Safety and Efficacy of a Large-Bore Biliary Metallic Stent for Malignant Biliary Obstruction
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patients
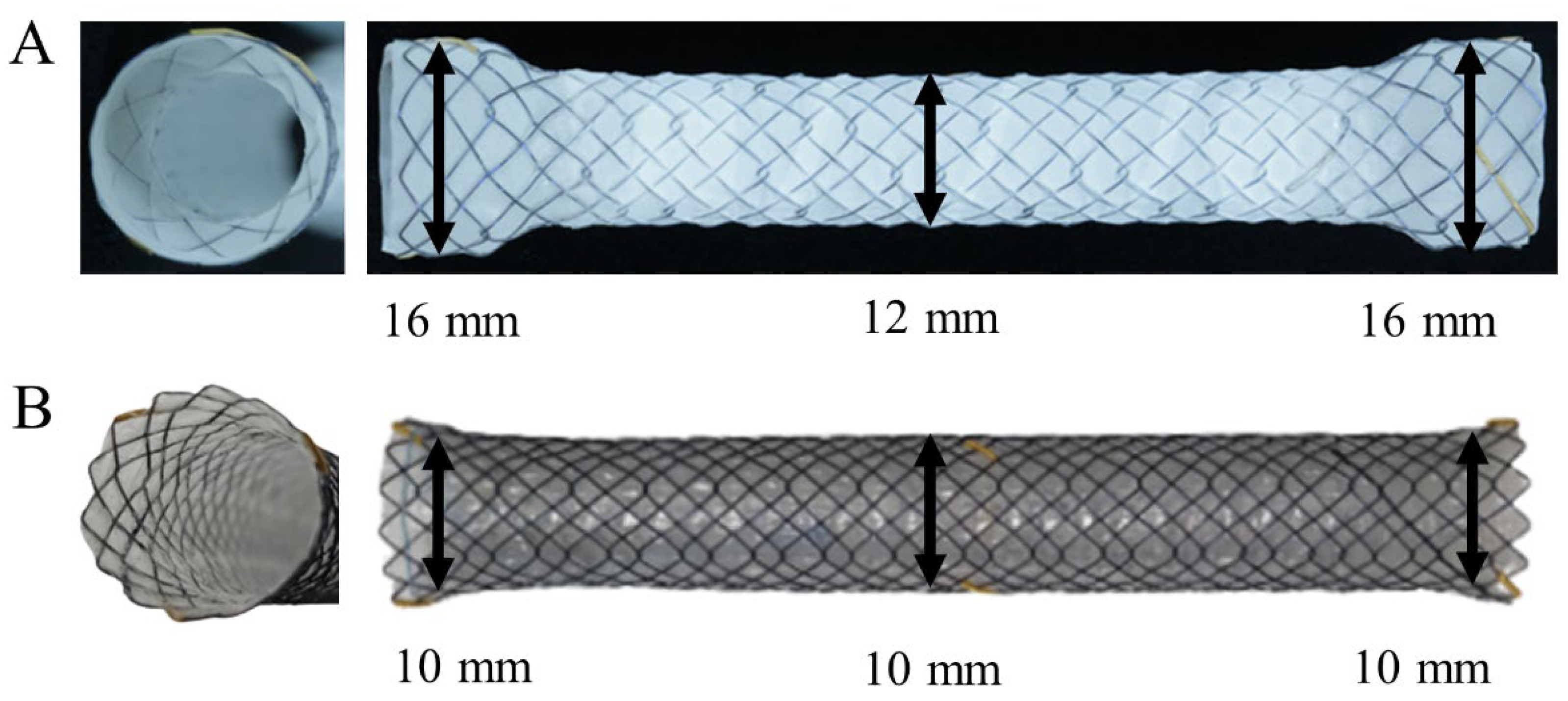
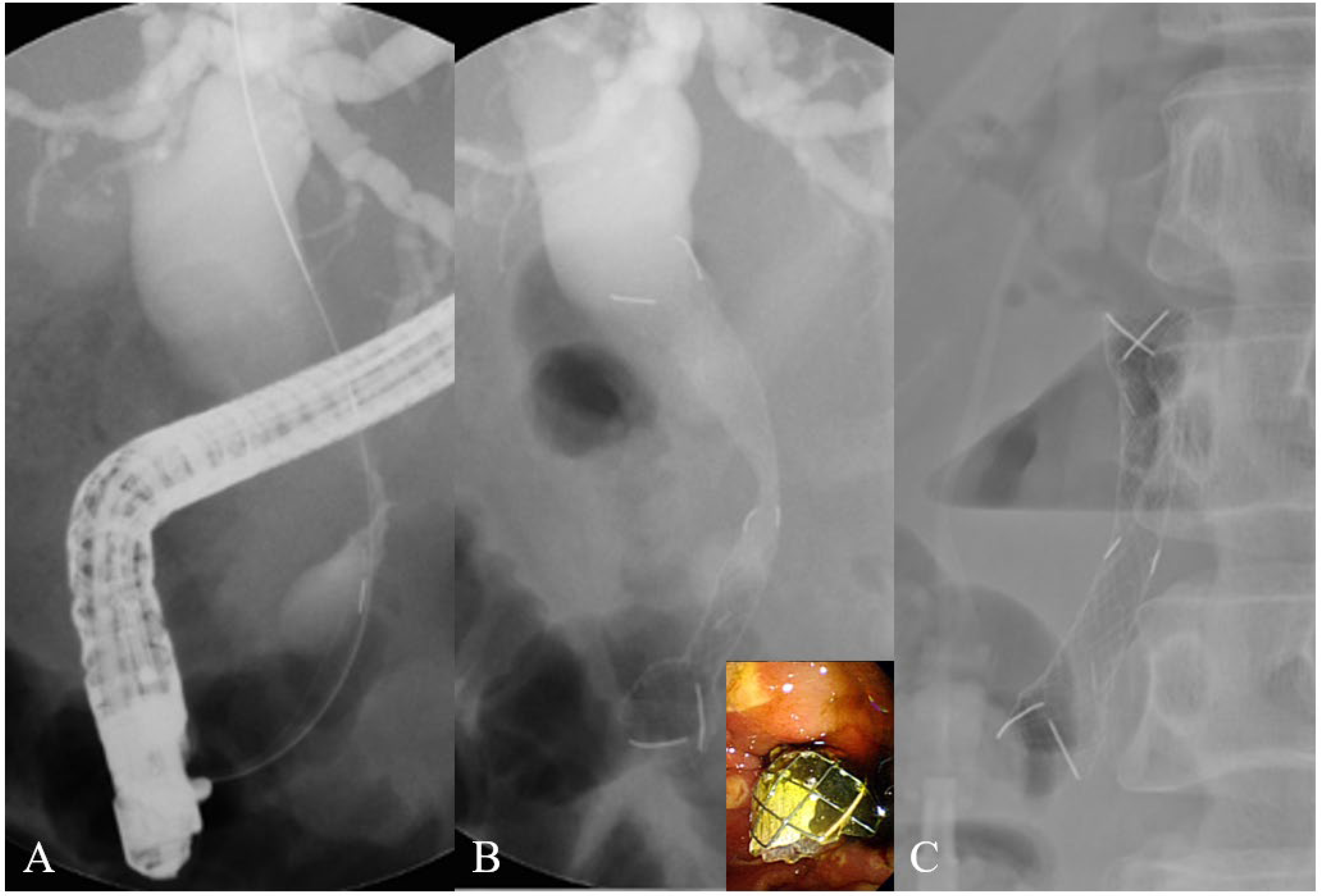
2.2. Stents
2.3. Definitions
2.4. Statistical Analysis
3. Results
3.1. Patient Characteristics
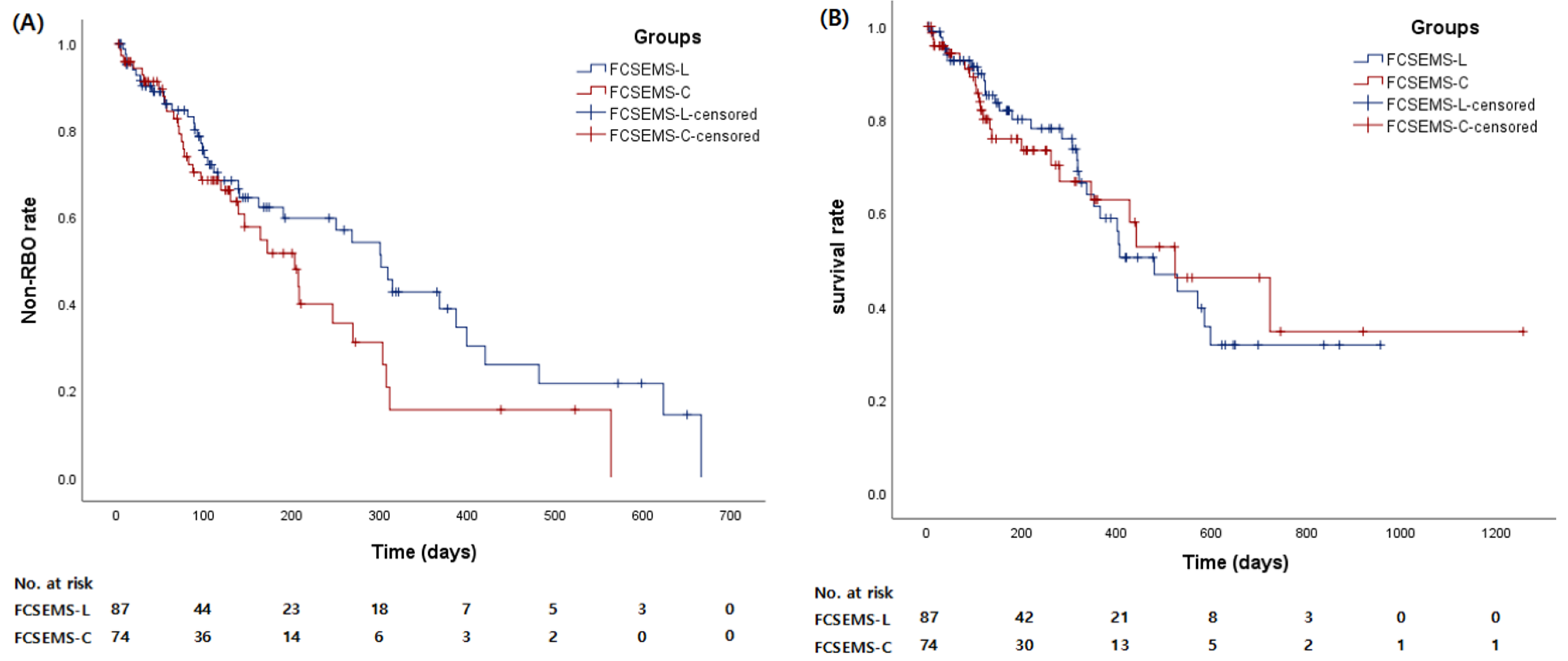
3.2. Clinical Outcomes
3.3. Reinterventions
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Boulay, B.R.; Birg, A. Malignant biliary obstruction: From palliation to treatment. World J. Gastrointest. Oncol. 2016, 8, 498–508. [Google Scholar] [CrossRef] [PubMed]
- Boulay, B.R.; Parepally, M. Managing malignant biliary obstruction in pancreas cancer: Choosing the appropriate strategy. World J. Gastroenterol. 2014, 20, 9345–9353. [Google Scholar] [CrossRef] [PubMed]
- Haag, G.M.; Herrmann, T.; Jaeger, D.; Stremmel, W.; Schemmer, P.; Sauer, P.; Gotthardt, D.N. Outcomes and risk factors for cancer patients undergoing endoscopic intervention of malignant biliary obstruction. BMC Gastroenterol. 2015, 15, 171. [Google Scholar] [CrossRef] [PubMed]
- Pu, L.Z.; Singh, R.; Loong, C.K.; de Moura, E.G. Malignant Biliary Obstruction: Evidence for Best Practice. Gastroenterol. Res. Pract. 2016, 2016, 3296801. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Srinivasan, I.; Kahaleh, M. Biliary stents in the millennium. Adv. Ther. 2011, 28, 960–972. [Google Scholar] [CrossRef]
- Szary, N.M.; Al-Kawas, F.H. Complications of endoscopic retrograde cholangiopancreatography: How to avoid and manage them. Gastroenterol. Hepatol. 2013, 9, 496–504. [Google Scholar]
