Pediatric Infective Endocarditis: A Literature Review
Abstract
:1. Epidemiology
2. Predisposing Factors
2.1. Congenital Heart Disease
2.2. Acquired Risk Factors
2.3. No Known Risk Factors
3. Pathophysiology
- (1)
- Predisposing heart disease generating turbulent blood flow that produces endocardial damage that causes a thrombotic and fibrotic reaction;
- (2)
- Bloodstream bacterial or fungal infection (mainly from mucosal or skin source);
- (3)
- Foreign materials (catheters, heart conditions repaired with prosthetic material, cardiac implantable electronic devices) that facilitate the deposit of fibrin, platelets, and thrombus formation.
4. Clinical Presentation
5. Microbiology
6. Diagnosis
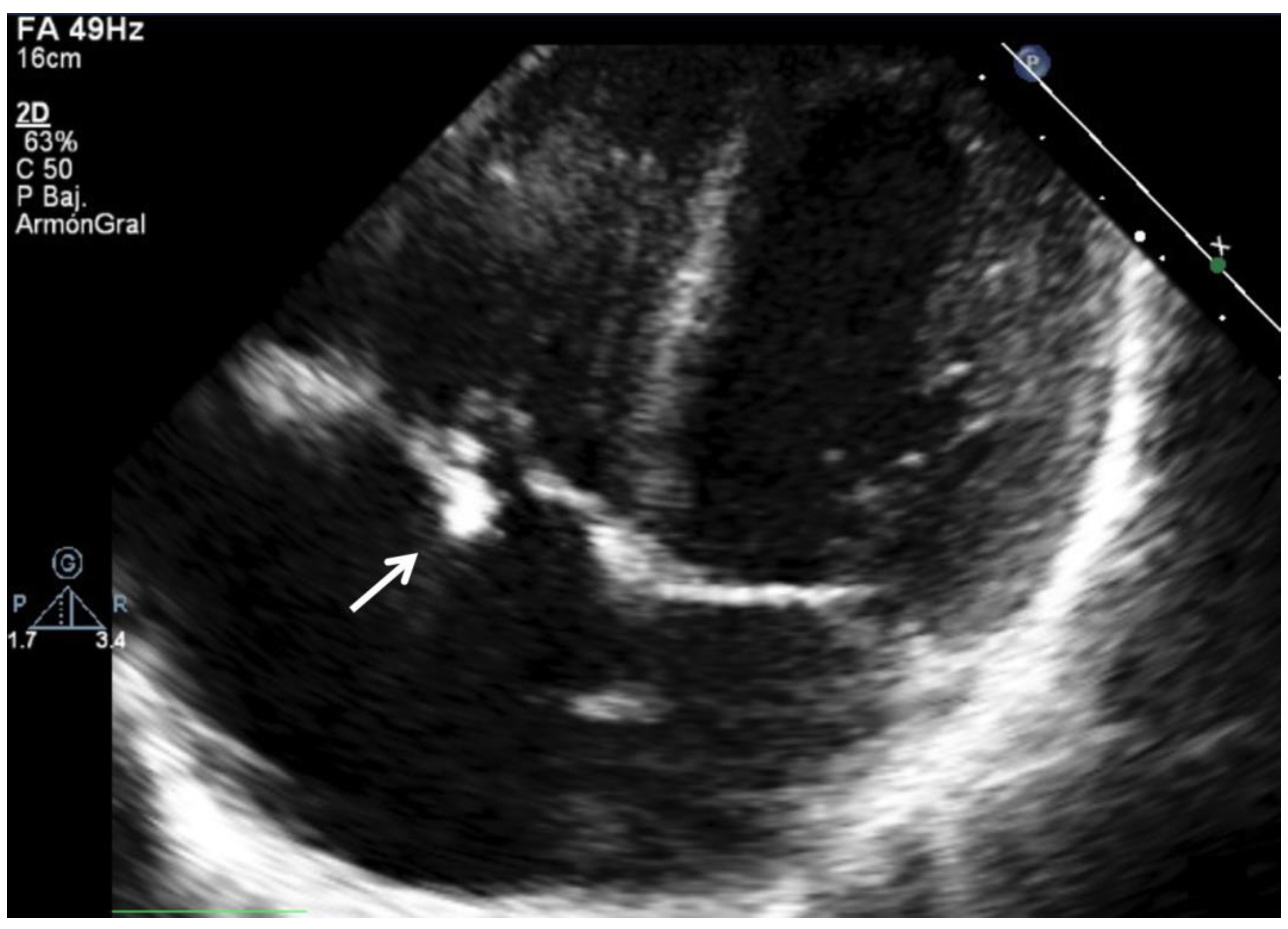
6.1. Echocardiography and Imaging Techniques in the Diagnosis of IE in Children
- (1)
- it requires frequently general anesthesia or sedatives;
- (2)
- a need to adapt the tube size, especially in younger children;
- (3)
- a possible vascular or airway compromise, especially with inappropriate probe sizes;
- (4)
- the interpretation of images may be complex and requires specific training.
6.2. Multimodality Cardiovascular Imaging
- exposure to ionizing radiation, which have a greater negative impact in children;
- interference with physiological activity (i.e., central nervous system, reactive intestinal ganglia, etc.);
- it requires preparation with a specific diet the days before the test;
- it requires differential diagnosis with other situations of tissue hypermetabolism, for example, after surgery or neoplasms. Therefore, the reliability of PET-CT for the diagnosis of IE in patients with recent cardiac surgery may be limited.
6.3. Blood Cultures
- Blood cultures should be taken as soon as possible, ideally < 1 h;
- Three sets of blood cultures should be drawn, in aerobic and anaerobic culture bottles. If a limited volume of blood is available, aerobic culture media should be preferred, as anaerobic IE is very rare;
- Usually, the incubation time necessary to observe bacterial growth and obtain antibiotic sensitivity is 24–48 h;
- If there is a high clinical suspicion of bacterial IE and negative blood cultures, it is important to consider molecular techniques to increase sensitivity, such as PCR, to detect bacterial DNA or the 16S subunit of bacterial ribosomes, which is species-specific. Bacterial identification by PCR also allows an earlier result to be obtained [63];
- It is of great importance to take blood cultures in the absence of antibiotic treatment, in those stable patients in whom the clinical situation allows the antibiotic to be discontinued;
- Consider repeating the cultures at 48–72 h in the presence of persistent or recurrent symptoms (fever, inflammatory parameters in laboratory tests, systemic inflammatory response).
