1. Introduction
Tear drop (TD) fractures of the cervical spine are divided into flexion TD fractures caused by flexion-compression force and extension TD fractures (avulsion fracture) caused by hyperextension. Flexion TD fractures commonly occur at the C4–C7 (cervical) vertebra. In comparison, extension TD fractures occur more commonly at C2 or C3. Anterior TD fractures of the C2 vertebra are a relatively rare cervical spine injury. Its incidence is about 9–12% of upper cervical spine injuries and 1–3% of all cervical spine injuries [
1,
2,
3,
4,
5,
6]. Anterior C2 TD fractures are commonly caused by extension injury that differs in several ways from TD fractures in the lower cervical spine. To date, a few studies, including series with a small number of cases or case reports, have reported treatment methods and outcomes for anterior C2 TD fractures [
1,
2,
3,
4]. Most anterior C2 TD fractures can be successfully managed with conservative treatment because an extension TD fracture is more stable [
7,
8]. However, a close analysis of previous studies showed that anterior C2 TD fractures successfully managed with conservative treatment were small-sized or simple anterior TD fractures. Furthermore, a few case reports have suggested that if anterior C2 TD fractures are huge or massive, it is better to reconstruct the anterior column through surgery [
9,
10,
11,
12,
13,
14]. However, the exact criteria for determining indications for surgical treatment of large-sized anterior C2 TD fractures have not been provided and are controversial.
It has been our experience that the larger the fracture size is, or the greater the fracture displacement is, the more likely nonunion is to occur. To the best of our knowledge, however, no one has previously investigated the relationship between the fracture characteristics of anterior C2 TD fractures and nonunion outcomes. Moreover, there have been no studies examining factors that influence nonunion for conservatively managed anterior C2 TD fractures. Therefore, we performed the current study to suggest guidelines for determining surgical treatment of anterior C2 TD fractures.
2. Materials and Methods
A total of 60 patients with anterior or posterior TD fractures of the C2 body were identified from the databases of 4 national trauma centers housed at tertiary university hospitals between the years 2000 and 2017. The inclusion criteria for this study were as follows: acute trauma history, anterior C2 TD fracture as diagnosed using lateral X-ray and sagittal 2-dimensional (2-D) reconstructed computed tomography (CT) scan, conservative treatment, and a minimum 1-year follow-up. Among them, 33 patients met the inclusion criteria and were included in this study.
All 33 patients with anterior C2 TD fractures were divided into union or nonunion groups depending on fusion status at the 1-year follow-up point. Fusion status was evaluated by neutral, flexion, and extension lateral radiographs. The criteria for fusion were as follows: formation of a bony bridge and no motion between the anterior C2 TD fracture and the anteroinferior portion of the C2 body. Plain radiographs, 2-D reconstructed CT, magnetic resonance imaging (MRI), and medical records were analyzed retrospectively and the results between the two groups were compared.