- Dumonceau, J.M.; Tringali, A.; Papanikolaou, I.S.; Blero, D.; Mangiavillano, B.; Schmidt, A.; Vanbiervliet, G.; Costamagna, G.; Devière, J.; García-Cano, J.; et al. Endoscopic biliary stenting: Indications, choice of stents, and results: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline—Updated October 2017. Endoscopy 2018, 50, 910–930. [Google Scholar] [CrossRef] [Green Version]
- Irisawa, A.; Katanuma, A.; Itoi, T. Otaru consensus on biliary stenting for unresectable distal malignant biliary obstruction. Dig. Endosc. 2013, 25 (Suppl. 2), 52–57. [Google Scholar] [CrossRef]
- Raijman, I. Biliary and pancreatic stents. Gastrointest. Endosc. Clin. N. Am. 2003, 13, 561–592. [Google Scholar] [CrossRef]
- Soderlund, C.; Linder, S. Covered metal versus plastic stents for malignant common bile duct stenosis: A prospective, randomized, controlled trial. Gastrointest. Endosc. 2006, 63, 986–995. [Google Scholar] [CrossRef]
- Knyrim, K.; Wagner, H.J.; Pausch, J.; Vakil, N. A prospective, randomized, controlled trial of metal stents for malignant obstruction of the common bile duct. Endoscopy 1993, 25, 207–212. [Google Scholar] [CrossRef] [PubMed]
- Davids, P.H.; Groen, A.K.; Rauws, E.A.; Tytgat, G.N.; Huibregtse, K. Randomised trial of self-expanding metal stents versus polyethylene stents for distal malignant biliary obstruction. Lancet 1992, 340, 1488–1492. [Google Scholar] [CrossRef]
- Abdel Samie, A.; Dette, S.; Vöhringer, U.; Stumpf, M.; Kopischke, K.; Theilmann, L. Fully covered self-expandable metal stents for treatment of malignant and benign biliary strictures. World J. Gastrointest. Endosc. 2012, 4, 405–408. [Google Scholar] [CrossRef] [PubMed]
