Predictors of Surgical Intervention for Pediatric Acute Rhinosinusitis with Periorbital Infection
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patients
2.2. Outcome
2.3. Statistical Analysis
2.4. Ethics
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Wald, E.R.; Applegate, K.E.; Bordley, C.; Darrow, D.H.; Glode, M.P.; Marcy, S.M.; Nelson, C.E.; Rosenfeld, R.M.; Shaikh, N.; Smith, M.J.; et al. Clinical Practice Guideline for the Diagnosis and Management of Acute Bacterial Sinusitis in Children Aged 1 to 18 Years. Pediatrics 2013, 132, e262–e280. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Levy, D.A.; Pecha, P.P.; Nguyen, S.A.; Schlosser, R.J. Trends in complications of pediatric rhinosinusitis in the United States from 2006 to 2016. Int. J. Pediatr. Otorhinolaryngol. 2020, 128, 109695. [Google Scholar] [CrossRef] [PubMed]
- Wu, D.; Wasserman, J.; Boruk, M. Practice Patterns of Systemic Corticosteroid Use in Complicated Acute Rhinosinusitis Among Rhinologists and Pediatric Otolaryngologist. Am. J. Rhinol. Allergy 2018, 32, 485–490. [Google Scholar] [CrossRef] [PubMed]
- Chandler, J.R.; Langenbrunner, D.J.; Stevens, E.R. The pathogenesis of orbital complications in acute sinusitis. Laryngoscope 1970, 80, 1414–1428. [Google Scholar] [CrossRef] [PubMed]
- Le, T.D.; Liu, E.S.; Adatia, F.A.; Buncic, J.R.; Blaser, S. The effect of adding orbital computed tomography findings to the Chandler criteria for classifying pediatric orbital cellulitis in predicting which patients will require surgical intervention. J. Am. Assoc. Pediatr. Ophthalmol. Strabismus 2014, 18, 271–277. [Google Scholar] [CrossRef]
- Lee, S.; Fernandez, J.; Mirjalili, S.A.; Kirkpatrick, J. Pediatric paranasal sinuses-Development, growth, pathology, & functional endoscopic sinus surgery. Clin. Anat. 2022. [Google Scholar] [CrossRef]
- Torretta, S.; Guastella, C.; Ibba, T.; Gaffuri, M.; Pignataro, L. Surgical Treatment of Paediatric Chronic Rhinosinusitis. J. Clin. Med. 2019, 8, 684. [Google Scholar] [CrossRef] [Green Version]
