Poor Long-Term Renal Allograft Survival in Patients with Chronic Antibody-Mediated Rejection, Irrespective of Treatment—A Single Center Retrospective Study
Abstract
1. Introduction
2. Materials and Methods
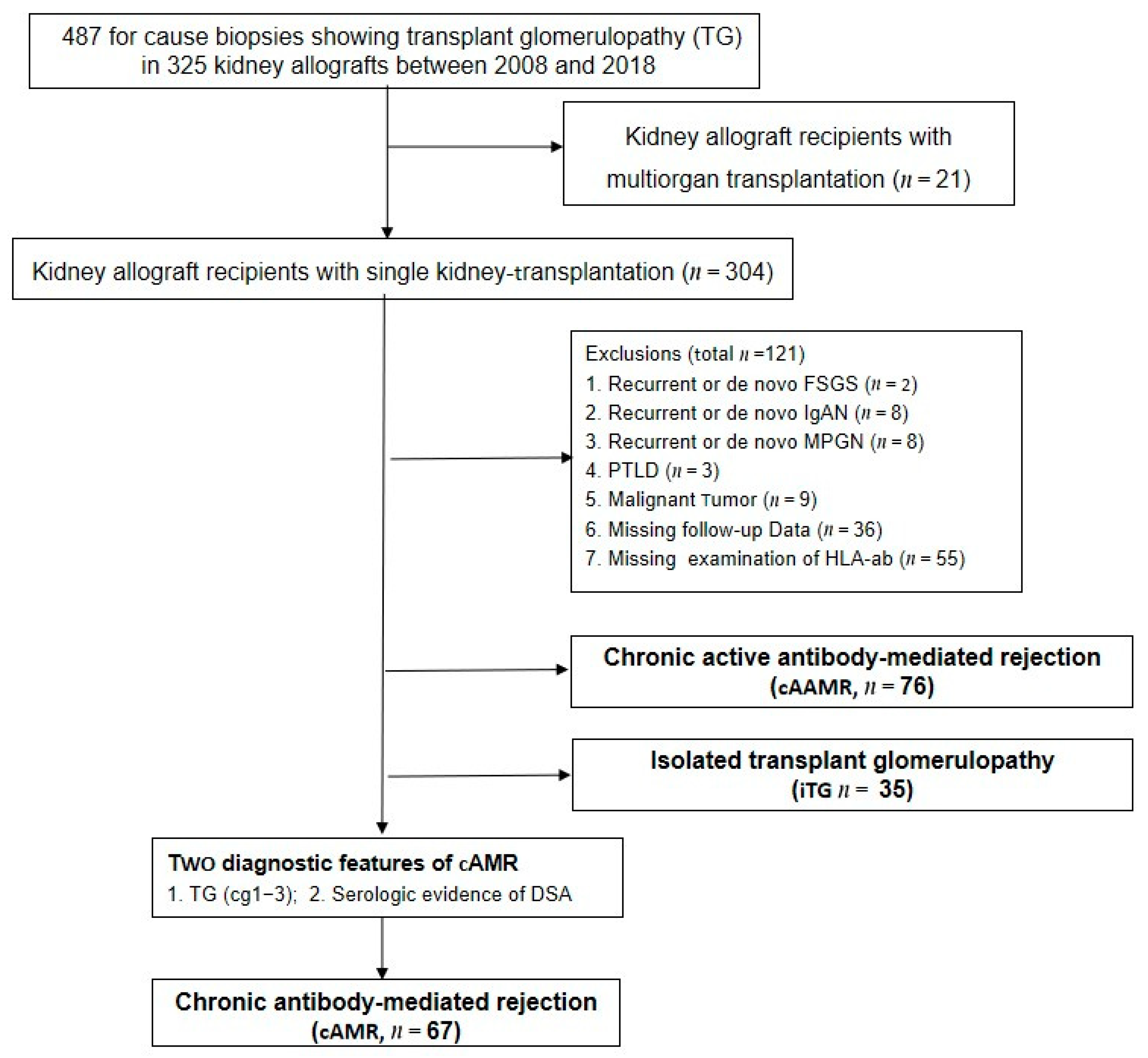
2.1. Study Population and Data Collection
2.2. Histopathology Evaluation
2.3. HLA-Antibodies Screening
2.4. Immunosuppression and Therapeutic Strategies
2.5. The Observation of Clinical Outcomes
2.6. Statistical Analysis
3. Results
3.1. Clinical Characteristics at Studied Biopsy
3.2. Effect of Antihumoral Therapy (AHT) on DSA
3.3. Effect of AHT on the Allograft Function
3.4. Effect of AHT on the Long-Term Clinical Outcomes
3.5. Histological Evaluation of the Studied Biopsy
3.6. Safety of AHT
3.7. Correlation of Histological and Clinical Features with Five-Year Outcome after Diagnosis of cAMR
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Mayrdorfer, M.; Liefeldt, L.; Wu, K.; Rudolph, B.; Zhang, Q.; Friedersdorff, F.; Lachmann, N.; Schmidt, D.; Osmanodja, B.; Naik, M.G.; et al. Exploring the complexity of death-censored kidney allograft failure. J. Am. Soc. Nephrol. 2021, 32, 1513–1526. [Google Scholar] [CrossRef] [PubMed]
- Einecke, G.; Sis, B.; Reeve, J.; Mengel, M.; Campbell, P.M.; Hidalgo, L.G.; Kaplan, B.; Halloran, P.F. Antibody-mediated microcirculation injury is the major cause of late kidney transplant failure. Am. J. Transplant. 2009, 9, 2520–2531. [Google Scholar] [CrossRef] [PubMed]
- Banfi, G.; Villa, M.; Cresseri, D.; Cresseri, D.; Ponticelli, C. The clinical impact of chronic tranplant glomerulopathy in cyclosporine era. Transplantation 2005, 80, 1392–1397. [Google Scholar] [CrossRef] [PubMed]
- Remport, A.; Ivanyi, B.; Mathe, Z.; Tinckam, K.; Mucsi, I.; Molnar, M.Z. Better understanding of transplant glomerulopathy secondary to chronic antibody-mediated rejection. Nephrol. Dial. Transplant. 2015, 30, 1825–1833. [Google Scholar] [CrossRef]
- Montgomery, R.A.; Cozzi, E.; West, L.J.; Warren, D.S. Humoral immunity and antibody-mediated rejection in solid organ transplantation. Semin. Immunol. 2011, 23, 224–234. [Google Scholar] [CrossRef]
- Solez, K.; Colvin, R.B.; Racusen, L.C.; Sis, B.; Halloran, P.F.; Birk, P.E.; Campbell, P.M.; Cascalho, M.; Collins, A.B.; Demetris, A.J.; et al. Banff ‘05 Meeting Report: Differential diagnosis of chronic allograft injury and elimination of chronic allograft nephropathy (’CAN’). Am. J. Transplant. 2007, 7, 518–526. [Google Scholar] [CrossRef]
- Haas, M.; Sis, B.; Racusen, L.C.; Solez, K.; Glotz, D.; Colvin, R.B.; Castro, M.C.R.; David, D.S.R.; David-Neto, E.; Bagnasco, S.M.; et al. Banff 2013 meeting report: Inclusion of c4d-negative antibody-mediated rejection and antibody-associated arterial lesions. Am. J. Transplant. 2014, 14, 272–283. [Google Scholar] [CrossRef]
