Evaluation of Functional Outcomes and Quality of Life in Elderly Patients (>75 y.o.) Undergoing Minimally Invasive Radical Cystectomy with Single Stoma Ureterocutaneostomy vs. Bricker Intracorporeal Ileal Conduit Urinary Diversion
Abstract
:1. Introduction
2. Materials and Methods
2.1. Bricker Ileal Conduit Diversion
2.2. Single Stoma Ureterocutaneostomy
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kirkali, Z.; Chan, T.; Manoharan, M.; Algaba, F.; Busch, C.; Cheng, L.; Kiemeney, L.; Kriegmair, M.; Montironi, R.; Murphy, W.M.; et al. Bladder cancer: Epidemiology, staging and grading, and diagnosis. Urology 2005, 66, 4–34. [Google Scholar] [CrossRef] [PubMed]
- Witjes, J.A.; Bruins, H.M.; Cathomas, R.; Compérat, E.; Cowan, N.C.; Gakis, G.; Hernández, V.; Lorchet, A.; Ribal, M.J.; Thalmann, G.N.; et al. EAU Guidelines on Muscle-Invasive and Metastatic Bladder Cancer. Eur. Assoc. Urol. 2021, 91, 82–104. [Google Scholar] [CrossRef] [PubMed]
- Babjuk, M.; Burger, M.; Compérat, E.M.; Gontero, P.; Mostafid, A.H.; Palou, J.; van Rhijn, B.W.G.; Roupret, M.; Shariat, S.F.; Sylvester, R.; et al. Guidelines on Non-muscle-invasive bladder cancer (Ta, T1 and CIS). In Proceedings of the 36th EAU Congress, Milan, Italy, 9–13 July 2021. [Google Scholar]
- Clavien, P.A.; Barkun, J.; de Oliviera, M.L.; Vauthey, J.N.; Dindo, D.; Schulick, R.D.; de Santibañes, E.; Pekolj, J.; Slankamenac, K.; Bassi, C.; et al. The Clavien-Dindo classification of surgical complications: Five-year experience. Ann. Surg. 2009, 250, 187–196. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Porter, M.P.; Penson, D.F. Health related quality of life after radical cystectomy and urinary diversion for bladder cancer: A systematic review and critical analysis of the literature. J. Urol. 2005, 173, 1318–1322. [Google Scholar] [CrossRef]
- Prieto, L.; Thorsen, H.; Juul, K. Development and validation of a quality-of-life questionnaire for patients with colostomy or ileostomy. Health Qual. Life Outcomes 2005, 3, 62. [Google Scholar] [CrossRef] [Green Version]
- Cella, D.F.; Tulsky, D.S.; Gray, G.; Sarafian, B.; Linn, E.; Bonomi, A.; Silberman, M.; Yellen, S.B.; Winicour, P.; Brannon, J. The Functional Assessment of Cancer Therapy scale: Development and validation of the general measure. J. Clin. Oncol. 1993, 11, 570–579. [Google Scholar] [CrossRef]
