Clinical Update Findings about pH-Impedance Monitoring Features in Laryngopharyngeal Reflux Patients
Abstract
:1. Introduction
2. Epidemiology
3. Diagnosis of Reflux and Place of pH Study
3.1. Clinical Diagnosis and Importance of pH Study
3.2. Place, Indications, and Features of pH Study
3.3. Single, Dual-, or Triple-Probe Esophageal pH Monitoring
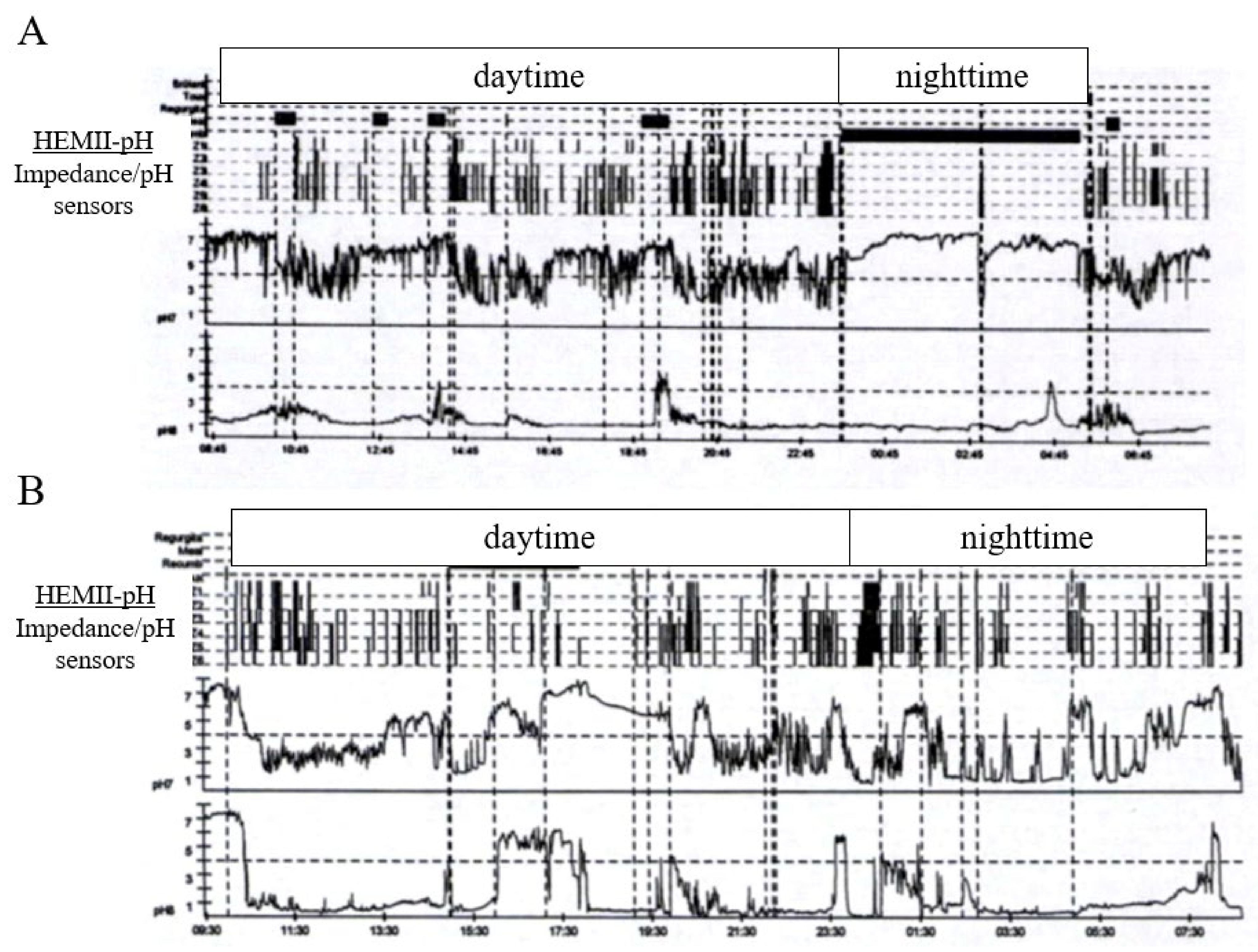
3.4. Multichannel Intraluminal Impedance–pH Monitoring
| Hypopharyngeal Reflux Event Definition and Features | References |
|---|---|
| 1. Episode reaching proximally to 1 cm above the upper border of UES (with decreased impedance). | [39,40] |
| 2. Episode reaching proximally to 0.5 cm above the upper border of UES (with decreased impedance). | [41] |
| 3. Retrograde 50% drop in impedance starting distally (UES) and reaching the more proximal impedance site. HRE event was considered only if it was preceded by retrograde impedance drop both distally and proximally within the esophagus and if no swallow occurred during the pharyngeal impedance drop. | [42] |
| 4. Episode when the time of pH reaching to the lowest point was no more than 30 s (Restech). | [43] |
| 5. Reflux reaching Z1 Z2 (hypopharyngeal) impedance segment. | [44,45] |
| 6. Episode reaching oropharyngeal sensor. | [46,47,48,49] |
| Outcomes | Definition and Features | References |
|---|---|---|
| Reflux Event Composition | ||
| Gas HRE | 1. Simultaneous increase in impedance of >3000 W in any two consecutive impedance sites with one site with an absolute value >7000 W in the absence of swallowing. | [39,40,41,42,44,45,50,51,52] |
| 2. Abrupt increase of impedance by ≥50% in two adjacent channels with simultaneous or near-simultaneous propagation in the retrograde direction. | [53] | |
| Liquid HRE | 1. Retrograde 50% drop in impedance starting distally (LES) and propagating at least to the next two or more proximal impedance measuring segments. | [39,40,41,42,44,45,50,51,53] |
| 2. Retrograde moving 40% fall in impedance in two distal impedance sites. | [52] | |
| Mixed HRE | 1. Gas reflux occurring immediately before or during a liquid reflux. | [39,40,41,42,45,50] |
| 2. Combination of the gas reflux and liquid reflux patterns. | [44,53] | |
| 3. <50% fall in impedance of resting impedance (liquid) preceded or followed by an abrupt rise in impedance (gas). | [51] | |
| Reflux Event Types | ||
| Acid HRE/PRE | 1. Hypopharyngeal or proximal esophageal event with pH < 4. | [39,40,44,50] |
| 2. Hypopharyngeal and proximal esophageal events with pH < 4. | [41] | |
| 3. Drop/event in pH < 4 for at least 5 s in the proximal esophagus. | [52,53] | |
| 4. Drop/event in pH < 4.0 from a pre-event pH > 4.0 units lasting for >5 s. | [40,51] | |
| Superimposed acid PRE | 1. Reflux event while pH < 4 during an acid clearing interval. | [50] |
| 2. Liquid reflux monitored by impedance electrodes while esophageal pH is still <4.0. | [40,51] | |
| Weakly acid HRE/PRE | 1. Hypopharyngeal or proximal esophageal pH 4–7. | [39,40,50,51] |
| 2. Hypopharyngeal and proximal esophageal pH > 4. | [41] | |
| 3. Decrease of more than 1 pH unit with a nadir pH above 4. | [53] | |
| Nonacid HRE/PRE (Weakly alkaline) | 1. Hypopharyngeal or proximal esophageal pH > 7. | [39,40,41,50] |
| 2. No change of pH or a decrease of less than 1 pH unit. | [53] | |
| 3. Hypopharyngeal or proximal esophageal pH > 4. | [44] | |
| 4. Hypopharyngeal or proximal esophageal pH ≥ 7.0. | [40,51] | |
3.5. Oropharyngeal pH Monitoring
