Photodynamic Therapy with 5-Aminolevulinic Acid Patch for the Treatment of Actinic Keratosis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Selection and Data Collection
2.2. Patients
2.3. Inclusion Criteria
2.4. Exclusion Criteria
2.5. Therapeutic Procedure
3. Review of the Current Literature
3.1. Studies on the Use of Self-Adhesive 5-Aminolevulinic Acid Patch for Actinic Keratosis
3.2. 5-Aminolevulinic Acid Patch for Actinic Cheilitis
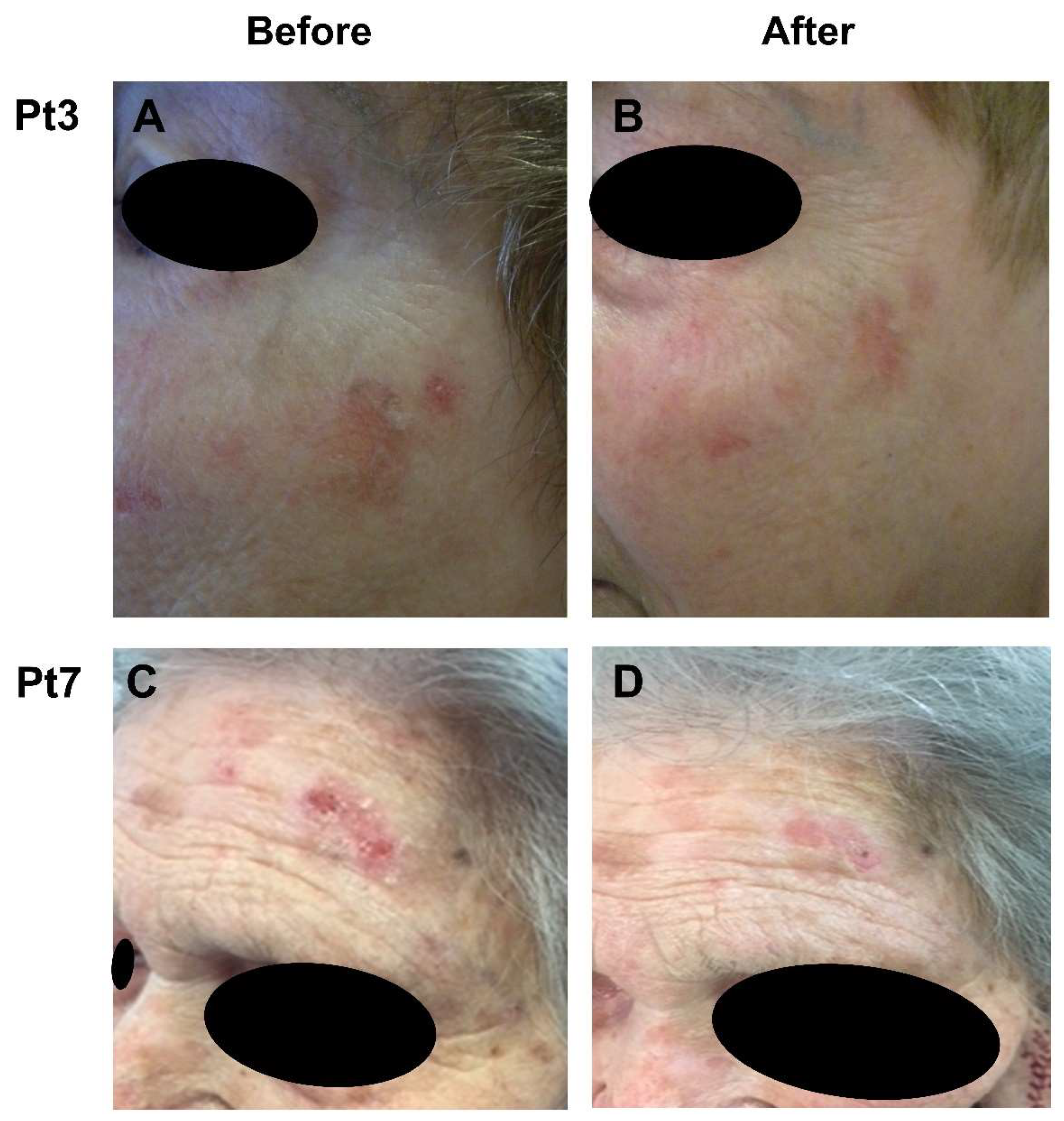
4. Results
5. Discussion
Advantages and Limitations
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Apalla, Z.; Lallas, A.; Sotiriou, E.; Lazaridou, E.; Ioannides, D. Epidemiological trends in skin cancer. Dermatol. Pract. Concept. 2017, 7, 1–6. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Morton, C.A.; Szeimies, R.M.; Sidoroff, A.; Braathen, L.R. European guidelines for topical photodynamic therapy part 1: Treatment delivery and current indications-actinic keratoses, Bowen’s disease, basal cell carcinoma. J. Eur. Acad. Dermatol. Venereol. 2013, 27, 536–544. [Google Scholar] [CrossRef]
- Figueras Nart, I.; Cerio, R.; Dirschka, T.; Dreno, B.; Lear, J.T.; Pellacani, G.; Peris, K.; Ruiz de Casas, A. Defining the actinic keratosis field: A literature review and discussion. J. Eur. Acad. Dermatol. Venereol. 2018, 32, 544–563. [Google Scholar] [CrossRef] [Green Version]
- de Berker, D.; McGregor, J.M.; Mohd Mustapa, M.F.; Exton, L.S.; Hughes, B.R. British Association of Dermatologists’ guidelines for the care of patients with actinic keratosis 2017. Br. J. Dermatol. 2017, 176, 20–43. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Radakovic, S.; Tanew, A. 5-aminolaevulinic acid patch-photodynamic therapy in the treatment of actinic cheilitis. Photodermatol. Photoimmunol. Photomed. 2017, 33, 306–310. [Google Scholar] [CrossRef] [PubMed]
- Kitajima, Y.; Ishii, T.; Kohda, T.; Ishizuka, M.; Yamazaki, K.; Nishimura, Y.; Tanaka, T.; Dan, S.; Nakajima, M. Mechanistic study of PpIX accumulation using the JFCR39 cell panel revealed a role for dynamin 2-mediated exocytosis. Sci. Rep. 2019, 9, 8666. [Google Scholar] [CrossRef] [Green Version]
- Tarstedt, M.; Gillstedt, M.; Wennberg Larko, A.M.; Paoli, J. Aminolevulinic acid and methyl aminolevulinate equally effective in topical photodynamic therapy for non-melanoma skin cancers. J. Eur. Acad. Dermatol. Venereol. 2016, 30, 420–423. [Google Scholar] [CrossRef]
- Gutierrez Garcia-Rodrigo, C.; Pellegrini, C.; Piccioni, A.; Maini, M.; Fargnoli, M.C. Long-term efficacy data for daylight-PDT. G. Ital. Dermatol. Venereol. 2018, 153, 800–805. [Google Scholar] [CrossRef]
