The Role of Humeral Neck-Shaft Angle in Reverse Total Shoulder Arthroplasty: 155° versus <155°—A Systematic Review
Abstract
:1. Introduction
2. Materials and Methods
2.1. Eligibility Criteria
2.2. Inclusion Criteria
2.3. Exclusion Criteria
2.4. Search
2.5. Data Collection Process
2.6. Data Items
| Author and Year | Type of Study and Loe | Tot. Sample Size | Sample Size Groups (n) | Shoulders | Tot. Mean Age | Mean Age Groups | Gender | |
|---|---|---|---|---|---|---|---|---|
| M | F | |||||||
| Beltrame et al., 2019 [35] | Prospective study, IV | 42 | 145° (21) 155° (21) | 42 | 145° = 77 155° = 75 | 12 | 30 | |
| Boutsiadis et al., 2018 [36] | Prognostic study, II | 46 | 155 (I) (13) 155 (III) (11) 145 (II) (10) 145 (IV) (12) | 46 | 77 ± 7.5 (62–90) | 9 | 37 | |
| Edwards et al., 2012 [37] | Randomized control trial, treatment study, I | 42 | 155 (T) (20) 155 (NT) (22) | 42 | 69 | T = 71.8 ± 8.0 NT = 66.3 ± 9.8 | 19 | 23 |
| Franceschetti et al., 2019 [27] | Retrospective cohort study, III | 57 | 145 (29) 145 (BIO-RSA) (30) | 59 | 69.9 ± 8.8 | BIORSA = 69.7 ± 9.9 RSA = 70.2 ± 7.8 | 22 | 35 |
| Gobezie et al., 2018 [38] | Randomized control trial, I | 68 | 155 (31) 135 (37) | 73 (43–94) | 155 = 73 135 = 71 | 155 = 9 135 = 14 | 155 = 22 135 = 23 | |
| Katz et al., 2015 [39] | Retrospective case series study, IV | 134 | 155 (140) | 140 | 72 (52–90) | 34 | 100 | |
| Lindbloom et al., 2019 [40] | Retrospective cohort study, III | 221 | 135 (221) | 221 | 88 | 133 | ||
| Merolla et al., 2017 [41] | Retrospective cohort study, III | 68 | 155 (36) 145 (38) | 74 | 155 = 75.8 (55–88) 145 = 74.7 (55–91) | 155 = 10 145 = 13 | 155 = 26 145 = 25 | |
| Moroder et al., 2016 [26] | Case-control study, III | 24 | m134 (24) | 24 | 75.6 ± 4.6 | 7 | 17 | |
| Rhee et al., 2018 [25] | Case-series, IV | 138 | 155 (146) | 146 | 71 ± 5.7 | 26 | 112 | |
| Streit et al., 2015 [42] | Retrospective case-control study, III | 28 (10CG) | 155 (9) 135 (9) | 28 | 70.6 | 155 = 70.9 135 = 70.4 | 155 = 3 135 = 2 | 155 = 6 135 = 4 |
| Author and Year | Surgical Approach | Prosthesis Design | Surgical Characteristics | Follow Up (Months) | ||||
|---|---|---|---|---|---|---|---|---|
| NSA (°) | Glenosphere Size (mm) | Glenoid Tilt | Mean | Max | Min | |||
| Beltrame et al., 2019 [35] | Deltopectoral | SMR, Ascend Flex | 155, 145 | 12 | ||||
| Boutsiadis et al., 2018 [36] | Deltopectoral | Aequalis, Ascend Flex | 155, 145 | 36, 32 | Inferior | 39 ± 18 | 84 | 24 |
| Edwards et al., 2012 [37] | Deltopectoral | Aequalis | 155 | 36 | Inferior | 21 | 12 | |
| Franceschetti et al., 2019 [27] | Deltopectoral | Aequalis II, Ascend Flex | 145 | 24 | ||||
| Gobezie et al., 2018 [38] | Deltopectoral | Universe Reverse | 155, 135 | 36, 39, 42 | Neutral | 38 | 45 | 29 |
| Katz et al., 2015 [39] | Superior (82.1%), deltopectoral (17.8%) | Arrow | 155 | 36 (83%) | Slightly inferior | 45 | 120 | 24 |
| Lindbloom et al., 2019 [40] | Deltopectoral | RSP, RSP Monoblock, AltiVate | 135 | |||||
| Merolla et al., 2017 [41] | Deltopectoral | Aequalis II, Ascend Flex | 155, 145 | 36, 42 | Centered, inferior | 155 = 35.1 145 = 29.1 | 24 | |
| Moroder et al., 2016 [26] | Deltopectoral | TESS | 134.4 (116–152) | 35 | 75 | 24 | ||
| Rhee et al., 2018 [25] | Deltopectoral | Trabecular metal, Aequalis Biomet comprehensive, Reverse System | 155 | 36 | Inferior | 20.6 | 64 | 12 |