- Capra, G.; Liming, B.; Boseley, M.E.; Brigger, M.T. Trends in Orbital Complications of Pediatric Rhinosinusitis in the United States. JAMA Otolaryngol. Head Neck Surg. 2015, 141, 12–17. [Google Scholar] [CrossRef] [Green Version]
- Segal, N.; Nissani, R.; Kordeluk, S.; Holcberg, M.; Hertz, S.; Kassem, F.; Mansour, A.; Segal, A.; Gluck, O.; Roth, Y.; et al. Orbital compli-cations associated with paranasal sinus infections—A 10-year experience in Israel. Int. J. Pediatr. Otorhinolaryngol. 2016, 86, 60–62. [Google Scholar] [CrossRef]
- Sciarretta, V.; Demattè, M.; Farneti, P.; Fornaciari, M.; Corsini, I.; Piccin, O.; Saggese, D.; Fernandez, I.J. Management of orbital celluli-tis and subperiosteal orbital abscess in pediatric patients: A ten-year review. Int. J. Pediatr. Otorhinolaryngol. 2017, 96, 72–76. [Google Scholar] [CrossRef]
- Arjmand, E.M.; Lusk, R.P.; Muntz, H.R. Pediatric Sinusitis and Subperiosteal Orbital Abscess Formation: Diagnosis and Treatment. Otolaryngol. Neck Surg. 1993, 109, 886–894. [Google Scholar] [CrossRef] [PubMed]
- Mair, E.A.; Bolger, W.E.; Breisch, E.A. Sinus and Facial Growth After Pediatric Endoscopic Sinus Surgery. Arch. Otolaryngol.-Head Neck Surg. 1995, 121, 547–552. [Google Scholar] [CrossRef] [PubMed]
- Carpenter, K.M.; Graham, S.; Smith, R. Facial Skeletal Growth after Endoscopic Sinus Surgery in the Piglet Model. Am. J. Rhinol. 1997, 11, 211–217. [Google Scholar] [CrossRef]
- Wong, S.J.; Levi, J. Management of pediatric orbital cellulitis: A systematic review. Int. J. Pediatr. Otorhinolaryngol. 2018, 110, 123–129. [Google Scholar] [CrossRef]
- Tabarino, F.; Elmaleh-Bergès, M.; Quesnel, S.; Lorrot, M.; Abbeele, T.V.D.; Teissier, N. Subperiosteal orbital abscess: Volumetric criteria for surgical drainage. Int. J. Pediatr. Otorhinolaryngol. 2015, 79, 131–135. [Google Scholar] [CrossRef] [PubMed]
- McDermott, S.M.; Onwuka, A.; Elmaraghy, C.; Walz, P.C. Management Patterns in Pediatric Complicated Sinusitis. Otolaryngol. Neck Surg. 2020, 163, 814–821. [Google Scholar] [CrossRef]
- Adil, E.A.; Muir, M.E.; Kawai, K.; Dombrowski, N.D.; Cunningham, M.J. Pediatric Subperiosteal Abscess Secondary to Acute Sinusi-tis: A Systematic Review and Meta-analysis. Laryngoscope 2020, 130, 2906–2912. [Google Scholar] [CrossRef]