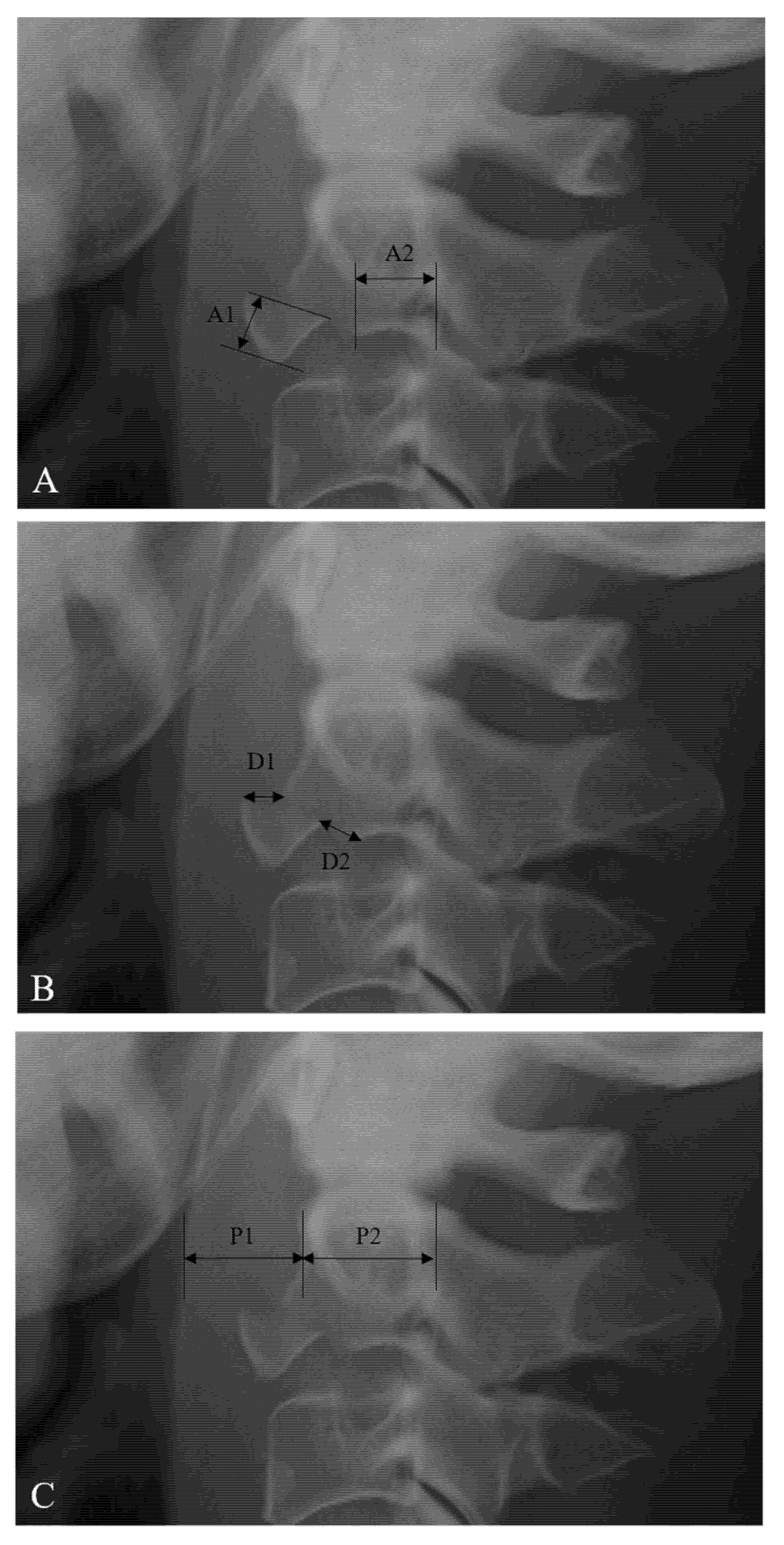
The avulsion fracture ratio of anterior C2 TD fractures was measured from lateral X-ray images (
Figure 1A) [
9]. The sagittal diameter of the inferior C2 endplate includes A1 and A2 (inferior endplate diameter of C2 TD fragment (A1) and remaining C2 body (A2)). The avulsion fracture ratio of anterior C2 TD fractures was defined as A1/(A1 + A2) × 100%. The fracture displacement of anterior C2 TD fractures was measured from lateral X-ray (
Figure 1B) [
7,
8,
9]. The displacement of the anterior C2 TD fragment was measured at the superior point (D1) and the posteroinferior point (D2). The fracture displacement of anterior C2 TD fractures was defined as (D1 + D2)/2. The prevertebral soft tissue thickness (PSVT) was measured from lateral X-ray (
Figure 1C) [
15]. The sagittal diameter of PSVT (P1) and the C2 body (P2) was measured at the C2 body midpoint. The ratio of PSVT was defined as P1/P2. The severity of PSVT at C2 was classified on a scale of grade 1 (mild, <0.4), grade 2 (moderate, 0.4–0.7), and grade 3 (severe, >0.7). The characteristics of the anterior C2 TD fractures, including associated C2 injury, associated C1 injury, associated C3–7 or thoracolumbar injuries, and neurologic status, were investigated. Clinical outcomes were evaluated using Odom’s criteria [
16] and the visual analog scale (VAS) for neck pain [
17]. All radiographic data were examined independently by two spine surgeons. Each independent observer checked the avulsion fracture ratio, fracture displacement, and severity of PSVT twice, and the average of the four measurements was used as the final result.