- Haas, M.; Loupy, A.; Lefaucheur, C.; Roufosse, C.; Glotz, D.; Seron, D.; Nankivell, B.J.; Halloran, P.F.; Colvin, R.B.; Akalin, E.; et al. The Banff 2017 kidney meeting report: Revised diagnostic criteria for chronic active T-cell-mediated rejection, antibody-mediated rejection, and prospects for integrative endpoints for next-generation clinical trials. Am. J. Transplant. 2018, 18, 293–307. [Google Scholar]
- Archdeacon, P.; Chan, M.; Neuland, C.; Velidedeoglu, E.; Meyer, J.; Tracy, L.; Cavaille-Coll, M.; Bala, S.; Hernandez, A.; Albrecht, R. Summary of FDA antibody-mediated rejection workshop. Am. J. Transplant. 2011, 11, 896–906. [Google Scholar] [CrossRef]
- Lefaucheur, C.; Nochy, D.; Andrade, J.; Verine, J.; Gautreau, C.; Charron, D.; Hill, G.S.; Glotz, D.; Suberbielle-Boissel, C. Comparison of combination plasmapheresis/IVIG/anti-CD20 versus high-dose IVIG in the treatment of antibody-mediated rejection. Am. J. Transplant. 2009, 9, 1099–1107. [Google Scholar] [CrossRef]
- Schinstock, C.A.; Mannon, R.B.; Budde, K.; Chong, A.S.; Haas, M.; Knechtle, S.; Lefaucheur, C.; Montgomery, R.A.; Nickerson, P.; Tullius, S.G.; et al. Recommended Treatment for Antibody-mediated Rejection After Kidney Transplantation: The 2019 expert Consensus From the Transplantion Society Working Group. Transplantation 2020, 104, 911–922. [Google Scholar] [CrossRef]
- Sis, B.; Campbell, P.M.; Mueller, T.; Hunter, C.; Cockfield, S.M.; Cruz, J.; Meng, C.; Wishart, D.; Solez, K.; Halloran, P.F. Transplant glomerulopathy, late antibody-mediated rejection and the ABCD tetrad in kidney allograft biopsies for cause. Am. J. Transplant. 2007, 7, 1743–1752. [Google Scholar] [CrossRef]
- Schmidt, D.; Osmanodja, B.; Pfefferkorn, M.; Graf, V.; Raschke, D.; Duettmann, W.; Naik, M.G.; Gethmann, C.J.; Mayrdorfer, M.; Halleck, F.; et al. TBase—An Integrated Electronic Health Record and Research Database for Kidney Transplant Recipients. J. Vis. Exp. 2021, 170, e61971. [Google Scholar] [CrossRef]
- Haas, M. Transplant glomerulopathy: It′s not always about chronic rejection. Kidney Int. 2011, 80, 801–803. [Google Scholar] [CrossRef][Green Version]
- Tait, D.B.; Süsal, C.; Gebel, M.H.; Nickerson, P.W.; Zachary, A.A.; Claas, F.H.J.; Reed, E.F.; Bray, R.A.; Campbell, P.; Chapman, J.R.; et al. Consensus guidelines on the testing and clinical management issues associated with HLA and non-HLA antibodies in transplantation. Transplantation 2013, 95, 19–47. [Google Scholar] [CrossRef]
- Huber, L.; Lachmann, N.; Dürr, M.; Matz, M.; Liefeldt, L.; Neumayer, H.H.; Schönemann, C.; Budde, K. Identification and therapeutic management of highly sensitized patients undergoing renal transplantation. Drugs 2012, 72, 1335–1354. [Google Scholar] [CrossRef] [PubMed]
