Vertical Bite Rehabilitation of Severely Worn Dentitions with Direct Composite Restorations: Clinical Performance up to 11 Years
Abstract
1. Introduction
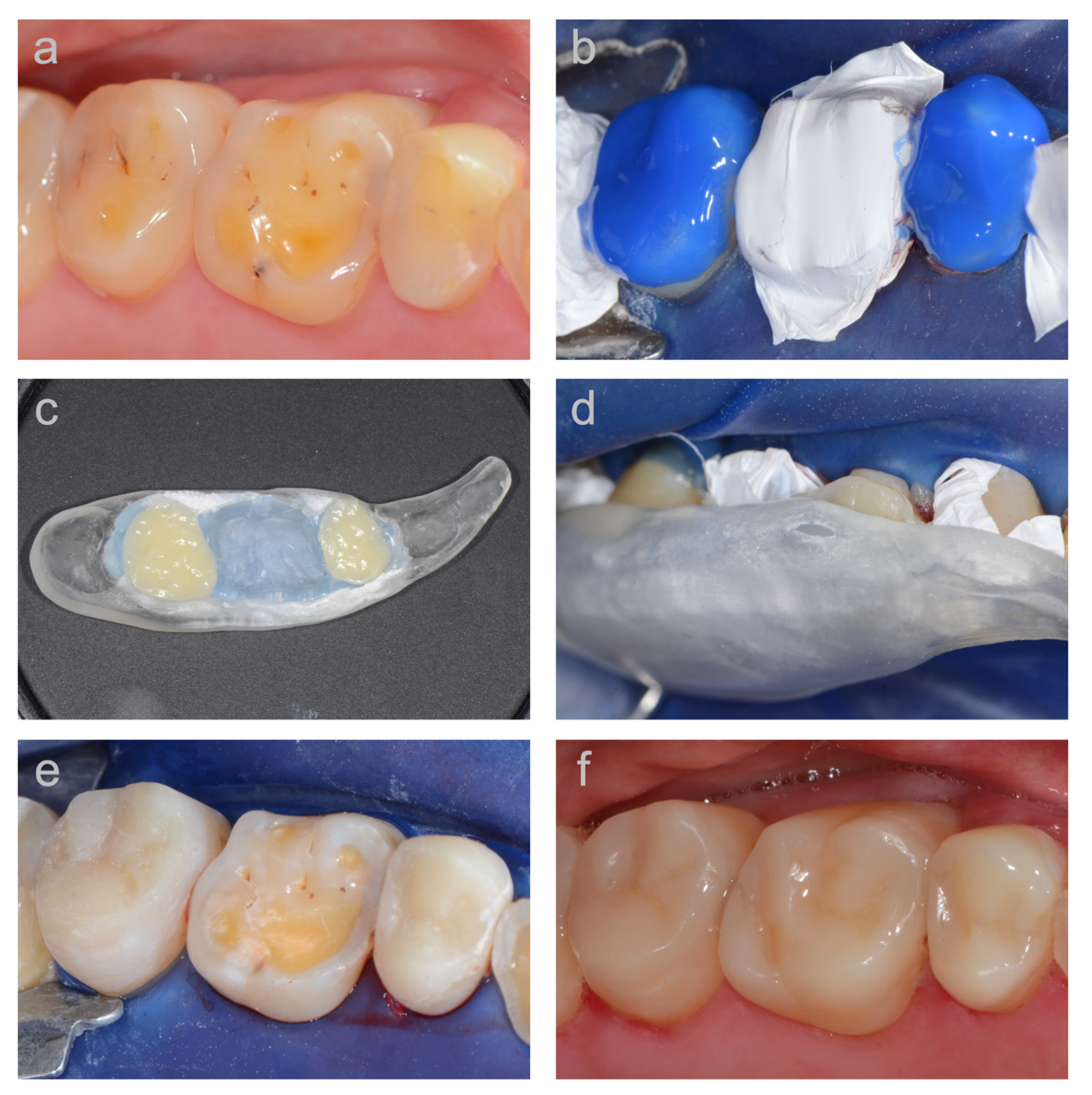
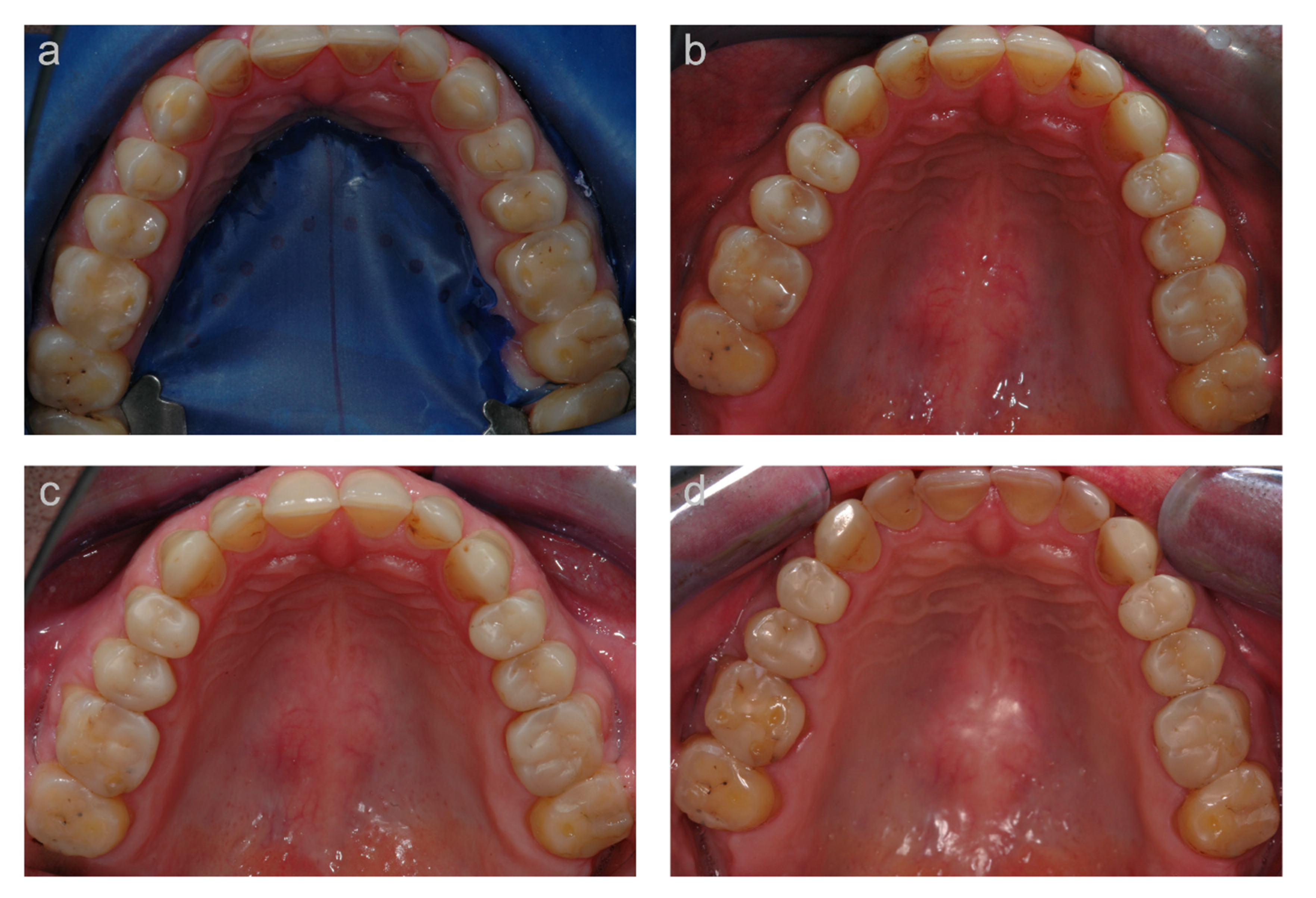
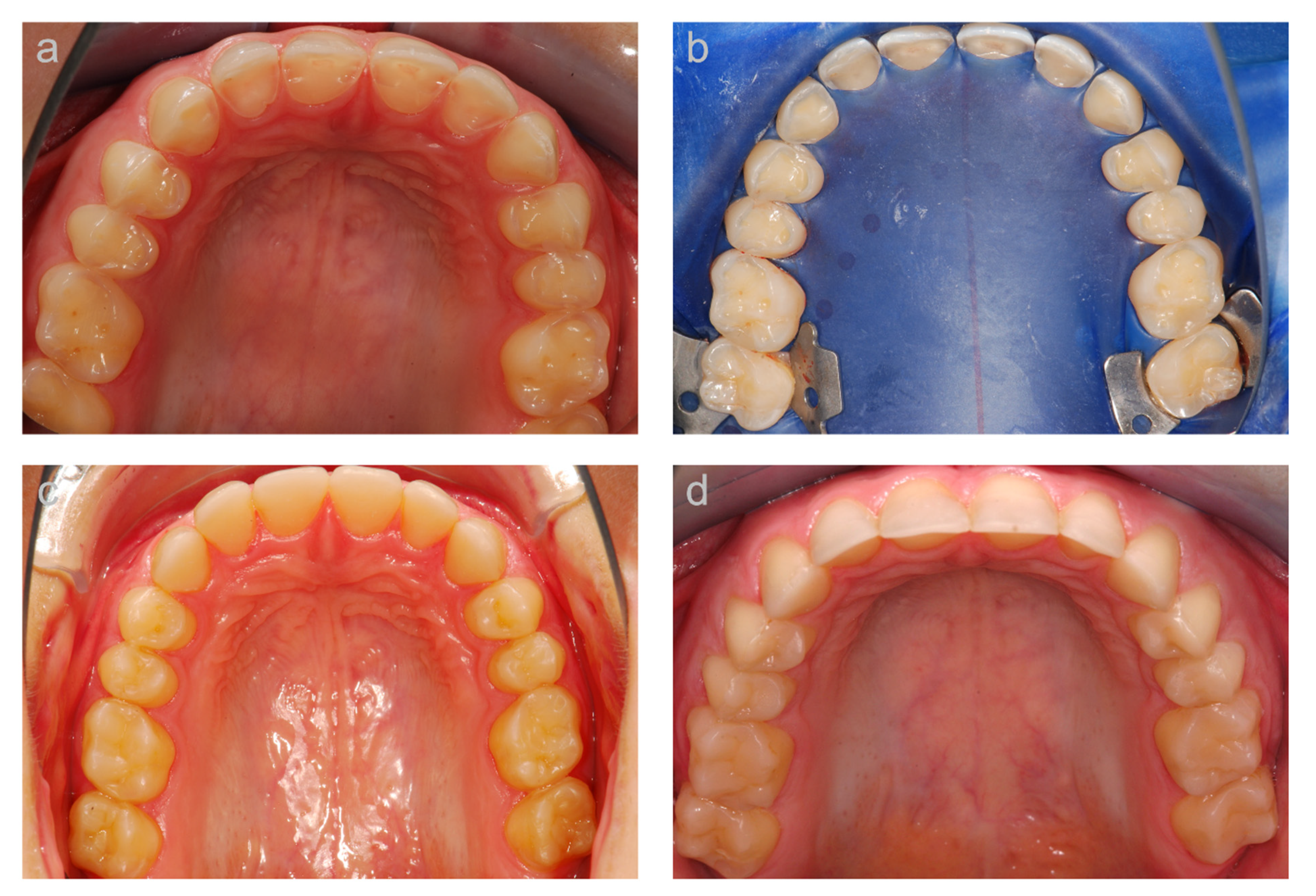
2. Materials and Methods
2.1. Patients and Treatment
2.2. Clinical Evaluation
2.3. Patient Satisfaction/Compliance
3. Results
3.1. First (Long-Term) Cohort
3.2. Second (Medium-Term) Cohort
3.3. Patient Satisfaction/Compliance
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Attin, T.; Becker, K.; Wiegand, A.; Tauböck, T.T.; Wegehaupt, F.J. Impact of laminar flow velocity of different acids on enamel calcium loss. Clin. Oral Investig. 2013, 17, 595–600. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Shellis, R.P.; Addy, M. The interactions between attrition, abrasion and erosion in tooth wear. Monogr. Oral Sci. 2014, 25, 32–45. [Google Scholar] [PubMed]
- Van’t Spijker, A.; Rodriguez, J.M.; Kreulen, C.M.; Bronkhorst, E.M.; Bartlett, D.W.; Creugers, N.H. Prevalence of tooth wear in adults. Int. J. Prosthodont. 2009, 22, 35–42. [Google Scholar] [PubMed]
- Jaeggi, T.; Lussi, A. Prevalence, incidence and distribution of erosion. Monogr. Oral Sci. 2014, 25, 55–73. [Google Scholar]
- Wetselaar, P.; Vermaire, J.H.; Visscher, C.M.; Lobbezoo, F.; Schuller, A.A. The prevalence of tooth wear in the dutch adult population. Caries Res. 2016, 50, 543–550. [Google Scholar] [CrossRef] [PubMed]
- Peutzfeldt, A.; Jaeggi, T.; Lussi, A. Restorative therapy of erosive lesions. Monogr. Oral Sci. 2014, 25, 253–261. [Google Scholar]