- Aaronson, N.K.; Ahmedzai, S.; Bergman, B.; Bullinger, M.; Cull, A.; Duez, N.J.; Filiberti, A.; Flechtner, H.; Fleishman, S.B.; De Haes, J.C.J.M.; et al. The European Organization for Research and Treatment of Cancer QLQ-C30: A quality-of-life instrument for use in international clinical trials in oncology. J. Natl. Cancer Inst. 1993, 85, 365–376. [Google Scholar] [CrossRef]
- Sogni, F.; Brausi, M.; Frea, B.; Martinengo, C.; Faggiano, F.; Tizzani, A.; Gontero, P. Morbidity and quality of life in elderly patients receiving ileal conduit or orthotopic neobladder after radical cystectomy for invasive bladder cancer. Urology 2008, 71, 919–923. [Google Scholar] [CrossRef]
- Ware, J.E., Jr.; Sherbourne, C.D. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med. Care 1992, 30, 473–483. [Google Scholar] [CrossRef]
- Ware, J.E., Jr.; Keller, S.D.; Gandek, B.; Brazier, J.E.; Sullivan, M. Evaluating translations of health status questionnaires. Methods from the IQOLA project. Int. J. Technol. Assess. Health Care 1995, 11, 525–551. [Google Scholar] [CrossRef]
- Gilbert, S.M.; Dunn, R.L.; Hollenbeck, B.K.; Montie, J.E.; Lee, C.T.; Wood, D.P.; Wei, J.T. Development and validation of the Bladder Cancer Index: A comprehensive, disease specific measure of health-related quality of life in patients with localized bladder cancer. J. Urol. 2010, 183, 1764–1770. [Google Scholar] [CrossRef] [PubMed]
- Deliveliotis, C.; Papatsoris, A.; Chrisofos, M.; Dellis, A.; Liakouras, C.; Skolarikos, A. Urinary diversion in high-risk elderly patients: Modified cutaneous ureterostomy or ileal conduit? Urology 2005, 66, 299–304. [Google Scholar] [CrossRef] [PubMed]
- Hollenbeck, B.K.; Miller, D.C.; Taub, D.; Dunn, R.L.; Underwood, W.; Montie, J.E.; Wei, J.T. Aggressive treatment for bladder cancer is associated with improved overall survival among patients 80 years old or older. Urology 2004, 64, 292–297. [Google Scholar] [CrossRef] [PubMed]
- Prout, G.R., Jr.; Wesley, M.N.; Yancik, R.; Ries, L.A.; Havlik, R.J.; Edwards, B.K. Age and comorbidity impact surgical therapy in older bladder carcinoma patients: A population-based study. Cancer 2005, 104, 1638–1647. [Google Scholar] [CrossRef]
