Tinnitus and Neuropsychological Dysfunction in the Elderly: A Systematic Review on Possible Links
Abstract
1. Introduction
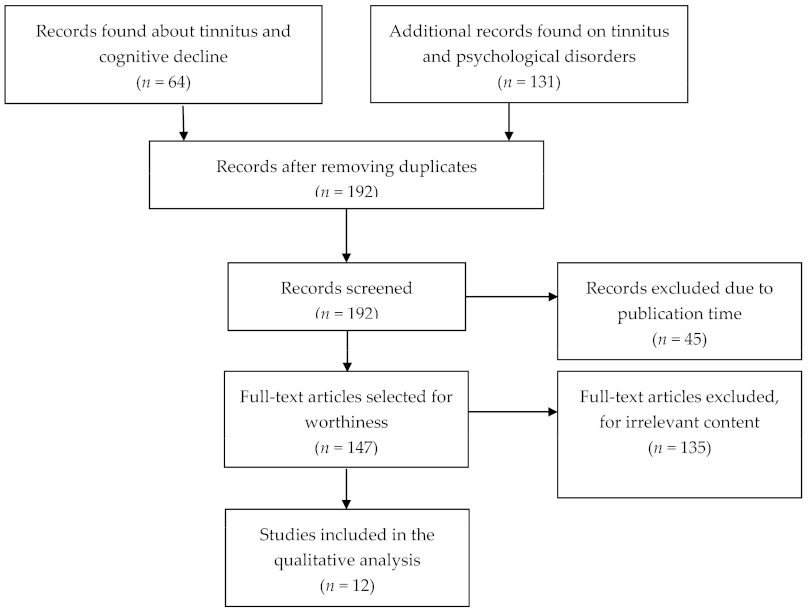
2. Methods
2.1. Study Selection
2.2. Qualitative Analysis
3. Results
3.1. Psychological Distress
3.2. Cognitive Impairment
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Sindhusake, D.; Mitchell, P.; Newall, P.; Golding, M.; Rochtchina, E.; Rubin, G. Prevalence and characteristics of tinnitus in older adults: The Blue Mountains Hearing Study: Prevalencia y características del acúfeno en adultos mayores: El Estudio de Audición Blue Mountains. Int. J. Audiol. 2003, 42, 289–294. [Google Scholar] [CrossRef] [PubMed]
- Ralli, M.; Balla, M.P.; Greco, A.; Altissimi, G.; Ricci, P.; Turchetta, R.; De Virgilio, A.; De Vincentiis, M.; Ricci, S.; Cianfrone, G. Work-Related Noise Exposure in a Cohort of Patients with Chronic Tinnitus: Analysis of Demographic and Audiological Characteristics. Int. J. Environ. Res. Public Health 2017, 14, 1035. [Google Scholar] [CrossRef] [PubMed]
- Paciello, F.; Podda, M.V.; Rolesi, R.; Cocco, S.; Petrosini, L.; Troiani, D.; Fetoni, A.R.; Paludetti, G.; Grassi, C. Anodal transcranial direct current stimulation affects auditory cortex plasticity in normal-hearing and noise-exposed rats. Brain Stimul. 2018, 11, 1008–1023. [Google Scholar] [CrossRef] [PubMed]
- Skarzynski, P.H.; Dziendziel, B.; Gos, E.; Wlodarczyk, E.; Miaskiewicz, B.; Rajchel, J.J.; Skarzynski, H. Prevalence and Severity of Tinnitus in Otosclerosis: Preliminary Findings from Validated Questionnaires. J. Int. Adv. Otol. 2019, 15, 277–282. [Google Scholar] [CrossRef] [PubMed]
- Nakashima, T.; Pyykkö, I.; Arroll, M.A.; Casselbrant, M.L.; Foster, C.A.; Manzoor, N.F.; Megerian, C.A.; Naganawa, S.; Young, Y.-H. Meniere’s disease. Nat. Rev. Dis. Prim. 2016, 2, 16028. [Google Scholar] [CrossRef] [PubMed]
- Cascella, V.; Giordano, P.; Hatzopoulos, S.; Petruccelli, J.; Prosser, S.; Simoni, E.; Astolfi, L.; Fetoni, A.R.; Skarżyński, H.; Martini, A. A new oral otoprotective agent. Part 1: Electrophysiology data from protection against noise-induced hearing loss. Med. Sci. Monit. 2012, 18, BR1–BR8. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Huang, Y.-S.; Koo, M.; Chen, J.-C.; Hwang, J.-H. The association between tinnitus and the risk of ischemic cerebrovascular disease in young and middle-aged patients: A secondary case-control analysis of a nationwide, population-based health claims database. PLoS ONE 2017, 12, e0187474. [Google Scholar] [CrossRef] [PubMed]
- Shih, C.-P.; Lin, H.-C.; Chung, C.-H.; Hsiao, P.-J.; Wang, C.-H.; Lee, J.-C.; Chien, W.-C. Increased risk of tinnitus in patients with chronic kidney disease: A nationwide, population-based cohort study. PLoS ONE 2017, 12, e0183192. [Google Scholar] [CrossRef] [PubMed]
- Ralli, M.; Lobarinas, E.; Fetoni, A.R.; Stolzberg, D.; Paludetti, G.; Salvi, R. Comparison of Salicylate- and Quinine-Induced Tinnitus in Rats. Otol. Neurotol. 2010, 31, 823–831. [Google Scholar] [CrossRef]
- Hwang, J.-H.; Tsai, S.-J.; Liu, T.-C.; Chen, Y.-C.; Lai, J.-T. Association of Tinnitus and Other Cochlear Disorders with a History of Migraines. JAMA Otolaryngol. Neck Surg. 2018, 144, 712–717. [Google Scholar] [CrossRef]