3.6. Placement and Technical Point
4. Perspective of pH Study in Otolaryngology
5. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Lechien, J.R.; Akst, L.M.; Hamdan, A.L.; Schindler, A.; Karkos, P.D.; Barillari, M.R.; Calvo-Henriquez, C.; Crevier-Buchman, L.; Finck, C.; Eun, Y.G.; et al. Evaluation and Management of Laryngopharyngeal Reflux Disease: State of the Art Review. Otolaryngol. Head Neck Surg. 2019, 160, 762–782. [Google Scholar] [CrossRef] [PubMed]
- Sikavi, D.R.; Cai, J.X.; Leung, R.; Carroll, T.L.; Chan, W.W. Impaired Proximal Esophageal Contractility Predicts Pharyngeal Reflux in Patients With Laryngopharyngeal Reflux Symptoms. Clin. Transl. Gastroenterol. 2021, 12, e00408. [Google Scholar] [CrossRef]
- Karkos, P.D.; Benton, J.; Leong, S.C.; Karkanevatos, A.; Badran, K.; Srinivasan, V.R.; Temple, R.H.; Issing, W.J. Trends in laryngopharyngeal reflux: A British ENT survey. Eur. Arch. Otorhinolaryngol. 2007, 264, 513–517. [Google Scholar] [CrossRef] [PubMed]
- Spantideas, N.; Drosou, E.; Bougea, A.; Assimakopoulos, D. Laryngopharyngeal reflux disease in the Greek general population, prevalence and risk factors. BMC Ear Nose Throat Disord. 2015, 15, 7. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kamani, T.; Penney, S.; Mitra, I.; Pothula, V. The prevalence of laryngopharyngeal reflux in the English population. Eur. Arch. Otorhinolaryngol. 2012, 269, 2219–2225. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.M.; Li, Y.; Guo, W.L.; Wang, W.T.; Lu, M. Prevalence of laryngopharyngeal reflux disease in Fuzhou region of China. Zhonghua Er Bi Yan Hou Tou Jing Wai Ke Za Zhi 2016, 51, 909–913. [Google Scholar] [PubMed]
- Connor, N.P.; Palazzi-Churas, K.L.; Cohen, S.B.; Leverson, G.E.; Bless, D.M. Symptoms of extraesophageal reflux in a community—Dwelling sample. J. Voice 2007, 21, 189–202. [Google Scholar] [CrossRef]
- Hamdan, A.L.; Daou, C.A.Z.; Nawfal, N.; Lechien, J.R. Prevalence of Laryngopharyngeal Reflux Related Symptoms in Patients with Allergy. J. Voice 2022, S0892-1997(21)00420-3. [Google Scholar] [CrossRef]
- Eren, E.; Arslanoğlu, S.; Aktaş, A.; Kopar, A.; Ciğer, E.; Önal, K.; Katılmiş, H. Factors confusing the diagnosis of laryngopharyngeal reflux: The role of allergic rhinitis and inter-rater variability of laryngeal findings. Eur. Arch. Otorhinolaryngol. 2014, 271, 743–747. [Google Scholar] [CrossRef]
- Randhawa, P.S.; Mansuri, S.; Rubin, J.S. Is dysphonia due to allergic laryngitis being misdiagnosed as laryngopharyngeal reflux? Logoped. Phoniatr. Vocol. 2010, 35, 1–5. [Google Scholar] [CrossRef]
- Ren, J.; Zhao, Y.; Wang, J.; Ren, X.; Xu, Y.; Tang, W.; He, Z. PepsinA as a Marker of Laryngopharyngeal Reflux Detected in Chronic Rhinosinusitis Patients. Otolaryngol. Head Neck Surg. 2017, 156, 893–900. [Google Scholar] [CrossRef] [PubMed]
- Lechien, J.R.; Bock, J.M.; Carroll, T.L.; Akst, L.M. Is empirical treatment a reasonable strategy for laryngopharyngeal reflux? A contemporary review. Clin. Otolaryngol. 2020, 45, 450–458. [Google Scholar] [CrossRef] [PubMed]
- Belafsky, P.C.; Postma, G.N.; Koufman, J.A. Validity and reliability of the reflux symptom index (RSI). J. Voice 2002, 16, 274–277. [Google Scholar] [CrossRef]
- Lechien, J.R.; Bobin, F.; Muls, V.; Thill, M.P.; Horoi, M.; Ostermann, K.; Huet, K.; Harmegnies, B.; Dequanter, D.; Dapri, G.; et al. Validity and reliability of the reflux symptom score. Laryngoscope 2020, 130, E98–E107. [Google Scholar] [CrossRef] [PubMed]