- Kahaleh, M.; Talreja, J.P.; Loren, D.E.; Kowalski, T.E.; Poneros, J.M.; Degaetani, M.; Raijman, I.; Sejpal, D.V.; Patel, S.; Rosenkranz, L.; et al. Evaluation of a fully covered self-expanding metal stent with flared ends in malignant biliary obstruction: A multicenter study. J. Clin. Gastroenterol. 2013, 47, e96–e100. [Google Scholar] [CrossRef] [PubMed]
- Moy, B.T.; Birk, J.W. An update to hepatobiliary stents. J. Clin. Transl. Hepatol. 2015, 3, 67. [Google Scholar] [CrossRef]
- Mukai, T.; Yasuda, I.; Isayama, H.; Iwashita, T.; Itoi, T.; Kawakami, H.; Kogure, H.; Nakai, Y. Pilot study of a novel, large-bore, fully covered self-expandable metallic stent for unresectable distal biliary malignancies. Dig. Endosc. 2016, 28, 671–679. [Google Scholar] [CrossRef]
- Siegel, J.H.; Pullano, W.; Kodsi, B.; Cooperman, A.; Ramsey, W. Optimal palliation of malignant bile duct obstruction: Experience with endoscopic 12 French prostheses. Endoscopy 1988, 20, 137–141. [Google Scholar] [CrossRef]
- Speer, A.G.; Cotton, P.B.; MacRae, K.D. Endoscopic management of malignant biliary obstruction: Stents of 10 French gauge are preferable to stents of 8 French gauge. Gastrointest. Endosc. 1988, 34, 412–417. [Google Scholar] [CrossRef]
- Loew, B.J.; Howell, D.A.; Sanders, M.K.; Desilets, D.J.; Kortan, P.P.; May, G.R.; Shah, R.J.; Chen, Y.K.; Parsons, W.G.; Hawes, R.H.; et al. Comparative performance of uncoated, self-expanding metal biliary stents of different designs in 2 diameters: Final results of an international multicenter, randomized, controlled trial. Gastrointest. Endosc. 2009, 70, 445–453. [Google Scholar] [CrossRef]
- Kikuyama, M.; Shirane, N.; Kawaguchi, S.; Terada, S.; Mukai, T.; Sugimoto, K. New 14-mm diameter Niti-S biliary uncovered metal stent for unresectable distal biliary malignant obstruction. World J. Gastrointest. Endosc. 2018, 10, 16. [Google Scholar] [CrossRef]