| Streit et al., 2015 [42] | Deltopectoral | Aequalis, Encore | 155, 135 | 36 | 155 = 9.6 135 = 6.6 | |||
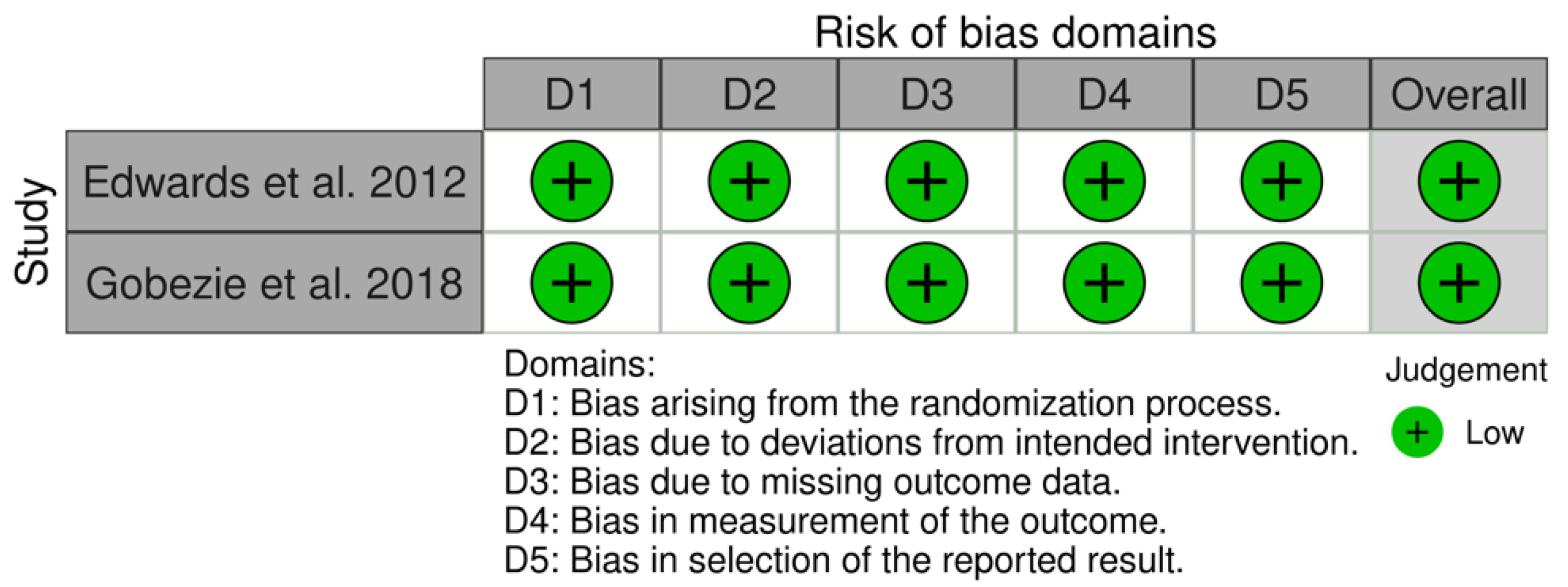
2.7. Study Risk of Bias Assessment
3. Results
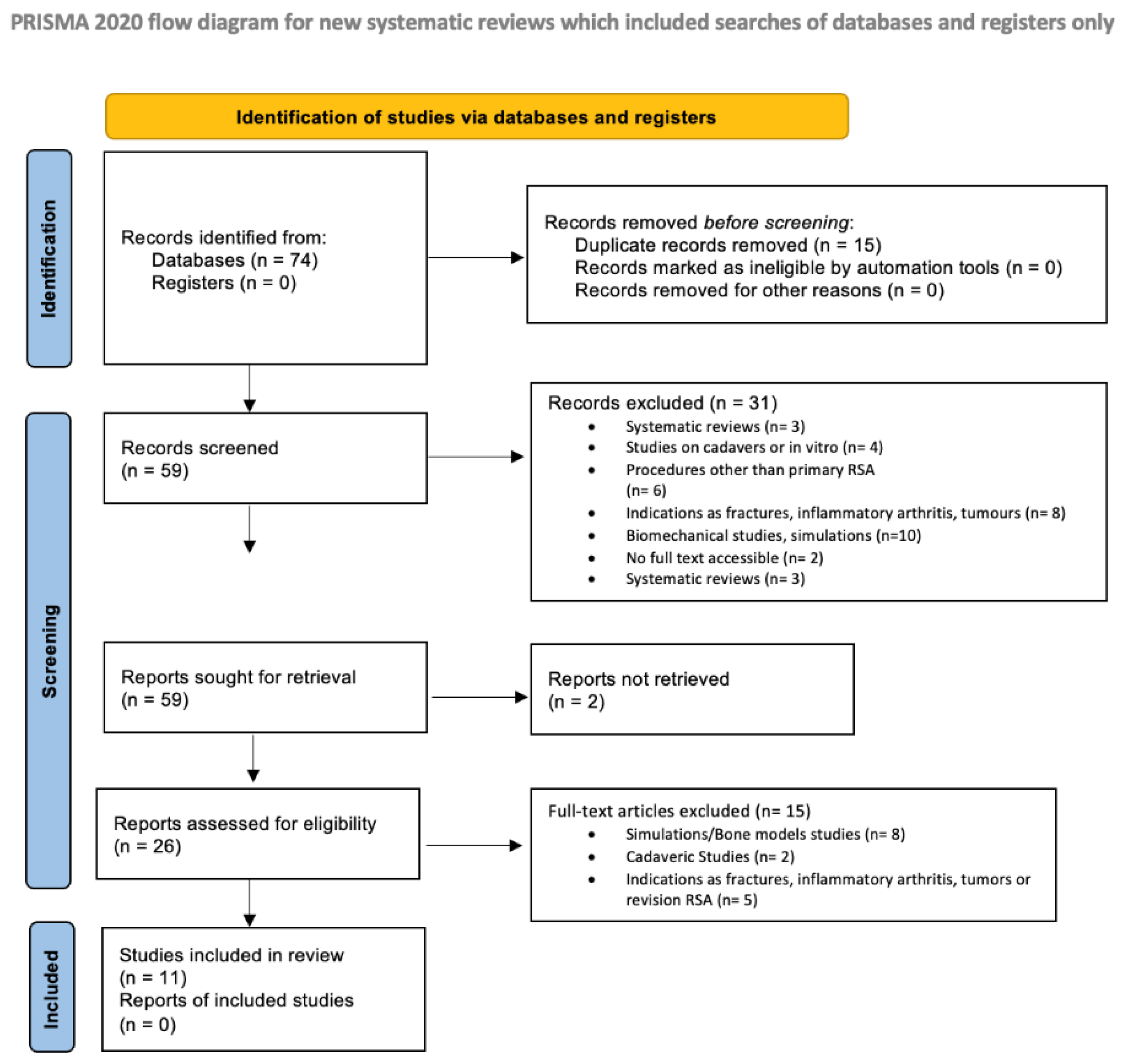
3.1. Study Selection
3.2. Study Characteristics
3.3. Quality of Evidence
3.4. Surgical Procedure
3.5. Outcome Score
3.6. Complications and Revisions
3.7. Scapular Notching
3.8. Active ROMs
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Tashjian, R.Z. Epidemiology, natural history, and indications for treatment of rotator cuff tears. Clin. Sports Med. 2012, 31, 589–604. [Google Scholar] [CrossRef] [PubMed]
- Chakravarty, K.; Webley, M. Shoulder joint movement and its relationship to disability in the elderly. J. Rheumatol. 1993, 20, 1359–1361. [Google Scholar]
- Ecklund, K.J.; Lee, T.Q.; Tibone, J.; Gupta, R. Rotator cuff tear arthropathy. J. Am. Acad. Orthop. Surg. 2007, 15, 340–349. [Google Scholar] [CrossRef]
- Jensen, K.L.; Williams, G.R.; Russell, I.J.; Rockwood, C.A. Rotator cuff tear arthropathy. J. Bone Jt. Surg. 1999, 81, 1312–1324. [Google Scholar] [CrossRef]
- Longo, U.G.; Berton, A.; Khan, W.S.; Maffulli, N.; Denaro, V. Histopathology of rotator cuff tears. Sports Med. Arthrosc. Rev. 2011, 19, 227–236. [Google Scholar] [CrossRef]
- Longo, U.G.; Rizzello, G.; Loppini, M.; Locher, J.; Buchmann, S.; Maffulli, N.; Denaro, V. Multidirectional Instability of the Shoulder: A Systematic Review. Arthroscopy 2015, 31, 2431–2443. [Google Scholar] [CrossRef]
- Petrillo, S.; Longo, U.G.; Papalia, R.; Denaro, V. Reverse shoulder arthroplasty for massive irreparable rotator cuff tears and cuff tear arthropathy: A systematic review. Musculoskelet. Surg. 2017, 101, 105–112. [Google Scholar] [CrossRef]
- Ackland, D.C.; Pak, P.; Richardson, M.; Pandy, M.G. Moment arms of the muscles crossing the anatomical shoulder. J. Anat. 2008, 213, 383–390. [Google Scholar] [CrossRef]
- Boileau, P.; Watkinson, D.; Hatzidakis, A.M.; Hovorka, I. Neer Award 2005: The Grammont reverse shoulder prosthesis: Results in cuff tear arthritis, fracture sequelae, and revision arthroplasty. J. Shoulder Elb. Surg. 2006, 15, 527–540. [Google Scholar] [CrossRef]
- Kontaxis, A.; Johnson, G.R. The biomechanics of reverse anatomy shoulder replacement-A modelling study. Clin. Biomech. 2009, 24, 254–260. [Google Scholar] [CrossRef]
- Mohammed, A.A.; Frostick, S.P. Linked shoulder replacement: Current design problems and a new design proposal. Musculoskelet. Surg. 2016, 100, 25–29. [Google Scholar] [CrossRef] [PubMed]
- Nalbone, L.; Adelfio, R.; D’Arienzo, M.; Ingrassia, T.; Nigrelli, V.; Zabbara, F.; Paladini, P.; Campi, F.; Pellegrini, A.; Porcellini, G. Optimal positioning of the humeral component in the reverse shoulder prosthesis. Musculoskelet. Surg. 2014, 98, 135–142. [Google Scholar] [CrossRef] [PubMed]
- Randelli, P.; Randelli, F.; Arrigoni, P.; Ragone, V.; D’Ambrosi, R.; Masuzzo, P.; Cabitza, P.; Banfi, G. Optimal glenoid component inclination in reverse shoulder arthroplasty. How to improve implant stability. Musculoskelet. Surg. 2014, 98 (Suppl. S1), 15–18. [Google Scholar] [CrossRef]
- Longo, U.G.; Loppini, M.; Rizzello, G.; Ciuffreda, M.; Berton, A.; Maffulli, N.; Denaro, V. Remplissage, humeral osteochondral grafts, weber osteotomy, and shoulder arthroplasty for the management of humeral bone defects in shoulder instability: Systematic review and quantitative synthesis of the literature. Arthroscopy 2014, 30, 1650–1666. [Google Scholar] [CrossRef] [PubMed]