- Al-Omiri, M.K.; Lamey, P.J.; Clifford, T. Impact of tooth wear on daily living. Int. J. Prosthodont. 2006, 19, 601–605. [Google Scholar] [PubMed]
- Van Roekel, N.B. Gastroesophageal reflux disease, tooth erosion, and prosthodontic rehabilitation: A clinical report. J. Prosthodont. 2003, 12, 255–259. [Google Scholar] [CrossRef]
- Kavoura, V.; Kourtis, S.G.; Zoidis, P.; Andritsakis, D.P.; Doukoudakis, A. Full-mouth rehabilitation of a patient with bulimia nervosa. A case report. Quintessence Int. 2005, 36, 501–510. [Google Scholar]
- Nam, J.; Tokutomi, H. Using zirconia-based prosthesis in a complete-mouth reconstruction treatment for worn dentition with the altered vertical dimension of occlusion. J. Prosthet. Dent. 2015, 113, 81–85. [Google Scholar] [CrossRef]
- Loomans, B.; Opdam, N.; Attin, T.; Bartlett, D.; Edelhoff, D.; Frankenberger, R.; Benic, G.; Ramseyer, S.; Wetselaar, P.; Sterenborg, B.; et al. Severe Tooth Wear: European Consensus Statement on Management Guidelines. J. Adhes. Dent. 2017, 19, 111–119. [Google Scholar]
- Wegehaupt, F.J.; Tauböck, T.T.; Attin, T. How to re-seal previously sealed dentin. Am. J. Dent. 2013, 26, 161–165. [Google Scholar]
- Dieckmann, P.; Baur, A.; Dalvai, V.; Wiedemeier, D.B.; Attin, T.; Tauböck, T.T. Effect of composite age on the repair bond strength after different mechanical surface pretreatments. J. Adhes. Dent. 2020, 22, 365–372. [Google Scholar]
- Gaengler, P.; Hoyer, I.; Montag, R. Clinical evaluation of posterior composite restorations: The 10-year report. J. Adhes. Dent. 2001, 3, 185–194. [Google Scholar] [PubMed]