- Knipper, M.; Van Dijk, P.; Nunes, I.; Rüttiger, L.; Zimmermann, U. Advances in the neurobiology of hearing disorders: Recent developments regarding the basis of tinnitus and hyperacusis. Prog. Neurobiol. 2013, 111, 17–33. [Google Scholar] [CrossRef]
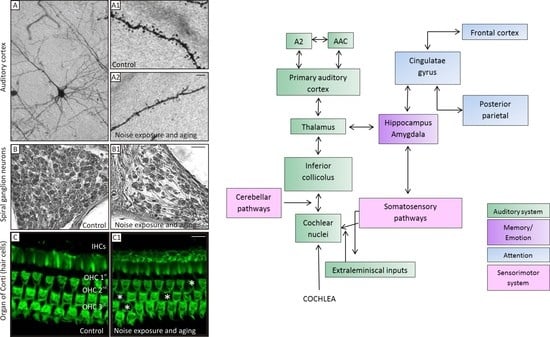
- Fetoni, A.R.; Etroiani, D.; Epetrosini, L.; Epaludetti, G. Cochlear Injury and Adaptive Plasticity of the Auditory Cortex. Front. Aging Neurosci. 2015, 7, 8. [Google Scholar] [CrossRef]
- Stolzberg, D.; Chen, G.-D.; Allman, B.; Salvi, R. Salicylate-induced peripheral auditory changes and tonotopic reorganization of auditory cortex. Neuroscience 2011, 180, 157–164. [Google Scholar] [CrossRef]
- Salvi, R.J.; Wang, J.; Ding, D. Auditory plasticity and hyperactivity following cochlear damage. Hear. Res. 2000, 147, 261–274. [Google Scholar] [CrossRef]
- Diesch, E.; Andermann, M.; Flor, H.; Rupp, A. Interaction among the components of multiple auditory steady-state responses: Enhancement in tinnitus patients, inhibition in controls. Neuroscience 2010, 167, 540–553. [Google Scholar] [CrossRef]
- Vanneste, S.; De Ridder, D. The auditory and non-auditory brain areas involved in tinnitus. An emergent property of multiple parallel overlapping subnetworks. Front. Syst. Neurosci. 2012, 6, 31. [Google Scholar] [CrossRef]
- Hébert, S.; Fournier, P.; Noreña, A. The Auditory Sensitivity is Increased in Tinnitus Ears. J. Neurosci. 2013, 33, 2356–2364. [Google Scholar] [CrossRef]
- Rauschecker, J.P.; Leaver, A.M.; Mühlau, M. Tuning Out the Noise: Limbic-Auditory Interactions in Tinnitus. Neuron 2010, 66, 819–826. [Google Scholar] [CrossRef]
- Araneda, R.; De Volder, A.G.; Deggouj, N.; Philippot, P.; Heeren, A.; Lacroix, E.; Decat, M.; Rombaux, P.; Renier, L. Altered top-down cognitive control and auditory processing in tinnitus: Evidences from auditory and visual spatial stroop. Restor. Neurol. Neurosci. 2015, 33, 67–80. [Google Scholar] [CrossRef]
- Wang, Y.; Zhang, J.-N.; Hu, W.; Li, J.-J.; Zhou, J.-X.; Shi, G.-F.; He, P.; Li, Z.-W.; Li, M. The characteristics of cognitive impairment in subjective chronic tinnitus. Brain Behav. 2018, 8, e00918. [Google Scholar] [CrossRef]
- De Corso, E.; Cantone, E.; Galli, J.; Seccia, V.; Lucidi, D.; Di Cesare, T.; Ottaviano, G.; Sergi, B.; Paludetti, G.; Fetoni, A.R. Otitis media in children: Which phenotypes are most linked to allergy? A systematic review. Pediatr. Allergy Immunol. 2021, 32, 524–534. [Google Scholar] [CrossRef]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: Explanation and elaboration. BMJ 2009, 339, b2700. [Google Scholar] [CrossRef]
- Fetoni, A.R.; Di Cesare, T.; Settimi, S.; Sergi, B.; Rossi, G.; Malesci, R.; Marra, C.; Paludetti, G.; De Corso, E. The evaluation of global cognitive and emotional status of older patients with chronic tinnitus. Brain Behav. 2021, in press. [Google Scholar]
- Aazh, H.; Lammaing, K.; Moore, B.C.J. Factors related to tinnitus and hyperacusis handicap in older people. Int. J. Audiol. 2017, 56, 677–684. [Google Scholar] [CrossRef]
- Park, S.Y.; Han, J.J.; Hwang, J.H.; Whang, E.S.; Yeo, S.W.; Park, S.N. Comparison of tinnitus and psychological aspects between the younger and older adult patients with tinnitus. Auris Nasus Larynx 2017, 44, 147–151. [Google Scholar] [CrossRef]
