The Impact of Withdrawn vs. Agitated Relatives during Resuscitation on Team Workload: A Single-Center Randomised Simulation-Based Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Study Design
2.3. Simulator and Scenario
2.4. Family Member Presence
2.5. NASA Task Load Index
2.6. Data Analysis
2.7. Statistical Analysis
3. Results
3.1. Participants
3.2. Primary Outcomes
3.3. Secondary Outcomes
4. Discussion
4.1. Primary Outcome
4.2. Secondary Outcomes
4.3. NASA TLX
4.4. Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
- –
- quiet crying/mourning
- –
- quietly observes what is happening
- –
- does not talk directly to the participants; except when asked by the doctors
- –
- does not touch the patient or the participants
- –
- asks to stay with the relative in case the participants want to expel him/her from the room
- –
- loud crying/mourning
- –
- walks around the room worried and upset
- –
- tries to touch the patient once or twice
- –
- During resuscitation, asks the participants questions about the measures performed, the further procedure and the patient’s chances of survival
- –
- vehemently insists on staying with his relative in case the participants want to expel him from the room.
References
- Doyle, C.J.; Post, H.; Burney, R.E.; Maino, J.; Keefe, M.; Rhee, K.J. Family participation during resuscitation: An option. Ann. Emerg. Med. 1987, 16, 673–675. [Google Scholar] [CrossRef]
- Barreto, M.D.S.; Peruzzo, H.E.; Garcia-Vivar, C.; Marcon, S.S. Family presence during cardiopulmonary resuscitation and invasive procedures: A meta-synthesis. Rev. Esc. Enferm. USP 2019, 53, e03435. [Google Scholar] [CrossRef]
- Downar, J.; Kritek, P.A. Family Presence during Cardiac Resuscitation. N. Engl. J. Med. 2013, 368, 1060–1062. [Google Scholar]
- Fernandes, A.P.; de Souza, C.C.; Geocze, L.; Batista Santos, V.; Guizilini, S.; Lopes Moreira, R.S. Experiences and opinions of health professionals in relation to the presence of the family during in-hospital cardiopulmonary resuscitation: An integrative review. J. Nurs. Educ. Pract. 2014, 4, 85–94. [Google Scholar] [CrossRef] [Green Version]
- Perkins, G.D.; Graesner, J.T.; Semeraro, F.; Olasveengen, T.; Soar, J.; Lott, C.; Van de Voorde, P.; Madar, J.; Zideman, D.; Mentzelopoulos, S.; et al. European Resuscitation Council Guidelines 2021: Executive summary. Resuscitation 2021, 161, 1–60. [Google Scholar] [CrossRef]