- Belafsky, P.C.; Postma, G.N.; Koufman, J.A. The validity and reliability of the reflux finding score (RFS). Laryngoscope 2001, 111, 1313–1317. [Google Scholar] [CrossRef]
- Lechien, J.R.; Rodriguez Ruiz, A.; Dequanter, D.; Bobin, F.; Mouawad, F.; Muls, V.; Huet, K.; Harmegnies, B.; Remacle, S.; Finck, C.; et al. Validity and Reliability of the Reflux Sign Assessment. Ann. Otol. Rhinol. Laryngol. 2020, 129, 313–325. [Google Scholar] [CrossRef] [PubMed]
- Francis, D.O.; Patel, D.A.; Sharda, R.; Hovis, K.; Sathe, N.; Penson, D.F.; Feurer, I.D.; McPheeters, M.L.; Vaezi, M.F. Patient-Reported Outcome Measures Related to Laryngopharyngeal Reflux: A Systematic Review of Instrument Development and Validation. Otolaryngol. Head Neck Surg. 2016, 155, 923–935. [Google Scholar] [CrossRef] [Green Version]
- Lechien, J.R.; Muls, V.; Dapri, G.; Mouawad, F.; Eisendrath, P.; Schindler, A.; Nacci, A.; Barillari, M.R.; Finck, C.; Saussez, S.; et al. The management of suspected or confirmed laryngopharyngeal reflux patients with recalcitrant symptoms: A contemporary review. Clin. Otolaryngol. 2019, 44, 784–800. [Google Scholar] [CrossRef]
- Lechien, J.R.; Saussez, S.; Schindler, A.; Karkos, P.D.; Hamdan, A.L.; Harmegnies, B.; De Marrez, L.G.; Finck, C.; Journe, F.; Paesmans, M.; et al. Clinical outcomes of laryngopharyngeal reflux treatment: A systematic review and meta-analysis. Laryngoscope 2019, 129, 1174–1187. [Google Scholar] [CrossRef]
- De Vore, E.K.; Chan, W.W.; Shin, J.J.; Carroll, T.L. Does the Reflux Symptom Index Predict Increased Pharyngeal Events on HEMII-pH Testing and Correlate with General Quality of Life? J. Voice 2021, 35, 625–632. [Google Scholar] [CrossRef]
- Kim, S.I.; Jeong, S.J.; Kwon, O.E.; Park, J.M.; Lee, Y.C.; Eun, Y.G.; Ko, S.G. 24-Hour Multichannel Intraluminal Impedance-pH in Proton Pump Inhibitor Nonresponders vs Responders in Patients With Laryngopharyngeal Reflux. Otolaryngol. Head Neck Surg. 2022, 166, 910–916. [Google Scholar] [CrossRef] [PubMed]
- Lechien, J.R.; Bobin, F.; Dapri, G.; Eisendrath, P.; Salem, C.; Mouawad, F.; Horoi, M.; Thill, M.P.; Dequanter, D.; Rodriguez, A.; et al. Hypopharyngeal-Esophageal Impedance-pH Monitoring Profiles of Laryngopharyngeal Reflux Patients. Laryngoscope 2021, 131, 268–276. [Google Scholar] [CrossRef] [PubMed]
- Lechien, J.R.; Allen, J.E.; Barillari, M.R.; Karkos, P.D.; Jia, H.; Ceccon, F.P.; Imamura, R.; Metwaly, O.; Chiesa-Estomba, C.M.; Bock, J.M.; et al. Management of Laryngopharyngeal Reflux Around the World: An International Study. Laryngoscope 2021, 131, E1589–E1597. [Google Scholar] [CrossRef] [PubMed]
- Lechien, J.R.; Carroll, T.L.; Allen, J.E.; Ayad, T.; Enver, N.; Eun, Y.G.; Perazzo, P.S.; Ceccon, F.P.; Sant’Anna, G.D.; Imamura, R.; et al. Impact of subspecialty training on management of laryngopharyngeal reflux: Results of a worldwide survey. Eur. Arch. Otorhinolaryngol. 2021, 278, 1933–1943. [Google Scholar] [CrossRef]
- Lechien, J.R.; Hans, S.; Calvo-Henriquez, C.; Baudouin, R.; Saussez, S. Laryngopharyngeal Reflux may be Acute, Recurrent or Chronic Disease: Preliminary Observations. Eur. Arch. Otorhinolaryngol. 2022. Online ahead of print. [Google Scholar] [CrossRef]
- Koufman, J.A. The otolaryngologic manifestations of gastroesophageal reflux disease (GERD): A clinical investigation of 225 patients using ambulatory 24-hour pH monitoring and an experimental investigation of the role of acid and pepsin in the development of laryngeal injury. Laryngoscope 1991, 101 (Suppl. S53), 1–78. [Google Scholar]