- Gopinath, B.; McMahon, C.M.; Rochtchina, E.; Karpa, M.J.; Mitchell, P. Risk factors and impacts of incident tinnitus in older adults. Ann. Epidemiol. 2010, 20, 129–135. [Google Scholar] [CrossRef]
- Lasisi, A.O.; Abiona, T.; Gureje, O. Tinnitus in the elderly: Profile, correlates, and impact in the Nigerian study of ageing. Otolaryngol. Head Neck Surg. 2010, 143, 510–515. [Google Scholar] [CrossRef]
- Loprinzi, P.D.; Maskalick, S.; Brown, K.; Gilham, B. Association between depression and tinnitus in a nationally representative sample of US older adults. Aging Ment. Health 2013, 17, 714–717. [Google Scholar] [CrossRef]
- Beukes, E.W.; Baguley, D.M.; Allen, P.M.; Manchaiah, V.; Andersson, G. Audiologist-Guided Internet-Based Cognitive Behavior Therapy for Adults With Tinnitus in the United Kingdom: A Randomized Controlled Trial. Ear Hear. 2018, 39, 423–433. [Google Scholar] [CrossRef]
- Park, H.-M.; Jung, J.; Kim, J.-K.; Lee, Y.-J. Tinnitus and Its Association with Mental Health and Health-Related Quality of Life in an Older Population: A Nationwide Cross-Sectional Study. J. Appl. Gerontol. 2020, 733464820966512. [Google Scholar] [CrossRef]
- Lee, S.-Y.; Kim, H.; Lee, J.Y.; Kim, J.H.; Lee, D.Y.; Mook-Jung, I.; Kim, Y.H.; Kim, Y.K. Effects of Chronic Tinnitus on Metabolic and Structural Changes in Subjects With Mild Cognitive Impairment. Front. Aging Neurosci. 2020, 12, 594282. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.-Y.; Lee, J.Y.; Han, S.-Y.; Seo, Y.; Shim, Y.J.; Kim, Y.H. Neurocognition of Aged Patients with Chronic Tinnitus: Focus on Mild Cognitive Impairment. Clin. Exp. Otorhinolaryngol. 2020, 13, 8–14. [Google Scholar] [CrossRef] [PubMed]
- Yun, Y.; Lee, S.-Y.; Choi, W.H.; Park, J.-C.; Lee, D.H.; Kim, Y.K.; Lee, J.H.; Lee, J.-Y.; Lee, M.J.; Kim, Y.H. Proteasome Activity in the Plasma as a Novel Biomarker in Mild Cognitive Impairment with Chronic Tinnitus. J. Alzheimer’s Dis. 2020, 78, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Ruan, Q.; Chen, J.; Zhang, R.; Zhang, W.; Ruan, J.; Zhang, M.; Han, C.; Yu, Z. Heterogeneous Influence of Frailty Phenotypes in Age-Related Hearing Loss and Tinnitus in Chinese Older Adults: An Explorative Study. Front. Psychol. 2021, 11, 617610. [Google Scholar] [CrossRef]
- Fetoni, A.R.; Lucidi, D.; De Corso, E.; Fiorita, A.; Conti, G.; Paludetti, G. Relationship between Subjective Tinnitus Perception and Psychiatric Discomfort. Int. Tinnitus J. 2016, 20, 76–82. [Google Scholar] [CrossRef]
- Panza, F.; Solfrizzi, V.; Logroscino, G. Age-related hearing impairment—A risk factor and frailty marker for dementia and AD. Nat. Rev. Neurol. 2015, 11, 166–175. [Google Scholar] [CrossRef]
- Pattyn, T.; Eede, F.V.D.; Vanneste, S.; Cassiers, L.; Veltman, D.; Van De Heyning, P.; Sabbe, B. Tinnitus and anxiety disorders: A review. Hear. Res. 2016, 333, 255–265. [Google Scholar] [CrossRef]
- Taljaard, D.S.; Olaithe, M.; Brennan-Jones, C.G.; Eikelboom, R.H.; Bucks, R.S. The relationship between hearing impairment and cognitive function: A meta-analysis in adults. Clin. Otolaryngol. 2016, 41, 718–729. [Google Scholar] [CrossRef]
- Trevis, K.J.; McLachlan, N.M.; Wilson, S.J. Cognitive Mechanisms in Chronic Tinnitus: Psychological Markers of a Failure to Switch Attention. Front. Psychol. 2016, 7, 1262. [Google Scholar] [CrossRef]