- Mentzelopoulos, S.D.; Couper, K.; Voorde, P.V.; Druwé, P.; Blom, M.; Perkins, G.D.; Lulic, I.; Djakow, J.; Raffay, V.; Lilja, G.; et al. European Resuscitation Council Guidelines 2021: Ethics of resuscitation and end of life decisions. Resuscitation 2021, 161, 408–432. [Google Scholar] [CrossRef]
- Madar, J.; Roehr, C.C.; Ainsworth, S.; Ersdal, H.; Morley, C.; Rüdiger, M.; Skåre, C.; Szczapa, T.; Te Pas, A.; Trevisanuto, D.; et al. European Resuscitation Council Guidelines 2021: Newborn resuscitation and support of transition of infants at birth. Resuscitation 2021, 161, 291–326. [Google Scholar] [CrossRef]
- Bjørshol, C.A.; Myklebust, H.; Nilsen, K.L.; Hoff, T.; Bjørkli, C.; Illguth, E.; Søreide, E.; Sunde, K. Effect of socioemotional stress on the quality of cardiopulmonary resuscitation during advanced life support in a randomized manikin study. Crit. Care Med. 2011, 39, 300–304. [Google Scholar] [CrossRef]
- Hunziker, S.; Semmer, N.K.; Tschan, F.; Schuetz, P.; Mueller, B.; Marsch, S. Dynamics and association of different acute stress markers with performance during a simulated resuscitation. Resuscitation 2012, 83, 572–578. [Google Scholar] [CrossRef]
- Jabre, P.; Belpomme, V.; Azoulay, E.; Jacob, L.; Bertrand, L.; Lapostolle, F.; Tazarourte, K.; Bouilleau, G.; Pinaud, V.; Broche, C.; et al. Family Presence during Cardiopulmonary Resuscitation. N. Engl. J. Med. 2013, 368, 1008–1018. [Google Scholar] [CrossRef] [Green Version]
- Fernandez, R.; Compton, S.; Jones, K.A.; Velilla, M.A. The presence of a family witness impacts physician performance during simulated medical codes. Crit. Care Med. 2009, 37, 1956–1960. [Google Scholar] [CrossRef]
- Sak-Dankosky, N.; Andruszkiewicz, P.; Sherwood, P.R.; Kvist, T. Integrative review: Nurses’ and physicians’ experiences and attitudes towards inpatient-witnessed resuscitation of an adult patient. J. Adv. Nurs. 2014, 70, 957–974. [Google Scholar] [CrossRef]
- Willmes MSellmann, T.; Semmer, N.K.; Tschan, F.; Wetzchewald, D.; Schwager, H.; Russo, S.G.; Marsch, S. The impact of family presence during cardiopulmonary resuscitation on team performance and perceived task load: A prospective randomized simulator-based trial. BMJ Open 2022, 12, e056798. [Google Scholar] [CrossRef]
- Abella, B.S.; Sandbo, N.; Vassilatos, P.; Alvarado, J.P.; O’Hearn, N.; Wigder, H.N.; Hoffman, P.; Tynus, K.; Vanden Hoek, T.L.; Becker, L.B. Chest compression rates during cardiopulmonary resuscitation are suboptimal: A prospective study during in-hospital cardiac arrest. Circulation 2005, 111, 428–434. [Google Scholar] [CrossRef]