- Waiser, J.; Klotsche, J.; Lachmann, N.; Wu, K.; Rudolph, B.; Halleck, F.; Liefeldt, L.; Bachmann, F.; Budde, K.; Duerr, M. Predictors of graft survival at diagnosis of antibody-mediated renal allograft rejection: A retrospective single-center cohort study. Transplant. Int. 2020, 33, 149–160. [Google Scholar] [CrossRef] [PubMed]
- Ashman, N.; Chapagain, A.; Dobbie, H.; Raftery, M.J.; Sheaff, M.T.; Yaqoob, M.M. Belatacept as maintenance immunosuppression for postrenal transplant de novo drug-induced thrombotic microangiopathy. Am. J. Transplant. 2009, 9, 424–427. [Google Scholar] [CrossRef] [PubMed]
- Rule, A.D.; Bailey, K.R.; Schwartz, G.L.; Khosla, S.; Lieske, J.C.; Melton, L.J., 3rd. For estimating creatinine clearance measuring muscle mass gives better results thatn those based on demographics. Kidney Int. 2009, 75, 1071–1078. [Google Scholar] [CrossRef]
- Montgomery, R.A.; Loupy, A.; Segev, D.L. Antibody-mediated rejectdion: New approaches in prevention and management. Am. J. Transplant. 2018, 18 (Suppl. S3), 3–7. [Google Scholar] [CrossRef]
- Callemeyn, J.; Ameye, H.; Lerut, E.; Senev, A.; Coemans, M.; von Loon, E.; Sprangers, B.; van Sandt, V.; Rabeyrin, M.; Dubois, V.; et al. Revisiting the changes in the Banff classification for antibody-mediated rejection after kidney transplantation. Am. J. Transplant. 2021, 21, 2413–2423. [Google Scholar] [CrossRef] [PubMed]
- Wan, S.S.; Ying, T.D.; Wyburn, K.; Roberts, D.M.; Wyld, M.; Chadban, S.J. The treatment of antibody-mediated rejection in kidney transplantation: An updated systematic review and meta-analysis. Transplantation 2018, 102, 557–568. [Google Scholar] [CrossRef]
- Bartel, G.; Schwaiger, E.; Bohmig, G.A. Prevention and treatment of alloantibody-mediated kidney transplant rejection. Transpl. Int. 2011, 24, 1142–1155. [Google Scholar] [CrossRef]
- Takemoto, S.K.; Zeevi, A.; Feng, S.; Colvin, R.B.; Jordan, S.; Kobashigawa, J.; Kupiec-Weglinski, J.; Matas, A.; Montgomery, R.A.; Nickerson, P.; et al. National conference to assess antibody-mediated rejection in solid organ transplantation. Am. J. Transplant. 2004, 4, 1033–1041. [Google Scholar] [CrossRef]
- Stegall, M.D.; Gloor, J.; Winters, J.L.; Moore, S.B.; Degoey, S. A comparison of plasmapheresis versus high–dose IVIG desensitization in renal allograft recipients with high levels of donor specific alloantibody. Am. J. Transplant. 2006, 6, 346–351. [Google Scholar] [CrossRef]
- Walsh, R.C.; Brailey, P.; Girnita, A.; Alloway, R.R.; Shields, A.R.; Wall, G.E.; Sadaka, B.H.; Cardi, M.; Tevar, A.; Govil, A.; et al. Early and late acute antibody-mediated rejection differ immunologically and in response to proteasome inhibition. Transplantation 2011, 91, 1218–1226. [Google Scholar] [CrossRef]
- Gupta, G.; Abu Jawdeh, B.G.; Bhasin, B.; Bhasin, B.; Arend, L.; Trollinger, B.; Kraus, E.; Rabb, H.; Zachary, A.A.; Montgomery, R.A.; et al. Late antibody-mediated rejection in renal allografts: Outcome after conventional and novel therapies. Transplantation 2014, 97, 1240–1246. [Google Scholar] [CrossRef]
