Impact of Silver Diamine Fluoride Therapy on the Oral Health-Related Quality of Life of Preschool Children with Behavioral Problems after Three Months: A Pilot Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design, Subjects, and Setting
2.2. Variables
2.3. Data Sources and Measurements
2.4. Statistical Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Çolak, H.; Dülgergil, Ç.T.; Dalli, M.; Hamidi, M.M. Early childhood caries update: A review of causes, diagnoses, and treatments. J. Nat. Sci. Biol. Med. 2013, 4, 29. [Google Scholar] [PubMed] [Green Version]
- Kazeminia, M.; Abdi, A.; Shohaimi, S.; Jalali, R.; Vaisi-Raygani, A.; Salari, N.; Mohammadi, M. Dental caries in primary and permanent teeth in children’s worldwide, 1995 to 2019: A systematic review and meta-analysis. Head Face Med. 2020, 16, 1–21. [Google Scholar] [CrossRef] [PubMed]
- Bodenwinkler, A.; Sax, G.; Kerschbaum, H. Länder-Zahnstatuserhebung 2016: Sechsjährige in Österreich. Zahnstatus Sechsjähriger Kinder Mit und Ohne Migrationshintergrund; Gesundheit Österreich: Wien, Austria, 2017. [Google Scholar]
- Martins-Júnior, P.; Vieira-Andrade, R.; Corrêa-Faria, P.; Oliveira-Ferreira, F.; Marques, L.; Ramos-Jorge, M. Impact of early childhood caries on the oral health-related quality of life of preschool children and their parents. Caries Res. 2013, 47, 211–218. [Google Scholar] [CrossRef] [PubMed]
- Mansoori, S.; Mehta, A.; Ansari, M.I. Factors associated with oral health related quality of life of children with severe-early childhood caries. J. Oral Biol. Craniofacial Res. 2019, 9, 222–225. [Google Scholar] [CrossRef] [PubMed]
- Baier, K.; Milgrom, P.; Russell, S.; Mancl, L.; Yoshida, T. Children’s fear and behavior in private pediatric dentistry practices. Pediatr. Dent. 2004, 26, 316–321. [Google Scholar] [PubMed]
- Ramazani, N. Different aspects of general anesthesia in pediatric dentistry: A review. Iran. J. Pediatr. 2016, 26, e2613. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, H.H.; Milgrom, P.; Starks, H.; Burke, W. Trends in death associated with pediatric dental sedation and general anesthesia. Pediatr. Anesth. 2013, 23, 741–746. [Google Scholar] [CrossRef] [Green Version]
- Oubenyahya, H.; Bouhabba, N. General anesthesia in the management of early childhood caries: An overview. J. Dent. Anesth. Pain Med. 2019, 19, 313–322. [Google Scholar] [CrossRef]
- Kanellis, M.J.; Damiano, P.C.; Momany, E.T. Medicaid costs associated with the hospitalization of young children for restorative dental treatment under general anesthesia. J. Public Health Dent. 2000, 60, 28–32. [Google Scholar] [CrossRef]
- McCann, M.E.; Soriano, S.G. Does general anesthesia affect neurodevelopment in infants and children? BMJ 2019, 367, l6459. [Google Scholar] [CrossRef] [Green Version]
- Gordon, N.B. Silver diamine fluoride staining is acceptable for posterior primary teeth and is preferred over advanced pharmacologic behavior management by many parents. J. Evid.-Based Dent. Pract. 2018, 18, 94–97. [Google Scholar] [CrossRef] [PubMed]