- Abella, B.S.; Alvarado, J.P.; Myklebust, H.; Edelson, D.P.; Barry, A.; O’Hearn, N.; Vanden Hoek, T.L.; Becker, L.B. Quality of Cardiopulmonary Resuscitation During In-Hospital Cardiac Arrest. J. Am. Med. Assoc. 2005, 293, 305–310. [Google Scholar] [CrossRef] [Green Version]
- Hunziker, S.; Tschan, F.; Semmer, N.K.; Zobrist, R.; Spychiger, M.; Breuer, M.; Hunziker, P.R.; Marsch, S.C. Hands-on time during cardiopulmonary resuscitation is affected by the process of teambuilding: A prospective randomised simulator-based trial. BMC Emerg. Med. 2009, 9, 3. [Google Scholar] [CrossRef] [Green Version]
- Marsch, S.C.; Muller, C.; Marquardt, K.; Conrad, G.; Tschan, F.; Hunziker, P.R. Human factors affect the quality of cardiopulmonary resuscitation in simulated cardiac arrests. Resuscitation 2004, 60, 51–56. [Google Scholar] [CrossRef]
- Tschan, F.; Vetterli, M.; Semmer, N.K.; Hunziker, S.; Marsch, S.C. Activities during interruptions in cardiopulmonary resuscitation: A simulator study. Resuscitation 2011, 82, 1419–1423. [Google Scholar] [CrossRef]
- Goldberger, Z.D.; Nallamothu, B.K.; Nichol, G.; Chan, P.S.; Curtis, J.R.; Cooke, C.R. Policies Allowing Family Presence During Resuscitation and Patterns of Care During In-Hospital Cardiac Arrest. Circ. Cardiovasc. Qual. Outcomes 2015, 8, 226–234. [Google Scholar] [CrossRef] [Green Version]
- Waldemar, A.; Bremer, A.; Holm, A.; Strömberg, A.; Thylén, I. In-hospital family-witnessed resuscitation with a focus on the prevalence, processes, and outcomes of resuscitation: A retrospective observational cohort study. Resuscitation 2021, 165, 23–30. [Google Scholar] [CrossRef]
- Arriaga, A.F.; Bader, A.M.; Wong, J.M.; Lipsitz, S.R.; Berry, W.R.; Ziewacz, J.E.; Hepner, D.L.; Boorman, D.J.; Pozner, C.N.; Smink, D.S.; et al. Simulation-Based Trial of Surgical-Crisis Checklists. N. Engl. J. Med. 2013, 368, 246–253. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cheng, A.; Kessler, D.; Mackinnon, R.; Chang, T.P.; Nadkarni, V.M.; Hunt, E.A.; Duval-Arnould, J.; Lin, Y.; Cook, D.A.; Pusic, M.; et al. Reporting Guidelines for Health Care Simulation Research: Extensions to the CONSORT and STROBE Statements. Simul. Healthc. 2016, 11, 238–248. [Google Scholar] [CrossRef]