- Baulot, E.; Sirveaux, F.; Boileau, P. Grammont’s idea: The story of Paul Grammont’s functional surgery concept and the development of the reverse principle. Clin. Orthop. Relat. Res. 2011, 469, 2425–2431. [Google Scholar] [CrossRef] [Green Version]
- Berliner, J.L.; Regalado-Magdos, A.; Ma, C.B.; Feeley, B.T. Biomechanics of reverse total shoulder arthroplasty. J. Shoulder Elb. Surg. 2015, 24, 150–160. [Google Scholar] [CrossRef]
- Smithers, C.J.; Young, A.A.; Walch, G. Reverse shoulder arthroplasty. Curr. Rev. Musculoskelet. Med. 2011, 4, 183–190. [Google Scholar] [CrossRef] [Green Version]
- Teissier, P.; Teissier, J.; Kouyoumdjian, P.; Asencio, G. The TESS reverse shoulder arthroplasty without a stem in the treatment of cuff-deficient shoulder conditions: Clinical and radiographic results. J. Shoulder Elb. Surg. 2015, 24, 45–51. [Google Scholar] [CrossRef]
- Alessandra, B. Delayed Rehabilitation Protocol after Rotator Cuff Repair. Osteology 2021, 1, 29–38. [Google Scholar] [CrossRef]
- Boileau, P.; Watkinson, D.J.; Hatzidakis, A.M.; Balg, F. Grammont reverse prosthesis: Design, rationale, and biomechanics. J. Shoulder Elb. Surg. 2005, 14, 147S–161S. [Google Scholar] [CrossRef]
- Wall, B.; Nové-Josserand, L.; O’Connor, D.P.; Edwards, T.B.; Walch, G. Reverse total shoulder arthroplasty: A review of results according to etiology. J. Bone Jt. Surg. 2007, 89, 1476–1485. [Google Scholar] [CrossRef]
- Zumstein, M.A.; Pinedo, M.; Old, J.; Boileau, P. Problems, complications, reoperations, and revisions in reverse total shoulder arthroplasty: A systematic review. J. Shoulder Elb. Surg. 2011, 20, 146–157. [Google Scholar] [CrossRef] [PubMed]
- Guery, J.; Favard, L.; Sirveaux, F.; Oudet, D.; Mole, D.; Walch, G. Reverse total shoulder arthroplasty. Survivorship analysis of eighty replacements followed for five to ten years. J. Bone Jt. Surg. 2006, 88, 1742–1747. [Google Scholar] [CrossRef]
- Gerber, C.; Canonica, S.; Catanzaro, S.; Ernstbrunner, L. Longitudinal observational study of reverse total shoulder arthroplasty for irreparable rotator cuff dysfunction: Results after 15 years. J. Shoulder Elb. Surg. 2018, 27, 831–838. [Google Scholar] [CrossRef] [PubMed]
- Rhee, S.M.; Lee, J.D.; Park, Y.B.; Yoo, J.C.; Oh, J.H. Prognostic Radiological Factors Affecting Clinical Outcomes of Reverse Shoulder Arthroplasty in the Korean Population. Clin. Orthop. Surg. 2019, 11, 112–119. [Google Scholar] [CrossRef]
- Moroder, P.; Ernstbrunner, L.; Zweiger, C.; Schatz, M.; Seitlinger, G.; Skursky, R.; Becker, J.; Resch, H.; Krifter, R.M. Short to mid-term results of stemless reverse shoulder arthroplasty in a selected patient population compared to a matched control group with stem. Int. Orthop. 2016, 40, 2115–2120. [Google Scholar] [CrossRef] [Green Version]
- Franceschetti, E.; Ranieri, R.; Giovanetti de Sanctis, E.; Palumbo, A.; Franceschi, F. Clinical results of bony increased-offset reverse shoulder arthroplasty (BIO-RSA) associated with an onlay 145° curved stem in patients with cuff tear arthropathy: A comparative study. J. Shoulder Elb. Surg. 2020, 29, 58–67. [Google Scholar] [CrossRef] [Green Version]
- Pearl, M.L. Proximal humeral anatomy in shoulder arthroplasty: Implications for prosthetic design and surgical technique. J. Shoulder Elb. Surg. 2005, 14, 99S–104S. [Google Scholar] [CrossRef]