- Yee, R.; Holmgren, C.; Mulder, J.; Lama, D.; Walker, D.; van Palenstein Helderman, W. Efficacy of silver diamine fluoride for arresting caries treatment. J. Dent. Res. 2009, 88, 644–647. [Google Scholar] [CrossRef] [PubMed]
- Sihra, R.; Schroth, R.J.; Bertone, M.; Martin, H.; Patterson, B.; Mittermuller, B.; Lee, V.; Moffatt, M.E.; Klus, B.; Fontana, M.; et al. The effectiveness of silver diamine fluoride and fluoride varnish when used to arrest caries in young children and associated oral health-related quality of life. J. Can. Dent. Assoc. 2020, 86, k9. [Google Scholar]
- Magno, M.B.; Silva, L.P.D.; Ferreira, D.M.; Barja-Fidalgo, F.; Fonseca-Gonçalves, A. Aesthetic perception, acceptability and satisfaction in the treatment of caries lesions with silver diamine fluoride: A scoping review. Int. J. Paediatr. Dent. 2019, 29, 257–266. [Google Scholar] [CrossRef] [PubMed]
- Omara, M.; Stamm, T.; Bekes, K. Four-dimensional oral health-related quality of life impact in children: A systematic review. J. Oral. Rehabil. 2020, 48, 293–304. [Google Scholar] [CrossRef] [PubMed]
- Pahel, B.T.; Rozier, R.G.; Slade, G.D. Parental perceptions of children’s oral health: The Early Childhood Oral Health Impact Scale (ECOHIS). Health Qual. Life Outcomes 2007, 5, 6. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bekes, K.; Omara, M.; Safar, S.; Stamm, T. The German version of early childhood oral health impact scale (ECOHIS-G): Translation, reliability, and validity. Clin. Oral Investig. 2019, 23, 4449–4454. [Google Scholar] [CrossRef] [Green Version]
- Ruff, R.R.; Whittemore, R.; Grochecki, M.; Bateson, J.; Barry Godín, T.J. Silver diamine fluoride and oral health-related quality of life: A review and network meta-analysis. PLoS ONE 2022, 17, e0261627. [Google Scholar] [CrossRef]
- Pitts, N.B.; Ekstrand, K.R.; Foundation, I. International Caries Detection and Assessment System (ICDAS) and its International Caries Classification and Management System (ICCMS)—Methods for staging of the caries process and enabling dentists to manage caries. Community Dent. Oral Epidemiol. 2013, 41, e41–e52. [Google Scholar] [CrossRef]
- Ambjørnsen, E.; Valderhaug, J.; Norheim, P.W.; Fløystrand, F. Assessment of an additive index for plaque accumulation on complete maxillary dentures. Acta Odontol. Scand. 1982, 40, 203–208. [Google Scholar] [CrossRef]
- Chen, Y.-P.; Hsieh, C.-Y.; Hsu, W.-T.; Wu, F.-Y.; Shih, W.-Y. A 10-year trend of dental treatments under general anesthesia of children in Taipei Veterans General Hospital. J. Chin. Med. Assoc. 2017, 80, 262–268. [Google Scholar] [CrossRef] [PubMed]
- Yawary, R.; Hegde, S. Silver Diamine Fluoride Protocol for Reducing Preventable Dental Hospitalisations in Victorian Children. Int. Dent. J. 2021, 72, 322–330. [Google Scholar] [CrossRef] [PubMed]
- Renugalakshmi, A.; Vinothkumar, T.S.; Hakami, F.B.; Salem, R.M.; Qadri, A.A.; Harbosh, Z.M.; Hakami, Z. Impact of silver diamine fluoride therapy on oral health-related quality of life of uncooperative preschool children: A prospective study. Oral Health Prev. Dent. 2021, 19, 93–99. [Google Scholar] [PubMed]