7. Differential Diagnosis
8. Complications
9. Treatment
9.1. Antimicrobial Therapy
9.2. Surgery Timing and Indications
9.3. Other Therapeutic Considerations
10. Prognosis
11. Prophylaxis
12. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Gupta, S.; Sakhuja, A.; McGrath, E.; Asmar, B. Trends, Microbiology, and Outcomes of Infective Endocarditis in Children during 2000-2010 in the United States. Congenit. Heart Dis. 2017, 12, 196–201. [Google Scholar] [CrossRef] [PubMed]
- Mahony, M.; Lean, D.; Pham, L.; Horvath, R.; Suna, J.; Ward, C.; Veerappan, S.; Versluis, K.; Nourse, C. Infective Endocarditis in Children in Queensland, Australia: Epidemiology, Clinical Features and Outcome. Pediatr. Infect. Dis. J. 2021, 40, 617–622. [Google Scholar] [CrossRef] [PubMed]
- Cresti, A.; Chiavarelli, M.; Scalese, M.; Nencioni, C.; Valentini, S.; Guerrini, F.; D’Aiello, I.; Picchi, A.; De Sensi, F.; Habib, G. Epidemiological and Mortality Trends in Infective Endocarditis, a 17-Year Population-Based Prospective Study. Cardiovasc. Diagn. Ther. 2017, 7, 27–35. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ahmadi, A.; Daryushi, H. Infective Endocarditis in Children: A 5 Year Experience from Al-Zahra Hospital, Isfahan, Iran. Adv. Biomed. Res. 2014, 3, 228. [Google Scholar] [CrossRef]
- Jortveit, J.; Klcovansky, J.; Eskedal, L.; Birkeland, S.; Døhlen, G.; Holmstrøm, H. Endocarditis in Children and Adolescents with Congenital Heart Defects: A Norwegian Nationwide Register-Based Cohort Study. Arch. Dis. Child. 2018, 103, 670–674. [Google Scholar] [CrossRef] [Green Version]
- Ferrieri, P.; Gewitz, M.H.; Gerber, M.A.; Newburger, J.W.; Dajani, A.S.; Shulman, S.T.; Wilson, W.; Bolger, A.F.; Bayer, A.; Levison, M.E.; et al. Unique Features of Infective Endocarditis in Childhood. Circulation 2002, 105, 2115–2126. [Google Scholar] [CrossRef] [Green Version]
- Luca, A.-C.; Curpan, A.-S.; Adumitrachioaiei, H.; Ciobanu, I.; Dragomirescu, C.; Manea, R.-S.; Vlad, E.; Surguci-Copaceanu, A. Difficulties in Diagnosis and Therapy of Infective Endocarditis in Children and Adolescents-Cohort Study. Healthcare 2021, 9, 760. [Google Scholar] [CrossRef]
- Carceller, A.; Lebel, M.H.; Larose, G.; Boutin, C. New trends in pediatric endocarditis. An. Pediatr. 2005, 63, 396–402. [Google Scholar] [CrossRef]
- Fortún, J.; Centella, T.; Martín-Dávila, P.; Lamas, M.J.; Pérez-Caballero, C.; Fernández-Pineda, L.; Otheo, E.; Cobo, J.; Navas, E.; Pintado, V.; et al. Infective Endocarditis in Congenital Heart Disease: A Frequent Community-Acquired Complication. Infection 2013, 41, 167–174. [Google Scholar] [CrossRef]
- Vicent, L.; Goenaga, M.A.; Muñoz, P.; Marín-Arriaza, M.; Valerio, M.; Fariñas, M.C.; Cobo-Belaustegui, M.; de Alarcón, A.; Rodríguez-Esteban, M.Á.; Miró, J.M.; et al. Infective Endocarditis in Children and Adolescents: A Different Profile with Clinical Implications. Pediatr. Res. 2022, 1–7. [Google Scholar] [CrossRef]
- Rushani, D.; Kaufman, J.S.; Ionescu-Ittu, R.; Mackie, A.S.; Pilote, L.; Therrien, J.; Marelli, A.J. Infective Endocarditis in Children with Congenital Heart Disease: Cumulative Incidence and Predictors. Circulation 2013, 128, 1412–1419. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rosenthal, L.B.; Feja, K.N.; Levasseur, S.M.; Alba, L.R.; Gersony, W.; Saiman, L. The Changing Epidemiology of Pediatric Endocarditis at a Children’s Hospital over Seven Decades. Pediatr. Cardiol. 2010, 31, 813–820. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cahill, T.J.; Jewell, P.D.; Denne, L.; Franklin, R.C.; Frigiola, A.; Orchard, E.; Prendergast, B.D. Contemporary Epidemiology of Infective Endocarditis in Patients with Congenital Heart Disease: A UK Prospective Study. Am. Heart J. 2019, 215, 70–77. [Google Scholar] [CrossRef] [PubMed]
- Snygg-Martin, U.; Giang, K.W.; Dellborg, M.; Robertson, J.; Mandalenakis, Z. Cumulative Incidence of Infective Endocarditis in Patients with Congenital Heart Disease: A Nationwide, Case-Control Study Over Nine Decades. Clin. Infect. Dis. 2021, 73, 1469–1475. [Google Scholar] [CrossRef]
- Baddour, L.M.; Wilson, W.R.; Bayer, A.S.; Fowler, V.G.J.; Tleyjeh, I.M.; Rybak, M.J.; Barsic, B.; Lockhart, P.B.; Gewitz, M.H.; Levison, M.E.; et al. Infective Endocarditis in Adults: Diagnosis, Antimicrobial Therapy, and Management of Complications: A Scientific Statement for Healthcare Professionals From the American Heart Association. Circulation 2015, 132, 1435–1486. [Google Scholar] [CrossRef]