- Wu, T.-Y.; Majeed, A.; Kuo, K.N. An overview of the healthcare system in Taiwan. Lond. J. Prim. Care 2010, 3, 115–119. [Google Scholar] [CrossRef] [Green Version]
- Topilow, N.J.; Tran, A.Q.; Koo, E.B.; Alabiad, C.R. Etiologies of proptosis: A review. Intern. Med. Rev. 2020, 6. [Google Scholar] [CrossRef]
- Oxford, L.E.; McClay, J. Medical and surgical management of subperiosteal orbital abscess secondary to acute sinusitis in chil-dren. Int. J. Pediatr. Otorhinolaryngol. 2006, 70, 1853–1861. [Google Scholar] [CrossRef]
- Rahbar, R.; Robson, C.D.; Petersen, R.A.; DiCanzio, J.; Rosbe, K.W.; McGill, T.J.; Healy, G.B. Management of orbital subperiosteal ab-scess in children. Arch. Otolaryngol. Head Neck Surg. 2001, 127, 281–286. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Smith, J.M.; Bratton, E.M.; DeWitt, P.; Davies, B.W.; Hink, E.M.; Durairaj, V.D. Predicting the need for surgical intervention in pediat-ric orbital cellulitis. Am. J. Ophthalmol. 2014, 158, 387–394.e1. [Google Scholar] [CrossRef] [PubMed]
- McCoy, J.L.; Dixit, R.; Dohar, J.E.; Tobey, A.B. Pediatric subperiosteal orbital abscess characterization and prediction of size, location, and management. Int. J. Pediatr. Otorhinolaryngol. 2021, 144, 110693. [Google Scholar] [CrossRef] [PubMed]
- Wei, S.-H.; Chiang, C.-S.; Chen, C.-L.; Chiu, C.-H. Pneumococcal disease and use of pneumococcal vaccines in Taiwan. Clin. Exp. Vaccine Res. 2015, 4, 121–129. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Peña, M.T.; Preciado, D.; Orestes, M.; Choi, S. Orbital complications of acute sinusitis: Changes in the post-pneumococcal vaccine era. JAMA Otolaryngol. Head Neck Surg. 2013, 139, 223–227. [Google Scholar] [CrossRef] [Green Version]
- McCoul, E.D.; Jourdy, D.N.; Schaberg, M.R.; Anand, V.K. Methicillin-resistant Staphylococcus aureus sinusitis in nonhospitalized patients: A systematic review of prevalence and treatment outcomes. Laryngoscope 2012, 122, 2125–2131. [Google Scholar] [CrossRef]