- Moreso, F.; Crespo, M.; Ruiz, J.C.; Torres, A.; Gutierrez-Dalmau, A.; Osuna, A.; Perello, M.; Pascual, J.; Torres, I.B.; Redondo-Pachon, D.; et al. Treatment of chronic antibody mediated rejection with intravenous immunoglobulins and rituximab: A multicenter, prospective, randomized, double-blind clinical trial. Am. J. Transplant. 2018, 18, 927–935. [Google Scholar] [CrossRef] [PubMed]
- Kamar, N.; Milioto, O.; Puissant-Lubrano, B.; Esposito, L.; Pierre, M.C.; Mohamed, A.O.; Lavayssiere, L.; Cointault, O.; Ribes, D.; Cardeau, I.; et al. Incidence and predictive factors for infectious disease after rituximab therapy in kidney-transplant patients. Am. J. Transplant. 2010, 10, 89–98. [Google Scholar] [CrossRef] [PubMed]
- Touzot, M.; Couvrat-Desvergnes, G.; Castagnet, S.; Cesbron, A.; Renaudin, K.; Cantarovich, D.; Giral, M. Differential modulation of donor-specific antibodies after B-cell depleting therapies to cure chronic antibody mediated rejection. Transplantation 2015, 99, 63–68. [Google Scholar] [CrossRef] [PubMed]
- Haas, M. The relationship between pathologic lesions of active and chronic antibody-mediated rejection in renal allografts. Am. J. Transplant. 2018, 18, 2849–2856. [Google Scholar] [PubMed]
- Heilman, R.L.; Nijim, A.; Desmarteau, Y.M.; Khamash, H.; Pando, M.J.; Chakera, H.A.; Huskey, J.; Valdez, R.; Reddy, K.S. De Novo Donor-Specific Human Leukocyte Antigen Antibodies Early After Kidney Transplantation. Transplantation 2014, 98, 1310–1315. [Google Scholar] [CrossRef] [PubMed]
- Lefaucheur, C.; Loupy, A.; Hill, G.S.; Andrade, J.; Nochy, D.; Antoine, C.; Gautreau, C.; Charron, D.; Glotz, D.; Suberbielle-Boissel, C. Preexisting donor-specific HLA antibodies predict outcome in kidney transplantation. J. Am. Soc. Nephrol. 2010, 21, 1398–1406. [Google Scholar] [CrossRef] [PubMed]
- Hönger, G.; Hopfer, H.; Arnold, M.L.; Spriewald, B.M.; Schaub, S.; Amico, P. Pretransplant IgG subclasses of donor-specific human leukocyte antigen antibodies and development of antibodymediated rejection. Transplantation 2011, 92, 41–47. [Google Scholar] [CrossRef] [PubMed]
- Cicciarelli, J.C.; Kasahara, N.; Lemp, N.A.; Adamson, R.; Dembitsky, W.; Browne, B.; Steinberg, S. Immunoglobulin G subclass analysis of HLA donor specific antibodies in heart and renal transplant recipients. Clin. Transpl. 2013, 2013, 413–422. [Google Scholar]
- Loupy, A.; Jordan, S.C. Donor-specific HLA antibodies and renal allograft failure. Nat. Rev. Nephrol. 2013, 9, 130–131. [Google Scholar] [CrossRef]
- Loupy, A.; Suberbielle-Boissel, C.; Hill, G.S.; Lefaucheur, C.; Anglicheau, D.; Zuber, J.; Martinez, F.; Thervet, E.; Mejean, A.; Charron, D.; et al. Outcome of subclinical antibody-mediated rejection in kidney transplant recipients with preformed donor-specific antibodies. Am. J. Transplant. 2009, 9, 2561–2570. [Google Scholar] [CrossRef]