- Martin, J.M.; Neches, W.H.; Wald, E.R. Infective Endocarditis: 35 Years of Experience at a Children’s Hospital. Clin. Infect. Dis. 1997, 24, 669–675. [Google Scholar] [CrossRef] [Green Version]
- Castillo, J.C.; Anguita, M.P.; Torres, F.; Siles, J.R.; Mesa, D.; Vallés, F. Risk Factors Associated with Endocarditis without Underlying Heart Disease. Rev. Esp. Cardiol. 2002, 55, 304–307. [Google Scholar] [CrossRef]
- Rech, A.; Loss, J.F.; Machado, A.; Brunetto, A.L. Infective Endocarditis (IE) in Children Receiving Treatment for Cancer. Pediatr Blood Cancer 2004, 43, 159–163. [Google Scholar] [CrossRef]
- Bendig, E.A.; Singh, J.; Butler, T.J.; Arrieta, A.C. The Impact of the Central Venous Catheter on the Diagnosis of Infectious Endocarditis Using Duke Criteria in Children with Staphylococcus Aureus Bacteremia. Pediatr. Infect. Dis. J. 2008, 27, 636–639. [Google Scholar] [CrossRef]
- Baltimore, R.S.; Gewitz, M.; Baddour, L.M.; Beerman, L.B.; Jackson, M.A.; Lockhart, P.B.; Pahl, E.; Schutze, G.E.; Shulman, S.T.; Willoughby, R. Infective Endocarditis in Childhood: 2015 Update. Circulation 2015, 132, 1487–1515. [Google Scholar] [CrossRef] [Green Version]
- Marom, D.; Levy, I.; Gutwein, O.; Birk, E.; Ashkenazi, S. Healthcare-Associated Versus Community-Associated Infective Endocarditis in Children. Pediatr. Infect. Dis. J. 2011, 30, 585–588. [Google Scholar] [CrossRef] [PubMed]
- Millar, B.C.; Jugo, J.; Moore, J.E. Fungal Endocarditis in Neonates and Children. Pediatr. Cardiol. 2005, 26, 517–536. [Google Scholar] [CrossRef] [PubMed]
- Woodruff, R.C.; Eliapo-Unutoa, I.; Chiou, H.; Gayapa, M.; Noonan, S.; Podila, P.S.B.; Rayle, V.; Sanchez, G.; Tulafono, R.; Van Beneden, C.A.; et al. Period Prevalence of Rheumatic Heart Disease and the Need for a Centralized Patient Registry in American Samoa, 2016 to 2018. J. Am. Heart. Assoc. 2021, 10, e020424. [Google Scholar] [CrossRef] [PubMed]
- Beaudoin, A.; Edison, L.; Introcaso, C.E.; Goh, L.; Marrone, J.; Mejia, A.; Van Beneden, C. Acute Rheumatic Fever and Rheumatic Heart Disease among Children-American Samoa, 2011–2012. MMWR Morb. Mortal Wkly. Rep. 2015, 64, 555–558. [Google Scholar]
- Rai, K.; Supriya, S.; Hegde, A.M. Oral Health Status of Children with Congenital Heart Disease and the Awareness, Attitude and Knowledge of Their Parents. J. Clin. Pediatr. Dent. 2009, 33, 315–318. [Google Scholar] [CrossRef]
- Suma, G.; Usha, M.D.; Ambika, G. Jairanganath Oral Health Status of Normal Children and Those Affiliated with Cardiac Diseases. J. Clin. Pediatr. Dent. 2011, 35, 315–318. [Google Scholar] [CrossRef]
- Lin, Y.-T.; Hsieh, K.-S.; Chen, Y.-S.; Huang, I.-F.; Cheng, M.-F. Infective Endocarditis in Children without Underlying Heart Disease. J. Microbiol. Immunol. Infect. 2013, 46, 121–128. [Google Scholar] [CrossRef] [Green Version]
- Holland, T.L.; Baddour, L.M.; Bayer, A.S.; Hoen, B.; Miro, J.M.; Fowler, V.G. Infective Endocarditis. Nat. Rev. Dis. Primers 2016, 2, 16059. [Google Scholar] [CrossRef]
- Bayliss, R.; Clarke, C.; Oakley, C.M.; Somerville, W.; Whitfield, A.G.; Young, S.E. The Microbiology and Pathogenesis of Infective Endocarditis. Br. Heart J. 1983, 50, 513–519. [Google Scholar] [CrossRef]
- Freedman, L.R. The Pathogenesis of Infective Endocarditis. J. Antimicrob. Chemother. 1987, 20, 1–6. [Google Scholar] [CrossRef]
- Freedman, L.R.; Valone, J.J. Experimental Infective Endocarditis. Prog. Cardiovasc. Dis. 1979, 22, 169–180. [Google Scholar] [CrossRef]
- Penk, J.S.; Webb, C.L.; Shulman, S.T.; Anderson, E.J. Echocardiography in Pediatric Infective Endocarditis. Pediatr. Infect. Dis. J. 2011, 30, 1109–1111. [Google Scholar] [CrossRef] [PubMed]
- Kelchtermans, J.; Grossar, L.; Eyskens, B.; Cools, B.; Roggen, M.; Boshoff, D.; Louw, J.; Frerich, S.; Veloso, T.R.; Claes, J.; et al. Clinical Characteristics of Infective Endocarditis in Children. Pediatr. Infect. Dis. J. 2019, 38, 453–458. [Google Scholar] [CrossRef]
- Dixon, G.; Christov, G. Infective Endocarditis in Children: An Update. Curr. Opin. Infect. Dis. 2017, 30, 257–267. [Google Scholar] [CrossRef] [PubMed]
- Liesman, R.M.; Pritt, B.S.; Maleszewski, J.J.; Patel, R.; Kraft, C.S. Laboratory Diagnosis of Infective Endocarditis. J. Clin. Microbiol. 2017, 55, 2599–2608. [Google Scholar] [CrossRef] [Green Version]
- Johnson, J.A.; Boyce, T.G.; Cetta, F.; Steckelberg, J.M.; Johnson, J.N. Infective Endocarditis in the Pediatric Patient: A 60-Year Single-Institution Review. Mayo Clin. Proc. 2012, 87, 629–635. [Google Scholar] [CrossRef] [Green Version]
- Day, M.D.; Gauvreau, K.; Shulman, S.; Newburger, J.W. Characteristics of Children Hospitalized with Infective Endocarditis. Circulation 2009, 119, 865–870. [Google Scholar] [CrossRef] [Green Version]