- Nakaoka, K.; Hashimoto, S.; Kawabe, N.; Nakano, T.; Kan, T.; Ohki, M.; Ochi, Y.; Takamura, T.; Kurashita, T.; Nomura, S.; et al. Evaluation of a 12-mm diameter covered self-expandable end bare metal stent for malignant biliary obstruction. Endosc. Int. Open 2018, 6, E1164–E1170. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Isayama, H.; Hamada, T.; Yasuda, I.; Itoi, T.; Ryozawa, S.; Nakai, Y.; Kogure, H.; Koike, K. TOKYO criteria 2014 for transpapillary biliary stenting. Dig. Endosc. 2015, 27, 259–264. [Google Scholar] [CrossRef] [PubMed]
- van Berkel, A.M.; Bruno, M.J.; Bergman, J.J.; van Deventer, S.J.; Tytgat, G.N.; Huibregtse, K. A prospective randomized study of hydrophilic polymer-coated polyurethane versus polyethylene stents in distal malignant biliary obstruction. Endoscopy 2003, 35, 478–482. [Google Scholar] [CrossRef]
- Dua, K.S.; Reddy, N.D.; Rao, V.G.; Banerjee, R.; Medda, B.; Lang, I. Impact of reducing duodenobiliary reflux on biliary stent patency: An in vitro evaluation and a prospective randomized clinical trial that used a biliary stent with an antireflux valve. Gastrointest. Endosc. 2007, 65, 819–828. [Google Scholar] [CrossRef]
- Misra, S.P.; Dwivedi, M. Reflux of duodenal contents and cholangitis in patients undergoing self-expanding metal stent placement. Gastrointest. Endosc. 2009, 70, 317–321. [Google Scholar] [CrossRef] [PubMed]
- Okamoto, T.; Fujioka, S.; Yanagisawa, S.; Yanaga, K.; Kakutani, H.; Tajiri, H.; Urashima, M. Placement of a metallic stent across the main duodenal papilla may predispose to cholangitis. Gastrointest. Endosc. 2006, 63, 792–796. [Google Scholar] [CrossRef]
