** |
| Cr—umol/L (median [Q1, Q2]) | 80.55 (59.80, 128.10) | 130.55 (100.40, 229.65) | 63.70 (50.28, 74.13) | −8.081 | 0.000 *** |
| BUN—mmol/L (median [Q1, Q2]) | 9.92 (5.89, 15.12) | 12.90 (10.22, 21.89) | 6.34 (4.38, 8.42) | −5.821 | 0.000 *** |
| PCT—ng/ mL(median [Q1, Q2]) | 2.91 (0.70, 19.40) | 19.07 (3.31, 33.84) | 1.31 (0.55, 4.44) | −5.594 | 0.000 *** |
| Lac—mmol/L (median [Q1, Q2]) | 1.50 (1.10, 2.00) | 1.80 (1.15, 3.08) | 1.40 (1.00, 1.83) | −3.054 | 0.002 ** |
| OI (median [Q1, Q2]) | 248.00 (180.00, 342.00) | 245.00 (184.50, 368.75) | 257.00 (178.25, 325.75) | −0.760 | 0.447 |
| WBC—x109/L (median [Q1, Q2]) | 11.57 (8.17, 16.77) | 12.49 (7.99, 22.18) | 12.02 (8.28, 14.59) | −1.180 | 0.238 |
| GR—x109/L (median [Q1, Q2]) | 10.29 (6.84, 15.09) | 11.45 (7.08, 20.03) | 10.41 (6.78, 12.92) | −1.600 | 0.110 |
| LY—x109/L (median [Q1, Q2]) | 0.72 (0.50, 1.08) | 0.72 (0.47, 1.28) | 0.87 (0.54, 1.13) | −0.720 | 0.471 |
| NLR (median [Q1, Q2]) | 13.31 (8.72, 20.56) | 16.65 (0.24, 32.78) | 11.80 (7.71, 18.40) | −2.680 | 0.007 ** |
| Immune indexes | |||||
| T-lymphocyte ratio—% (median [Q1, Q2]) | 69.01 (62.58, 78.81) | 68.81 (55.49, 75.65) | 70.59 (62.91, 83.97) | −1.301 | 0.193 |
| CD4+ T-lymphocyte ratio—% (median [Q1, Q2]) | 40.50 (27.72, 50.74) | 39.72 (27.88, 49.54) | 42.79 (26.69, 51.18) | −0.410 | 0.682 |
| Treg cell ratio—% (median [Q1, Q2]) | 1.40 (0.77, 2.25) | 1.34 (0.59, 2.32) | 1.49 (0.86, 2.23) | −0.510 | 0.610 |
| Th17 cell ratio—% (median [Q1, Q2]) | 0.13 (0.08, 0.23) | 0.15 (0.11, 0.24) | 0.09 (0.06, 0.19) | −3.511 | 0.000 *** |
| Th17/Treg ratio (median [Q1, Q2]) | 0.10 (0.05, 0.21) | 0.11 (0.07, 0.28) | 0.06 (0.05, 0.16) | −3.240 | 0.001 ** |
| IL10—pg/ mL(median [Q1, Q2]) | 25.55 (10.70, 63.84) | 35.55 (25.46, 109.01) | 14.48 (7.41, 37.94) | −4.541 | 0.000 *** |
| IL17—pg/ mL(median [Q1, Q2]) | 2.70 (1.03, 6.48) | 4.87 (2.03, 12.02) | 1.71 (0.70, 3.32) | −4.399 | 0.000 *** |
| TNF-α—pg/ mL(median [Q1, Q2]) | 6.48 (4.03, 11.16) | 8.51 (4.05, 12.98) | 5.59 (3.95, 10.55) | −0.403 | 0.687 |
| General outcomes | |||||
| 28-day mortality [n (%)] | 20 (16.1) | 10 (16.7) | 10 (15.6) | 0.025 | 0.875 |
| Hospital length of stay in days (median [Q1, Q2]) | 15.00 (10.00, 35.00) | 15.50 (8.00, 32.00) | 14.50 (10.00, 39.50) | −0.671 | 0.502 |
| ICU length of stay in days (median [Q1, Q2]) | 10.00 (6.00, 17.00) | 9.50 (7.00, 17.00) | 10.00 (5.00, 17.50) | −0.802 | 0.423 |
| Expenses in ICU—CNY ten thousand (median [Q1, Q2]) | 7.06 (3.47, 14.08) | 7.90 (4.04, 17.84) | 5.69 (3.46, 13.64) | −1.430 | 0.153 |
| Treatments during hospitalization | |||||
| ventilator [n (%)] | 72 (58.1) | 36 (60.0) | 36 (56.3) | 0.179 | 0.672 |
| vasoactive drugs [n (%)] | 78 (62.9) | 44 (73.3) | 34 (53.1) | 5.420 | 0.020 |