- Zhu, L.; Wang, P.; Zhang, G.; Zhang, L.; Liu, X.; Hu, C.; Yang, X.; Sroka, R.; Zhou, Z.; Wang, X. Conventional versus daylight photodynamic therapy for actinic keratosis: A randomized and prospective study in China. Photodiagnosis Photodyn. Ther. 2018, 24, 366–371. [Google Scholar] [CrossRef]
- Salido-Vallejo, R.; Jiménez-Nájar, F.; Garnacho-Sucedo, G.; Vélez, A. Combined daylight and conventional photodynamic therapy with 5-aminolaevulinic acid nanoemulsion (BF-200 ALA) for actinic keratosis of the face and scalp: A new and efficient approach. Arch. Dermatol. Res. 2020, 312, 675–680. [Google Scholar] [CrossRef]
- Lieb, S.; Szeimies, R.M.; Lee, G. Self-adhesive thin films for topical delivery of 5-aminolevulinic acid. Eur. J. Pharm. Biopharm. 2002, 53, 99–106. [Google Scholar] [CrossRef]
- Fauteck, J.D.; Ackermann, G.; Birkel, M.; Breuer, M.; Moor, A.C.; Ebeling, A.; Ortland, C. Fluorescence characteristics and pharmacokinetic properties of a novel self-adhesive 5-ALA patch for photodynamic therapy of actinic keratoses. Arch. Dermatol. Res. 2008, 300, 53–60. [Google Scholar] [CrossRef] [PubMed]
- Szeimies, R.M.; Stockfleth, E.; Popp, G.; Borrosch, F.; Bruning, H.; Dominicus, R.; Mensing, H.; Reinhold, U.; Reich, K.; Moor, A.C.; et al. Long-term follow-up of photodynamic therapy with a self-adhesive 5-aminolaevulinic acid patch: 12 months data. Br. J. Dermatol. 2010, 162, 410–414. [Google Scholar] [CrossRef] [PubMed]
- Hauschild, A.; Popp, G.; Stockfleth, E.; Meyer, K.G.; Imberger, D.; Mohr, P.; Itschert, G.; Kaufmann, R.; Neuber, K.; Frambach, Y.; et al. Effective photodynamic therapy of actinic keratoses on the head and face with a novel, self-adhesive 5-aminolaevulinic acid patch. Exp. Dermatol. 2009, 18, 116–121. [Google Scholar] [CrossRef] [PubMed]
- Hauschild, A.; Stockfleth, E.; Popp, G.; Borrosch, F.; Bruning, H.; Dominicus, R.; Mensing, H.; Reinhold, U.; Reich, K.; Moor, A.C.; et al. Optimization of photodynamic therapy with a novel self-adhesive 5-aminolaevulinic acid patch: Results of two randomized controlled phase III studies. Br. J. Dermatol. 2009, 160, 1066–1074. [Google Scholar] [CrossRef]
- Braathen, L.R. Successful Daylight-PDT using a self-adhesive 5-aminolaevulinic acid patch. Eur. J. Dermatol. 2018, 28, 545. [Google Scholar] [CrossRef]
- Radakovic, S.; Dangl, M.; Tanew, A. 5-Aminolevulinic acid patch (Alacare) photodynamic therapy for actinic cheilitis: Data from a prospective 12-month follow-up study on 21 patients. J. Eur. Acad. Dermatol. Venereol. 2020, 34, 2011–2015. [Google Scholar] [CrossRef] [Green Version]
