Single-Breath Counting Test Predicts Non-Invasive Respiratory Support Requirements in Patients with COVID-19 Pneumonia
Abstract
:1. Introduction
2. Materials and Methods
2.1. Protocol and Data Collection
2.2. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Huang, C.; Wang, Y. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020, 395, 497–506. [Google Scholar] [CrossRef] [Green Version]
- Zanza, C.; Racca, F.; Longhitano, Y.; Piccioni, A.; Franceschi, F.; Artico, M.; Abenavoli, L.; Maiese, A.; Passaro, G.; Volonnino, G.; et al. Risk Management and Treatment of Coagulation Disorders Related to COVID-19 Infection. Int. J. Env. Res. Public Health 2021, 18, 1268. [Google Scholar] [CrossRef] [PubMed]
- Wang, D.; Hu, B.; Hu, C.; Zhu, F.; Liu, X.; Zhang, J.; Wang, B.; Xiang, H.; Cheng, Z.; Xiong, Y.; et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA 2020, 323, 1061–1069. [Google Scholar] [CrossRef] [PubMed]
- Longhitano, Y.; Racca, F.; Zanza, C.; Piccioni, A.; Audo, A.; Muncinelli, M.; Santi, R.; Kozel, D.; Geraci, C.; Taverna, M.; et al. Venous thromboembolism in critically ill patients affected by ARDS related to COVID-19 in Northern-West Italy. Eur. Rev. Med. Pharmacol. Sci. 2020, 24, 9154–9160. [Google Scholar] [PubMed]
- Grasselli, G.; Tonetti, T.; Protti, A.; Langer, T.; Girardis, M.; Ballani, G.; Laffey, J.; Carrafiello, G.; Carsana, L.; Rizzuto, C.; et al. Pathophysiology of COVID-19-associated acute respiratory distress syndrome: A multicentre prospective observational study. Lancet Respir. Med. 2020, 8, 1201–1208. [Google Scholar] [CrossRef]
- Wei, Y.Y.; Wang, R.R.; Zhang, D.-W.; Tu, Y.-H.; Chen, C.-S.; Ji, S.; Li, C.-X.; Li, X.-Y.; Zhou, M.-X.; Cao, W.-S.; et al. Risk factors for severe COVID-19: Evidence from 167 hospitalized patients in Anhui, China. J. Infect. 2020, 81, e89–e92. [Google Scholar] [CrossRef]
- Xie, J.; Covassin, N.; Fan, Z.; Singh, P.; Gao, W.; Li, G.; Kara, T.; Somers, V.K. Association Between Hypoxemia and Mortality in Patients With COVID-19. Mayo Clin. Proc. 2020, 95, 1138–1147. [Google Scholar] [CrossRef]
- Alhazzani, W.; Møller, M.H.; Arabi, Y.M.; Loeb, M.; Gong, M.N.; Fan, E.; Oczkowski, S.; Levy, M.M.; Derde, L.; Dzierba, A.; et al. Surviving Sepsis Campaign: Guidelines on the Management of Critically Ill Adults with Coronavirus Disease 2019 (COVID-19). Crit. Care Med. 2020, 48, e440–e469. [Google Scholar] [CrossRef]
- Frat, J.P.; Thille, A.W.; Mercat, A.; Girault, C.; Ragot, S.; Perbet, S.; Prat, G.; Boulain, T.; Morawiec, E.; Cottereau, A.; et al. High-flow oxygen through nasal cannula in acute hypoxemic respiratory failure. N. Engl. J. Med. 2015, 372, 2185–2196. [Google Scholar] [CrossRef] [Green Version]
- Antonelli, M.; Conti, G.; Esquinas, A.; Montini, L.; Maggiore, S.M.; Bello, G.; Rocco, M.; Maviglia, R.; Pennisi, M.A.; Gonzalez-Diaz, G.; et al. A multiple-center survey on the use in clinical practice of noninvasive ventilation as a first-line intervention for acute respiratory distress syndrome. Crit. Care Med. 2007, 35, 18–25. [Google Scholar] [CrossRef]
- Carteaux, G.; Millán-Guilarte, T.; De Prost, N.; Razazi, K.; Abid, S.; Thille, A.W.; Schortgen, F.; Brochard, L.; Brun-Buisson, C.; Dessap, A.M. Failure of noninvasive ventilation for de novo acute hypoxemic respiratory failure: Role of tidal volume. Crit. Care Med. 2016, 44, 282–290. [Google Scholar] [CrossRef]
- Mukhtar, A.; Rady, A.; Hasanin, A.; Lotfy, A.; El Adawy, A.; Hussein, A.; El-Hefnawy, I.; Hassan, M.; Mostafa, H. Admission SpO2 and ROX index predict outcome in patients with COVID-19. Am. J. Emerg. Med. 2021, 50, 106–110. [Google Scholar] [CrossRef]