Statistical analysis was performed using the independent t-test, paired t-test, chi-squared test, and Pearson correlation test. A p-value of less than 0.05 was considered significant.
3. Results
3.1. Demographic Data
The mean age at the time of diagnosis was 51.6 years (range: 21–77 years). The mean follow-up period was 14.7 months (range: 12–43 months). Twenty-four patients were men and nine patients were women. Regarding the injury mechanism, 13 patients (39.4%) were involved in a traffic accident, 12 (36.4%) experienced a fall from height, and 8 (24.2%) slipped and fell. At admission, all 33 patients (100%) were neurologically intact. In terms of conservative treatment methods, 12 patients (36.4%) wore a Philadelphia brace, 14 patients (42.4%) wore a Miami brace, 5 patients (15.2%) wore a Minerva brace, and 2 patients (6.0%) wore a Halo vest.
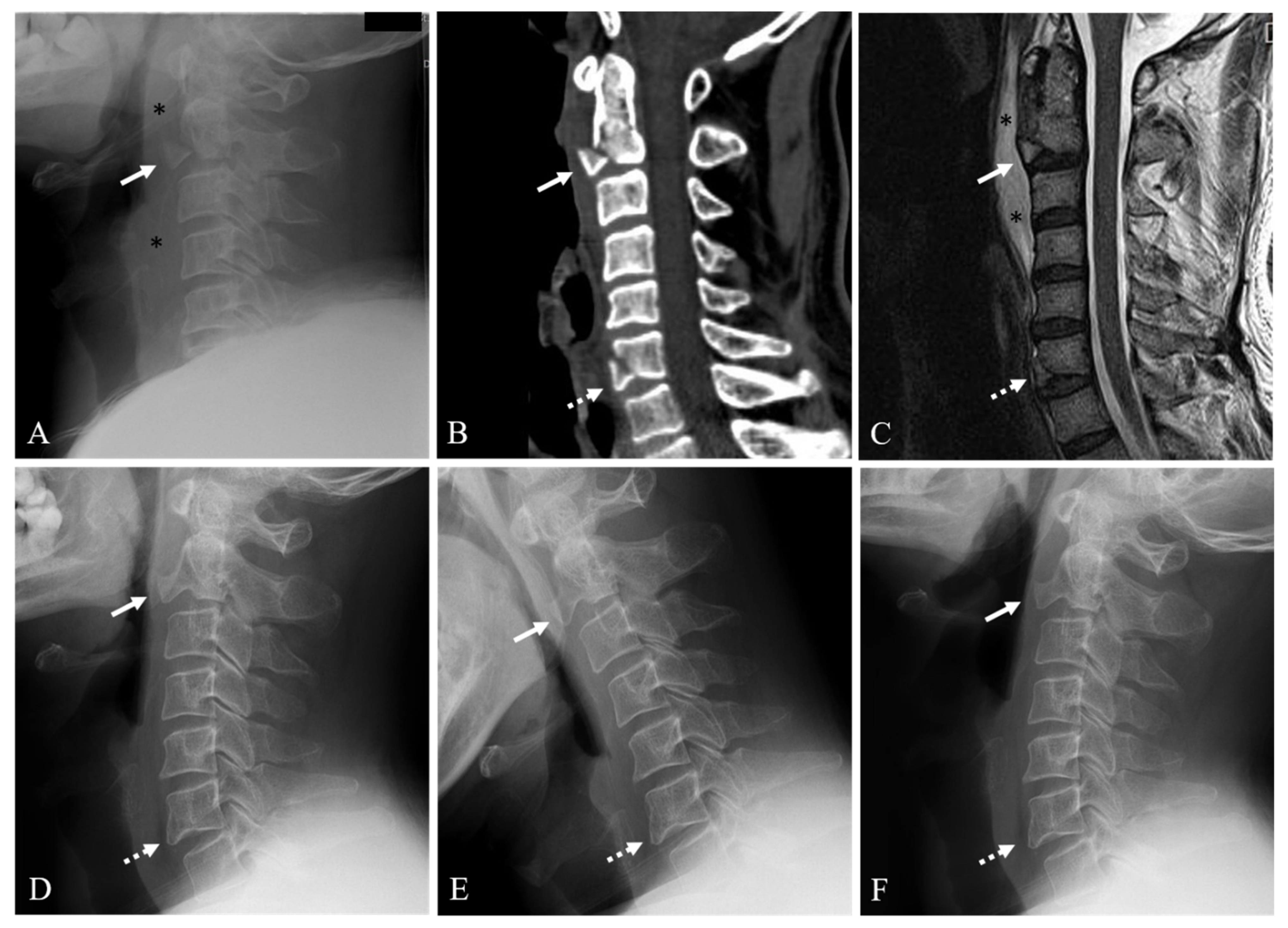
Twenty-six patients (78.8%) were in the union group (
Figure 2) and seven patients (21.2%) were in the nonunion group (
Figure 3). The demographic data and information for the union and nonunion groups of conservatively managed anterior C2 TD fractures are summarized in
Table 1. Mean age at the time of diagnosis was not statistically different between the union and nonunion groups (51.5 years vs. 51.9 years,
p = 0.961). Mean follow-up time was not statistically different between the union and nonunion groups (15.4 months vs. 12.0 months,
p = 0.282). At the time of diagnosis, all patients were neurologically intact.
3.2. Radiological Outcomes
The correlation coefficients for intra-observer reliability for avulsion fracture ratio, fracture displacement, and PSVT severity were 0.721, 0.725, and 0.743 (all, p < 0.001), respectively, which indicated a strong reliability. The correlation coefficients for inter-observer reliability for avulsion fracture ratio, fracture displacement, and PSVT severity were 0.581, 0.592, and 0.597 (all, p < 0.001), respectively, which indicated a moderate reliability. The avulsion fracture ratio was significantly higher in the nonunion group compared to the union group (29.5% vs. 