- Hart, S.; Staveland, L. Development of NASA-TLX (Task Load Index): Results of Empirical and Theoretical Research. In Human Mental Workload; Hancock, P., Meshkati, N., Eds.; North Holland Press: Amsterdam, The Netherlands, 1988; pp. 139–183. [Google Scholar]
- Hart, S.G. Nasa-Task Load Index (NASA-TLX); 20 Years Later. Proc. Hum. Factors Ergon. Soc. Annu. Meet. 2006, 50, 904–908. [Google Scholar] [CrossRef] [Green Version]
- Colligan, L.; Potts, H.W.W.; Finn, C.T.; Sinkin, R.A. Cognitive workload changes for nurses transitioning from a legacy system with paper documentation to a commercial electronic health record. Int. J. Med. Inform. 2015, 84, 469–476. [Google Scholar] [CrossRef] [PubMed]
- Jabre, P.; Tazarourte, K.; Azoulay, E.; Borron, S.W.; Belpomme, V.; Jacob, L.; Bertrand, L.; Lapostolle, F.; Combes, X.; Galinski, M.; et al. Offering the opportunity for family to be present during cardiopulmonary resuscitation: 1-year assessment. Intensive Care Med. 2014, 40, 981–987. [Google Scholar] [CrossRef] [PubMed]
- Goldberger, Z.D.; Chan, P.S.; Berg, R.A.; Kronick, S.L.; Cooke, C.R.; Lu, M.; Banerjee, M.; Hayward, R.A.; Krumholz, H.M.; Nallamothu, B.K.; et al. Duration of resuscitation efforts and survival after in-hospital cardiac arrest: An observational study. Lancet 2012, 380, 1473–1481. [Google Scholar] [CrossRef] [Green Version]
- Oczkowski, S.J.; Mazzetti, I.; Cupido, C.; Fox-Robichaud, A.E. The offering of family presence during resuscitation: A systematic review and meta-analysis. J. Intensive Care 2015, 3, 41. [Google Scholar] [CrossRef] [Green Version]
- Toronto, C.E.; LaRocco, S.A. Family perception of and experience with family presence during cardiopulmonary resuscitation: An integrative review. J. Clin. Nurs. 2019, 28, 32–46. [Google Scholar] [CrossRef]
- Crowley, C.P.; Salciccioli, J.D.; Kim, E.Y. The association between ACLS guideline deviations and outcomes from in-hospital cardiac arrest. Resuscitation 2020, 153, 65–70. [Google Scholar] [CrossRef]
- Honarmand, K.; Mepham, C.; Ainsworth, C.; Khalid, Z. Adherence to advanced cardiovascular life support (ACLS) guidelines during in-hospital cardiac arrest is associated with improved outcomes. Resuscitation 2018, 129, 76–81. [Google Scholar] [CrossRef]

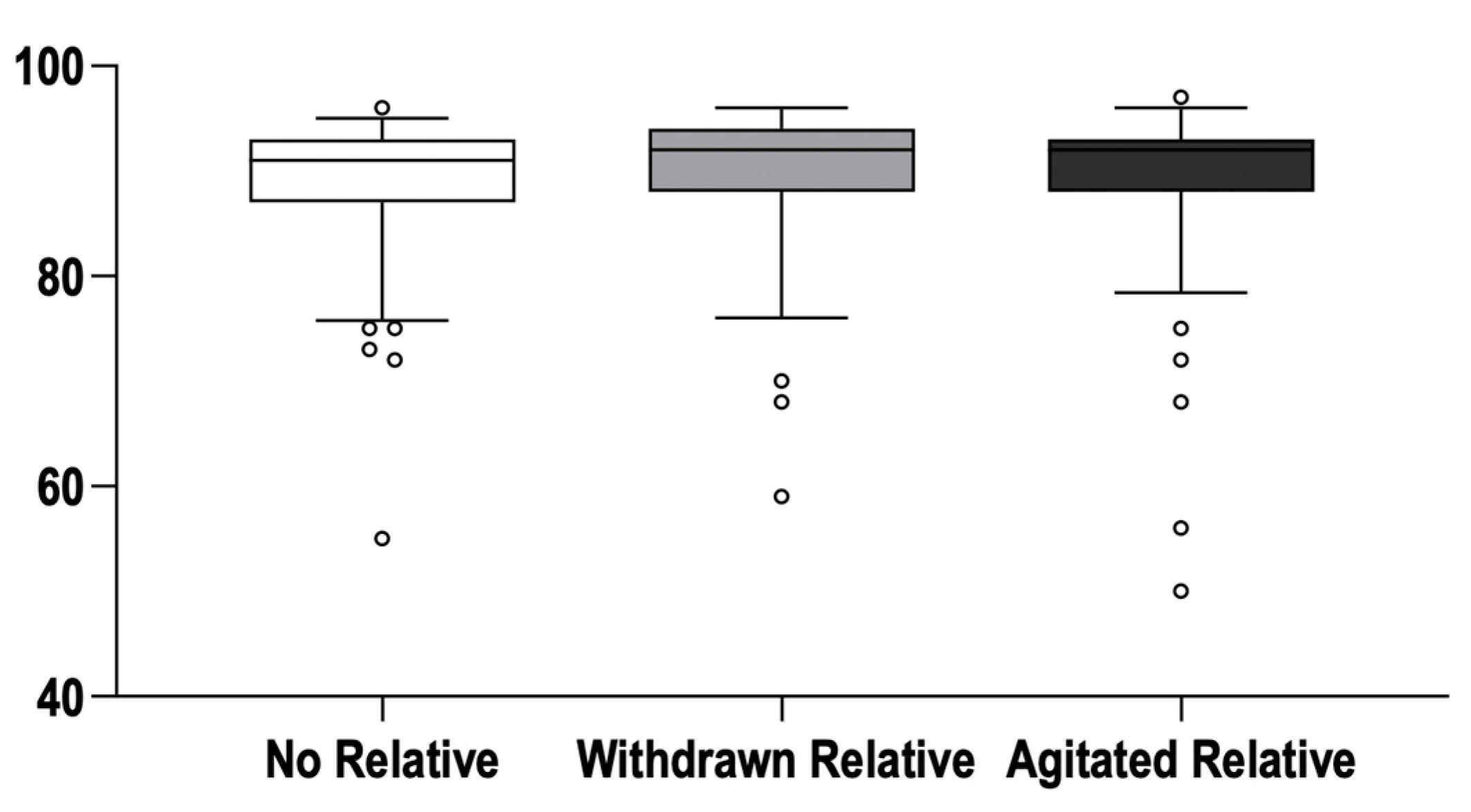
| No Relative (Control) (n = 113) | Withdrawn Relative (n = 105) | Agitated Relative (n = 117) | |
|---|---|---|---|
| Chest compression | |||
| Time interval to CPR start (s) | 14 [12–19] | 17 [13–21] | 18 [14–24] * |