- Wiebe, C.; Gibson, I.W.; Blydt-Hansen, T.D.; Pochinco, D.; Birk, P.E.; Ho, J.; Karpinski, M.; Goldberg, A.; Storsley, L.; Rush, D.N.; et al. Rates and determinants of progression to graft failure in kidney allograft recipients with de novo donorspecifific antibody. Am. J. Transplant. 2015, 15, 2921–2930. [Google Scholar] [CrossRef]
- Böhmig, G.A.; Eskandary, F.; Doberer, K.; Halloran, P.F. The therapeutic challenge of late antibody-mediated kidney allograft rejection. Transpl. Int. 2019, 32, 775–788. [Google Scholar] [CrossRef]
- Dunn, T.B.; Noreen, H.; Gillingham, K.; Maurer, D.; Ozturk, O.G.; Pruett, T.L.; Gebel, H.M.; Matas, A.J. Revisiting traditional risk factors for rejection and graft loss after kidney transplantation. Am. J. Transplant. 2011, 11, 2132–2143. [Google Scholar] [CrossRef]
- Meier-Kriesche, H.U.; Schold, J.D.; Srinivas, T.R.; Kaplan, B. Lack of improvement in renal allograft survival despite a marked decrease in acute rejection rates over the most recent era. Am. J. Transplant. 2004, 4, 378–383. [Google Scholar] [CrossRef]
- Randhawa, P. T-cell-mediated rejection of the kidney in the era of donor-specific antibodies: Diagnostic challenges and clinical significance. Curr. Opin. Organ Transplant. 2015, 20, 325–332. [Google Scholar] [CrossRef]
- Naesens, M.; Kuypers, D.R.; De Vusser, K.; Evenepoel, P.; Claes, K.; Bammens, B.; Meijers, B.; Sprangers, B.; Pirenne, J.; Monbaliu, D.; et al. The histology of kidney transplant failure: A long-term follow-up study. Transplantation 2014, 98, 427–435. [Google Scholar] [CrossRef]
- Hillebrands, J.L.; Rozing, J. Chronic transplant dysfunction and transplant arteriosclerosis: New insights into underlying mechanisms. Expert Rev. Mol. Med. 2003, 5, 1–23. [Google Scholar] [CrossRef]
- Lefaucheur, C.; Loupy, A.; Vernerey, D.; Duog-Van-Huyen, J.P.; Suberbielle, C.; Anglicheau, D.; Verine, J.; Beuscart, T.; Nochy, D.; Bruneval, P.; et al. Antibody-mediated vascular rejection of kidney allografts: A population-based study. Lancet 2013, 381, 313–319. [Google Scholar] [CrossRef]
- Oberbauer, R. Progression of interstitial fibrosis in kidney transplantation. Clin. J. Am. Soc. Nephrol. 2016, 11, 2110–2112. [Google Scholar] [CrossRef] [PubMed]
- Patri, P.; Seshan, S.V.; Matignon, M.; Matignon, M.; Desvaux, D.; Lee, J.R.; Lee, J.; Dadhania, D.M.; Serur, D.; Grimbert, P.; et al. Development and validation of a prognostic index for allograft outcome in kidney recipients with transplant glomerulopathy. Kidney Int. 2016, 89, 450–458. [Google Scholar] [CrossRef] [PubMed]

| (A) Demographics | |||
| cAMRwo (n = 46) | cAMR-AHT (n = 21) | p-Value | |
|---|---|---|---|
| Recipient age (years, median IQR) | 43 (18–69) | 41 (25–67) | 0.99 |