43.3%, p < 0.05). Fracture displacement was significantly higher in the nonunion group compared to the union group (3.6 mm vs. 5.1 mm, p < 0.05). In terms of PSVT severity, 8 patients were grade 1 (30.8%), 4 patients were grade 2 (15.4%), and 14 patients were grade 3 (53.8%) in the union group. In the nonunion group, 2 patients were grade 1 (28.6%), 1 patient was grade 2 (14.3%), and 4 patients were grade 3 (57.1%); therefore, the PSVT severity was not statistically different between the two groups (p = 0.988). The incidence of associated C1 injury (3.8% vs. 12.5%, p = 0.421) and associated C3–7 or thoracolumbar injury (26.9% vs. 28.6%, p = 1.000) was not statistically different between the union and nonunion groups. However, the incidence of associated C2 injury was significantly higher in the nonunion group compared to the union group (15.4% vs. 57.1%, p < 0.05). The Pearson correlation test results showed that the union status in conservatively managed anterior C2 TD fractures was negatively correlated with associated C2 injury (correlation coefficient, CC = −0.398, p < 0.05).
3.3. Clinical Outcomes
According to clinical outcomes using Odom’s criteria, all 26 union patients showed excellent (
N = 16, 61.5%) and good (
N = 10, 38.5%) results. However, four nonunion patients (57.1%) showed good results and three nonunion patients (42.9%) showed fair results. The difference in satisfactory outcome was statistically significant between the union and nonunion groups (100% vs. 57.1%,
p < 0.001) (
Table 2). The VAS score for neck pain was significantly improved in the union group (4.1 vs. 1.2,
p < 0.001), but not in the nonunion group (4.3 vs. 3.6,
p = 0.094) (
Table 3). At the last follow-up, the VAS score for neck pain was significantly lower in the union group compared to the nonunion group (1.2 vs. 3.6,
p < 0.01). In terms of dysphagia, one patient complained of difficulty with swallowing solid foods due to displaced nonunion compressing the pharynx. However, the patient refused surgery. The remaining two patients with fair results did not want additional treatment despite the discomfort.