- Hoyer, A.; Silberbach, M. Infective Endocarditis. Pediatr. Rev. 2005, 26, 394–400. [Google Scholar] [CrossRef]
- Fournier, P.-E.; Gouriet, F.; Casalta, J.-P.; Lepidi, H.; Chaudet, H.; Thuny, F.; Collart, F.; Habib, G.; Raoult, D. Blood Culture-Negative Endocarditis: Improving the Diagnostic Yield Using New Diagnostic Tools. Medicine 2017, 96, 8392. [Google Scholar] [CrossRef]
- Fournier, P.-E.; Thuny, F.; Richet, H.; Lepidi, H.; Casalta, J.-P.; Arzouni, J.-P.; Maurin, M.; Célard, M.; Mainardi, J.-L.; Caus, T.; et al. Comprehensive Diagnostic Strategy for Blood Culture-Negative Endocarditis: A Prospective Study of 819 New Cases. Clin. Infect. Dis. 2010, 51, 131–140. [Google Scholar] [CrossRef] [Green Version]
- Li, J.S.; Sexton, D.J.; Mick, N.; Nettles, R.; Fowler, V.G.J.; Ryan, T.; Bashore, T.; Corey, G.R. Proposed Modifications to the Duke Criteria for the Diagnosis of Infective Endocarditis. Clin. Infect. Dis. 2000, 30, 633–638. [Google Scholar] [CrossRef] [PubMed]
- Tissières, P.; Gervaix, A.; Beghetti, M.; Jaeggi, E.T. Value and Limitations of the von Reyn, Duke, and Modified Duke Criteria for the Diagnosis of Infective Endocarditis in Children. Pediatrics 2003, 112, e467–e471. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Del Pont, J.; De Cicco, L.; Vartalitis, C.; Ithurralde, M.; Gallo, J.; Vargas, F.; Gianantonio, C.; Quirós, R. Infective Endocarditis in Children: Clinical Analyses and Evaluation of Two Diagnostic Criteria. Pediatr. Infect. Dis. J. 1995, 14, 1079–1086. [Google Scholar] [CrossRef] [PubMed]
- Stockheim, J.A.; Chadwick, E.G.; Kessler, S.; Amer, M.; Abdel-Haq, N.; Dajani, A.S.; Shulman, S.T. Are the Duke Criteria Superior to the Beth Israel Criteria for the Diagnosis of Infective Endocarditis in Children? Clin. Infect. Dis. 1998, 27, 1451–1456. [Google Scholar] [CrossRef] [Green Version]
- Durack, D.T.; Lukes, A.S.; Bright, D.K. Duke Endocarditis Service New Criteria for Diagnosis of Infective Endocarditis: Utilization of Specific Echocardiographic Findings. Am. J. Med. 1994, 96, 200–209. [Google Scholar] [CrossRef]
- Habib, G.; Lancellotti, P.; Antunes, M.J.; Bongiorni, M.G.; Casalta, J.-P.; Del Zotti, F.; Dulgheru, R.; El Khoury, G.; Erba, P.A.; Iung, B.; et al. 2015 ESC Guidelines for the Management of Infective Endocarditis: The Task Force for the Management of Infective Endocarditis of the European Society of Cardiology (ESC)Endorsed by: European Association for Cardio-Thoracic Surgery (EACTS), the European Association of Nuclear Medicine (EANM). Eur. Heart J. 2015, 36, 3075–3128. [Google Scholar] [CrossRef]
- Evangelista, A.; Gonzalez-Alujas, M.T. Echocardiography in Infective Endocarditis. Heart 2004, 90, 614–617. [Google Scholar] [CrossRef] [Green Version]
- Puchalski, M.D.; Lui, G.K.; Miller-Hance, W.C.; Brook, M.M.; Young, L.T.; Bhat, A.; Roberson, D.A.; Mercer-Rosa, L.; Miller, O.I.; Parra, D.A.; et al. Guidelines for Performing a Comprehensive Transesophageal Echocardiographic: Examination in Children and All Patients with Congenital Heart Disease: Recommendations from the American Society of Echocardiography. J. Am. Soc. Echocardiogr. 2019, 32, 173–215. [Google Scholar] [CrossRef]
- Aly, A.M.; Simpson, P.M.; Humes, R.A. The Role of Transthoracic Echocardiography in the Diagnosis of Infective Endocarditis in Children. Arch. Pediatr. Adolesc. Med. 1999, 153, 950–954. [Google Scholar] [CrossRef] [Green Version]
- Kelly, P.; Hua, N.; Madriago, E.J.; Holmes, K.W.; Shaughnessy, R.; Ronai, C. The Utility of Echocardiography in Pediatric Patients with Structurally Normal Hearts and Suspected Endocarditis. Pediatr. Cardiol. 2020, 41, 62–68. [Google Scholar] [CrossRef]
- Di Filippo, S.; Delahaye, F.; Semiond, B.; Celard, M.; Henaine, R.; Ninet, J.; Sassolas, F.; Bozio, A. Current Patterns of Infective Endocarditis in Congenital Heart Disease. Heart 2006, 92, 1490–1495. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Caiati, C.; Pollice, P.; Lepera, M.E.; Favale, S. Pacemaker Lead Endocarditis Investigated with Intracardiac Echocardiography: Factors Modulating the Size of Vegetations and Larger Vegetation Embolic Risk during Lead Extraction. Antibiotics 2019, 8, 228. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Caiati, C.; Luzzi, G.; Pollice, P.; Favale, S.; Lepera, M.E. A Novel Clinical Perspective on New Masses after Lead Extraction (Ghosts) by Means of Intracardiac Echocardiography. J. Clin. Med. 2020, 9, 2571. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.C.; Aung, T.T.; Khan, S.; Wase, A. Utility of Intracardiac Echocardiography to Diagnose Infective Endocarditis. J. Investig. Med. High Impact Case Rep. 2019, 7, 2075. [Google Scholar] [CrossRef] [PubMed]