- Shih, E.J.; Chen, J.K.; Tsai, P.J.; Bee, Y.S. Differences in characteristics, aetiologies, isolated pathogens, and the efficacy of antibiotics in adult patients with preseptal cellulitis and orbital cellulitis between 2000–2009 and 2010–2019. Br. J. Ophthalmol. 2021. online ahead of print. [Google Scholar] [CrossRef]
- Dykewicz, M.S. 7. Rhinitis and sinusitis. J. Allergy Clin. Immunol. 2003, 111 (Suppl. S2), S520–S529. [Google Scholar] [CrossRef]
- Mahalingam, S.; Hone, R.; Lloyd, G.; Grounds, R.; Shamil, E.; Wong, G.; Al-Lami, A.; Pervez, A.; Rudd, J.; Poon, J.S.; et al. The manage-ment of periorbital cellulitis secondary to sinonasal infection: A multicenter prospective study in the United Kingdom. Int. Forum Allergy Rhinol. 2020, 10, 726–737. [Google Scholar] [CrossRef]
| Age, years (±SD) | 6.94 (± 4.99) |
| Gender | |
| Male, N (%) | 74 (52.48) |
| Female, N (%) | 67 (47.52) |
| Hospital-staying period, days (±SD) | 9.74 (±7.98) |
| Symptoms onset to intravenous antibiotics, days (±SD) | 2.50 (±1.64) |
| Surgical intervention, N (%) | 42 (29.79) |
| Extent of Disease | N (%) | Surgical Rate, N (%) |
|---|---|---|
| Chandler’s classification | ||
| Stage I | 54 (38) | 1 (2) |
| Stage II | 22 (16) | 5 (23) |
| Stage III | 55 (39) | 26 (47) |
| Stage IV | 9 (22) | 9 (100) |
| Stage V | 1 (0.7) | 1 (100) |
| Patient Variables | Medical Therapy (N = 99) | Surgical Therapy (N = 42) | p-Value (Univariable) |
|---|---|---|---|
| Age, years | 6.73 ± 4.90 | 7.45 ± 5.21 | 0.435 |
| Hospital-staying period, days | 7.65 ± 4.46 | 14.69 ± 11.59 | <0.001 *** |
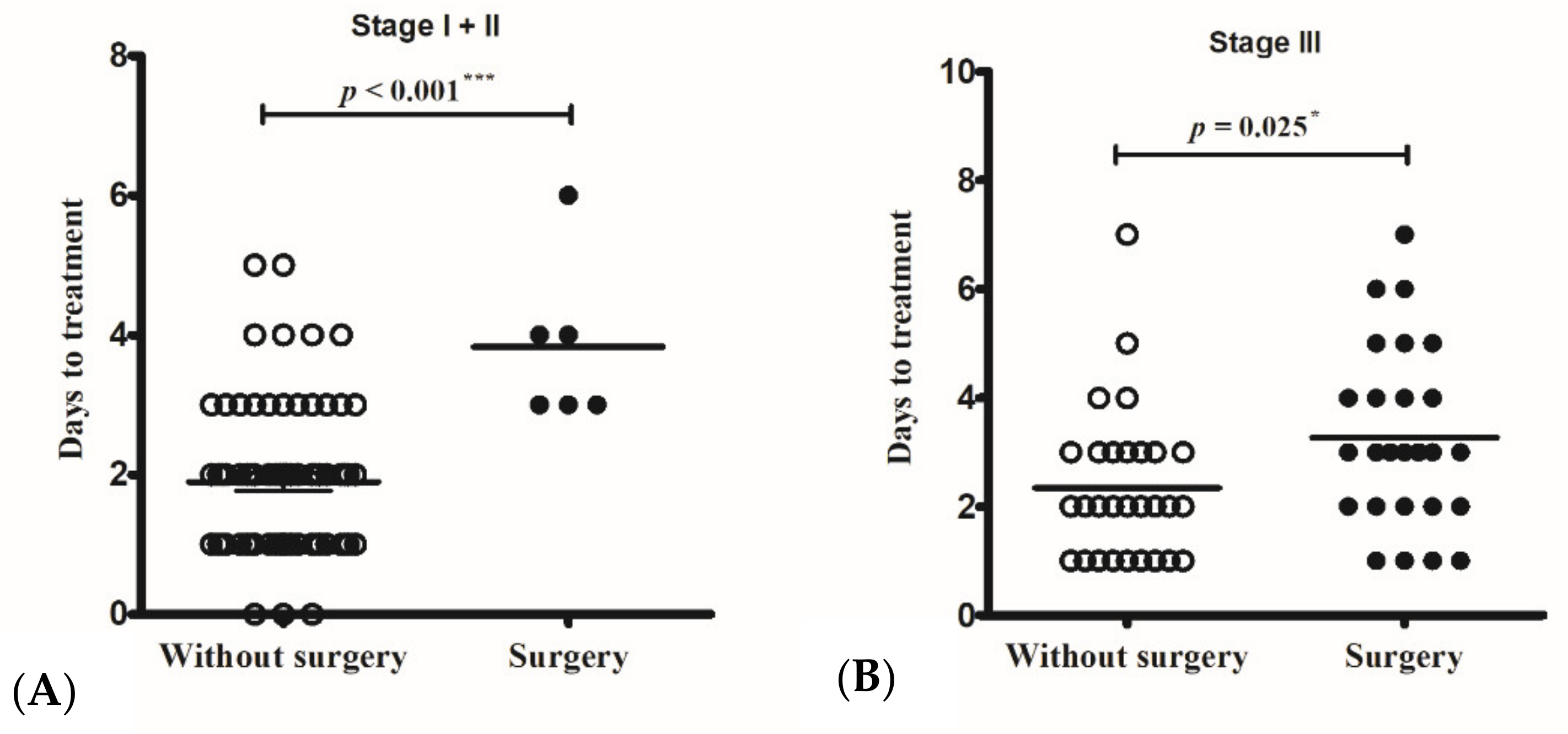
| Symptoms onset to parenteral antibiotic, days | 2.03 ± 1.20 | 3.62 ± 1.99 | <0.001 *** |
| Male gender | 54 (55%) | 20 (48%) | 0.467 |
| Symptoms at presentation | |||
| Underlying diseases | |||
| Asthma | 3 (3%) | 2 (5%) | 0.634 |
| Allergic rhinitis | 15 (15%) | 10 (24%) | 0.234 |
| Chronic sinusitis | 4 (4%) | 3 (7%) | 0.425 |
| Fever | 72 (72%) | 36 (86%) | 0.128 |
| Purulent rhinorrhea | 65 (66%) | 34 (81%) | 0.074 |
| Headache | 13 (13%) | 10 (24%) | 0.137 |
| EOM limitation | 19 (19%) | 25 (60%) | <0.001 *** |
| Proptosis | 32 (32%) | 36 (86%) | <0.001 *** |
| Periorbital pain/swelling | 99 (100%) | 42 (100%) | 1.000 |
| Blurred vision | 2 (2%) | 5 (12%) | 0.024 * |