- Pisegna, J.M.; Yang, S.; Purcell, A.; Rubio, A. A Mixed-Methods Study of Patient Views on Reflux Symptoms and Medication Routines. J. Voice 2017, 31, 381.e15–381.e25. [Google Scholar] [CrossRef]
- De Bortoli, N.; Nacci, A.; Savarino, E.; Martinucci, I.; Bellini, M.; Fattori, B.; Ceccarelli, L.; Costa, F.; Mumolo, M.G.; Ricchiuti, A.; et al. How many cases of laryngopharyngeal reflux suspected by laryngoscopy are gastroesophageal reflux disease-related? World J. Gastroenterol. 2012, 18, 4363–4370. [Google Scholar] [CrossRef]
- Jamieson, J.R.; Stein, H.J.; DeMeester, T.R.; Bonavina, L.; Schwizer, W.; Hinder, R.A.; Albertucci, M. Ambulatory 24-h esophageal pH monitoring: Normal values, optimal thresholds, specificity, sensitivity, and reproducibility. Am. J. Gastroenterol. 1992, 87, 1102–1111. [Google Scholar]
- Wahba, G.; Neshkova, E.; Jutras, G.; Liu Chen Kiow, J.; Clément, M.; Willems, P.; Eouani, B.D.; Courbette, O.; Ayuso, É.; Bouin, M. Lidocaine before esophageal manometry and ambulatory pH monitoring: A randomized controlled trial. Neurogastroenterol. Motil. 2021, 33, e14167. [Google Scholar] [CrossRef]
- Muderris, T.; Gokcan, M.K.; Yorulmaz, I. The clinical value of pharyngeal pH monitoring using a double-probe, triple-sensor catheter in patients with laryngopharyngeal reflux. Arch. Otolaryngol. Head Neck Surg. 2009, 135, 163–167. [Google Scholar] [CrossRef] [Green Version]
- Lechien, J.R.; Bobin, F.; Muls, V.; Mouawad, F.; Dequanter, D.; Horoi, M.; Thill, M.P.; Rodriguez Ruiz, A.; Saussez, S. The efficacy of a personalised treatment depending on the characteristics of reflux at multichannel intraluminal impedance-pH monitoring in patients with acid, non-acid and mixed laryngopharyngeal reflux. Clin. Otolaryngol. 2021, 46, 602–613. [Google Scholar] [CrossRef] [PubMed]
- Koufman, J.; Sataloff, R.T.; Toohill, R. Laryngopharyngeal reflux: Consensus conference report. J. Voice 1996, 10, 215–216. [Google Scholar] [CrossRef]
- Harrell, S.; Evans, B.; Goudy, S.; Winstead, W.; Lentsch, E.; Koopman, J.; Wo, J.M. Design and implementation of an ambulatory pH monitoring protocol in patients with suspected laryngopharyngeal reflux. Laryngoscope 2005, 115, 89–92. [Google Scholar] [CrossRef] [PubMed]
- Maldonado, A.; Diederich, L.; Castell, D.O.; Gideon, R.M.; Katz, P.O. Laryngopharyngeal reflux identified using a new catheter design: Defining normal values and excluding artifacts. Laryngoscope 2003, 113, 349–355. [Google Scholar] [CrossRef] [PubMed]
- Postma, G.N. Ambulatory pH monitoring methodology. Ann. Otol. Rhinol. Laryngol. Suppl. 2000, 184, 10–14. [Google Scholar] [CrossRef] [PubMed]
- Lechien, J.R.; Chan, W.W.; Akst, L.M.; Hoppo, T.; Jobe, B.A.; Chiesa-Estomba, C.M.; Muls, V.; Bobin, F.; Saussez, S.; Carroll, T.L.; et al. Normative Ambulatory Reflux Monitoring Metrics for Laryngopharyngeal Reflux: A Systematic Review of 720 Healthy Individuals. Otolaryngol. Head Neck Surg. 2022, 166, 1945998211029831. [Google Scholar] [CrossRef]
- Kim, S.I.; Jeong, S.J.; Kwon, O.E.; Park, J.M.; Doo, J.G.; Park, S.I.; Kim, B.H.; Lee, Y.C.; Eun, Y.G.; Ko, S.G. Pharyngeal reflux episodes in patients with suspected laryngopharyngealreflux versus healthy subjects: A prospective cohort study. Eur. Arch. Otorhinolaryngol. 2021, 278, 3387–3392. [Google Scholar] [CrossRef]