| Recipient gender (m/f) | 21/25 | 9/12 | 0.41 |
| Recipient BMI (kg/m2 median, IQR) | 24.8 (18.3–35.5) | 22.8 (19.7–34.4) | 0.40 |
| First kidney transplant N (%) | 31 (67.4%) | 15 (71.4%) | 0.83 |
| PRA before transplantation >10% N (%) | 4 (8.7%) | 5 (23.8%) | 0.24 |
| Broad HLA-mismatches (N, median IQR) | 3 (0–6) | 3 (0–5) | 0.75 |
| CIT (hours median IQR) | 5.8 (0.5–20.3) | 7.5(0.5–18.5) | 0.03 |
| Presence of DGF N (%) | 14 (32.6%) | 11 (52.4%) | 0.10 |
| Donor age (years, median, IQR) | 50 (17–83) | 49 (16–71) | 0.21 |
| Donor gender (m/f) | 19/25 | 10/11 | 0.53 |
| Living donation N (%) | 18 (40.0%) | 7 (33.3%) | 0.55 |
| (B) Clinical characteristics | |||
| Indications of the studied biopsy for graft dysfunction/proteinuria/or both (N) | 21/5/18 | 15/0/6 | 0.09 |
| Duration between transplantation and studied biopsy (years, median IQR) | 7.3 (1.2–18.7) | 5.3 (0.3–14.2) | 0.03 |
| Follow-up after biopsy (years, median IQR) | 5.6 (0.5–15.0) | 6.3 (0.7–11.5) | 0.10 |
| Detectable DSA in serum (months post transplantation, median IQR) | 79.1 (14.8–197.6) | 63.9 (0.5–177.0) | 0.90 |
| HLA-antibody class type I/II/both | 8/28/10 | 3/13/5 | 0.58 |
| Maintenance immunosuppression regimens at studied biopsy N (%) | |||
| Tac + MMF/MPA + PDN | 24 (52.2%) | 16 (76.2%) | 0.06 |
| CyA + MMF/MPA + PDN | 6 (13.0%) | 1 (4.8%) | 0.29 |
| Rapamycin + MMF/MPA + PDN | 2 (4.3%) | 1 (4.8%) | 0.91 |
| Tac + MMF/MPA | 1 (2.2%) | 1 (4.8%) | 0.22 |
| CyA + MMF/MPA | 6 (13.0%) | 1 (4.8%) | 0.38 |
| CyA + Azathioprine + PDN | 1 (2.2%) | 0 (0.0%) | 0.45 |
| Tac + PDN | 3 (6.5%) | 0 (0.0%) | 0.40 |
| CyA + PDN | 1 (2.2%) | 0 (0.0%) | 0.54 |
| MMF/MPA + PDN | 2 (4.3%) | 1 (4.8%) | 0.73 |
| Antihumoral therapy N (%) | |||
| PPh + IVIG | -- | 12 (57.1%) | -- |
| PPh + IVIG + rituximab | -- | 5 (23.8%) | -- |
| PPh + IVIG + bortezomib | -- | 4 (19.0%) | -- |
| Steroid bolus to treat concomitant TCMR | 9 (19.6%) | 10 (47.6%) | 0.04 |
| Change of CNI after the studied biopsies N (%) | |||
| Increasing dose of CyA or Tac | 10 (21.7%) | 5(23.8%) | 0.27 |
| Reducing dose of CyA or Tac | 9 (19.6%) | 3 (14.3%) | 0.36 |
| Withdrawal of CyA or Tac | 3 (6.5%) | 1 (4.8%) | 0.87 |
| Switch between CyA and Tacrolimus | 7 (15.2%) | 7 (33.3%) | 0.40 |
| Switch CNI to mTor inhibitor | 0 (0.0%) | 0 (0.0%) | 0.10 |
| Switch CNI to Belatacept | 5 (10.9%) | 1 (4.8%) | 0.56 |
| No change | 12 (26.1%) | 4 (19.0%) | 0.32 |
| Presence of advere events in the 6 months post studied biopsy | |||
| Urinary tract infection N (%) | 3 (6.5%) | 3 (14.3%) | 0.45 |
| Respiratory tract infection N (%) | 1 (2.2%) | 0 (0.0%) | 0.44 |
| CMV infectious colitis N (%) | 0 (0.0%) | 2 (9.5%) | 0.02 |
| Polyoma virus nephropathy N (%) | 2 (4.4%) | 0(0.0%) | 0.09 |
| Pancytopenia N (%) | 3 (6.5%) | 3(14.3%) | 0.33 |
| Overall | 9 (19.6%) | 8 (38.1%) | 0.04 |