- Heo, J.; Han, D.; Kim, H.-J.; Kim, D.; Lee, Y.-K.; Lim, D.; Hong, S.O.; Park, M.-J.; Ha, B.; Seog, W. Prediction of patients requiring intensive care for COVID-19: Development and validation of an integer-based score using data from Centers for Disease Control and Prevention of South Korea. J. Intensive Care 2021, 9, 16. [Google Scholar] [CrossRef]
- Hao, B.; Sotudian, S.; Wang, T.; Xu, T.; Hu, Y.; Gaitanidis, A.; Breen, K.; Velmahos, G.C.; Paschalidis, I.C. Early prediction of level-of-care requirements in patients with COVID-19. eLife 2020, 9, e60519. [Google Scholar] [CrossRef]
- Simonson, T.S.; Baker, T.L.; Banzett, R.B.; Bishop, T.; Dempsey, J.A.; Feldman, J.L.; Guyenet, P.G.; Hodson, E.J.; Mitchell, G.S.; Moya, E.A.; et al. Silent hypoxaemia in COVID-19 patients. J. Physiol. 2021, 599, 1057–1065. [Google Scholar] [CrossRef]
- Richardson, S.; Hirsch, J.S.; Narasimhan, M.; Crawford, J.M.; McGinn, T.; Davidson, K.W.; Barnaby, D.P.; Becker, L.B.; Chelico, J.D.; Cohen, S.L.; et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City area. JAMA 2020, 323, 2052–2059. [Google Scholar] [CrossRef]
- Bartfield, J.M.; Ushkow, B.S.; Rosen, J.M.; Dylong, K. Single breath counting in the assessment of pulmonary function. Ann. Emerg. Med. 1994, 24, 256–259. [Google Scholar] [CrossRef]
- Ali, S.S.; O’Connell, C.; Kass, L.; Graff, G. Single-breath counting: A pilot study of a novel technique for measuring pulmonary function in children. Am. J. Emerg. Med. 2011, 29, 33–36. [Google Scholar] [CrossRef]
- Ushkow, B.S.; Bartfield, J.M.; Reicho, P.R.; Raccio-Robak, N. Single-breath counting for the assessment of bronchospastic patients in the ED. Am. J. Emerg. Med. 1998, 16, 100–101. [Google Scholar] [CrossRef]
- Elsheikh, B.; Arnold, W.D.; Gharibshahi, S.; Reynolds, J.; Freimer, M.; Kissel, J.T. Correlation of single-breath count test and neck flexor muscle strength with spirometry in myasthenia gravis. Muscle Nerve 2016, 53, 134–136. [Google Scholar] [CrossRef]
- Yadaw, A.S.; Li, Y.-C.; Bose, S.; Iyengar, R.; Bunyavanich, S.; Pandey, G. Clinical features of COVID-19 mortality: Development and validation of a clinical prediction model. Lancet Digit. Health 2020, 2, e516–e525. [Google Scholar] [CrossRef]
- Zhou, F.; Yu, T.; Du, R.; Fan, G.; Liu, Y.; Liu, Z.; Xiang, J.; Wang, Y.; Song, B.; Gu, X.; et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. Lancet 2020, 395, 1054–1062. [Google Scholar] [CrossRef]
- Xu, X.P.; Zhang, X.C.; Hu, S.L.; Xu, J.Y.; Xie, J.F.; Liu, S.Q.; Liu, L.; Huang, Y.Z.; Guo, F.M.; Yang, Y.; et al. Noninvasive Ventilation in Acute Hypoxemic Nonhypercapnic Respiratory Failure: A Systematic Review and Meta-Analysis. Crit. Care Med. 2017, 45, e727–e733. [Google Scholar] [CrossRef]
- Couzin-Frankel, J. The mystery of the pandemic’s ‘happy hypoxia’. Science 2020, 368, 455–456. [Google Scholar] [CrossRef]
- Tobin, M.J.; Laghi, F.; Jubran, A. Why COVID-19 silent hypoxemia is baffling to physicians. Am. J. Respir. Crit. Care Med. 2020, 202, 356–360. [Google Scholar] [CrossRef]
- Allado, E.; Poussel, M.; Valentin, S.; Kimmoun, A.; Levy, B.; Nguyen, D.T.; Rumeau, C.; Chenuel, B. The Fundamentals of Respiratory Physiology to Manage the COVID-19 Pandemic: An Overview. Front. Physiol. 2021, 11, 615690. [Google Scholar] [CrossRef]
- Guan, W.J.; Ni, Z.Y.; Hu, Y.; Liang, W.-H.; Ou, C.-Q.; He, J.-X.; Liu, L.; Shan, H.; Lei, C.-L.; Hui, D.S.C.; et al. Clinical Characteristics of Coronavirus Disease 2019 in China. N. Engl. J. Med. 2020, 382, 1708–1720. [Google Scholar] [CrossRef]
- Global Initiative for Asthma (GINA). Global Strategy for Asthma Management and Prevention. Available online: www.ginasthma.org (accessed on 18 May 2021).