| Start of CPR with CC (teams) | 112/113 | 102/105 | 114/117 |
| CC rates (strokes/min) | 118 [112–125] | 121 [112–126] | 120 [111–127] |
| CC < 100/min (teams) | 6/113 | 3/105 | 4/117 |
| Change-overs per 2 min CPR (n) | 1.4 [0.9–1.6] | 1.5 [1.0–1.8] | 1.3 [0.9–1.7] |
| Defibrillation | |||
| Time to 1st defibrillation (s) | 75 [55–102] | 71 [52–103] | 71 [53–106] |
| Shock with adequate (≥150 J) energy (teams) | 113/113 | 105/105 | 117/117 |
| VF not recognised ≥ once (teams) | 4/113 | 2/105 | 4/117 |
| Unsafe defibrillation ≥ once (teams) | 30/113 | 31/105 | 54/117 * |
| Airway Management | |||
| Advanced Airway Management (teams) | 111/113 | 100/105 | 111/117 |
| Time to Advanced Airway Management (s) | 142 [95–194] | 140 [111–205] | 150 [105–214] |
| Advance airway position confirmed by capnography (teams) | 89/111 | 85/100 | 90/111 |
| Ventilation rate (b/min) | 12 [4–10] | 13 [8–19] | 15 [10–20] * |
| Medication | |||
| Time to i.v. line insertion (s) | 112 [77–146] | 93 [66–132] | 111 [70–163] |
| Epinephrine administered (teams) | 80/113 | 68/105 | 71/111 |
| Correct dose (1 mg) administered (teams) | 80/80 | 68/68 | 71/71 |
| 2nd dose after 3–5 min (teams) | 2/6 | 0/6 | 2/5 |
| Amiodarone administered (teams) | 79/113 | 75/105 | 79/117 |
| Correct dose (300 mg) administered (teams) | 79/79 | 75/75 | 79/79 |
| Administered after epinephrine AND 3rd shock (teams) | 41/79 | 41/75 | 43/117 |
| False ACLS drug administered (teams) | 0/113 | 0/105 | 0/117 |
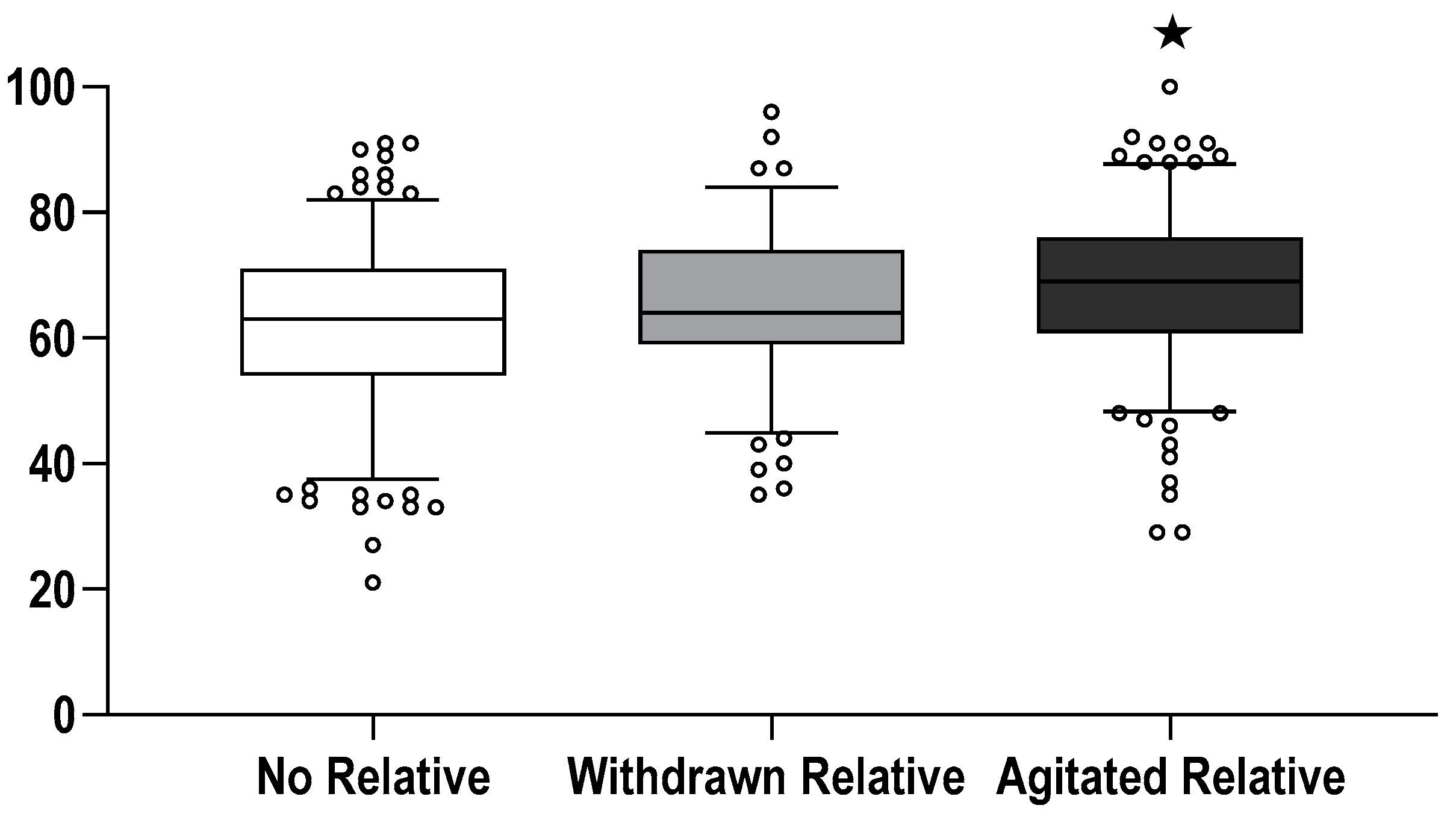
| No Relative (Control) (n = 407) | Withdrawn Relative (n = 403) | Agitated Relative (n = 419) | |
|---|---|---|---|
| Task Load | 63 [54–71] | 64 [59–73] | 69 [61–73] *,† |
| Mental demand | 70 [50–80] | 70 [55–85] | 75 [60–85] *,† |
| Physical demand | 50 [30–70] | 55 [40–75] | 55 [35–70] |
| Temporal demand | 70 [55–80] | 75 [60–90] * | 80 [65–90] * |
| Performance | 55 [35–70] | 55 [35–70] | 55 [35–70] |
| Effort | 65 [50–75] | 70 [55–75] * | 75 [60–85] *,† |
| Frustration | 50 [30–70] | 60 [45–75] * | 65 [45–80] *,† |
| Effect of Leadership Assignment | Effect of Relative Assignment | Interactive Term Leadership × Relative | |
|---|---|---|---|
| Chest compression | |||
| Hands-on time | 0.65 | 0.55 | 0.09 |
| Time interval to start of CPR | 0.46 | 0.015 | 0.92 |
| Start of CPR with massage | 0.99 | 0.99 | 0.92 |
| Chest compression rates | 0.70 | 0.34 | 0.83 |