- Wang, A.J.; Liang, M.J.; Jiang, A.Y.; Lin, J.K.; Xiao, Y.L.; Peng, S.; Chen, J.; Wen, W.P.; Chen, M.H. Gastroesophageal and laryngopharyngeal reflux detected by 24-hour combined impedance and pH monitoring in healthy Chinese volunteers. J. Dig. Dis. 2011, 12, 173–180. [Google Scholar] [CrossRef]
- Xiao, Y.L.; Liu, F.Q.; Li, J.; Lv, J.T.; Lin, J.K.; Wen, W.P.; Chen, M.H. Gastroesophageal and laryngopharyngeal reflux profiles in patients with obstructive sleep apnea/hypopnea syndrome as determined by combined multichannel intraluminal impedance-pH monitoring. Neurogastroenterol. Motil. 2012, 24, e258–e265. [Google Scholar] [CrossRef]
- Hoppo, T.; Sanz, A.F.; Nason, K.S.; Carroll, T.L.; Rosen, C.; Normolle, D.P.; Shaheen, N.J.; Luketich, J.D.; Jobe, B.A. How much pharyngeal exposure is “normal”? Normative data for laryngopharyngeal reflux events using hypopharyngeal multichannel intraluminal impedance (HMII). J. Gastrointest Surg. 2012, 16, 16–24, discussion 24–25. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Desjardin, M.; Roman, S.; des Varannes, S.B.; Gourcerol, G.; Coffin, B.; Ropert, A.; Mion, F.; Zerbib, F. Pharyngeal pH alone is not reliable for the detection of pharyngeal refluxevents: A study with oesophageal and pharyngeal pH-impedance monitoring. United Eur. Gastroenterol. J. 2013, 1, 438–444. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Feng, G.; Wang, J.; Zhang, L.; Liu, Y. A Study to Draw a Normative Database of Laryngopharynx pH Profile in Chinese. J. Neurogastroenterol. Motil. 2014, 20, 347–351. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hou, C.; Chen, M.; Chen, T.; Yang, Y.; Yang, X.; Lin, Z.; Zeng, Y.; Chen, L.; Liu, C. Study on laryngopharyngeal and esophageal reflux characteristics using 24-h multichannel intraluminal impedance-pH monitoring in healthy volunteers. Eur. Arch. Otorhinolaryngol. 2020, 277, 2801–2811. [Google Scholar] [CrossRef]
- Doo, J.G.; Kim, S.I.; Park, J.M.; Kwon, O.E.; Lee, Y.C.; Eun, Y.G. Changes in Pharyngeal Baseline Impedance in Patients With Laryngopharyngeal Reflux. Otolaryngol. Head Neck Surg. 2020, 163, 194599820918820. [Google Scholar] [CrossRef]
- Sun, G.; Muddana, S.; Slaughter, J.C.; Casey, S.; Hill, E.; Farrokhi, F.; Garrett, C.G.; Vaezi, M.F. A new pH catheter for laryngopharyngeal reflux: Normal values. Laryngoscope 2009, 119, 1639–1643. [Google Scholar] [CrossRef]
- Yadlapati, R.; Adkins, C.; Jaiyeola, D.-M.; Lidder, A.K.; Gawron, A.J.; Tan, B.K.; Shabeeb, N.; Price, C.P.; Agrawal, N.; Ellenbogen, M.; et al. Abilities of Oropharyngeal pH Tests and Salivary Pepsin Analysis to Discriminate Between Asymptomatic Volunteers and Subjects With Symptoms of Laryngeal Irritation. Clin. Gastroenterol. Hepatol. 2016, 14, 535–542.e2. [Google Scholar] [CrossRef] [Green Version]
- Ayazi, S.; Lipham, J.C.; Hagen, J.A.; Tang, A.L.; Zehetner, J.; Leers, J.M.; Oezcelik, A.; Abate, E.; Banki, F.; Demeester, S.R. A new technique for measurement of pharyngeal pH: Normal values and discriminating pH threshold. J. Gastrointest. Surg. 2009, 13, 1422–1429. [Google Scholar] [CrossRef]
- Chheda, N.N.; Seybt, M.W.; Schade, R.R.; Postma, G.N. Normal values for pharyngeal pH monitoring. Ann. Otol. Rhinol. Laryngol. 2009, 118, 166–171. [Google Scholar] [CrossRef]
- Shay, S.S.; Tutuian, R.; Sifrim, D.; Vela, M.F.; Wise, J.L.; Balaji, N.S.; Zhang, X.; Adhami, T.; Murray, J.; Peters, J.H.; et al. Twenty-four hour ambulatory simultaneous impedance and pH monitoring: A multicenter report of normal values from 60 healthy volunteers. Am. J. Gastroenterol. 2004, 99, 1037–1043. [Google Scholar] [CrossRef]