- Izquierdo, L.; Peri, L.; Leon, P.; Ramírez-Backhaus, M.; Manning, T.; Alcaraz, A.; Rouprêt, M.; Solsona, E.; Rubio, J.; Sengupta, S.; et al. The role of cystectomy in elderly patients—A multicentre analysis. BJU Int. 2015, 116 (Suppl. S3), 73–79. [Google Scholar] [CrossRef] [Green Version]
- Nogueira, L.; Reis, R.; Machado, R.D.; Tobias-Machado, M.; Carvalhal, G.F.; Freitas, C., Jr.; Magnabosco, W.J.; Menezes, C.L.; Corradi, C.; Reis, L.; et al. Cutaneous ureterostomy with definitive ureteral stent as urinary diversion option in unfit patients after radical cystectomy. Acta Cir. Bras. 2013, 28, 43–47. [Google Scholar] [CrossRef]
- Siddiqui, K.M.; Izawa, J.I. Ileal conduit: Standard urinary diversion for elderly patients undergoing radical cystectomy. World J. Urol. 2016, 34, 19–24. [Google Scholar] [CrossRef]
- Mucciardi, G.; Macchione, L.; Gal, A.; Di Benedetto, A.; Subba, E.; Pappalardo, R.; Mucciardi, M.; Butticè, S.; Inferrera, A.; Magno, C. Quality of life and overall survival in high risk patients after radical cystectomy with a simple urinary derivation. Cir. Esp. 2015, 93, 368–374. [Google Scholar] [CrossRef]
- Chang, S.S.; Alberts, G.; Cookson, M.S.; Smith, J.A. Radical cystectomy is safe in elderly patients at high risk. J. Urol. 2001, 166, 938–941. [Google Scholar] [CrossRef]
- Liu, Z.; Meng, Y.; Li, S.; Yu, W.; Jin, J. Perioperative recovery in different urinary reconstruction approaches of radical cystectomy: Are the advantages of laparoscopy consistent? J. Minim. Access Surg. 2020, 16, 390–398. [Google Scholar]
- Mortezavi, A.; Crippa, A.; Edeling, S.; Pokupic, S.; Dell’Oglio, P.; Montorsi, F.; D’Hondt, F.; Mottrie, A.; Decaestecker, K.; Wijburg, C.J.; et al. Morbidity and mortality after robot-assisted radical cystectomy with intracorporeal urinary diversion in octogenarians: Results from the European Association of Urology Robotic Urology Section Scientific Working Group. BJU Int. 2020, 27, 585–595. [Google Scholar] [CrossRef] [PubMed]
- Miller, D.C.; Taub, D.A.; Dunn, R.L.; Montie, J.E.; Wei, J.T. The impact of co-morbid disease on cancer control and survival following radical cystectomy. J. Urol. 2003, 169, 105–109. [Google Scholar] [CrossRef]
- Kulkarni, J.N. Perioperative morbidity of radical cystectomy: A review. Indian J. Urol. 2011, 27, 226–232. [Google Scholar] [CrossRef] [PubMed]