- Mohamad, N.; Hoare, D.J.; Hall, D.A. The consequences of tinnitus and tinnitus severity on cognition: A review of the behavioural evidence. Hear. Res. 2016, 332, 199–209. [Google Scholar] [CrossRef]
- De Ridder, D.; Schlee, W.; Vanneste, S.; Londero, A.; Weisz, N.; Kleinjung, T.; Shekhawat, G.S.; Elgoyhen, A.B.; Song, J.-J.; Andersson, G.; et al. Tinnitus and tinnitus disorder: Theoretical and operational definitions (an international multidisciplinary proposal). Neuroendocrinol. Pathol. Situa. Dis. 2021, 260, 1–25. [Google Scholar] [CrossRef]
- Fortunato, S.; Forli, F.; Guglielmi, V.; De Corso, E.; Paludetti, G.; Berrettini, S.; FetonI, A. Ipoacusia e declino cognitivo: Revisione della letteratura. Acta Otorhinolaryngol. Ital. 2016, 36, 155–166. [Google Scholar] [CrossRef]
- Wingfield, A.; Grossman, M. Language and the Aging Brain: Patterns of Neural Compensation Revealed by Functional Brain Imaging. J. Neurophysiol. 2006, 96, 2830–2839. [Google Scholar] [CrossRef]
- Peelle, J.E.; Wingfield, A. The Neural Consequences of Age-Related Hearing Loss. Trends Neurosci. 2016, 39, 486–497. [Google Scholar] [CrossRef]
- Tangalos, E.G.; Petersen, R.C. Mild Cognitive Impairment in Geriatrics. Clin. Geriatr. Med. 2018, 34, 563–589. [Google Scholar] [CrossRef]
- Anzivino, R.; Conti, G.; Di Nardo, W.; Fetoni, A.R.; Picciotti, P.M.; Marra, C.; Guglielmi, V.; Fortunato, S.; Forli, F.; Paludetti, G.; et al. Prospective Evaluation of Cognitive Functions after Rehabilitation with Cochlear Implant or Hearing Aids: Preliminary Results of a Multicentric Study on Elderly Patients. Am. J. Audiol. 2019, 28, 762–774. [Google Scholar] [CrossRef]
- Guglielmi, V.; Marra, C.; Picciotti, P.M.; Iacobucci, G.M.; Giovannini, S.; Quaranta, D.; Anzivino, R.; Paludetti, G.; Conti, G. Does Hearing Loss in the Elderly Individuals Conform to Impairment of Specific Cognitive Domains? J. Geriatr. Psychiatry Neurol. 2019, 33, 231–240. [Google Scholar] [CrossRef]
- Savastano, M. Tinnitus with or without hearing loss: Are its characteristics different? Eur. Arch. Otorhinolaryngol. 2008, 265, 1295–1300. [Google Scholar] [CrossRef]
- Mazurek, B.; Olze, H.; Haupt, H.; Szczepek, A.J. The More the Worse: The Grade of Noise-Induced Hearing Loss Associates with the Severity of Tinnitus. Int. J. Environ. Res. Public Health 2010, 7, 3071–3079. [Google Scholar] [CrossRef]
- Deary, I.J.; Corley, J.; Gow, A.J.; Harris, S.E.; Houlihan, L.M.; Marioni, R.E.; Penke, L.; Rafnsson, S.B.; Starr, J.M. Age-associated cognitive decline. Br. Med Bull. 2009, 92, 135–152. [Google Scholar] [CrossRef]
- Harada, C.N.; Love, M.C.N.; Triebel, K.L. Normal Cognitive Aging. Clin. Geriatr. Med. 2013, 29, 737–752. [Google Scholar] [CrossRef]
- Shahidipour, Z.; Geshani, A.; Jafari, Z.; Jalaie, S.; Khosravifard, E. Auditory memory deficit in elderly people with hearing loss. Iran J. Otorhinolaryngol. 2013, 25, 169–176. [Google Scholar]
- Aghamolaei, M.; Jafari, Z.; Grimm, S.; Zarnowiec, K.; Najafi-Koopaie, M.; Escera, C. The effects of aging on early stages of the auditory deviance detection system. Clin. Neurophysiol. 2018, 129, 2252–2258. [Google Scholar] [CrossRef]