| The level of HbA1c and blood pressure at studied biopsy | |||
| HbA1c level at studied biopsy (% means ± SD) | 5.6 ± 0.7 | 5.2 ± 0.4 | 0.02 |
| SBP at studied biopsy (mmHg mean ± SD) | 141.3 ± 19.5 | 129.4 ± 16.6 | 0.02 |
| DBP at studied biopsy (mmHg mean ± SD) | 83.4 ± 10.5 | 80.1 ± 14.1 | 0.29 |
| Antihypertensive therapy at studied biopsy | |||
| ACEi N (%) | 24 (51.7%) | 11 (52.4%) | 0.71 |
| ARB N (%) | 16 (34.0%) | 11 (52.4%) | 0.14 |
| CCB N (%) | 27 (57.4%) | 13 (61.9%) | 0.87 |
| Beta-blocker N (%) | 7 (14.9%) | 2 (9.5%) | 0.64 |
| cAMRwo (n = 46) | cAMR-AHT (n = 21) | p-Value | |
|---|---|---|---|
| The values of MFI at and post the studied biopsies (median IQR) | |||
| MFI_max at biopsy, median (IQR) | 7500 (528–23,336) | 8293 (48–16,275) | 0.98 |
| MFI_max at 6 months post biopsy, median (IQR) | 6234 (2018–18,209) | 4470 (369–12,811) | 0.61 |
| MFI_max at 1 year post biopsy, median (IQR) | 6368 (593–21,934) | 4920 (43–16,817) | 0.50 |
| The values of eGFR at and post the studied biopsies (mL/min median IQR) | |||
| eGFR value at 6 months before studied biopsy | 35.3 (12.0–86.0) | 40.1 (10.5–88.6) | 0.04 |
| eGFR value at studied biopsy | 28.5 (5.4–67.9) | 26.4 (10.0–52.0) | 0.60 |
| eGFR value at 6 months post studied biopsy | 26.7 (5.0–89.0) | 21.6 (5.0–52.0) | 0.30 |
| The decline in eGFR values at and post the studied biopsies (mL/min median IQR) | |||
| ∆ eGFR value at studied biopsy | −6.6 (−6.0–30.0) | −13.1 (−1.0–60.6) | 0.04 |
| ∆ eGFR value at 6 months post studied biopsy | −2.6 (−31.0–25.0) | −4.9 (−18.8–7.0) | 0.61 |
| The variation in the proteinuria at and post the studied biopsies (mg/day median IQR) | |||
| PU value at 6 months before studied biopsy | 991(59–5155) | 653 (45–2613) | 0.09 |
| PU value at studied biopsy | 918 (48–11,579) | 969 (143–5812) | 0.78 |
| PU value at 6 months post studied biopsy | 665(89–6989) | 1114 (208–3732) | 0.57 |
| The decline in proteinuria at and post the studied biopsies (mg/day median IQR) | |||
| ∆ PU value at studied biopsy | −21 (−3744–7465) | 304 (−950–5588) | 0.11 |
| ∆ PU value at 6 months post studied biopsy | 89 (−8272–4318) | 27 (−3145–1195) | 0.47 |
| cAMRwo (n = 46) | cAMR-AHT (n = 21) | p-Value | |
|---|---|---|---|
| (A) Histological diagnosis in for-cause allograft biopsies before studied biopsies | |||
| Episode of TCMRi > = 1, N (%) | 13 (28.3%) | 8 (38.1%) | 0.09 |
| Episode of TCMRv > = 1, N (%) | 4 (8.7%) | 0(0.0%) | 0.38 |
| Episode of active AMR > = 1, N (%) | 2 (4.3%) | 5 (23.9%) | 0.11 |
| Episode of ATI > = 1, N (%) | 11 (23.9%) | 3 (14.3%) | 0.49 |
| (B) Histological diagnosis in for-cause allograft biopsies after studied biopsies | |||
| Episode of cAAMR > = 1, N (%) | 9 (19.6%) | 4 (19.0%) | 0.81 |
| Episode of cAMR > = 1, N (%) | 12 (26.1%) | 9 (42.9%) | 0.03 |