- Zentilin, P.; Iiritano, E.; Dulbecco, P.; Bilardi, C.; Savarino, E.; De Conca, S.; Parodi, A.; Reglioni, S.; Vigneri, S. Normal values of 24-h ambulatory intraluminal impedance combined with pH-metry in subjects eating a Mediterranean diet. Dig. Liver Dis. 2006, 38, 226–232. [Google Scholar] [CrossRef] [PubMed]
- Jetté, M.E.; Gaumnitz, E.A.; Birchall, M.A.; Welham, N.V.; Thibeault, S.L. Correlation between Reflux and multichannel intraluminal impedance pH monitoring in untreated volunteers. Laryngoscope 2014, 124, 2345–2351. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kawamura, O.; Kohata, Y.; Kawami, N.; Iida, H.; Kawada, A.; Hosaka, H.; Shimoyama, Y.; Kuribayashi, S.; Fujiwara, Y.; Iwakiri, K.; et al. Liquid-containing Refluxes and Acid Refluxes May Be Less Frequent in the Japanese Population Than in Other Populations: Normal Values of 24- hour Esophageal Impedance and pH Monitoring. J. Neurogastroenterol. Motil. 2016, 22, 620–629. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sikavi, D.R.; Cai, J.X.; Carroll, T.L.; Chan, W.W. Prevalence and clinical significance of esophageal motility disorders in patients with laryngopharyngeal reflux symptoms. J. Gastroenterol. Hepatol. 2021, 36, 2076–2082. [Google Scholar] [CrossRef]
- Lechien, J.R.; Bobin, F.; Muls, V.; Eisendrath, P.; Horoi, M.; Thill, M.P.; Dequanter, D.; Durdurez, J.P.; Rodriguez, A.; Saussez, S. Gastroesophageal reflux in laryngopharyngeal reflux patients: Clinical features and therapeutic response. Laryngoscope 2020, 130, E479–E489. [Google Scholar] [CrossRef]
- Han, H.; Lyu, Q.; Liang, Y. Different Characteristics of Oropharyngeal pH Changes in Different Laryngeal Diseases. Ear Nose Throat J. 2022, 1455613221081568. [Google Scholar] [CrossRef]
- Waxman, J.; Yalamanchali, S.; Valle, E.S.; Pott, T.; Friedman, M. Effects of Proton Pump Inhibitor Therapy for Laryngopharyngeal Reflux on Post-treatment Symptoms and Hypopharyngeal pH. Otolaryngol. Head Neck Surg. 2014, 150, 1010–1017. [Google Scholar] [CrossRef]
- Vance, D.; Park, J.; Alnouri, G.; Turner, R.R.; Daggumati, S.; Ferster, A.P.O.; Ahmad, A.; Lyons, K.; Ross, J.; Russell, K.; et al. Diagnosing Laryngopharyngeal Reflux: A Comparison between 24-hour pH-Impedance Testing and Pharyngeal Probe (Restech) Testing, with Introduction of the Sataloff Score. J. Voice 2021, S0892-1997(21)00136-3. [Google Scholar] [CrossRef]
- Wang, J.Y.; Peng, T.; Zhao, L.L.; Feng, G.J.; Liu, Y.L. Poor consistency between reflux symptom index and laryngopharyngeal pH monitoring in laryngopharyngeal reflux diagnosis in Chinese population. Ann. Transl. Med. 2021, 9, 25. [Google Scholar] [CrossRef]
- Bobin, F.; Journe, F.; Lechien, J.R. Saliva pepsin level of laryngopharyngeal reflux patients is not correlated with reflux episodes. Laryngoscope 2020, 130, 1278–1281. [Google Scholar] [CrossRef]
- Lechien, J.R.; De Vos, N.; Everard, A.; Saussez, S. Laryngopharyngeal reflux: The microbiota theory. Med. Hypotheses 2021, 146, 110460. [Google Scholar] [CrossRef] [PubMed]
- Bobin, F.; Saussez, S.; Lechien, J.R. Otolaryngological complications of hypopharyngeal-esophageal multichannel intraluminal impedance-pH monitoring. Clin. Case Rep. 2020, 8, 2634–2637. [Google Scholar] [CrossRef] [PubMed]
- Kang, H.J.; Park, J.M.; Choi, S.Y.; Kim, S.I.; Lee, Y.C.; Eun, Y.G.; Ko, S.G. Comparison Between Manual and Automated Analyses in Multichannel Intraluminal Impedance: pH Monitoring for Laryngopharyngeal Reflux. Otolaryngol. Head Neck Surg. 2022, 166, 128–132. [Google Scholar] [CrossRef] [PubMed]