- Livingston, G.; Sommerlad, A.; Orgeta, V.; Costafreda, S.G.; Huntley, J.; Ames, D.; Ballard, C.; Banerjee, S.; Burns, A.; Cohen-Mansfield, J.; et al. Dementia prevention, intervention, and care. Lancet 2017, 390, 2673–2734. [Google Scholar] [CrossRef]
- Loughrey, D.G.; Kelly, M.E.; Kelley, G.A.; Brennan, S.; Lawlor, B.A. Association of Age-Related Hearing Loss With Cognitive Function, Cognitive Impairment, and Dementia. JAMA Otolaryngol. Neck Surg. 2018, 144, 115–126. [Google Scholar] [CrossRef] [PubMed]
| Author, Year [Ref] | Inclusion Criteria | Exclusion Criteria | N° of Cases, Age | Type of Study | Objective | Methods (Outcome Evaluation) | Results | Level of Evidence | Evidence of Association |
|---|---|---|---|---|---|---|---|---|---|
| Fetoni AR, 2021 [23] | -Chronic tinnitus -Age ≥ 55 y -With or without HL | -History of neurological diseases -Psychiatric disorders -Otologic diseases-Antipsychotic drugs use | 102 patients ≥55 y; 70.4 ± 9.6 y (range 55–94 y | Prospective cross-sectional study | To assess the value of self-administered screening tests in comparing severity of tinnitus perception with emotional disorders and cognitive status | THI, HADS, MMSE (questionnaires) | THI score related to HADS-A score, HADS-D score, there was no relationship between tinnitus severity and MMSE | II | Yes |
| Aazh H, 2017 [24] | -Age ≥ 60 y -Tinnitus sufferers with/without hyperacusis -With/without HL | History of neurologic and psychiatric diseases, or sleep disorders | 184 patients ≥60 y; mean age of 69 y | Retrospective cross-sectional study | To assess issues associated with tinnitus and hyperacusis handicap | HADS, HQ, ISI, THI, VAS (questionnaires) | THI was significant in predicting tinnitus annoyance. Hyperacusis handicap and insomnia were both predicted by level of depression | III | Yes |
| Park SY, 2017 [25] | -Age < and ≥ 65 y -With/without HL | History of psychiatric or neurologic diseases | 76 patients ≥65 y | Retrospective cohort study | To assess differences between tinnitus-related features and psychological aspects between younger and older tinnitus sufferers | THI, BDI, and BEPSI (questionnaires) | No differences in tinnitus severity, depression, and stress between younger and older subjects | III | Yes/No |
| Gopinath B, 2010 [26] | -Age ≥ 50 y -With/without tinnitus -With/without HL | History of psychiatric diseases | 1214 participants (602 with tinnitus) ≥50 y | Longitudinal cohort study | To evaluate the risk factors and effects of tinnitus (depression) | SF-36; MHI for depression and/or CES-D (questionnaires) | Lessened quality of life and wellbeing in patients with tinnitus | II | Yes |
| Lasisi AO, 2010 [27] | -Age ≥ 65 y -With/without tinnitus; -With/without HL | History of neuropsychologic diseases | 184 patients ≥65 y; mean age of 77.3 y | Longitudinal cohort study | To establish the prevalence of tinnitus in the elderly and its influence on their life quality | WHOQOL (questionnaire) | Tinnitus sufferers had a lower perception of their overall health and a worse life quality; twofold likelihood to suffer activities impairment in daily living | II | Yes |