- Goldberg, R.W.; Williamson, D.F.; Hoyen, H.A.; Liu, R.W. Humeral version and neck-shaft angle correlated with demographic parameters in a study of 1104 cadaveric humeri. J. Shoulder Elb. Surg. 2020, 29, 1236–1241. [Google Scholar] [CrossRef]
- Robertson, D.D.; Yuan, J.; Bigliani, L.U.; Flatow, E.L.; Yamaguchi, K. Three-dimensional analysis of the proximal part of the humerus: Relevance to arthroplasty. J. Bone Jt. Surg. 2000, 82, 1594–1602. [Google Scholar] [CrossRef]
- Merolla, G.; Walch, G.; Ascione, F.; Paladini, P.; Fabbri, E.; Padolino, A.; Porcellini, G. Grammont humeral design versus onlay curved-stem reverse shoulder arthroplasty: Comparison of clinical and radiographic outcomes with minimum 2-year follow-up. J. Shoulder Elb. Surg. 2018, 27, 701–710. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; Group, P. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [Green Version]
- Sirveaux, F.; Favard, L.; Oudet, D.; Huquet, D.; Walch, G.; Molé, D. Grammont inverted total shoulder arthroplasty in the treatment of glenohumeral osteoarthritis with massive rupture of the cuff. Results of a multicentre study of 80 shoulders. J. Bone Jt. Surg. Br. 2004, 86, 388–395. [Google Scholar] [CrossRef] [PubMed]
- Beltrame, A.; Di Benedetto, P.; Cicuto, C.; Cainero, V.; Chisoni, R.; Causero, A. Onlay versus Inlay humeral steam in Reverse Shoulder Arthroplasty (RSA): Clinical and biomechanical study. Acta Biomed. 2019, 90, 54–63. [Google Scholar] [CrossRef]
- Boutsiadis, A.; Lenoir, H.; Denard, P.J.; Panisset, J.C.; Brossard, P.; Delsol, P.; Guichard, F.; Barth, J. The lateralization and distalization shoulder angles are important determinants of clinical outcomes in reverse shoulder arthroplasty. J. Shoulder Elb. Surg. 2018, 27, 1226–1234. [Google Scholar] [CrossRef]
- Edwards, T.B.; Trappey, G.J.; Riley, C.; O’Connor, D.P.; Elkousy, H.A.; Gartsman, G.M. Inferior tilt of the glenoid component does not decrease scapular notching in reverse shoulder arthroplasty: Results of a prospective randomized study. J. Shoulder Elb. Surg. 2012, 21, 641–646. [Google Scholar] [CrossRef]
- Gobezie, R.; Shishani, Y.; Lederman, E.; Denard, P.J. Can a functional difference be detected in reverse arthroplasty with 135° versus 155° prosthesis for the treatment of rotator cuff arthropathy: A prospective randomized study. J. Shoulder Elb. Surg. 2019, 28, 813–818. [Google Scholar] [CrossRef]
- Katz, D.; Valenti, P.; Kany, J.; Elkholti, K.; Werthel, J.D. Does lateralisation of the centre of rotation in reverse shoulder arthroplasty avoid scapular notching? Clinical and radiological review of one hundred and forty cases with forty five months of follow-up. Int. Orthop. 2016, 40, 99–108. [Google Scholar] [CrossRef] [Green Version]
- Lindbloom, B.J.; Christmas, K.N.; Downes, K.; Simon, P.; McLendon, P.B.; Hess, A.V.; Mighell, M.A.; Frankle, M.A. Is there a relationship between preoperative diagnosis and clinical outcomes in reverse shoulder arthroplasty? An experience in 699 shoulders. J. Shoulder Elb. Surg. 2019, 28, S110–S117. [Google Scholar] [CrossRef]
- Merolla, G.; Cerciello, S.; Marenco, S.; Fabbri, E.; Paladini, P.; Porcellini, G. Comparison of shoulder replacement to treat osteoarthritis secondary to instability surgery and primary osteoarthritis: A retrospective controlled study of patient outcomes. Int Orthop 2018, 42, 2147–2157. [Google Scholar] [CrossRef] [PubMed]