- Roper, J.; Fleming, M.E.; Long, B.; Koyfman, A. Myasthenia Gravis and Crisis: Evaluation and Management in the Emergency Department. J. Emerg. Med. 2017, 53, 843–853. [Google Scholar] [CrossRef]
- Herridge, M.S.; Cheung, A.M.; Tansey, C.M.; Matte-Martyn, A.; Diaz-Granados, N.; Al-Saidi, F.; Cooper, A.B.; Guest, C.B.; Mazer, C.D.; Mehta, S.; et al. One-year outcomes in survivors of the acute respiratory distress syndrome. N. Engl. J. Med. 2003, 348, 683–693. [Google Scholar] [CrossRef] [Green Version]
- Heyland, D.K.; Groll, D.; Caeser, M. Survivors of acute respiratory distress syndrome: Relationship between pulmonary dysfunction and long-term health-related quality of life. Crit. Care Med. 2005, 33, 1549–1556. [Google Scholar] [CrossRef]
- Kouri, A.; Gupta, S.; Yadollahi, A.; Ryan, C.; Gershon, A.S.; To, T.; Tarlo, S.M.; Goldstein, R.S.; Chapman, K.R.; Chow, C.-W. Addressing Reduced Laboratory-Based Pulmonary Function Testing During a Pandemic. Chest 2020, 158, 2502–2510. [Google Scholar] [CrossRef] [PubMed]
- Juel, V.C. Myasthenia gravis: Management of myasthenic crisis and perioperative care. Semin. Neurol. 2004, 24, 75–81. [Google Scholar] [CrossRef] [PubMed]
- Prediletto, I.; D’Antoni, L.; Carbonara, P.; Daniele, F.; Dongilli, R.; Flore, R.; Pacilli, A.M.G.; Pisani, L.; Tomsa, C.; Vega, M.L.; et al. Standardizing PaO2 for PaCO2 in P/F ratio predicts in-hospital mortality in acute respiratory failure due to COVID-19: A pilot prospective study. Eur. J. Intern. Med. 2021, 92, 48–54. [Google Scholar] [CrossRef] [PubMed]