| Loprinzi PD, 2013 [28] | -Age ≥ 70 y -With/without tinnitus -With/without HL | Age < 70 years old | 696 patients 76 ± 0.2 y (range 70–85 y) | Prospective cross-sectional study | To evaluate the association between tinnitus and depression | Patient Health Questionnaire-9 (questionnaire) | Positive association between tinnitus (at least a moderate) and depression; patients bothered by tinnitus before going to bed were nearly 3 times more likely to be depressed | II | Yes, in moderate/severe tinnitus |
| Beukes EW, 2018 [29] | -Age< and > 60 y -Chronic tinnitus -With/without HL who completed therapy | History of neuropsychiatric diseases | 146 patientsstratified for age (> 60 y) | A randomized, delayed intervention efficacy trial | To establish if an internet-based cognitive behavioral therapy is useful in reducing tinnitus severity and associated comorbidities | ISI, Generalized Anxiety Disorder-7, Patient Health Questionnaire-9, Hearing Handicap Inventory for adults, HQ, Cognitive Failures Questionnaire, Satisfaction with Life Scales (questionnaires | Significant reduction in tinnitus and comorbidities (insomnia, depression, hyperacusis, cognitive failures) and improving of life quality | I | Yes |
| Park HM, 2020 [30] | -Age ≥ 60 y -With/without tinnitus -With/without HL | History of neurologic or psychiatric diseases | 5129 patients ≥60 y (range 60–79 y) | Retrospective cross-sectional study | To find a possible association of tinnitus, mental health, and health-related quality of life | Stress was tested asking: “How much stress do you usually feel in your daily life?”; depression was tested using CIDI-SF; suicide ideation with the question: “Have you ever thought about committing suicide within 12 months?” (questionnaires) | The annoying tinnitus patients had more depression, psychological stress, and suicidal ideation if compared to control group | III | Yes |
| Author, Year [Ref] | Inclusion Criteria | Exclusion Criteria | N° of Cases, Age | Type of Study | Objective | Methods (Outcome Evaluation) | Results | Level of Evidence | Evidence of Association |
|---|---|---|---|---|---|---|---|---|---|
| Lee SY, 2020 [31] | -Age > 60 y -Diagnosed for MCI -With/without tinnitus | -Moderate or severe hearing loss -Otologic diseases -History of psychiatric or neurologic disorders | 23 patients (12 with tinnitus) 74.0 ± 6.1 y (range 63–83 y) | Retrospective cohort study | To examine the glucose metabolism and gray matter volume in patients with MCI and tinnitus | MCI with or without tinnitus: FDG-PET and magnetic resonance imaging were performed (imaging) | Specific brain regions are associated with cognitive decline and increased tinnitus severity | III | Yes |
| Lee SY, 2020 [32] | -Age ≥ 65 y -With/without HL | History of psychiatric or neurologic disorders | 58 patients68.1 ± 5.1 y (range 65–82 y) | Prospective cohort study | To examine the cognitive domains and the association between tinnitus severity and cognitive functions | K-PHQ-9, K-IADL, MoCA-K (questionnaires) | THI score in the MCI group was higher than in the non-MCI | II | Yes |
| Yun Y, 2020 [33] | -Age > 50 y -Chronic tinnitus | -History of Alzheimer’s disease or neurologic diseases -Hearing loss or otologic diseases | 55 patients > 50 y | Cross-sectional study | To examine plasma c-proteasome activity in association with cognitive functions in chronic tinnitus patients | Plasma c-proteasome activity was achieved with fluorogenic reporter substrate; MoCA (cut-off score of 22/23) to assess MCI (markers and questionnaires) | Circulating proteasomes were lower in patients with chronic tinnitus and MCI | III | Yes |