- Longo, N.; Imbimbo, C.; Fusco, F.; Ficarra, V.; Mangiapia, F.; Di Lorenzo, G.; Creta, M.; Imperatore, V.; Mirone, V. Complications and quality of life in elderly patients with several comorbidities undergoing cutaneous ureterostomy with single stoma or ileal conduit after radical cystectomy. BJU Int. 2016, 118, 521–526. [Google Scholar] [CrossRef] [PubMed]
- De Nunzio, C.; Cicione, A.; Leonardo, F.; Rondoni, M.; Franco, G.; Cantiani, A.; Tubaro, A. Extraperitoneal radical cystectomy and ureterocutaneostomy in octogenarians. Int. Urol. Nephrol. 2011, 43, 663–667. [Google Scholar] [CrossRef]
- Ahmadi, H.; Lee, C.T. Health-related quality of life with urinary diversion. Curr. Opin. Urol. 2015, 25, 562–569. [Google Scholar] [CrossRef]
- Saika, T.; Arata, R.; Tsushima, T.; Nasu, Y.; Suyama, B.; Takeda, K.; Ebara, S.; Manabe, D.; Kobayashi, T.; Tanimoto, R.; et al. Health-related quality of life after radical cystectomy for bladder cancer in elderly patients with an ileal conduit, ureterocutaneostomy, or orthotopic urinary reservoir: A comparative questionnaire survey. Acta Med. Okayama 2007, 61, 199–203. [Google Scholar]
| Group A | Group B | p Value | |
|---|---|---|---|
| Patients, n. (m–f) | 37 (25–12) | 41 (28–13) | |
| Age, y.o. (ES) | 77.2 (0.97) | 82.4 (0.91) | 0.0005 |
| BMI, kg/m2 (ES) | 24.1 (0.64) | 23.2 (0.6) | 0.892 |
| ASA, (ES) | 2.4 (0.08) | 2.8 (0.075) | 0.029 |
| CCI, (ES) | 5.3 (0.11) | 6.4 (0.09) | 0.014 |
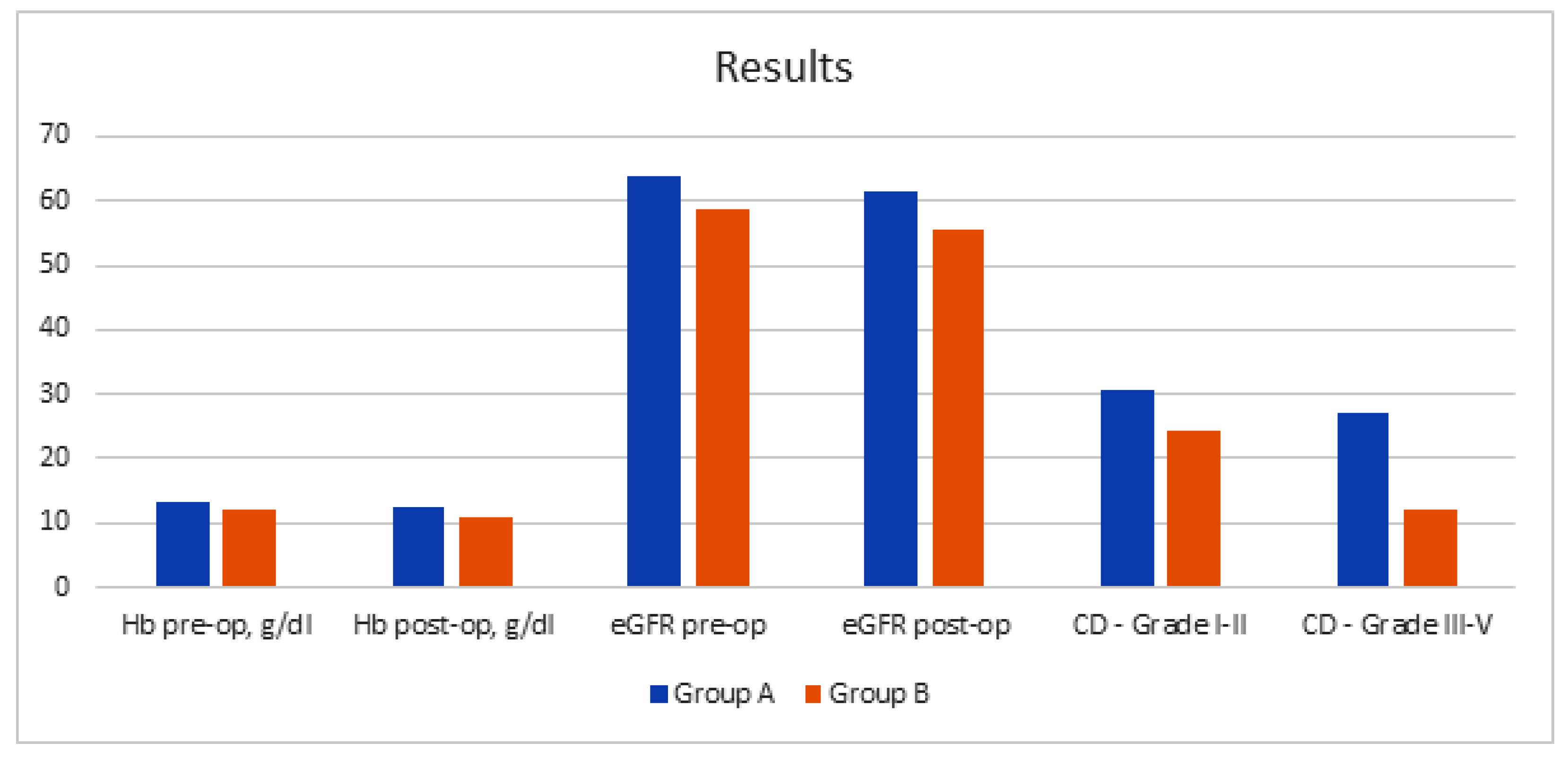
| Hb pre-op, g/dL (ES) | 13.4 (0.23) | 12.1 (0.28) | 0.084 |
| Hb post-op, g/dL (ES) | 12.4 (0.27) | 10.9 (0.31) | 0.071 |
| eGFR pre-op, (ES) | 63.8 (4.2) | 58.58 (4) | 0.375 |
| eGFR post-op, (ES) | 61.4 (3.8) | 55.52 (3.7) | 0.213 |
| Neoadjuvant CH, % | 33 | 30 | 0.311 |
| Total Operative Time, min (ES) | 334 (4.15) | 186 (3.89) | <0.0001 |
| Intra-op blood transfusion, % | 3.8 | 4.2 | 0.064 |
| Post-op blood transfusion, % | 6.8 | 8.4 | 0.041 |
| Intensive Care, days (ES) | 1.4 (0.07) | 1.6 (0.05) | 0.151 |
| Hospital Stay, days (ES) | 9.2 (0.67) | 6.5 (0.55) | 0.002 |
| Bowel function recovery, days (ES) | 3.6 (0.12) | 1.5 (0.04) | 0.0043 |
| Lymphnode involvement, % | 14.2 | 17.1 | 0.067 |