- Wen, F.; Lu, Z.; Mao, X.; Liang, H.; Guo, Q. Bridging across the ampulla with metal stents: Evidences for intestinal bile reflux. Hepato-Gastroenterol. 2013, 60, 1903–1905. [Google Scholar]
- Pfau, P.R.; Pleskow, D.K.; Banerjee, S.; Barth, B.A.; Bhat, Y.M.; Desilets, D.J.; Gottlieb, K.T.; Maple, J.T.; Siddiqui, U.D.; Tokar, J.L.; et al. Pancreatic and biliary stents. Gastrointest. Endosc. 2013, 77, 319–327. [Google Scholar] [CrossRef]
- Li, J.; Li, T.; Sun, P.; Yu, Q.; Wang, K.; Chang, W.; Song, Z.; Zheng, Q. Covered versus Uncovered Self-Expandable Metal Stents for Managing Malignant Distal Biliary Obstruction: A Meta-Analysis. PLoS ONE 2016, 11, e0149066. [Google Scholar] [CrossRef]
- Maetani, I.; Shigoka, H.; Omuta, S.; Gon, K.; Saito, M. What is the preferred shape for an esophageal stent flange? Dig. Endosc. 2012, 24, 401–406. [Google Scholar] [CrossRef]
- Moon, J.H.; Choi, H.J.; Koo, H.C.; Han, S.H.; Lee, T.H.; Cho, Y.D.; Park, S.-H.; Kim, S.-J. Feasibility of placing a modified fully covered self-expandable metal stent above the papilla to minimize stent-induced bile duct injury in patients with refractory benign biliary strictures (with videos). Gastrointest. Endosc. 2012, 75, 1080–1085. [Google Scholar] [CrossRef] [PubMed]
- Choi, S.J.; Kim, J.H.; Choi, J.W.; Lim, S.G.; Shin, S.J.; Lee, K.M.; Lee, K.J. Fully covered, retrievable self-expanding metal stents (Niti-S) in palliation of malignant dysphagia: Long-term results of a prospective study. Scand. J. Gastroenterol. 2011, 46, 875–880. [Google Scholar] [CrossRef] [PubMed]
- Yamada, T.; Ogura, T.; Okuda, A.; Imanishi, M.; Kamiyama, R.; Miyano, A.; Nishioka, N.; Higuchi, K. Pilot Study of Dumbbell-Type Covered Self-Expandable Metal Stent Deployment for Benign Pancreatic Duct Stricture (with Videos). J. Gastrointest. Surg. 2018, 22, 2194–2200. [Google Scholar] [CrossRef] [PubMed]