| Compression rates < 100/min | 0.92 | 0.83 | 0.89 |
| Change-overs per 2 min CPR | 0.43 | 0.08 | 0.67 |
| Defibrillation | |||
| Time to 1st defibrillation | 0.38 | 0.52 | 0.017 |
| VF not recognised ≥ once | 0.99 | 0.99 | 0.98 |
| Unsafe defibrillation ≥ once | 0.31 | 0.03 | 0.62 |
| Airway Management | |||
| Advanced Airway Management | 0.99 | 0.99 | 0.82 |
| Time to Advanced Airway Management | 0.45 | 0.59 | 0.31 |
| Capnography to confirm airway position | 0.87 | 0.67 | 0.20 |
| Ventilation rate | 0.72 | 0.06 | 0.16 |
| Medication | |||
| Time to i.v. line insertion | 0.60 | 0.12 | 0.31 |
| Time to epinephrine administration | 0.46 | 0.12 | 0.60 |
| Epinephrine administered | 0.15 | 0.25 | 0.23 |
| Amiodarone administered | 0.46 | 0.79 | 0.36 |
| Administered after epinephrine AND 3rd shock | 0.25 | 0.82 | 0.94 |
| NASA Taskload | |||
| Task Load | 0.98 | 0.001 | 0.31 |
| Mental demand | 0.35 | 0.007 | 0.29 |
| Physical demand | 0.60 | 0.08 | 0.74 |
| Temporal demand | 0.48 | 0.001 | 0.30 |
| Performance | 0.20 | 0.65 | 0.003 |
| Effort | 0.46 | 0.001 | 0.30 |
| Frustration | 0.09 | 0.001 | 0.09 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sellmann, T.; Oendorf, A.; Wetzchewald, D.; Schwager, H.; Thal, S.C.; Marsch, S. The Impact of Withdrawn vs. Agitated Relatives during Resuscitation on Team Workload: A Single-Center Randomised Simulation-Based Study. J. Clin. Med. 2022, 11, 3163. https://doi.org/10.3390/jcm11113163
Sellmann T, Oendorf A, Wetzchewald D, Schwager H, Thal SC, Marsch S. The Impact of Withdrawn vs. Agitated Relatives during Resuscitation on Team Workload: A Single-Center Randomised Simulation-Based Study. Journal of Clinical Medicine. 2022; 11(11):3163. https://doi.org/10.3390/jcm11113163
Chicago/Turabian StyleSellmann, Timur, Andrea Oendorf, Dietmar Wetzchewald, Heidrun Schwager, Serge Christian Thal, and Stephan Marsch. 2022. "The Impact of Withdrawn vs. Agitated Relatives during Resuscitation on Team Workload: A Single-Center Randomised Simulation-Based Study" Journal of Clinical Medicine 11, no. 11: 3163. https://doi.org/10.3390/jcm11113163
APA StyleSellmann, T., Oendorf, A., Wetzchewald, D., Schwager, H., Thal, S. C., & Marsch, S. (2022). The Impact of Withdrawn vs. Agitated Relatives during Resuscitation on Team Workload: A Single-Center Randomised Simulation-Based Study. Journal of Clinical Medicine, 11(11), 3163. https://doi.org/10.3390/jcm11113163