- Streit, J.J.; Shishani, Y.; Gobezie, R. Medialized Versus Lateralized Center of Rotation in Reverse Shoulder Arthroplasty. Orthopedics 2015, 38, e1098–e1103. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, J.H.; Chun, Y.M.; Kim, D.S.; Lee, D.H.; Shin, S.J. Early restoration of shoulder function in patients with the Grammont prosthesis compared to lateralized humeral design in reverse shoulder arthroplasty. J. Shoulder Elb. Surg. 2021, 30, 2533–2542. [Google Scholar] [CrossRef]
- Sterne, J.A.C.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ 2019, 366, l4898. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sterne, J.A.; Hernán, M.A.; Reeves, B.C.; Savović, J.; Berkman, N.D.; Viswanathan, M.; Henry, D.; Altman, D.G.; Ansari, M.T.; Boutron, I.; et al. ROBINS-I: A tool for assessing risk of bias in non-randomised studies of interventions. BMJ 2016, 355, i4919. [Google Scholar] [CrossRef] [Green Version]
- Sandeep, M. Chapter 7: Systematic reviews of etiology and risk. In Joanna Briggs Institute Reviewer’s Manual; Aromataris, E., Munn, Z., Eds.; The Joanna Briggs Institute: Adelaide, Australia, 2017; Available online: https://reviewersmanual.joannabriggs.org/ (accessed on 20 April 2022).
- Moroder, P.; Stefanitsch, V.; Auffarth, A.; Matis, N.; Resch, H.; Plachel, F. Treatment of recurrent anterior shoulder instability with the Latarjet or Bristow procedure in older patients. J. Shoulder Elb. Surg. 2018, 27, 824–830. [Google Scholar] [CrossRef]
- Moroder, P.; Schulz, E.; Mitterer, M.; Plachel, F.; Resch, H.; Lederer, S. Long-Term Outcome After Pectoralis Major Transfer for Irreparable Anterosuperior Rotator Cuff Tears. J. Bone Jt. Surg Am. 2017, 99, 239–245. [Google Scholar] [CrossRef]
- Locher, J.; Wilken, F.; Beitzel, K.; Buchmann, S.; Longo, U.G.; Denaro, V.; Imhoff, A.B. Hill-Sachs Off-track Lesions as Risk Factor for Recurrence of Instability After Arthroscopic Bankart Repair. Arthroscopy 2016, 32, 1993–1999. [Google Scholar] [CrossRef]
- Ferle, M.; Pastor, M.F.; Hagenah, J.; Hurschler, C.; Smith, T. Effect of the humeral neck-shaft angle and glenosphere lateralization on stability of reverse shoulder arthroplasty: A cadaveric study. J. Shoulder Elb. Surg. 2019, 28, 966–973. [Google Scholar] [CrossRef]
- Longo, U.G.; De Salvatore, S.; Zompanti, A.; Di Naro, C.; Grasso, S.; Casciaro, C.; Sabatini, A.; Mazzola, A.; Pennazza, G.; Santonico, M.; et al. Biosensors for Detection and Monitoring of Joint Infections. Chemosensors 2021, 9, 256. [Google Scholar] [CrossRef]
- Longo, U.G.; Candela, V.; De Salvatore, S.; Piergentili, I.; Panattoni, N.; Casciani, E.; Faldetta, A.; Marchetti, A.; De Marinis, M.G.; Denaro, V. Arthroscopic Rotator Cuff Repair Improves Sleep Disturbance and Quality of Life: A Prospective Study. Int. J. Environ. Res. Public Health 2021, 18, 3797. [Google Scholar] [CrossRef] [PubMed]
- Oh, J.H.; Shin, S.J.; McGarry, M.H.; Scott, J.H.; Heckmann, N.; Lee, T.Q. Biomechanical effects of humeral neck-shaft angle and subscapularis integrity in reverse total shoulder arthroplasty. J. Shoulder Elb. Surg. 2014, 23, 1091–1098. [Google Scholar] [CrossRef] [PubMed]
- Panattoni, N.; Longo, U.G.; De Salvatore, S.; Castaneda, N.S.C.; Risi Ambrogioni, L.; Piredda, M.; De Marinis, M.G.; Denaro, V. The influence of psychosocial factors on patient-reported outcome measures in rotator cuff tears pre- and post-surgery: A systematic review. Qual. Life Res. 2021, 31, 91–116. [Google Scholar] [CrossRef] [PubMed]