| (C) Histological scores of Banff lesions in the studied biopsy (scores mean ± SD) | |||
| g (0–3) | 0.1 ± 0.3 | 0.4 ± 0.5 | 0.01 |
| ci (0–3) | 1.0 ± 0.9 | 0.5 ± 0.8 | 0.04 |
| ct (0–3) | 1.0 ± 0.9 | 0.5 ± 0.8 | 0.04 |
| mm (0–3) | 0.7 ± 0.9 | 0.3 ± 0.6 | 0.06 |
| ptc (0–3) | 0.1 ± 0.3 | 0.1 ± 0.2 | 0.08 |
| ah (0–3) | 2.5 ± 0.9 | 2.4 ± 0.8 | 0.12 |
| cv (0–3) | 1.7 ± 1.1 | 1.4 ± 1.0 | 0.17 |
| v (0–3) | 0.1 ± 0.3 | 0.1 ± 0.3 | 0.17 |
| i (0–3) | 0.7 ± 1.0 | 0.9 ± 1.0 | 0.27 |
| cg (0–3) | 2.1 ± 0.8 | 2.4 ± 0.7 | 0.33 |
| t (0–3) | 0.3 ± 0.7 | 0.5 ± 0.6 | 0.38 |
| C4d (0–3) | 0.0 ± 0.0 | 0.0 ± 0.0 | 0.99 |
| Concomitant TCMR N (%) | 9 (19.6%) | 10 (47.6%) | 0.04 |
| Overall Graft Loss | Patient Death | Death-Censored Graft Loss | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Clinical factors | OR | 95% CI | p-value | OR | 95% CI | p-value | OR | 95% CI | p-value | |||
| eGFR above median at biopsy | 0.4 | 0.1 | 1.5 | 0.18 | 0.4 | 0.1 | 1.6 | 0.20 | 0.4 | 0.1 | 1.6 | 0.19 |
| PU above median at biopsy | 2.2 | 0.6 | 8.5 | 0.24 | 2.3 | 0.6 | 8.9 | 0.23 | 2.2 | 0.6 | 8.5 | 0.18 |
| Receiving antihumoral therapy | 2.5 | 0.6 | 10.0 | 0.21 | 1.9 | 0.5 | 7.8 | 0.38 | 2.6 | 0.6 | 10.7 | 0.18 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wu, K.; Schmidt, D.; López del Moral, C.; Osmanodja, B.; Lachmann, N.; Zhang, Q.; Halleck, F.; Choi, M.; Bachmann, F.; Ronicke, S.; et al. Poor Long-Term Renal Allograft Survival in Patients with Chronic Antibody-Mediated Rejection, Irrespective of Treatment—A Single Center Retrospective Study. J. Clin. Med. 2022, 11, 199. https://doi.org/10.3390/jcm11010199
Wu K, Schmidt D, López del Moral C, Osmanodja B, Lachmann N, Zhang Q, Halleck F, Choi M, Bachmann F, Ronicke S, et al. Poor Long-Term Renal Allograft Survival in Patients with Chronic Antibody-Mediated Rejection, Irrespective of Treatment—A Single Center Retrospective Study. Journal of Clinical Medicine. 2022; 11(1):199. https://doi.org/10.3390/jcm11010199
Chicago/Turabian StyleWu, Kaiyin, Danilo Schmidt, Covadonga López del Moral, Bilgin Osmanodja, Nils Lachmann, Qiang Zhang, Fabian Halleck, Mira Choi, Friederike Bachmann, Simon Ronicke, and et al. 2022. "Poor Long-Term Renal Allograft Survival in Patients with Chronic Antibody-Mediated Rejection, Irrespective of Treatment—A Single Center Retrospective Study" Journal of Clinical Medicine 11, no. 1: 199. https://doi.org/10.3390/jcm11010199
APA StyleWu, K., Schmidt, D., López del Moral, C., Osmanodja, B., Lachmann, N., Zhang, Q., Halleck, F., Choi, M., Bachmann, F., Ronicke, S., Duettmann, W., Naik, M. G., Schrezenmeier, E., Rudolph, B., & Budde, K. (2022). Poor Long-Term Renal Allograft Survival in Patients with Chronic Antibody-Mediated Rejection, Irrespective of Treatment—A Single Center Retrospective Study. Journal of Clinical Medicine, 11(1), 199. https://doi.org/10.3390/jcm11010199