- Chau, A.; Renella, P.; Arrieta, A. Multimodality Cardiovascular Imaging in the Diagnosis and Management of Prosthetic Valve Infective Endocarditis in Children Report of Two Cases and Brief Review of the Literature. Cardiol. Young 2019, 29, 1526–1529. [Google Scholar] [CrossRef] [PubMed]
- Parlow, S.; Beamish, P.; Desjardins, I.; Fulop, J.; Maharajh, G.; Castellucci, L. Infected Rastelli Conduit in an Immunocompromised Patient That Was Not Visible on Transthoracic Echocardiogram. CJC Open 2019, 1, 324–326. [Google Scholar] [CrossRef]
- Kawamura, J.; Ueno, K.; Taimura, E.; Matsuba, T.; Imoto, Y.; Jinguji, M.; Kawano, Y. Case Report: (18)F-FDG PET-CT for Diagnosing Prosthetic Device-Related Infection in an Infant With CHD. Front. Pediatr. 2021, 9, 584741. [Google Scholar] [CrossRef]
- Jasper, N.; Däbritz, J.; Frosch, M.; Loeffler, M.; Weckesser, M.; Foell, D. Diagnostic Value of [(18)F]-FDG PET/CT in Children with Fever of Unknown Origin or Unexplained Signs of Inflammation. Eur. J. Nucl. Med. Mol. Imaging 2010, 37, 136–145. [Google Scholar] [CrossRef]
- Walter, C.; Zuccarino, F.; Carretero Bellón, J.M. PET/CT Role in the Diagnosis of Infective Endocarditis in Patients with Congenital Heart Disease. Anales de Pediatría 2022, 96, 260–263. [Google Scholar] [CrossRef]
- Corey, K.M.; Campbell, M.J.; Hill, K.D.; Hornik, C.P.; Krasuski, R.; Barker, P.C.; Jaquiss, R.D.B.; Li, J.S. Pulmonary Valve Endocarditis: The Potential Utility of Multimodal Imaging Prior to Surgery. World J. Pediatr. Congenit. Heart Surg. 2020, 11, 192–197. [Google Scholar] [CrossRef]
- Meyer, Z.; Fischer, M.; Koerfer, J.; Laser, K.T.; Kececioglu, D.; Burchert, W.; Ulrich, S.; Preuss, R.; Haas, N.A. The Role of FDG-PET-CT in Pediatric Cardiac Patients and Patients with Congenital Heart Defects. Int. J. Cardiol. 2016, 220, 656–660. [Google Scholar] [CrossRef]
- Servaes, S. Imaging Infection and Inflammation in Children with (18)F-FDG PET and (18)F-FDG PET/CT. J. Nucl. Med. Technol. 2011, 39, 179–182. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- O’Hagan, S.; Nelson, P.; Speirs, L.; Moriarty, P.; Mallett, P. How to Interpret a Paediatric Blood Culture. Arch. Dis. Child Educ. Pract. Ed. 2021, 106, 244. [Google Scholar] [CrossRef] [PubMed]
- Dien Bard, J.; McElvania TeKippe, E. Diagnosis of Bloodstream Infections in Children. J. Clin. Microbiol. 2016, 54, 1418–1424. [Google Scholar] [CrossRef] [Green Version]
- Pericàs, J.M.; Hernández-Meneses, M.; Muñoz, P.; Martínez-Sellés, M.; Álvarez-Uria, A.; de Alarcón, A.; Gutiérrez-Carretero, E.; Goenaga, M.A.; Zarauza, M.J.; Falces, C.; et al. Characteristics and Outcome of Acute Heart Failure in Infective Endocarditis: Focus on Cardiogenic Shock. Clin. Infect. Dis. 2021, 73, 765–774. [Google Scholar] [CrossRef] [PubMed]
- Wilson, W.R.; Danielson, G.K.; Giuliani, E.R.; Washington, J.A., 2nd; Jaumin, P.M.; Geraci, J.E. Cardiac Valve Replacement in Congestive Heart Failure Due to Infective Endocarditis. Mayo Clin. Proc. 1979, 54, 223–226. [Google Scholar] [PubMed]
- Nadji, G.; Rusinaru, D.; Rémadi, J.-P.; Jeu, A.; Sorel, C.; Tribouilloy, C. Heart Failure in Left-Sided Native Valve Infective Endocarditis: Characteristics, Prognosis, and Results of Surgical Treatment. Eur. J. Heart Fail. 2009, 11, 668–675. [Google Scholar] [CrossRef]
- Anguera, I.; Miro, J.M.; Evangelista, A.; Cabell, C.H.; San Roman, J.A.; Vilacosta, I.; Almirante, B.; Ripoll, T.; Fariñas, M.C.; Anguita, M.; et al. Periannular Complications in Infective Endocarditis Involving Native Aortic Valves. Am. J. Cardiol. 2006, 98, 1254–1260. [Google Scholar] [CrossRef]
- Shmueli, H.; Thomas, F.; Flint, N.; Setia, G.; Janjic, A.; Siegel, R.J. Right-Sided Infective Endocarditis 2020: Challenges and Updates in Diagnosis and Treatment. J. Am. Heart. Assoc. 2020, 9, e017293. [Google Scholar] [CrossRef]
- Pettersson, G.B.; Hussain, S.T. Current AATS Guidelines on Surgical Treatment of Infective Endocarditis. Ann. Cardiothorac. Surg. 2019, 8, 630–644. [Google Scholar] [CrossRef] [Green Version]
- Habib, G. Embolic Risk in Subacute Bacterial Endocarditis: Determinants and Role of Transesophageal Echocardiography. Curr. Cardiol. Rep. 2003, 5, 129–136. [Google Scholar] [CrossRef] [PubMed]
- Restrepo, M.S.; Turek, J.W.; Reinking, B.; Bergen, N.V. Mycotic Aneurysm in a Child with History of Coarctation of the Aorta Repair. Ann. Pediatr. Cardiol 2014, 7, 138–141. [Google Scholar] [CrossRef] [PubMed]