- Longo, U.G.; Berton, A.; De Salvatore, S.; Piergentili, I.; Casciani, E.; Faldetta, A.; De Marinis, M.G.; Denaro, V. Minimal Clinically Important Difference and Patient Acceptable Symptom State for the Pittsburgh Sleep Quality Index in Patients Who Underwent Rotator Cuff Tear Repair. Int. J. Environ. Res. Public Health 2021, 18, 8666. [Google Scholar] [CrossRef] [PubMed]
- Berton, A.; Longo, U.G.; De Salvatore, S.; Sciotti, G.; Santamaria, G.; Piergentili, I.; De Marinis, M.G.; Denaro, V. A Historical Analysis of Randomized Controlled Trials in the Management of Pain in Rotator Cuff Tears. J. Clin. Med. 2021, 10, 4072. [Google Scholar] [CrossRef] [PubMed]
- Lädermann, A.; Denard, P.J.; Boileau, P.; Farron, A.; Deransart, P.; Terrier, A.; Ston, J.; Walch, G. Effect of humeral stem design on humeral position and range of motion in reverse shoulder arthroplasty. Int. Orthop. 2015, 39, 2205–2213. [Google Scholar] [CrossRef] [Green Version]
- Hill, K.G.; Woodward, D.; Woelfel, T.; Hawkins, J.D.; Green, S. Planning for Long-Term Follow-Up: Strategies Learned from Longitudinal Studies. Prev. Sci. 2016, 17, 806–818. [Google Scholar] [CrossRef] [Green Version]
| Author and Year | Nsa (°) (n) | Constant–Murley Score | Absolute ASES Score | SST | |||
|---|---|---|---|---|---|---|---|
| Pre | Post | Pre | Post | Pre | Post | ||
| Beltrame et al., 2019 [35] | 155 (21) | 41 | 70 | ||||
| 145 (21) | 39 | 71 | |||||
| Boutsiadis et al., 2018 [36] | 155 (I) (13) | 23 ± 3 (12–45) | 62 ± 3 (45–71) | 75 ± 4 (53–98) | 7 ± 0.5 (4–11) | ||
| 155 (III) (11) | 19 ± 3.5 (2–33) | 65 ± 2 (53–77) | 77 ± 4 (57–98) | 7 ± 0.8 (3–11) | |||
| 145 (II) (10) | 21 ± 2.5 (8–30) | 67 ± 4 (41–86) | 79 ± 5 (53–100) | 7 ± 1 (2–12) | |||
| 145 (IV) (12) | 26 ± 1 (16–34) | 62 ± 5 (34–87) | 72 ± 8 (33–100) | 7 ± 1 (1–11) | |||
| Edwards et al., 2012 [37] | 155 (T) (20) | 13.1 ± 9.2 | 63.6 ± 12.3 | ||||
| 155 (NT) (22) | 15.7 ± 10.8 | 71.4 ± 14.9 | |||||
| Franceschetti et al., 2019 [27] | 145 (29) | 32.7 ± 18.9 | 80.1 ± 16.7 | ||||
| 145 (BIO–RSA) (30) | 29.4 ± 16.4 | 77.1 ± 20.9 | |||||
| Gobezie et al., 2018 [38] | 155 (31) | 37 ± 18.8 | 78 ± 15.1 | 3 ± 2.7 | 7 ± 2.2 | ||
| 135 (37) | 37 ± 22.6 | 74 ± 24.6 | 3 ± 2.8 | 8 ± 3.0 | |||
| Katz et al., 2015 [39] | 155 (140) | 26 (11–53) | 64 (26–85) | 8.66 | |||
| Lindbloom et al., 2019 [40] | M = 135 (88) | 43 (38–47) | 76 (71–81) | 3 (2–3) | 7 (6–7) | ||
| F = 135 (133) | 36 (33–40) | 68 (64–72) | 2 (1–2) | 5 (5–6) | |||
| Merolla et al., 2017 [41] | 155 (36) | 17.9 | 69.6 | ||||
| 145 (38) | 27 | 71.2 | |||||
| Moroder et al., 2016 [26] | m134.4 (24) | 65.4 ± 12.9 | 76.2 ± 10.8 | ||||
| Rhee et al., 2018 [25] | 155 (146) | 26 (0–73) | 53.9 (23–90) | 35.9 (7–72) | 67.3 (22–93) | 2.6 (0–7) | 5.9 (1–10) |
| Streit et al., 2015 [42] | 155 (I) (9) | 75.1 | |||||
| 135 (II) (9) | 71 | ||||||
| Author and Year | Nsa (°) (N) | Complications (N) | Revisions |
|---|---|---|---|
| Beltrame et al., 2019 [35] | 155 (21) | / | / |
| 145 (21) | / | / | |
| Boutsiadis et al., 2018 [36] | 155 (I) (13) | / | / |
| 155 (III) (11) | / | / | |
| 145 (II) (10) | / | / | |
| 145 (IV) (12) | / | / | |
| Edwards et al., 2012 [37] | 155 (T) (20) | / | |
| 155 (NT) (22) | (1) dislocation | / | |