- Szeimies, R.M.; Hauschild, A.; Ortland, C.; Moor, A.C.; Stocker, M.; Surber, C. Photodynamic therapy simplified: Nonprepared, moderate-grade actinic keratosis lesions respond equally well to 5-aminolaevulinic acid patch photodynamic therapy as do mild lesions. Br. J. Dermatol. 2015, 173, 1277–1279. [Google Scholar] [CrossRef]
- Vegter, S.; Tolley, K. A network meta-analysis of the relative efficacy of treatments for actinic keratosis of the face or scalp in Europe. PLoS ONE 2014, 9, e96829. [Google Scholar] [CrossRef] [Green Version]
- Szeimies, R.M. A network meta-analysis of the relative efficacy of treatments for actinic keratosis of the face or scalp in Europe. J. Eur. Acad. Dermatol. Venereol. 2016, 30, 1619–1620. [Google Scholar] [CrossRef]
- Morton, C.A.; Szeimies, R.M.; Basset-Seguin, N.; Calzavara-Pinton, P.; Gilaberte, Y.; Haedersdal, M.; Hofbauer, G.F.L.; Hunger, R.E.; Karrer, S.; Piaserico, S.; et al. European Dermatology Forum guidelines on topical photodynamic therapy 2019 Part 1: Treatment delivery and established indications-actinic keratoses, Bowen’s disease and basal cell carcinomas. J. Eur. Acad. Dermatol. Venereol. 2019, 33, 2225–2238. [Google Scholar] [CrossRef] [PubMed]
- Gorelick, J.; Freeman, S. Aminolevulinic Acid 20% Solution Combined With Photodynamic Therapy for Treatment of Actinic Keratoses: A Review. J. Drugs Dermatol. 2021, 20, 1239–1244. [Google Scholar] [CrossRef] [PubMed]
- Morton, C.A.; Braathen, L.R. Daylight Photodynamic Therapy for Actinic Keratoses. Am. J. Clin. Dermatol. 2018, 19, 647–656. [Google Scholar] [CrossRef] [PubMed]
- Sharma, A.; Vincent, L. Actinic keratosis area and severity index is not correlated with photodynamic therapy procedural pain. Photodiagn. Photodyn. Ther. 2020, 31, 101946. [Google Scholar] [CrossRef]
| First Author (Study Year) | No. of Pt | No. of Lesions | Type of PDT (5-ALA Patch Application Time) | Follow-Up | Complete Clearance | Adverse Event | Pain | |
|---|---|---|---|---|---|---|---|---|
| Actinic keratosis | Hauschild et al. (2008) [14] | 140 | 520 | Conventional (0.5 h–1 h–2 h–4 h) | 8 weeks | 51%–72%–73%–86% | Mild to severe | Mild to severe |
| 34 | 130 | Conventional (4 h) | 8 weeks | 86% | Mild to severe | Mild to severe | ||
| Hauschild et al. (2009) [15] | 69 | 384 | Conventional (4 h) | 12 weeks | 82% | Mild or moderate | Mild or moderate 43% | |
| 148 | 750 | Conventional (4 h) | 12 weeks | 89% | Mild or moderate | Mild or moderate 35% | ||
| Szeimies et al. (2010) [13] | 174 | NR | Conventional (NR) | 12 months | 79% | NR | NR | |
| Braathen et al. (2018) [16] | 1 | 4 | Daylight (0.5 h) | 7 weeks | 75% | Mild | Absent | |