- Bergsland, J.; Kawaguchi, A.; Roland, J.M.; Pieroni, D.R.; Subramanian, S. Mycotic Aortic Aneurysms in Children. Ann. Thorac. Surg. 1984, 37, 314–318. [Google Scholar] [CrossRef]
- Johnson, J.R.; Ledgerwood, A.M.; Lucas, C.E. Mycotic Aneurysm. New Concepts in Therapy. Arch. Surg 1983, 118, 577–582. [Google Scholar] [CrossRef]
- AlBassri, T.; Sheikho, M.; Chaikhouni, F.; Al Habshan, F.; Kabbani, M.S. Neurological Complications in Children with Infective Endocarditis: Incidence, Risk Factors, and Outcome: A 10-Year Single-Center Experience. Int. J. Pediatr. Adolesc. Med. 2021, 8, 198–202. [Google Scholar] [CrossRef]
- Asakai, H.; Cardamone, M.; Hutchinson, D.; Stojanovski, B.; Galati, J.C.; Cheung, M.M.H.; Mackay, M.T. Arterial Ischemic Stroke in Children with Cardiac Disease. Neurology 2015, 85, 2053–2059. [Google Scholar] [CrossRef] [Green Version]
- Okazaki, S.; Yoshioka, D.; Sakaguchi, M.; Sawa, Y.; Mochizuki, H.; Kitagawa, K. Acute Ischemic Brain Lesions in Infective Endocarditis: Incidence, Related Factors, and Postoperative Outcome. Cerebrovasc. Dis. 2013, 35, 155–162. [Google Scholar] [CrossRef]
- Takagi, Y.; Higuchi, Y.; Kondo, H.; Akita, K.; Ishida, M.; Kaneko, K.; Hoshino, R.; Sato, M.; Ando, M. The Importance of Preoperative Magnetic Resonance Imaging in Valve Surgery for Active Infective Endocarditis. Gen. Thorac. Cardiovasc. Surg. 2011, 59, 467–471. [Google Scholar] [CrossRef]
- Goulenok, T.; Klein, I.; Mazighi, M.; Messika-Zeitoun, D.; Alexandra, J.F.; Mourvillier, B.; Laissy, J.P.; Leport, C.; Iung, B.; Duval, X. Infective Endocarditis with Symptomatic Cerebral Complications: Contribution of Cerebral Magnetic Resonance Imaging. Cerebrovasc. Dis. 2013, 35, 327–336. [Google Scholar] [CrossRef]
- Bonaros, N.; Czerny, M.; Pfausler, B.; Müller, S.; Bartel, T.; Thielmann, M.; Shehada, S.-E.; Folliguet, T.; Obadia, J.-F.; Holfeld, J.; et al. Infective Endocarditis and Neurologic Events: Indications and Timing for Surgical Interventions. Eur. Heart J. 2020, 22, M19–M25. [Google Scholar] [CrossRef]
- Sadikoglu, B.; Bilge, I.; Kilicaslan, I.; Gokce, M.G.; Emre, S.; Ertugrul, T. Crescentic Glomerulonephritis in a Child with Infective Endocarditis. Pediatr. Nephrol. 2006, 21, 867–869. [Google Scholar] [CrossRef] [PubMed]
- Daimon, S.; Mizuno, Y.; Fujii, S.; Mukai, K.; Hanakawa, H.; Otsuki, N.; Yasuhara, S.; Saga, T.; Koni, I. Infective Endocarditis-Induced Crescentic Glomerulonephritis Dramatically Improved by Plasmapheresis. Am. J. Kidney Dis. 1998, 32, 309–313. [Google Scholar] [CrossRef] [PubMed]
- Rajaratnam, D.; Rajaratnam, R. Outpatient Antimicrobial Therapy for Infective Endocarditis Is Safe. Heart Lung Circ. 2021, 30, 207–215. [Google Scholar] [CrossRef] [PubMed]
- Hendarto, A.; Putri, N.D.; Yunita, D.R.; Efendi, M.; Prayitno, A.; Karyanti, M.R.; Satari, H.I.; Hadinegoro, S.R.S.; Chan, M. First Pediatric Outpatient Parenteral Antibiotic Therapy Clinic in Indonesia. Front. Pediatr. 2020, 8, 156. [Google Scholar] [CrossRef] [Green Version]
- Khoo, B.; Buratto, E.; Fricke, T.A.; Gelbart, B.; Brizard, C.P.; Brink, J.; d’Udekem, Y.; Konstantinov, I.E. Outcomes of Surgery for Infective Endocarditis in Children: A 30-Year Experience. J. Thorac. Cardiovasc. Surg. 2019, 158, 1399–1409. [Google Scholar] [CrossRef]
- Beierlein, W.; Becker, V.; Yates, R.; Tsang, V.; Elliott, M.; de Leval, M.; van Doorn, C. Long-Term Follow-up after Mitral Valve Replacement in Childhood: Poor Event-Free Survival in the Young Child. Eur. J. Cardiothorac. Surg. 2007, 31, 860–865. [Google Scholar] [CrossRef] [Green Version]
- Harris, C.; Albaeni, A.; Norris, K. Impact of Malnutrition in Patients With Infective Endocarditis. Nutr. Clin. Pract. 2020, 36, 472–479. [Google Scholar] [CrossRef]
- Rasmussen, T.B.; Zwisler, A.-D.; Risom, S.S.; Sibilitz, K.L.; Christensen, J.; Bundgaard, H.; Moons, P.; Thygesen, L.C.; Lindschou, J.; Norekvål, T.M.; et al. Comprehensive Cardiac Rehabilitation for Patients Following Infective Endocarditis: Results of the Randomized CopenHeartIE Trial. Eur. J. Cardiovasc. Nurs. 2021, 21, 261–270. [Google Scholar] [CrossRef]
- Rhodes, J.; Curran, T.J.; Camil, L.; Rabideau, N.; Fulton, D.R.; Gauthier, N.S.; Gauvreau, K.; Jenkins, K.J. Sustained Effects of Cardiac Rehabilitation in Children with Serious Congenital Heart Disease. Pediatrics 2006, 118, 586–593. [Google Scholar] [CrossRef]
- Rhodes, J.; Curran, T.J.; Camil, L.; Rabideau, N.; Fulton, D.R.; Gauthier, N.S.; Gauvreau, K.; Jenkins, K.J. Impact of Cardiac Rehabilitation on the Exercise Function of Children with Serious Congenital Heart Disease. Pediatrics 2005, 116, 1339–1345. [Google Scholar] [CrossRef]