| Franceschetti et al., 2019 [27] | 145 (29) | 0 | / |
| 145 (BIO-RSA) (30) | (1) instability | / | |
| Gobezie et al., 2018 [38] | 155 (31) | (3) fractures (1) loosening | 4 |
| 135 (37) | (2) fractures (3) loosening | 2 | |
| Katz et al., 2015 [39] | 155 (140) | (4) brachial plexus palsy (1) traumatic fracture of greater tuberosity (1) acromial fracture (6) dissociation of humeral bearing (2) wear of humeral bearing (3) loosening of uncemented humeral (4) glenoid loosening (3) infection (3) stiffness | 12 (8.9%) |
| Lindbloom et al., 2019 [40] | M =135 (88) | (1) glenosphere dissociation (1) instability | 2 (0.9%) |
| F =135 (133) | |||
| Merolla et al., 2017 [41] | 155 (36) | (2) dislocation | 0 |
| 145 (36) | (2) scapular spine fracture (1) acromial fracture (3) infection (1) instability | 2 | |
| Moroder et al., 2016 [26] | 134.4 (24) | (1) dislocation (1) acromial spine fracture (1) symptomatic mesacromion (3) stiffness (2) hematomas (1) transient paresthesia (1) inlay snapping | 3 |
| Rhee et al., 2018 [25] | 155 (146) | (3) infection (7) neurologic complications | / |
| Streit et al., 2015 [42] | 155 (I) (9) | / | / |
| 135 (II) (9) | / | / |
| Author and Year | Nsa° (n) | Scapular Notching | Grades of Notching (% or n) | ||||
|---|---|---|---|---|---|---|---|
| N | % | Grade I | Grade II | Grade III | Grade IV | ||
| Beltrame et al., 2019 [35] | 155 (21) | 3 | 24 | 3 | 0 | 0 | 0 |
| 145 (21) | |||||||
| Boutsiadis et al., 2018 [36] | I 155 (13) | ||||||
| III 155 (11) | |||||||
| II 145 (10) | |||||||
| IV 145 (12) | |||||||
| Edwards et al., 2012 [37] | T 155 (20) | 15 | 5 | 8 | 2 | ||
| NT 155 (22) | 19 | 8 | 10 | 1 | |||
| Franceschetti et al., 2019 [27] | 145 (BIO-RSA) (30) | 4 | 13.3 | 4 | |||
| 145 (29) | 5 | 17.2 | 4 | 1 | |||
| Gobezie et al., 2018 [38] | 155 (31) | 18 | 58 | 5 | 10 | 1 | 2 |
| 135 (37) | 8 | 21 | 3 | 3 | 1 | 1 | |
| Katz et al., 2015 [39] | 155 (140) | 41 | 29 | 20 | 18 | 3 | 0 |
| Lindbloom et al., 2019 [40] | M = 135 (88) | ||||||
| F = 135 (133) | |||||||
| Merolla et al., 2017 [41] | 155 (36) | 14 | 39.0 | 11 | 1 | 0 | 0 |
| 145 (38) | 2 | 5 | 2 | 0 | 0 | 0 | |
| Moroder et al., 2016 [26] | m134.4 (24) | 2 | |||||
| Rhee et al., 2018 [25] | 155 (146) | 44 | 30 | 37 | 7 | ||
| Streit et al., 2015 [42] | 155 (9) | ||||||
| 135 (9) | |||||||
| Author and Year | Nsa° (n) | ROM | |||||
|---|---|---|---|---|---|---|---|
| Forward Flexion | Abduction | External Rotation Arm at the Side (°) | |||||
| Pre | Post | Pre | Post | Pre | Post | ||
| Beltrame et al., 2019 [35] | 155 (21) | 153 | 142 | −42 | |||
| 145 (21) | 158 | 144 | −37 | ||||
| Boutsiadis et al., 2018 [36] | I 155 (13) | 63 ± 21 (10–100) | 148 ± 7 (100–170) | 134 ± 8.5 (90–170) | 14 ± 20 (−30–50) | 14 ± 13 (−10–35) | |
| III 155 (11) | 74 ± 35 (10–120) | 158 ± 4 (130–175) | 145 ± 7 (100–170) | 5 ± 20 (−30–40) | 24 ± 12 (0–40) | ||
| II 145 (10) | 53 ± 22 (30–90) | 149 ± 8 (90–175) | 134 ± 9 (80–175) | 8 ± 21 (−30–20) | 31 ± 13 (15–60) | ||
| IV 145 (12) | 80 ± 35 (0–120) | 152 ± 8 (80–180) | 129 ± 11 (80–170) | 14 ± 20 (−30–40) | 30 ± 16 (0–50) | ||
| Edwards et al., 2012 [37] | T (20) | 51.6 ± 49.1 | 156.6 ± 21.2 | 49.8 ± 49 | 155.9 ± 21.0 | 0.7 ± 1.8 | 8.3 ± 2.6 |
| NT (22) | 36.0 ± 45.6 | 148.0 ± 19.4 | 32.3 ± 37.4 | 141.8 ± 27.3 | 0.3 ± 1.3 | 7.4 ± 1.8 | |
| Franceschetti et al., 2019 [27] | 145 (BIO-RSA) (30) | 78 ± 31 | 136 ± 21 | 67 ± 28 | 118 ± 19 | 15 ± 11 | 32 ± 20 |