- Da Rosa Rodolpho, P.A.; Donassollo, T.A.; Cenci, M.S.; Loguércio, A.D.; Moraes, R.R.; Bronkhorst, E.M.; Opdam, N.J.; Demarco, F.F. 22-Year clinical evaluation of the performance of two posterior composites with different filler characteristics. Dent. Mater. 2011, 27, 955–963. [Google Scholar] [CrossRef] [PubMed]
- Pallesen, U.; van Dijken, J.W. A randomized controlled 30 years follow up of three conventional resin composites in Class II restorations. Dent. Mater. 2015, 31, 1232–1244. [Google Scholar] [CrossRef]
- Körner, P.; El Gedaily, M.; Attin, R.; Wiedemeier, D.B.; Attin, T.; Tauböck, T.T. Margin integrity of conservative composite restorations after resin infiltration of demineralized enamel. J. Adhes. Dent. 2017, 19, 483–489. [Google Scholar]
- Wiegand, A.; Credé, A.; Tschammler, C.; Attin, T.; Tauböck, T.T. Enamel wear by antagonistic restorative materials under erosive conditions. Clin. Oral Investig. 2017, 21, 2689–2693. [Google Scholar] [CrossRef] [PubMed]
- Par, M.; Spanovic, N.; Tauböck, T.T.; Attin, T.; Tarle, Z. Degree of conversion of experimental resin composites containing bioactive glass 45S5: The effect of post-cure heating. Sci. Rep. 2019, 9, 17245. [Google Scholar] [CrossRef] [PubMed]
- Par, M.; Marovic, D.; Attin, T.; Tarle, Z.; Tauböck, T.T. The effect of rapid high-intensity light-curing on micromechanical properties of bulk-fill and conventional resin composites. Sci. Rep. 2020, 10, 10560. [Google Scholar] [CrossRef] [PubMed]
- Lynch, C.D.; Opdam, N.J.; Hickel, R.; Brunton, P.A.; Gurgan, S.; Kakaboura, A.; Shearer, A.C.; Vanherle, G.; Wilson, N.H.F. Guidance on posterior resin composites: Academy of Operative Dentistry-European Section. J. Dent. 2014, 42, 377–383. [Google Scholar] [CrossRef]