4. Discussion
4.1. Analysis of Our Results
In this study, we retrospectively analyzed clinical and radiological data of 33 anterior C2 TD fractures in patients who underwent conservative treatment and had a minimum 1-year follow-up. All 33 patients were assigned to the union group or the nonunion group based on their C2 union status at the 1-year follow-up time point. We found that the nonunion group had a higher avulsion fracture ratio of 43.3% and a fracture displacement of 5.1 mm; these findings were statistically significant compared to the union group. The nonunion group had a significantly higher incidence of associated C2 injury. Union status in conservatively managed anterior C2 TD fractures was negatively correlated with associated C2 injury. Finally, the nonunion group showed less satisfactory clinical outcomes compared to the union group. Based on the current findings, we suggest that surgical treatment could be considered for anterior C2 TD fractures with an avulsion fracture ratio > 43%, fracture displacement > 5 mm, or presence of an associated C2 injury. To the best of our knowledge, this is the first study to suggest guidelines for determining surgical treatment of anterior C2 TD fractures.
4.2. Outcomes of Previous Studies
In general, C2 fractures heal well with conservative treatment. In a review of the literature, the success rate of conservative treatment for C2 fractures was 78.4% [
18]. Like other C2 fractures, conservative treatment has been used as the standard treatment for anterior C2 TD fractures. Previous studies with mostly small case numbers and small-sized fractures have reported satisfactory outcomes for anterior C2 TD fractures managed conservatively [
4,
7,
8]. Kim et al. reported four extension-type C2 tear drop fractures out of 25 cervical tear drop fractures. They reported that all C2 tear drop fractures were well treated with conservative treatment [
19]. On the other hand, a few case reports have described surgical treatments for huge or large-sized anterior C2 TD fractures [
9,
10,
11,
12,
13,
14]. According to the review of the literature, as the fracture displacement of C2 increased, the proportion of nonunion after conservative treatment increased. In addition, when the fracture displacement was more than 5 mm, surgery was performed immediately [
18]. However, their suggestions were based on the overall C2 fracture, including dens fracture, and the exact criteria for surgical treatment of C2 anterior tear drop fracture were not provided.
4.3. Comparison with Previous Studies
In this study, the nonunion group of conservatively managed anterior C2 TD fractures showed a significantly higher avulsion fracture ratio of 43.3% compared to 29.5% in the union group. According to a few case reports [
9,
10,
11,
12,
13,
14] and case series with a small case number [
20,
21], anterior TD fractures that involve about 50% of the inferior C2 endplate need to be treated surgically to avoid nonunion. Our result showed a 7% lower avulsion fracture ratio compared to that in previous studies. In addition, our results were obtained with a larger number of cases through a multicenter study compared to prior studies. We believe the current study includes the largest number of cases of anterior C2 TD fractures compared to papers published so far. We also showed that nonunion may occur if the fracture displacement is over 5.1 mm, which was not mentioned in previous studies. These two radiological findings might be considered to cause nonunion of conservatively managed anterior C2 TD fractures and may serve as guidelines for determining surgical treatment of anterior C2 TD fractures.
4.4. Injury Mechanism and Associated Injuries
Anterior C2 TD fractures can occur alone or in conjunction with other associated spine injuries including C2, C1, and C3–7 or thoracolumbar spine. Since these injuries may have an effect on treatment methods and outcomes, special attention is needed to assess these associated injuries. Anterior C2 TD fracture is reported to be caused by extension injury. If the extension injury is more severe, anterior C2 TD fracture occurs, followed by C2 body or posterior bony elements. Anterior TD fractures are much more unstable if accompanied by fractures of the C2 body or posterior elements. If conservative treatment is performed in such cases, the risk of treatment failure is high and may lead to a displaced nonunion, such as that in
Figure 3. In our study, the nonunion group had a significantly higher incidence rate of associated C2 injury of 57.1% compared to 15.4% of the union group. In addition, the Pearson correlation test showed that union status was negatively correlated with associated C2 injury (CC = −0.398,
p < 0.05). The presence of associated C2 injury suggests that the C2 vertebra was in a more severely injured state due to the occurrence of multiple fractures. Therefore, the presence of this comorbid injury suggests a higher risk of nonunion if the anterior C2 TD fracture is treated conservatively. However, associated C1 injury, C3–7 injury, or thoracolumbar injuries were not statistically different between the union and nonunion groups. In addition, PSVT severity was not statistically different between the union and nonunion groups.