- Samuels, T.L.; Khampang, P.; Espahbodi, M.; McCormick, C.A.; Chun, R.H.; McCormick, M.E.; Yan, K.; Kerschner, J.E.; Johnston, N. Association of Pepsin With Inflammatory Signaling and Effusion Viscosity in Pediatric Otitis Media. Laryngoscope 2022, 132, 470–477. [Google Scholar] [CrossRef]
- Lechien, J.R.; Hans, S.; Simon, F.; Horoi, M.; Calvo-Henriquez, C.; Chiesa-Estomba, C.M.; Mayo-Yáñez, M.; Bartel, R.; Piersiala, K.; Nguyen, Y.; et al. Association Between Laryngopharyngeal Reflux and Media Otitis: A Systematic Review. Otol. Neurotol. 2021, 42, e801–e814. [Google Scholar] [CrossRef]
- Lechien, J.R.; Saussez, S.; Hopkins, C. Association between Laryngopharyngeal Reflux, Gastroesophageal Reflux and Recalcitrant Chronic Rhinosinusitis: A Systematic Review. Otolaryngol. Head Neck Surg. 2022, 83, 356–363. [Google Scholar]
- Lechien, J.R.; Saussez, S.; Nacci, A.; Barillari, M.R.; Rodriguez, A.; Le Bon, S.D.; Crevier-Buchman, L.; Harmegnies, B.; Finck, C.; Akst, L.M. Association between laryngopharyngeal reflux and benign vocal folds lesions: A systematic review. Laryngoscope 2019, 129, E329–E341. [Google Scholar] [CrossRef]
- Chen, Y.L.; Bao, Y.Y.; Zhou, S.H.; Yao, H.T.; Chen, Z. Relationship Between Pepsin Expression and Dysplasia Grade in Patients With Vocal Cord Leukoplakia. Otolaryngol. Head Neck Surg. 2021, 164, 160–165. [Google Scholar] [CrossRef]
- Lechien, J.R.; Akst, L.M.; Saussez, S.; Crevier-Buchman, L.; Hans, S.; Barillari, M.R.; Calvo-Henriquez, C.; Bock, J.M.; Carroll, T.L. Involvement of Laryngopharyngeal Reflux in Select Nonfunctional Laryngeal Diseases: A Systematic Review. Otolaryngol. Head Neck Surg. 2021, 164, 37–48. [Google Scholar] [CrossRef]
- Ding, L.; Lv, T.; Lou, Z. The recurrent factors of idiopathic vocal process granulomas after cold steel excision. Am. J. Otolaryngol. 2022, 43, 103454. [Google Scholar] [CrossRef]
- Yan, S.; Feng, Y.; Yao, L. Analysis of effects of laryngopharyngeal reflux disease and proton pump inhibitor treatment on Eustachian tube function in patients with obstructive sleep apnea hypopnea. Ear Nose Throat J. 2022, 1455613221076786. [Google Scholar] [CrossRef]
- Mayo-Yáñez, M.; Viña-Vázquez, S.; Lechien, J.R.; Chiesa-Estomba, C.M.; Calvo-Henríquez, C.; González-Torres, L. Involvement of Laryngopharyngeal Reflux in Ocular Diseases: A State-of-the-Art Review. J. Voice 2021, S0892-1997(21)00106-5. [Google Scholar] [CrossRef] [PubMed]
- Hamizan, A.W.; Choo, Y.Y.; Loh, P.V.; Abd Talib, N.F.; Mohd Ramli, M.F.; Zahedi, F.D.; Husain, S. The association between the reflux symptoms index and nasal symptoms among patients with non-allergic rhinitis. J. Laryngol. Otol. 2021, 135, 142–146. [Google Scholar] [CrossRef] [PubMed]
- Lechien, J.R.; Hans, S.; Bobin, F.; Calvo-Henriquez, C.; Saussez, S.; Karkos, P.D. Atypical Clinical Presentation of Laryngopharyngeal Reflux: A 5-Year Case Series. J. Clin. Med. 2021, 10, 2439. [Google Scholar] [CrossRef]
- Lechien, J.R.; Radulesco, T.; Calvo-Henriquez, C.; Hamdan, A.L. Laryngopharyngeal reflux, chronic rhinosinusitis and Nasopharyngeal pH monitoring. Auris Nasus Larynx 2022, S0385-8146(22)00096-7. [Google Scholar] [CrossRef] [PubMed]
- Wong, I.W.; Omari, T.I.; Myers, J.C.; Rees, G.; Nair, S.B.; Jamieson, G.G.; Wormald, P.J. Nasopharyngeal pH monitoring in chronic sinusitis patients using a novel four channel probe. Laryngoscope 2004, 114, 1582–1585. [Google Scholar] [CrossRef] [PubMed]