| 145 (29) | 81 ± 29 | 135 ± 25 | 65 ± 29 | 119 ± 26 | 16 ± 11 | 40 ± 18 | |
| Gobezie et al., 2018 [38] | 155 (31) | 76 ± 50 | 135 ± 17 | 29 ± 15 | 30 ± 14 | ||
| 135 (37) | 78 ± 47 | 132 ± 19 | 28 ± 14 | 29 ± 10 | |||
| Katz et al., 2015 [39] | 155 (140) | 73 | 132 | 61 | 108 | 20 | 29 |
| Lee et al., 2021 [43] | 155 (43) | 130 ± 16 | 127 ± 14 | 48 ± 14 | |||
| 145 (71) | 132 ± 16 | 125 ± 16 | 48 ± 12 | ||||
| Lindbloom et al., 2019 [40] | M =135 (88) | 81 (72–90) | 151 (142–159) | 75 (68–82) | 136 (126–146) | 32 (24–39) | 55 (46–64) |
| F =135 (133) | 70 (63–78) | 136 (128–144) | 66 (59–73) | 121 (113–130) | 26 (19–33) | 46 (38–54) | |
| Merolla et al., 2017 [41] | 155 (36) | 65 | 142 | 15 | 30 | ||
| 145 (38) | 83 | 142 | 0 | 32 | |||
| Moroder et al., 2016 [26] | m134.4 (24) | 7.8 ± 1.9 | 6.9 ± 2.0 | 6.6 ± 2.6 | |||
| Rhee et al., 2018 [25] | 155 (146) | 96.4 | 138.4 | 30.6 | 48.9 | ||
| Streit et al., 2015 [42] | 155 (9) | 143.9 | |||||
| 135 (9) | 115.6 | ||||||
| Teissier et al., 2015 [18] | m154 (91) | 96 | 143 | 89 | 138 | 47 | 68 |
| ACTIVE ROM (°) | SCAPULAR NOTCHING | ASES | CMS | SST | REVISIONS | COMPLICATIONS | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| FF | ABD | ER | DISLOCATIONS | FRACTURES | INFECTIONS | ||||||
| 155° | Pre: 77.4 ± 17.2 Post: 139.3 ± 8.3 | Pre: 56.3 ± 14.4 Post: 121.9 ± 18 | Pre: 21.4 ± 11.5 Post: 31.3 ± 29.1 | 154 (37%) | Pre: 36.1 ± 0.8 Post: 70.2 ± 4.7 | Pre: 24.6 ± 9.3 Post: 61.5 ± 6 | Pre: 2.7 ± 0.3 Post: 7.2 ± 1.1 | 16 (9.4%) | 3 (3.8%) | 7 (3.4%) | 6 (2.1%) |
| 145° | Pre: 78.3 ± 6.8 Post: 143 ± 9.8 | Pre: 66 ± 1.4 Post: 126.5 ± 12.2 | Pre: 14.4 ± 7.3 Post: 27.1 ± 31.8 | 11 (11.6%) | Pre: 31 ± 2.3 Post: 77.7 ± 2.5 | Pre: 29.3 ± 8.1 Post: 69.2 ± 3.9 | Pre: NA Post: 7 | 2 (5.6%) | 0 | 0 | 3 (8.3%) |
| 135° | Pre: 74.9 ± 2.6 Post: 128.8 ± 62 | Pre: 69.6 Post: 115.2 ± 84.9 | Pre: 28.3 ± 0.3 Post: 43.2 ± 21.5 | 8 (21.6%) | Pre: 38.5 ± 1.3 Post: 72 ± 2.5 | Pre: NA Post: 65.4 | Pre: 2.5 ± 0.4 Post: 6.1 ± 1.6 | 4 (1.6%) | 1 (4.2%) | 3 (4.9%) | 0 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Longo, U.G.; Gulotta, L.V.; De Salvatore, S.; Berton, A.; Piergentili, I.; Bandini, B.; Lalli, A.; Denaro, V. The Role of Humeral Neck-Shaft Angle in Reverse Total Shoulder Arthroplasty: 155° versus <155°—A Systematic Review. J. Clin. Med. 2022, 11, 3641. https://doi.org/10.3390/jcm11133641
Longo UG, Gulotta LV, De Salvatore S, Berton A, Piergentili I, Bandini B, Lalli A, Denaro V. The Role of Humeral Neck-Shaft Angle in Reverse Total Shoulder Arthroplasty: 155° versus <155°—A Systematic Review. Journal of Clinical Medicine. 2022; 11(13):3641. https://doi.org/10.3390/jcm11133641
Chicago/Turabian StyleLongo, Umile Giuseppe, Lawrence V. Gulotta, Sergio De Salvatore, Alessandra Berton, Ilaria Piergentili, Benedetta Bandini, Alberto Lalli, and Vincenzo Denaro. 2022. "The Role of Humeral Neck-Shaft Angle in Reverse Total Shoulder Arthroplasty: 155° versus <155°—A Systematic Review" Journal of Clinical Medicine 11, no. 13: 3641. https://doi.org/10.3390/jcm11133641
APA StyleLongo, U. G., Gulotta, L. V., De Salvatore, S., Berton, A., Piergentili, I., Bandini, B., Lalli, A., & Denaro, V. (2022). The Role of Humeral Neck-Shaft Angle in Reverse Total Shoulder Arthroplasty: 155° versus <155°—A Systematic Review. Journal of Clinical Medicine, 11(13), 3641. https://doi.org/10.3390/jcm11133641