| Actinic cheilitis | Radakovic et al. (2017) [5] | 11 | 15 | Conventional (4 h) 2. PDT session in 8 lesions | 12 months | 66.6% | Moderate to severe | Mild to severe |
| Radakovic et al. (2020) [17] | 19 | NR | Conventional (4 h) | 12 months | 84% | Mild, moderate, severe | Mild to moderate |
| Case No. | Sex | Age (Years) | Fitzpatrick Skin Type | Location | No. of Lesions | Light | Adverse Event | Pain | Overall Tolerability | Clinical Response at 12 Weeks |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | M | 72 | Type III | Forehead, cheeks | 5 | Conventional | Moderate erythema | Mild | Good | CR |
| 2 | F | 76 | Type II | Forehead, temple, nose | 4 | Conventional | Mild erythema | Absent | Excellent | PR |
| 3 | F | 68 | Type II | Forehead, cheeks | 6 | Conventional | Moderate erythema | Mild | Excellent | CR |
| 4 | M | 69 | Type III | Cheeks | 6 | Conventional | Mild erythema | Mild | Excellent | CR |
| 5 | F | 71 | Type II | Forehead, nose | 4 | Conventional | Absent | Absent | Excellent | PR |
| 6 | M | 65 | Type II | Right side of the scalp | 4 | Conventional | Absent | Absent | Excellent | PR |
| 7 | F | 90 | Type II | Left forehead | 2 | Daylight | Absent | Mild | Good | PR |
| 8 | F | 78 | Type III | Nose, left cheek, right temple | 3 | Daylight | Absent | Mild | Excellent | PR |
| 9 | M | 83 | Type II | Scalp | 4 | Daylight | Absent | Absent | Excellent | PR |
| 10 | M | 63 | Type II | Nose, left cheek | 2 | Daylight | Absent | Mild | Good | PR |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kiss, N.; Farkas, K.; Tosti, G.; De Gado, F.; Bergler-Czop, B.; Fazia, G.; Tammaro, A.; Cantisani, C. Photodynamic Therapy with 5-Aminolevulinic Acid Patch for the Treatment of Actinic Keratosis. J. Clin. Med. 2022, 11, 3164. https://doi.org/10.3390/jcm11113164
Kiss N, Farkas K, Tosti G, De Gado F, Bergler-Czop B, Fazia G, Tammaro A, Cantisani C. Photodynamic Therapy with 5-Aminolevulinic Acid Patch for the Treatment of Actinic Keratosis. Journal of Clinical Medicine. 2022; 11(11):3164. https://doi.org/10.3390/jcm11113164
Chicago/Turabian StyleKiss, Norbert, Klára Farkas, Giulio Tosti, Federico De Gado, Beata Bergler-Czop, Gilda Fazia, Antonella Tammaro, and Carmen Cantisani. 2022. "Photodynamic Therapy with 5-Aminolevulinic Acid Patch for the Treatment of Actinic Keratosis" Journal of Clinical Medicine 11, no. 11: 3164. https://doi.org/10.3390/jcm11113164
APA StyleKiss, N., Farkas, K., Tosti, G., De Gado, F., Bergler-Czop, B., Fazia, G., Tammaro, A., & Cantisani, C. (2022). Photodynamic Therapy with 5-Aminolevulinic Acid Patch for the Treatment of Actinic Keratosis. Journal of Clinical Medicine, 11(11), 3164. https://doi.org/10.3390/jcm11113164