4.5. Limitation of Study
The limitations of this study include its retrospective nature. Like other retrospective multicenter studies, we could not completely exclude potential confounders associated with retrospective data collection and selection bias, such as initial treatment methods. In addition, further increase in the number of study subjects was limited by the rarity of this injury, even when pooling data from multiple centers.
5. Conclusions
Our results showed that an avulsion fracture ratio > 43%, a fracture displacement > 5 mm, or the presence of associated C2 injury can increase the risk of nonunion for conservatively managed anterior C2 TD fractures. Nonunion, in turn, was associated with inferior clinical outcomes. Therefore, we suggest that surgical treatment could be considered for anterior C2 TD fractures in the presence of these radiological findings.
Author Contributions
Conceptualization, S.-K.K.; Data curation, E.T.P. and H.-Y.S.; Formal analysis, S.-K.K.; Investigation, S.-K.K.; Methodology, S.-K.K.; Project administration, S.-K.K.; Resources, E.T.P. and H.-Y.S.; Supervision, S.-K.K.; Validation, S.-K.K.; Writing—original draft, S.-K.K.; Writing—review and editing, J.M.R. All authors have read and agreed to the published version of the manuscript.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Institutional Review Board of Chonnam national university hospital (CNUH-2020-337).
Informed Consent Statement
Patient consent was waived due to the retrospective study design and permission by Ethics Committee.
Data Availability Statement
All data presented in this study are available on demand from the corresponding author.
Acknowledgments
We thank Heui-Jeon Park and Kyung-Jin Song for providing valuable resources for this study. Additionally, this research was supported by the Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education (NRF2018R1D1A1A02086142).
Conflicts of Interest
The authors declare no conflict of interests.
References
- Pryputniewicz, D.M.; Hadley, M.N. Axis Fractures. Neurosurgery 2010, 66, A68–A82. [Google Scholar] [CrossRef]
- Korres, D.S.; Zoubos, A.B.; Kavadias, K.; Babis, G.C.; Balalis, K. The “tear drop” (or avulsed) fracture of the anterior inferior angle of the axis. Eur. Spine J. 1994, 3, 151–154. [Google Scholar] [CrossRef]
- Scher, A.T. ’Tear-drop’ fractures of the cervical spine—Radiological features. S. Afr. Med. J. 1982, 61, 355–356. [Google Scholar] [PubMed]
- Boran, S.; Hurson, C.; Gul, R.; Higgins, T.; Poynton, A.; O’Byrne, J.; McCormack, D. Functional outcome following teardrop fracture of the axis. Eur. J. Orthop. Surg. Traumatol. 2005, 15, 229–232. [Google Scholar] [CrossRef]
- Chan, H.H.; Segreto, F.A.; Horn, S.R.; Bortz, C.; Choy, G.G.; Passias, P.G.; Deverall, H.H.; Baker, J.F. C2 fractures in the elderly: Single-center evaluation of risk factors for mortality. Asian Spine J. 2019, 13, 746–752. [Google Scholar] [CrossRef]
- Moon, M.-S.; Choi, W.R.; Lim, H.G.; Lee, S.-Y.; Wi, S.M. Pavlov’s Ratio of the Cervical Spine in a Korean Population: A Comparative Study by Age in Patients with Minor Trauma without Neurologic Symptoms. Clin. Orthop. Surg. 2021, 13, 71–75. [Google Scholar] [CrossRef] [PubMed]