- Alexiou, C.; Langley, S.M.; Monro, J.L. Surgery for Infective Valve Endocarditis in Children. Eur. J. Cardiothorac. Surg. 1999, 16, 653–659. [Google Scholar] [CrossRef] [Green Version]
- Ware, A.L.; Tani, L.Y.; Weng, H.-Y.; Wilkes, J.; Menon, S.C. Resource Utilization and Outcomes of Infective Endocarditis in Children. J. Pediatr. 2014, 165, 807–812. [Google Scholar] [CrossRef] [PubMed]
- Ahtela, E.; Oksi, J.; Porela, P.; Ekström, T.; Rautava, P.; Kytö, V. Trends in Occurrence and 30-Day Mortality of Infective Endocarditis in Adults: Population-Based Registry Study in Finland. BMJ Open 2019, 9, e026811. [Google Scholar] [CrossRef] [PubMed]
- Le, J.; Dam, Q.; Tran, T.; Nguyen, A.; Adler-Shohet, F.C.; Kim, S.; Schmidt, K.; Lieberman, J.M.; Bradley, J.S. Epidemiology and Hospital Readmission Associated with Complications of Staphylococcus Aureus Bacteremia in Pediatrics over a 25-Year Period. Epidemiol. Infect. 2017, 145, 2631–2639. [Google Scholar] [CrossRef] [Green Version]
- Pantoja, F.I.; Ricaurte, W.R.; Rosero, D.E. Relationship between death and admission of pediatric patients to intensive care due to Staphylococcus aureus bacteremia acquired in the community, 2014–2017. Biomedica 2021, 41, 145–152. [Google Scholar] [CrossRef]
- Maser, M.; Freisinger, E.; Bronstein, L.; Köppe, J.; Orwat, S.; Kaleschke, G.; Baumgartner, H.; Diller, G.-P.; Lammers, A. Frequency, Mortality, and Predictors of Adverse Outcomes for Endocarditis in Patients with Congenital Heart Disease: Results of a Nationwide Analysis Including 2512 Endocarditis Cases. J. Clin. Med. 2021, 10, 5071. [Google Scholar] [CrossRef]
- Vicent, L.; Saldivar, H.G.; Bouza, E.; Muñoz, P.; Cuerpo, G.; de Alarcón, A.; Vidal, B.; Cobo, M.; Goenaga, M.Á.; Carrasco-Chinchilla, F.; et al. Prognostic Implications of a Negative Echocardiography in Patients with Infective Endocarditis. Eur. J. Intern. Med. 2018, 52, 40–48. [Google Scholar] [CrossRef]
- Calderón-Parra, J.; Kestler, M.; Ramos-Martínez, A.; Bouza, E.; Valerio, M.; de Alarcón, A.; Luque, R.; Goenaga, M.Á.; Echeverría, T.; Fariñas, M.C.; et al. Clinical Factors Associated with Reinfection versus Relapse in Infective Endocarditis: Prospective Cohort Study. J. Clin. Med. 2021, 10, 748. [Google Scholar] [CrossRef]
- Alagna, L.; Park, L.P.; Nicholson, B.P.; Keiger, A.J.; Strahilevitz, J.; Morris, A.; Wray, D.; Gordon, D.; Delahaye, F.; Edathodu, J.; et al. Repeat Endocarditis: Analysis of Risk Factors Based on the International Collaboration on Endocarditis-Prospective Cohort Study. Clin. Microbiol. Infect. 2014, 20, 566–575. [Google Scholar] [CrossRef] [Green Version]
- Armiñanzas, C.; Fariñas-Alvarez, C.; Zarauza, J.; Muñoz, P.; González Ramallo, V.; Martínez Sellés, M.; Miró Meda, J.M.; Pericás, J.M.; Goenaga, M.Á.; Ojeda Burgos, G.; et al. Role of Age and Comorbidities in Mortality of Patients with Infective Endocarditis. Eur. J. Intern. Med. 2019, 64, 63–71. [Google Scholar] [CrossRef] [Green Version]
- Bonow, R.O.; Carabello, B.A.; Chatterjee, K.; de Leon, A.C.J.; Faxon, D.P.; Freed, M.D.; Gaasch, W.H.; Lytle, B.W.; Nishimura, R.A.; O’Gara, P.T.; et al. ACC/AHA 2006 Guidelines for the Management of Patients with Valvular Heart Disease: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 1998 Guidelines for the Management of Patients with Valvular Heart Disease) Developed in Collaboration with the Society of Cardiovascular Anesthesiologists Endorsed by the Society for Cardiovascular Angiography and Interventions and the Society of Thoracic Surgeons. J. Am. Coll. Cardiol. 2006, 48, 1–148. [Google Scholar] [CrossRef] [Green Version]
- Vähäsarja, N.; Lund, B.; Ternhag, A.; Götrick, B.; Olaison, L.; Hultin, M.; Krüger Weiner, C.; Naimi-Akbar, A. Incidence of Infective Endocarditis Caused by Viridans Group Streptococci in Sweden-Effect of Cessation of Antibiotic Prophylaxis in Dentistry for Risk Individuals. J. Oral Microbiol. 2020, 12, 1768342. [Google Scholar] [CrossRef] [PubMed]
- Mackie, A.S.; Liu, W.; Savu, A.; Marelli, A.J.; Kaul, P. Infective Endocarditis Hospitalizations Before and After the 2007 American Heart Association Prophylaxis Guidelines. Can. J. Cardiol. 2016, 32, 942–948. [Google Scholar] [CrossRef]
- Desimone, D.C.; Tleyjeh, I.M.; Correa de Sa, D.D.; Anavekar, N.S.; Lahr, B.D.; Sohail, M.R.; Steckelberg, J.M.; Wilson, W.R.; Baddour, L.M. Incidence of Infective Endocarditis Caused by Viridans Group Streptococci before and after Publication of the 2007 American Heart Association’s Endocarditis Prevention Guidelines. Circulation 2012, 126, 60–64. [Google Scholar] [CrossRef] [PubMed]