- Bartlett, D.; Sundaram, G. An up to 3-year randomized clinical study comparing indirect and direct resin composites used to restore worn posterior teeth. Int. J. Prosthodont. 2006, 19, 613–617. [Google Scholar]
- Schmidlin, P.R.; Filli, T.; Imfeld, C.; Tepper, S.; Attin, T. Three-year evaluation of posterior vertical bite reconstruction using direct resin composite–a case series. Oper. Dent. 2009, 34, 102–108. [Google Scholar] [CrossRef][Green Version]
- Hamburger, J.T.; Opdam, N.J.; Bronkhorst, E.M.; Kreulen, C.M.; Roeters, J.J.; Huysmans, M.C. Clinical performance of direct composite restorations for treatment of severe tooth wear. J. Adhes. Dent. 2011, 13, 585–593. [Google Scholar] [PubMed]
- Attin, T.; Filli, T.; Imfeld, C.; Schmidlin, P.R. Composite vertical bite reconstructions in eroded dentitions after 5.5 years: A case series. J. Oral Rehabil. 2012, 39, 73–79. [Google Scholar] [CrossRef] [PubMed]
- Ramseyer, S.T.; Helbling, C.; Lussi, A. Posterior vertical bite reconstructions of erosively worn dentitions and the “stamp technique”—A case series with a mean observation time of 40 months. J. Adhes. Dent. 2015, 17, 283–289. [Google Scholar] [PubMed]
- Loomans, B.A.C.; Kreulen, C.M.; Huijs-Visser, H.E.C.E.; Sterenborg, B.A.M.M.; Bronkhorst, E.M.; Huysmans, M.C.D.N.J.M.; Opdam, N.J.M. Clinical performance of full rehabilitations with direct composite in severe tooth wear patients: 3.5 years results. J. Dent. 2018, 70, 97–103. [Google Scholar] [CrossRef] [PubMed]