- Kawashima, H.; Hashimoto, S.; Ohno, E.; Ishikawa, T.; Morishima, T.; Matsubara, H.; Sugimoto, H.; Nonogaki, K.; Kanamori, A.; Hara, K.; et al. Comparison of 8- and 10-mm diameter fully covered self-expandable metal stents: A multicenter prospective study in patients with distal malignant biliary obstruction. Dig. Endosc. 2019, 31, 439–447. [Google Scholar] [CrossRef]
| FCSEMS-L (n = 87) | FCSEMS-C (n = 74) | |
|---|---|---|
| Age, mean ± SD, years | 67.1 ± 10.7 | 69.0 ± 13.2 |
| Male: Female | 45:42 | 33:41 |
| Diagnosis, n (%) | ||
| Pancreas cancer | 56 (64.4) | 39 (52.7) |
| CBD cancer | 15 (17.2) | 16 (21.6) |
| GB cancer | 8 (9.2) | 11 (14.9) |
| Ampulla of vater cancer | 2 (2.3) | 5 (6.8) |
| Metastatic disease | 6 (6.9) | 3 (4.1) |
| TNM Stage, n (%) | ||
| III | 33 (37.9) | 35 (47.3) |
| IV | 54 (62.1) | 39 (52.7) |
| Duodenal stricture, n (%) | 2 (2.3) | 1 (1.4) |
| Length of biliary stricture, mean ± SD, mm | 24.3 ± 9.9 | 26.4 ± 11.2 |
| Maximum diameter of proximal bile duct, mean ± SD, mm | 14.9 ± 5.0 | 15.0 ± 4.9 |
| Follow-up period, mean ± SD, day | 261.9 ± 220.1 | 225.7 ± 233.8 |
| Chemotherapy, n (%) | 68 (78.2) | 49 (66.2) |
| Serum bilirubin level, mean ± SD, mg/dL | ||
| Baseline | 6.7 ± 5.5 | 7.0 ± 6.0 |
| 1 Day after stent insertion | 4.6 ± 4.1 | 4.8 ± 4.3 |
| 4 Weeks after stent insertion | 1.2 ± 0.7 | 1.4 ± 1.2 |
| Variables | FCSEMS-L(n = 87) | FCSEMS-C(n = 74) | p Value |
|---|---|---|---|
| Length of stent, n (%) | 0.690 | ||
| 4 cm | 2 (2.3) | 0 | |
| 5 cm | 9 (10.3) | 7 (9.5) | |
| 6 cm | 36 (41.4) | 28 (37.8) | |
| 7 cm | 24 (27.6) | 24 (32.4) | |
| 8 cm | 16 (18.4) | 15 (20.3) | |