- Thornhill, M.H.; Dayer, M.; Lockhart, P.B.; Prendergast, B. Antibiotic Prophylaxis of Infective Endocarditis. Curr Infect Dis Rep 2017, 19, 1–8. [Google Scholar] [CrossRef] [PubMed] [Green Version]



| Congenital Heart Disease | Vulnerable: Acquired Risk Factors | Previous Healthy |
|---|---|---|
| Cyanotic disease | Immunodeficiency | Dental procedures |
| Recent cardiac surgery Left-sided lesions Endocardial cushion defects Recent corrective cardiac surgery | Cancer Hemodialysis | Skin infections/lacerations |
| No CHD | CHD |
|---|---|
| S. aureus 35–40% | S. aureus 25–30% |
| Streptococcus spp. 35–40% | Coagulase-negative Staphylococci 10–15% |
| Enterococcus 11% | Streptococcus spp. 20–30% |
| Gram-negative bacilli 10–15% | Enterococcus 3% |
| Coagulase-negative Staphylococci 0–5% | Gram-negative bacilli 25–30% |
| Infective Endocarditis–Modified Duke Criteria * |
|---|
| Major criteria |
| Blood culture positive for typical microorganism (i.e., Staphylococcus aureus, Enterococcus, Streptococci viridans) |
| Echocardiogram showing valvular vegetation |
| Minor criteria |
| Predisposing cardiac condition or injection drug use |
| Temperature > 38 °C |
| Embolic phenomena |
| Immunologic phenomena (glomerulonephritis, Osler’s nodes, Roth’s spots, and rheumatoid factor) |
| Positive blood culture not meeting above criteria |
| Infective Endocarditis Differential Diagnosis in Children |
|---|
| Familial Mediterranean Fever, juvenile rheumatoid arthritis |
| Rheumatic fever |
| Acute myocarditis |
| Pneumonia |
| Kawasaki disease |
| Acute myelocytic leukemia |
| Bacterial meningitis |
| Childhood vasculitis |
| Rheumatic diseases |
| Infections complicated with septicemia (i.e., soft tissues, urinary, etc.) |
| Risk Factors for IE Complications |
|---|
| Size of the vegetation > 1 cm |
| Younger age, prematurity |
| Staphyloccocus aureus, fungal infection |
| No known heart disease |
| Left-sided valvular lesion |
| Complex cyanotic congenital heart disease |
| Higher white blood cell counts and plasma C-reactive protein |
| Persistent fever |
| Causative Microorganism | Antibiotic Regimen | |
|---|---|---|
| Unknown agent |
| |
| S. aureus | Methicillin-sensitive | Methicillin-resistant |
| vancomycin or daptomycin 4–6 w | |
| Streptococcus | Penicillin-sensitive | Penicillin-resistant |
|
| |
| Enterococcus | Non high-level aminoglycoside resistance
| High-level aminoglycoside resistance
|
| HACEK group | Ceftriaxone OR cefotaxime OR ampicillin-sulbactam 4 w | Alternative regimen
|
| Fungi Candida spp., Aspergillus spp. | Cardiac surgery + antifungal agents
| Chronic suppressive therapy with oral fluconazole lifelong in patients who cannot undergo surgical resection |
| Indications for Surgery in Patients with Infective Endocarditis |
|---|
| Valve dysfunction resulting in symptoms of heart failure |
| Left-sided IE caused by S. aureus |
| Fungal or highly resistant microorganisms |
| Complications: heart block, annular or aortic abscess, pseudoaneurism or fistulae |
| Persistent infection (persistent bacteremia, fever > 5–7 days despite appropriate antimicrobial therapy) |
| Relapsing infection (recurrence of bacteremia after a complete antibiotic course) |
| Persistent vegetation and recurrent emboli despite appropriate antimicrobial therapy |
| Persistent fever |
| Previous IE |
|---|
| Previous cardiac surgery and prosthetic material for cardiac valve or congenital heart defects repair |
| Prosthetic valves |
| Cyanotic congenital heart disease |
| Heart transplant with heart valve disease |
| Mechanical circulatory support |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vicent, L.; Luna, R.; Martínez-Sellés, M. Pediatric Infective Endocarditis: A Literature Review. J. Clin. Med. 2022, 11, 3217. https://doi.org/10.3390/jcm11113217
Vicent L, Luna R, Martínez-Sellés M. Pediatric Infective Endocarditis: A Literature Review. Journal of Clinical Medicine. 2022; 11(11):3217. https://doi.org/10.3390/jcm11113217
Chicago/Turabian StyleVicent, Lourdes, Raquel Luna, and Manuel Martínez-Sellés. 2022. "Pediatric Infective Endocarditis: A Literature Review" Journal of Clinical Medicine 11, no. 11: 3217. https://doi.org/10.3390/jcm11113217
APA StyleVicent, L., Luna, R., & Martínez-Sellés, M. (2022). Pediatric Infective Endocarditis: A Literature Review. Journal of Clinical Medicine, 11(11), 3217. https://doi.org/10.3390/jcm11113217