- Duangthip, D.; Gao, S.S.; Chen, K.J.; Lo, E.C.M.; Chu, C.H. Oral health-related quality of life of preschool children receiving silver diamine fluoride therapy: A prospective 6-month study. J. Dent. 2019, 81, 27–32. [Google Scholar] [CrossRef] [PubMed]
- Milgrom, P.; Horst, J.A.; Ludwig, S.; Rothen, M.; Chaffee, B.W.; Lyalina, S.; Pollard, K.S.; DeRisi, J.L.; Mancl, L. Topical silver diamine fluoride for dental caries arrest in preschool children: A randomized controlled trial and microbiological analysis of caries associated microbes and resistance gene expression. J. Dent. 2018, 68, 72–78. [Google Scholar] [CrossRef]
| All n (%) | |
|---|---|
| Sex | |
| Male ♂ | 16 (53) |
| Female ♀ | 14 (47) |
| Age | |
| Mean (SD) | 2.8 years (1.0) |
| 0–1 years | 6 (20) |
| 2 years | 10 (33) |
| 3 years | 7 (23) |
| 4 years | 4 (13) |
| 5 years | 3 (10) |
| Baseline | |
| dmft index *, mean (SD) | 4.2 (2.9) |
| Plaque | 36 (17.2) |
| Distribution of teeth | |
| Mean (SD) | 2.6 (1.3) |
| Molars | 32 (41) |
| Incisors | 47 (59) |
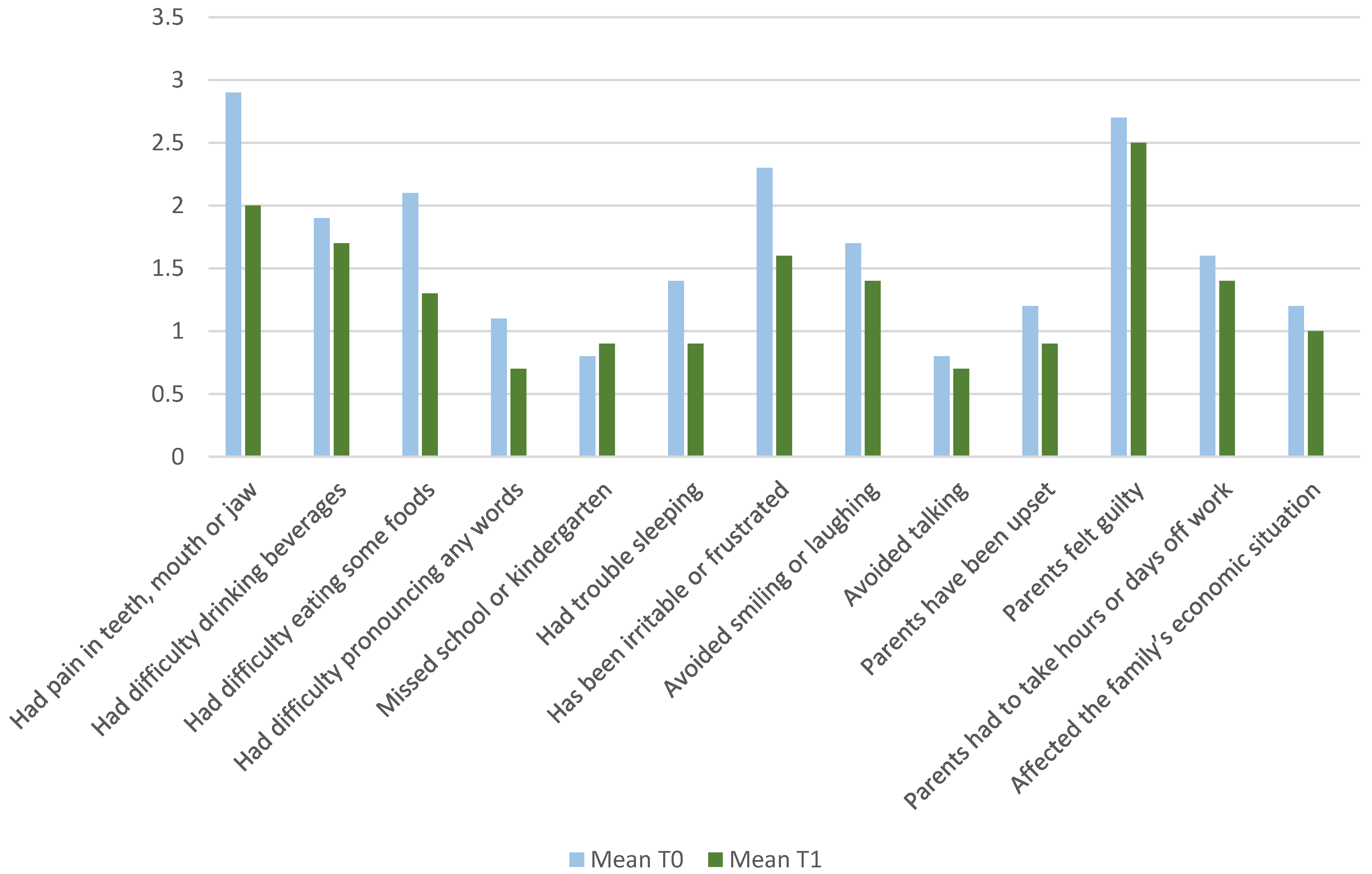
| ECOHIS Domain | Baseline (T0) Mean (SD) | Followup (T1) Mean (SD) | Effect Size | p-Value |
|---|---|---|---|---|
| Total Score | 21.4 (8.5) | 16.3 (5.6) | 0.7 | <0.001 |
| Child impact | 14.9 (6.7) | 10.8 (5.2) | 0.6 | <0.001 |
| Symptoms | 2.9 (2.1) | 2.0 (1.3) | 0.7 | <0.001 |
| Function | 5.8 (2.4) | 3.9 (2.0) | 1.0 | <0.001 |
| Child Psychology | 3.7 (1.9) | 2.9 (1.6) | 0.4 | 0.62 |
| Social interaction | 2.5 (2.2) | 2.1 (1.8) | 0.2 | 0.48 |
| Family impact | 6.7 (3.9) | 5.8 (4.1) | 0.2 | 0.09 |
| Parent distress | 3.9 (2.2) | 3.5 (2.4) | 0.1 | 0.34 |
| Family function | 2.8 (1.4) | 2.5 (0.9) | 0.2 | 0.11 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Altner, S.; Stroj, D.; Bekes, K. Impact of Silver Diamine Fluoride Therapy on the Oral Health-Related Quality of Life of Preschool Children with Behavioral Problems after Three Months: A Pilot Study. J. Clin. Med. 2022, 11, 3071. https://doi.org/10.3390/jcm11113071
Altner S, Stroj D, Bekes K. Impact of Silver Diamine Fluoride Therapy on the Oral Health-Related Quality of Life of Preschool Children with Behavioral Problems after Three Months: A Pilot Study. Journal of Clinical Medicine. 2022; 11(11):3071. https://doi.org/10.3390/jcm11113071
Chicago/Turabian StyleAltner, Sarra, Daniel Stroj, and Katrin Bekes. 2022. "Impact of Silver Diamine Fluoride Therapy on the Oral Health-Related Quality of Life of Preschool Children with Behavioral Problems after Three Months: A Pilot Study" Journal of Clinical Medicine 11, no. 11: 3071. https://doi.org/10.3390/jcm11113071
APA StyleAltner, S., Stroj, D., & Bekes, K. (2022). Impact of Silver Diamine Fluoride Therapy on the Oral Health-Related Quality of Life of Preschool Children with Behavioral Problems after Three Months: A Pilot Study. Journal of Clinical Medicine, 11(11), 3071. https://doi.org/10.3390/jcm11113071