- Zanza, C.; Tassi, M.F.; Romenskaya, T.; Piccolella, F.; Abenavoli, L.; Franceschi, F.; Piccioni, A.; Ojetti, V.; Saviano, A.; Canonico, B.; et al. Lock, Stock and Barrel: Role of Renin-Angiotensin-Aldosterone System in Coronavirus Disease 2019. Cells 2021, 10, 1752. [Google Scholar] [CrossRef] [PubMed]
| NIRS Not Required (42) | NIRS Required (78) | p-Value | ||
|---|---|---|---|---|
| Age (years) | 68.14 ± 13.62 | 66.15 ± 11.66 | 0.431 | |
| Gender | F | 21 (50%) | 27 (34.6%) | 0.121 |
| M | 21 (50%) | 51 (65.4%) | ||
| BMI (kg/m2) | 25.67 ± 2.48 | 26.82 ± 5.79 | 0.449 | |
| Tobacco use | 3 (7.1%) | 3 (3.8%) | 0.700 | |
| Comorbidities: | ||||
| Hypertension | 30 (71.4%) | 36 (46.1%) | 0.007 | |
| Diabetes mellitus | 3 (7.1%) | 9 (11.5%) | 0.433 | |
| Chronic kidney disease | 6 (14.3%) | 2 (2.5%) | 0.017 | |
| Congestive heart failure | 15 (35.7%) | 12 (15.4%) | 0.013 | |
| Coronary heart disease | 12 (28.6%) | 15 (19.2%) | 0.248 | |
| Chronic respiratory disease | 6 (14.3%) | 12 (15.4%) | 0.872 | |
| Clinical characteristics: | ||||
| Onset of COVID-19 symptoms (days) | 5.3 ± 3.3 | 7.3 ± 3.8 | 0.01 | |
| Body Temperature (°C) | 36.8 ±0.8 | 37.2± 0.9 | 0.038 | |
| Heart rate (bpm) | 86.6 ± 7.4 | 85.8 ± 8.7 | 0.654 | |
| Respiratory rate (breaths/min) | 21.5 ± 8.1 | 23.1 ± 7.7 | 0.314 | |
| Dyspnea at rest (Nº of patients) | 12 (28.6%) | 45 (57.7%) | 0.02 | |
| SCBT | 30.4 ± 6.9 | 24.5 ± 6.4 | <0.0001 | |
| FiO2 | 0.2 ±0.02 | 0.3 ± 0.2 | 0.005 | |
| SpO2/FiO2 | 431.1 ± 39.1 | 357.8 ± 104.9 | 0.001 | |