| blood transfusion [n (%)] | 38 (30.6) | 28 (46.7) | 10 (15.6) | 14.040 | 0.000 *** |
| Univariable Logistic Regression | Multivariable Logistic Regression | |||
|---|---|---|---|---|
| Odds Ratio (95% CI) | p Value | Odds Ratio (95% CI) | p Value | |
| SOFA | 1.49 (1.27–1.75) | 0.000 *** | 1.41 (1.13–1.75) | 0.002 ** |
| Septic shock | 0.45 (0.20–0.97) | 0.042 * | ||
| Infection of respiratory system | 2.22 (1.08–4.57) | 0.030 * | ||
| Infection of urinary system | 0.08 (0.02–0.34) | 0.001 ** | ||
| Infection of gastrointestinal | - | 0.999 | ||
| Infection of thoracic and abdominal cavity | 3.79 (1.69–8.50) | 0.001 ** | ||
| Infection of central nervous system | - | 0.999 | ||
| Number of organ dysfunctions caused by infection | 2.44 (1.78–3.36) | 0.000 *** | ||
| Use of vasoactive drugs | 0.41 (0.19–0.88) | 0.021 * | ||
| Use of blood transfusion | 0.21 (0.09–0.49) | 0.000 *** | ||
| NAGL | 1.06 (1.03–1.09) | 0.000 *** | 1.08 (1.03–1.31) | 0.000 *** |
| Urine output | 0.58 (0.41–0.82) | 0.002 ** | ||
| Cr | 1.04 (1.02–1.060) | 0.000 *** | ||
| BUN | 1.26 (1.15–1.39) | 0.000 *** | ||
| PCT | 1.09 (1.05–1.14) | 0.000 *** | 1.07 (1.02–1.13) | 0.002 ** |
| Lac | 1.33 (1.04–1.72) | 0.022 * | ||
| NLR | 1.01 (0.99–1.02) | 0.249 | ||
| Th17 | 95.39 (3.45–2600.43) | 0.007 ** | ||
| IL-10 | 1.01 (1.00–1.01) | 0.021 * | 0.99 (0.98–1.00) | 0.266 |
| IL-17 | 1.15 (1.06–1.24) | 0.006 ** | 1.12 (1.00–1.25) | 0.054 |
| Th17/Treg ratio | 46.63 (2.93–741.578) | 0.001 ** | 144.99 (1.20–17,383.77) | 0.034 * |
| Odds Ratio (95% CI) | p Value | |
|---|---|---|
| High Th17/Treg ratio | 8.16 (1.89–35.14) | 0.005 ** |
| SOFA | 1.36 (1.10–1.70) | 0.005 ** |
| PCT | 1.10 (1.04–1.15) | 0.000 *** |
| NAGL | 1.06 (1.02–1.11) | 0.001 ** |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhou, X.; Yao, J.; Lin, J.; Liu, J.; Dong, L.; Duan, M. Th17/Regulatory T-Cell Imbalance and Acute Kidney Injury in Patients with Sepsis. J. Clin. Med. 2022, 11, 4027. https://doi.org/10.3390/jcm11144027
Zhou X, Yao J, Lin J, Liu J, Dong L, Duan M. Th17/Regulatory T-Cell Imbalance and Acute Kidney Injury in Patients with Sepsis. Journal of Clinical Medicine. 2022; 11(14):4027. https://doi.org/10.3390/jcm11144027
Chicago/Turabian StyleZhou, Xiao, Jingyi Yao, Jin Lin, Jingfeng Liu, Lei Dong, and Meili Duan. 2022. "Th17/Regulatory T-Cell Imbalance and Acute Kidney Injury in Patients with Sepsis" Journal of Clinical Medicine 11, no. 14: 4027. https://doi.org/10.3390/jcm11144027
APA StyleZhou, X., Yao, J., Lin, J., Liu, J., Dong, L., & Duan, M. (2022). Th17/Regulatory T-Cell Imbalance and Acute Kidney Injury in Patients with Sepsis. Journal of Clinical Medicine, 11(14), 4027. https://doi.org/10.3390/jcm11144027