| Conscious change | 0 (0%) | 1 (2%) | 0.298 |
| CNS involvement | 0 (0%) | 4 (%) | 0.007 ** |
| Laboratory data at presentation | |||
| WBC, per μL | 14,387 ± 5819 | 15,767 ± 4339 | 0.170 |
| Segment, % | 66.75 ± 17.84 | 71.89 ± 15.29 | 0.106 |
| Band form, % | 0.28 ± 0.76 | 1.85 ± 5.17 | 0.004 ** |
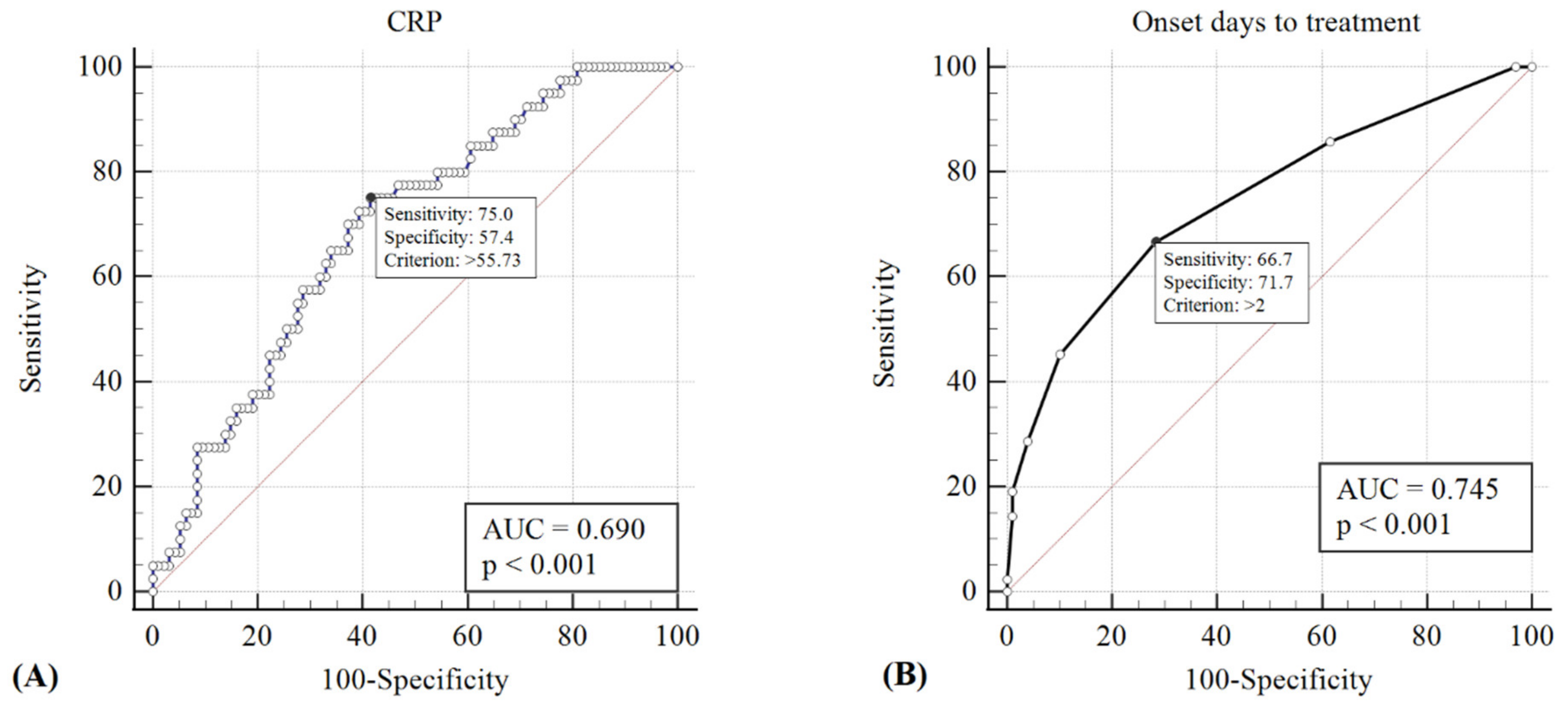
| CRP, mg/L | 63.30 ± 57.01 | 101.14 ± 67.79 | 0.001 ** |
| Variable | OR | 95% CI | β | SE (β) | p Value |
|---|---|---|---|---|---|
| Age (years) | 0.95 | 0.852–1.064 | −0.048 | 0.056 | 0.386 |
| Symptoms onset to intravenous antibiotics (days) | 1.94 | 1.339–2.795 | 0.660 | 0.187 | <0.001 *** |
| Gender (male) | 0.87 | 0.325–2.356 | −0.133 | 0.505 | 0.791 |
| EOM limitation | 1.10 | 0.312–3.906 | 0.099 | 0.644 | 0.877 |
| Proptosis | 6.63 | 1.634–26.909 | 1.891 | 0.714 | 0.008 ** |
| Blurred vision | 2.41 | 0.325–17.914 | 0.880 | 1.022 | 0.389 |
| Band neutrophil | 1.34 | 0.845–2.138 | 0.295 | 0.236 | 0.212 |
| CRP | 1.00 | 0.996–1.012 | 0.004 | 0.004 | 0.283 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wu, P.-W.; Lin, Y.-L.; Lee, Y.-S.; Chiu, C.-H.; Lee, T.-J.; Huang, C.-C. Predictors of Surgical Intervention for Pediatric Acute Rhinosinusitis with Periorbital Infection. J. Clin. Med. 2022, 11, 3831. https://doi.org/10.3390/jcm11133831
Wu P-W, Lin Y-L, Lee Y-S, Chiu C-H, Lee T-J, Huang C-C. Predictors of Surgical Intervention for Pediatric Acute Rhinosinusitis with Periorbital Infection. Journal of Clinical Medicine. 2022; 11(13):3831. https://doi.org/10.3390/jcm11133831
Chicago/Turabian StyleWu, Pei-Wen, Yen-Ling Lin, Yun-Shien Lee, Cheng-Hsun Chiu, Ta-Jen Lee, and Chien-Chia Huang. 2022. "Predictors of Surgical Intervention for Pediatric Acute Rhinosinusitis with Periorbital Infection" Journal of Clinical Medicine 11, no. 13: 3831. https://doi.org/10.3390/jcm11133831
APA StyleWu, P.-W., Lin, Y.-L., Lee, Y.-S., Chiu, C.-H., Lee, T.-J., & Huang, C.-C. (2022). Predictors of Surgical Intervention for Pediatric Acute Rhinosinusitis with Periorbital Infection. Journal of Clinical Medicine, 11(13), 3831. https://doi.org/10.3390/jcm11133831