| PaO2/FiO2 | 299.01 ± 95.1 | 235.1 ± 53.4 | 0.0001 | |
| PaCO2 (mmHg) | 40.1 ± 6.7 | 35.1 ± 4.1 | <0.0001 | |
| pH | 7.4 ± 0.02 | 7.5 ± 0.06 | 0.0001 | |
| D-dimer (mcg/mL) | 1.02 ± 0.8 | 0.9 ± 0.5 | 0.503 | |
| Ferritin (ng/mL) | 489.9 ± 440.5 | 993.9 ± 910.6 | 0.003 | |
| LDH (U/L) | 593.0 ± 107.2 | 698.9 ± 186.1 | 0.009 | |
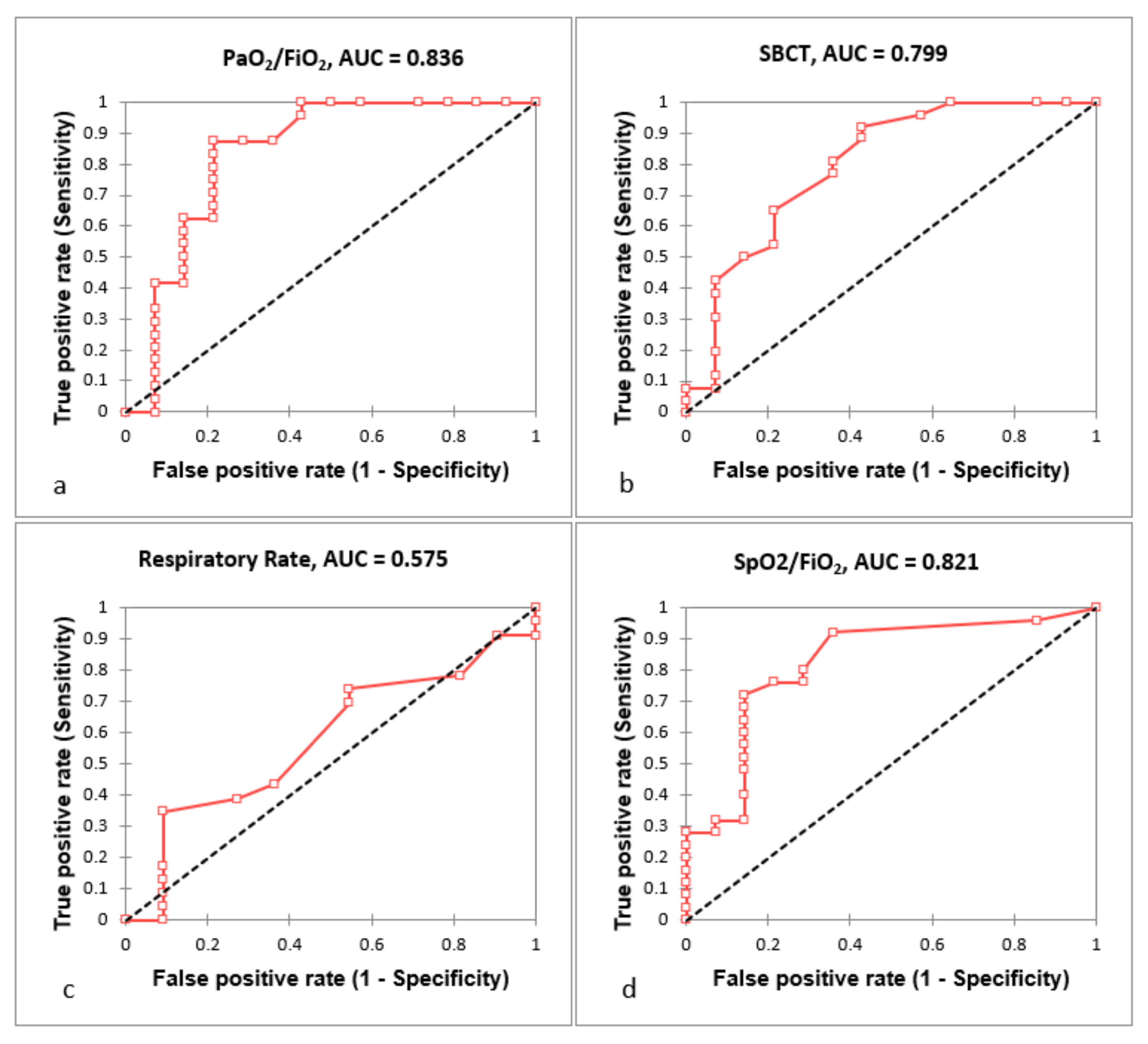
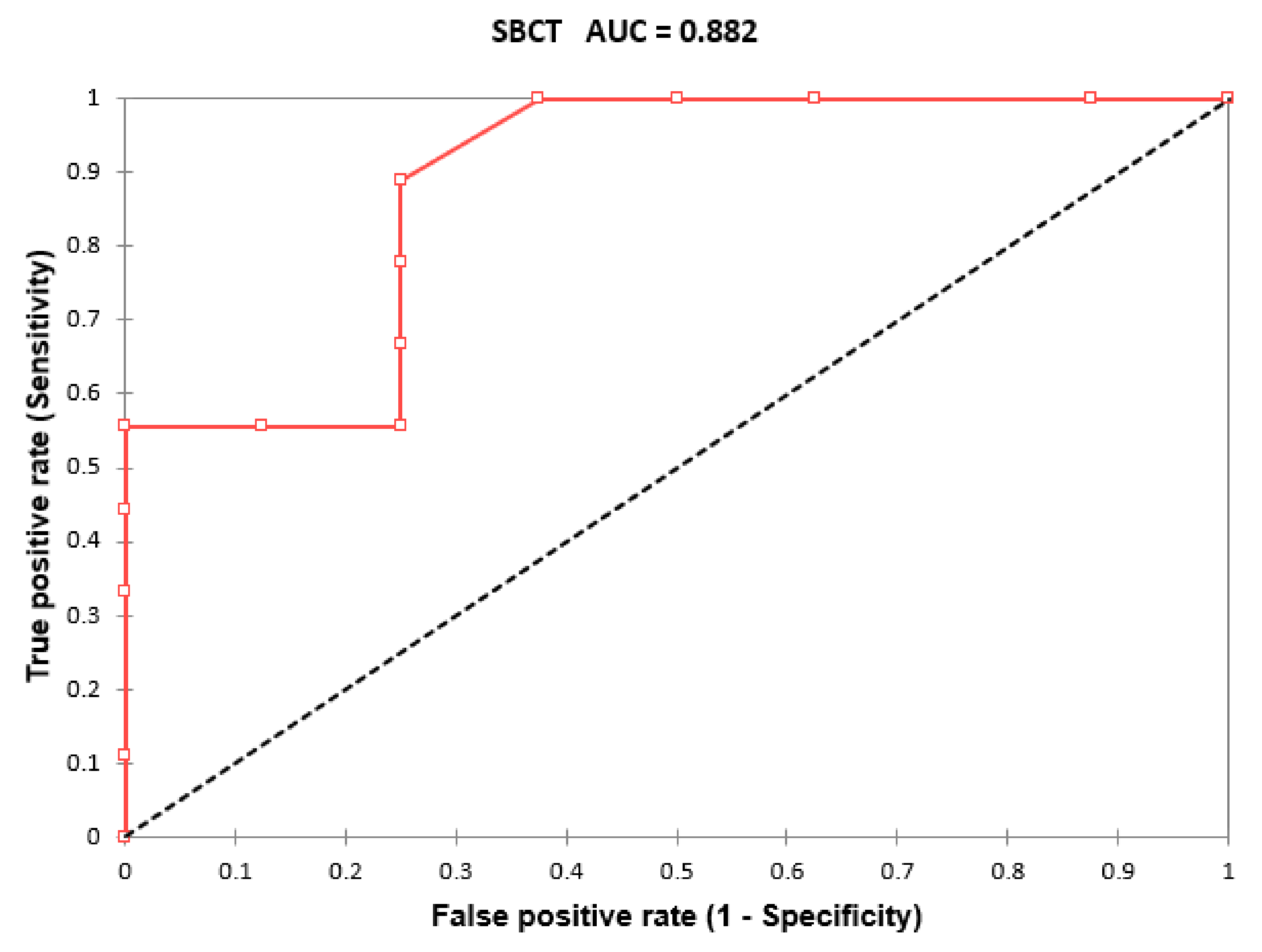
| AUC | Standard Error | Lower Bound (95%) | Upper Bound (95%) | Cut-Off | Sensitivity | Specificity | p-Value | |
|---|---|---|---|---|---|---|---|---|
| SBCT | 0.799 | 0.046 | 0.710 | 0.889 | 32 | 0.923 | 0.571 | <0.0001 |
| RR | 0.575 | 0.059 | 0.459 | 0.691 | 28 | 0.348 | 0.909 | 0.206 |
| PaO2/FiO2 | 0.836 | 0.057 | 0.725 | 0.948 | 280 | 0.875 | 0.786 | <0.0001 |
| SpO2/FiO2 | 0.821 | 0.052 | 0.720 | 0.923 | 438 | 0.720 | 0.857 | <0.0001 |
| SBCT in Patients Not Requiring NIRS | SBCT in Patients Requiring NIRS | p-Value | |
|---|---|---|---|
| Patients without chronic respiratory disease | 30.7 ± 7.5 | 25.3 ± 5.1 | <0.0001 |
| Patients not needing supplemental oxygen therapy | 30.1 ± 7.5 | 26.7 ± 3.0 | 0.007 |
| Patients needing supplemental oxygen therapy | 32.0 ± 0.0 | 20.8 ± 8.6 | 0.003 |
| Patients without dyspnea at rest | 31.5 ± 4.2 | 24.5 ± 3.2 | <0.0001 |
| Patients with PaO2/FiO2 > 280 | 29.7 ± 7.9 | 20.0 ± 6.6 | 0.0001 |
| Patients with SpO2/FiO2 > 438 | 30.1 ± 7.9 | 27.3 ± 3.8 | 0.135 |
| Patients with normal respiratory rate | 30.2 ± 8.1 | 25.1 ± 3.2 | 0.0001 |