| Clavien–Dindo Classification, % | |||
| Grade I–II | 30.5 | 24.3 | 0.003 |
| Grade III–V | 27.1 | 12.1 | 0.0041 |
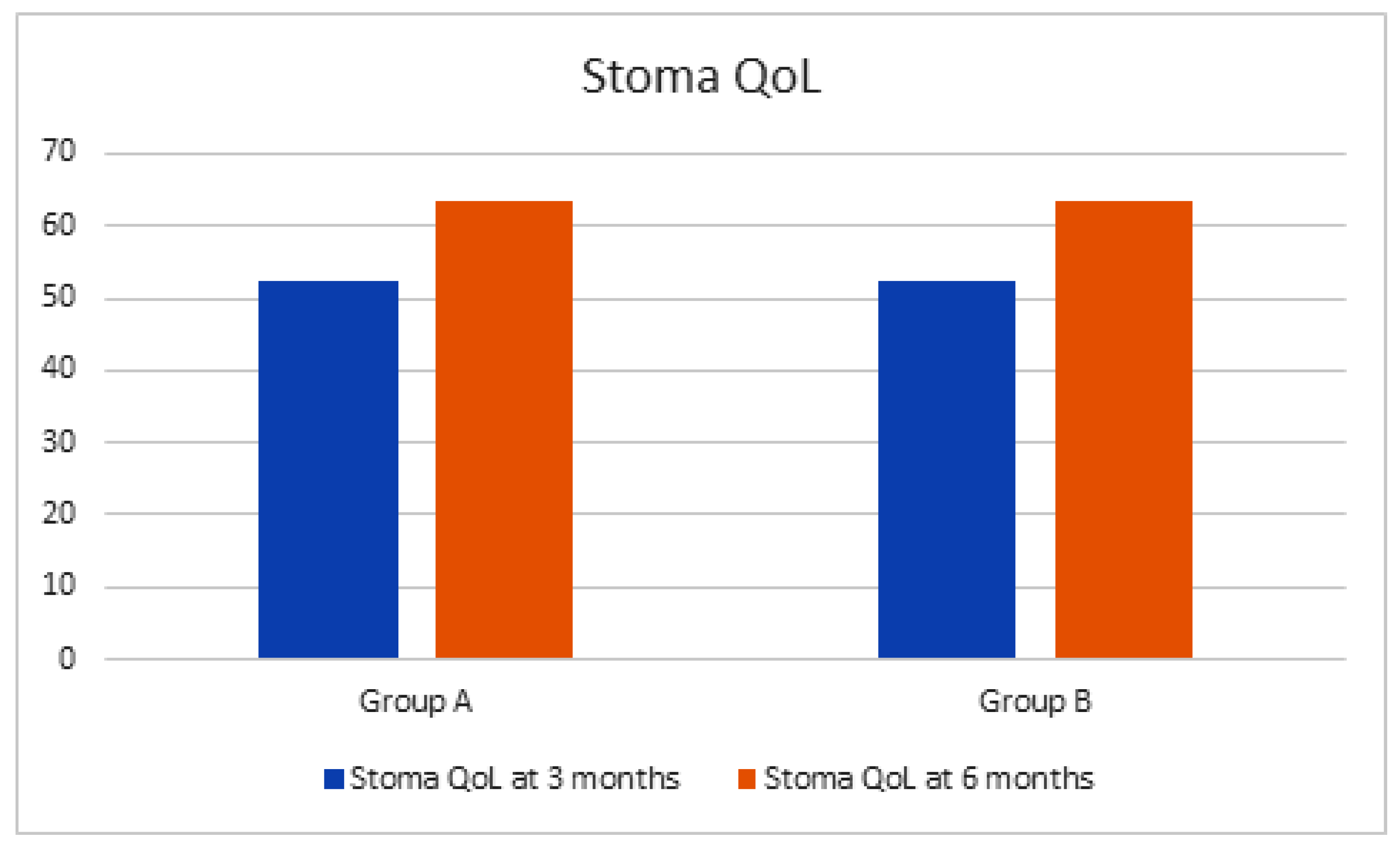
| Stoma QoL at 3 months, (ES) | 52.2 (1.61) | 52.4 (1.62 | 0.316 |
| Stoma QoL at 6 months, (ES) | 63.4 (1.84) | 63.6 (1.82) | 0.382 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fuschi, A.; Al Salhi, Y.; Sequi, M.B.; Velotti, G.; Martoccia, A.; Suraci, P.P.; Scalzo, S.; Asimakopoulos, A.; Bozzini, G.; Zucchi, A.; et al. Evaluation of Functional Outcomes and Quality of Life in Elderly Patients (>75 y.o.) Undergoing Minimally Invasive Radical Cystectomy with Single Stoma Ureterocutaneostomy vs. Bricker Intracorporeal Ileal Conduit Urinary Diversion. J. Clin. Med. 2022, 11, 136. https://doi.org/10.3390/jcm11010136
Fuschi A, Al Salhi Y, Sequi MB, Velotti G, Martoccia A, Suraci PP, Scalzo S, Asimakopoulos A, Bozzini G, Zucchi A, et al. Evaluation of Functional Outcomes and Quality of Life in Elderly Patients (>75 y.o.) Undergoing Minimally Invasive Radical Cystectomy with Single Stoma Ureterocutaneostomy vs. Bricker Intracorporeal Ileal Conduit Urinary Diversion. Journal of Clinical Medicine. 2022; 11(1):136. https://doi.org/10.3390/jcm11010136
Chicago/Turabian StyleFuschi, Andrea, Yazan Al Salhi, Manfredi Bruno Sequi, Gennaro Velotti, Alessia Martoccia, Paolo Pietro Suraci, Silvio Scalzo, Anastasios Asimakopoulos, Giorgio Bozzini, Alessandro Zucchi, and et al. 2022. "Evaluation of Functional Outcomes and Quality of Life in Elderly Patients (>75 y.o.) Undergoing Minimally Invasive Radical Cystectomy with Single Stoma Ureterocutaneostomy vs. Bricker Intracorporeal Ileal Conduit Urinary Diversion" Journal of Clinical Medicine 11, no. 1: 136. https://doi.org/10.3390/jcm11010136
APA StyleFuschi, A., Al Salhi, Y., Sequi, M. B., Velotti, G., Martoccia, A., Suraci, P. P., Scalzo, S., Asimakopoulos, A., Bozzini, G., Zucchi, A., De Nunzio, C., Carbone, A., & Pastore, A. L. (2022). Evaluation of Functional Outcomes and Quality of Life in Elderly Patients (>75 y.o.) Undergoing Minimally Invasive Radical Cystectomy with Single Stoma Ureterocutaneostomy vs. Bricker Intracorporeal Ileal Conduit Urinary Diversion. Journal of Clinical Medicine, 11(1), 136. https://doi.org/10.3390/jcm11010136