| RBO, n (%) | 31 (35.6) | 34 (45.9) | 0.184 |
| Stent occlusion, n (%) | 19 (21.8) | 22 (29.7) | 0.252 |
| Sludge impaction | 18 | 19 | |
| Food impaction | 10 | 7 | |
| Tumor ingrowth | 2 | 1 | |
| Tumor overgrowth | 1 | 4 | |
| Stent migration, n (%) | 12 (13.8) | 12 (16.2) | 0.667 |
| Proximal | 0 | 0 | |
| Distal | 12 | 12 | |
| Early complication, n (%) | 3 (3.4) | 7 (9.5) | 0.237 |
| Pancreatitis | 1 | 1 | |
| Non-occlusion cholangitis | 2 | 6 | |
| Late complication, n (%) | 3 (3.4) | 4 (5.4) | 0.808 |
| Non-occlusion cholangitis | 2 | 3 | |
| Cholecystitis | 1 | 1 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Do, M.Y.; Jang, S.I.; Cho, J.H.; Kim, Y.; Kim, I.-J.; Lee, K.-H.; Joo, S.-M.; Lee, D.K. Safety and Efficacy of a Large-Bore Biliary Metallic Stent for Malignant Biliary Obstruction. J. Clin. Med. 2022, 11, 3092. https://doi.org/10.3390/jcm11113092
Do MY, Jang SI, Cho JH, Kim Y, Kim I-J, Lee K-H, Joo S-M, Lee DK. Safety and Efficacy of a Large-Bore Biliary Metallic Stent for Malignant Biliary Obstruction. Journal of Clinical Medicine. 2022; 11(11):3092. https://doi.org/10.3390/jcm11113092
Chicago/Turabian StyleDo, Min Young, Sung Ill Jang, Jae Hee Cho, Yonsoo Kim, In-Jung Kim, Kwang-Hun Lee, Seung-Moon Joo, and Dong Ki Lee. 2022. "Safety and Efficacy of a Large-Bore Biliary Metallic Stent for Malignant Biliary Obstruction" Journal of Clinical Medicine 11, no. 11: 3092. https://doi.org/10.3390/jcm11113092
APA StyleDo, M. Y., Jang, S. I., Cho, J. H., Kim, Y., Kim, I.-J., Lee, K.-H., Joo, S.-M., & Lee, D. K. (2022). Safety and Efficacy of a Large-Bore Biliary Metallic Stent for Malignant Biliary Obstruction. Journal of Clinical Medicine, 11(11), 3092. https://doi.org/10.3390/jcm11113092