| Patients with normal respiratory rate and absence of dyspnea at rest | 31.9 ± 4.5 | 25.1 ± 3.3 | <0.0001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Longhitano, Y.; Zanza, C.; Romenskaya, T.; Saviano, A.; Persiano, T.; Leo, M.; Piccioni, A.; Betti, M.; Maconi, A.; Pindinello, I.; et al. Single-Breath Counting Test Predicts Non-Invasive Respiratory Support Requirements in Patients with COVID-19 Pneumonia. J. Clin. Med. 2022, 11, 179. https://doi.org/10.3390/jcm11010179
Longhitano Y, Zanza C, Romenskaya T, Saviano A, Persiano T, Leo M, Piccioni A, Betti M, Maconi A, Pindinello I, et al. Single-Breath Counting Test Predicts Non-Invasive Respiratory Support Requirements in Patients with COVID-19 Pneumonia. Journal of Clinical Medicine. 2022; 11(1):179. https://doi.org/10.3390/jcm11010179
Chicago/Turabian StyleLonghitano, Yaroslava, Christian Zanza, Tatsiana Romenskaya, Angela Saviano, Tonia Persiano, Mirco Leo, Andrea Piccioni, Marta Betti, Antonio Maconi, Ivano Pindinello, and et al. 2022. "Single-Breath Counting Test Predicts Non-Invasive Respiratory Support Requirements in Patients with COVID-19 Pneumonia" Journal of Clinical Medicine 11, no. 1: 179. https://doi.org/10.3390/jcm11010179
APA StyleLonghitano, Y., Zanza, C., Romenskaya, T., Saviano, A., Persiano, T., Leo, M., Piccioni, A., Betti, M., Maconi, A., Pindinello, I., Boverio, R., Rello, J., Franceschi, F., & Racca, F. (2022). Single-Breath Counting Test Predicts Non-Invasive Respiratory Support Requirements in Patients with COVID-19 Pneumonia. Journal of Clinical Medicine, 11(1), 179. https://doi.org/10.3390/jcm11010179