- Lechien, J.R.; Mouawad, F.; Mortuaire, G.; Remacle, M.; Bobin, F.; Huet, K.; Nacci, A.; Barillari, M.R.; Crevier-Buchman, L.; Hans, S.; et al. Awareness of European Otolaryngologists and General Practitioners Toward Laryngopharyngeal Reflux. Ann. Otol. Rhinol. Laryngol. 2019, 128, 1030–1040. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.I.; Lechien, J.R.; Ayad, T.; Jia, H.; Khoddami, S.M.; Enver, N.; Raghunandhan, S.K.; Hamdan, A.L.; Eun, Y.G. Management of Laryngopharyngeal Reflux in Asia. Clin. Exp. Otorhinolaryngol. 2020, 13, 299–307. [Google Scholar] [CrossRef]
- Lechien, J.R.; Perazzo, P.S.; Ceccon, F.P.; Eckley, C.A.; Lopes, K.C.; Maunsell, R.; Avelino, M.A.G.; Akst, L.M.; Sant’Anna, G.D.; Imamura, R. Management of laryngopharyngeal reflux in Brazil: A national survey. Braz. J. Otorhinolaryngol. 2020, S1808-8694(20)30238-X. [Google Scholar] [CrossRef]
- Ghisa, M.; Coletta, M.D.; Barbuscio, I.; Marabotto, E.; Barberio, B.; Frazzoni, M.; De Bortoli, N.; Zentilin, P.; Tolone, S.; Ottonello, A.; et al. Updates in the field of non-esophageal gastroesophageal reflux disorder. Expert Rev. Gastroenterol. Hepatol. 2019, 13, 827–838. [Google Scholar] [CrossRef]
- Calvo-Henríquez, C.; Ruano-Ravina, A.; Vaamonde, P.; Martínez-Capoccioni, G.; Martín-Martín, C. Is Pepsin a Reliable Marker of Laryngopharyngeal Reflux? A Systematic Review. Otolaryngol. Head Neck Surg. 2017, 157, 385–391. [Google Scholar] [CrossRef] [PubMed]
- Zeleník, K.; Hránková, V.; Vrtková, A.; Staníková, L.; Komínek, P.; Formánek, M. Diagnostic Value of the PeptestTM in Detecting Laryngopharyngeal Reflux. J. Clin. Med. 2021, 10, 2996. [Google Scholar] [CrossRef] [PubMed]
- Guo, Z.; Jiang, J.; Wu, H.; Zhu, J.; Zhang, S.; Zhang, C. Salivary peptest for laryngopharyngeal reflux and gastroesophageal refluxdisease: A systemic review and meta-analysis. Medicine 2021, 100, e26756. [Google Scholar] [CrossRef] [PubMed]
- Zhang, M.; Chia, C.; Stanley, C.; Phyland, D.J.; Paddle, P.M. Diagnostic Utility of Salivary Pepsin as Compared with 24-hour Dual pH/Impedance Probe in Laryngopharyngeal Reflux. Otolaryngol. Head Neck Surg. 2021, 164, 375–380. [Google Scholar] [CrossRef]
| Impedance–pH Monitoring Features | ||
|---|---|---|
| Outcomes | GERD | LPR |
| Distal esophageal events | Large number of acid episodes | May be normal |
| High acid exposure | ||
| Diagnostic criteria * | ||
| Proximal/pharyngeal events | Infrequent | >1 events |
| Acid events (if present) | Weakly/nonacid events | |
| Composition of reflux | Mainly liquid | Mainly gaseous |
| Time of events | Supine & upright | Upright |
| Favoring factor | Supine position | - |
| Types of reflux | Mainly acid | Mainly weakly/nonacid |
| Correlation between | Frequently significant | Rarely significant |
| Symptoms–events | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lechien, J.R. Clinical Update Findings about pH-Impedance Monitoring Features in Laryngopharyngeal Reflux Patients. J. Clin. Med. 2022, 11, 3158. https://doi.org/10.3390/jcm11113158
Lechien JR. Clinical Update Findings about pH-Impedance Monitoring Features in Laryngopharyngeal Reflux Patients. Journal of Clinical Medicine. 2022; 11(11):3158. https://doi.org/10.3390/jcm11113158
Chicago/Turabian StyleLechien, Jerome R. 2022. "Clinical Update Findings about pH-Impedance Monitoring Features in Laryngopharyngeal Reflux Patients" Journal of Clinical Medicine 11, no. 11: 3158. https://doi.org/10.3390/jcm11113158