- Watanabe, M.; Sakai, D.; Yamamoto, Y.; Sato, M.; Mochida, J. Clinical features of the extension teardrop fracture of the axis: Review of 13 cases. J. Neurosurg. Spine 2011, 14, 710–714. [Google Scholar] [CrossRef] [PubMed]
- Hu, Y.; Kepler, C.K.; Albert, T.J.; Hann, S.; Ma, W.-H.; Yuan, Z.-S.; Dong, W.-X.; Xu, R.-M. Conservative and Operative Treatment in Extension Teardrop Fractures of the Axis. Clin. Spine Surg. 2016, 29, E49–E54. [Google Scholar] [CrossRef]
- Jiang, T.; Yin, H.; Ren, X.J.; Chu, T.; Wang, W.; Li, C. Anterior reduction and fusion for treatment of massive tear drop fracture of axis combing with inferior endplate serious traversed lesion: A retrospective study. J. Orthop. Sci. 2017, 22, 816–821. [Google Scholar] [CrossRef]
- Yang, X.; Zheng, B.; Hao, D.; Liu, B.; Yan, L.; He, B. Treating Huge Tear-Drop Fracture of Axis with Trapezoidal Bone. Spine 2015, 40, E1187–E1190. [Google Scholar] [CrossRef] [PubMed]
- Xu, G.; Li, W.; Bao, G.; Sun, Y.; Wang, L.; Cui, Z. Tear drop fracture of the axis in a child with an 8-year follow-up: A case report. J. Pediatr. Orthop. B 2014, 23, 299–305. [Google Scholar] [CrossRef] [PubMed]
- Ma, L.; Yang, Y.; Gong, Q.; Ding, C.; Liu, H.; Hong, Y. Anterior Reduction, Discectomy, and Three Cortical Iliac Bone Grafting with Instrumentation to Treat A Huge Tear Drop Fracture of the Axis. Medicine 2016, 95, e3376. [Google Scholar] [CrossRef] [PubMed]
- Vialle, R.; Schmider, L.; Levassor, N.; Rillardon, L.; Drain, O.; Guigui, P. Extension tear-drop fracture of the axis. A surgically treated case. Rev. Chir. Orthop. Reparatrice L’appareil Mot. 2004, 90, 152–155. [Google Scholar] [CrossRef]
- Deniz, F.E.; Cağli, S.; Zileli, M. Compressive hyperextension injury of C2-C3 managed with anterior plate fixation: Case report. Turk. Neurosurg. 2007, 17, 125–128. [Google Scholar]
- Shiau, J.-P.; Chin, C.-C.; Yeh, C.-N.; Chen, J.-F.; Lee, S.-T.; Fang, J.-F.; Liao, C.-C. Does the ratio and thickness of prevertebral soft tissue provide benefit in blunt cervical spine injury? Eur. J. Trauma Emerg. Surg. 2013, 39, 297–303. [Google Scholar] [CrossRef]
- Odom, G.L.; Finney, W.; Woodhall, B. CERVICAL DISK LESIONS. J. Am. Med Assoc. 1958, 166, 23–28. [Google Scholar] [CrossRef]
- Gift, A.G. Visual analogue scales: Measurement of subjective phenomena. Nurs. Res. 1989, 38, 286–288. [Google Scholar] [CrossRef] [PubMed]
- Gembruch, O.; Lemonas, E.; Ahmadipour, Y.; Sure, U.; El Hindy, N.; Müller, O. Nonoperative management of C-2 dens fractures: Single center experience and review of the literature. Clin. Neurol. Neurosurg. 2018, 169, 166–173. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.J.; Lee, K.Y.; Kim, W.C. Treatment Outcome of Cervical Tear Drop Fracture. Asian Spine J. 2009, 3, 73–79. [Google Scholar] [CrossRef] [PubMed]
- Xin, X.; Zhang, Y.; Jin, T.; Liu, X. Zero-profile implantation combined with miniscrew fixation via anterior approach for huge teardrop fracture of axis. World Neurosurg. 2019, 128, 235–239. [Google Scholar] [CrossRef]
- Wang, L.; Xia, T.; Dong, S.; Zhao, Q.; Tian, J. Surgical treatment of complex axis fractures with adjacent segment instability. J. Clin. Neurosci. 2012, 19, 380–387. [Google Scholar] [CrossRef] [PubMed]
| Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).