| Fetoni AR, 2021 [23] | -Chronic tinnitus -Age ≥ 55 y -With/without HL | -History of neurological diseases -Psychiatric disorders -Otologic diseases-Antipsychotic drugs use | 102 patients ≥ 55 y | Prospective cross-sectional study | To evaluate the use of self-administered screening tests to correlate the severity of tinnitus with emotional disorders and the overall cognitive status | THI, HADS, MMSE (questionnaires) | THI score was directly related to HADS score, there was no relationship between tinnitus severity and MMSE | II | No |
| Beukes EW, 2018 [29] | -Age < and > 60 y -Chronic tinnitus-With/without HL -Who completed therapy | History of neuropsychiatric diseases | 146 patients stratified for age (>60 y) | Randomized delayed intervention efficacy trial | To establish if an internet-based cognitive behavioral therapy is useful to lessen tinnitus severity and associated comorbidities | ISI, Generalized Anxiety Disorder, Patient Health Questionnaire, Hearing Handicap Inventory for Adults Screening version, HQ, Cognitive Failures Questionnaire, Satisfaction with Life Scales (questionnaires) | Significant reduction in tinnitus and comorbidities (insomnia, depression, hyperacusis, cognitive failures) and a significant rise in life quality | I | Yes |
| Ruan Q, 2021 [34] | -Age ≥ 58 y -With/without frailty -With/without HL -With/without tinnitus | No history of disability, cophosis, and vision loss | 429 patients ≥58 y | Longitudinal cohort study | To study whether cognitive frailty is associated with HL and tinnitus | To assess MCI: with executive and attention domain (TMT A and B); language domain (BNT and animal list generation); memory domain (HVLT-R) (questionnaires) | Cognitive frailty patients had higher risks of severe HL and tinnitus. Cognitive impairment in tinnitus patients involved executive, memory, and attention domains; altered processing speed | II | Yes/No |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Malesci, R.; Brigato, F.; Di Cesare, T.; Del Vecchio, V.; Laria, C.; De Corso, E.; Fetoni, A.R. Tinnitus and Neuropsychological Dysfunction in the Elderly: A Systematic Review on Possible Links. J. Clin. Med. 2021, 10, 1881. https://doi.org/10.3390/jcm10091881
Malesci R, Brigato F, Di Cesare T, Del Vecchio V, Laria C, De Corso E, Fetoni AR. Tinnitus and Neuropsychological Dysfunction in the Elderly: A Systematic Review on Possible Links. Journal of Clinical Medicine. 2021; 10(9):1881. https://doi.org/10.3390/jcm10091881
Chicago/Turabian StyleMalesci, Rita, Francesca Brigato, Tiziana Di Cesare, Valeria Del Vecchio, Carla Laria, Eugenio De Corso, and Anna Rita Fetoni. 2021. "Tinnitus and Neuropsychological Dysfunction in the Elderly: A Systematic Review on Possible Links" Journal of Clinical Medicine 10, no. 9: 1881. https://doi.org/10.3390/jcm10091881
APA StyleMalesci, R., Brigato, F., Di Cesare, T., Del Vecchio, V., Laria, C., De Corso, E., & Fetoni, A. R. (2021). Tinnitus and Neuropsychological Dysfunction in the Elderly: A Systematic Review on Possible Links. Journal of Clinical Medicine, 10(9), 1881. https://doi.org/10.3390/jcm10091881