- Tauböck, T.T.; Attin, T.; Schmidlin, P.R. Implementation and experience of a new method for posterior vertical bite reconstruction using direct resin composite restorations in the private practice—A survey. Acta Odontol. Scand. 2012, 70, 309–317. [Google Scholar] [CrossRef] [PubMed]
- Abduo, J.; Lyons, K. Clinical considerations for increasing occlusal vertical dimension: A review. Aust. Dent. J. 2012, 57, 2–10. [Google Scholar] [CrossRef] [PubMed]
- Tauböck, T.T.; Tarle, Z.; Marovic, D.; Attin, T. Pre-heating of high-viscosity bulk-fill resin composites: Effects on shrinkage force and monomer conversion. J. Dent. 2015, 43, 1358–1364. [Google Scholar] [CrossRef] [PubMed]
- Manhart, J.; Chen, H.; Hamm, G.; Hickel, R. Buonocore Memorial Lecture. Review of the clinical survival of direct and indirect restorations in posterior teeth of the permanent dentition. Oper. Dent. 2004, 29, 481–508. [Google Scholar]
- Beck, F.; Lettner, S.; Graf, A.; Bitriol, B.; Dumitrescu, N.; Bauer, P.; Moritz, A.; Schedle, A. Survival of direct resin restorations in posterior teeth within a 19-year period (1996–2015): A meta-analysis of prospective studies. Dent. Mater. 2015, 31, 958–985. [Google Scholar] [CrossRef] [PubMed]
- Ilie, N.; Hickel, R. Investigations on mechanical behaviour of dental composites. Clin. Oral Investig. 2009, 13, 427–438. [Google Scholar] [CrossRef]
- Macedo, C.R.; Silva, A.B.; Machado, M.A.; Saconato, H.; Prado, G.F. Occlusal splints for treating sleep bruxism (tooth grinding). Cochrane Database Syst. Rev. 2007, CD005514. [Google Scholar] [CrossRef] [PubMed]
- Koottathape, N.; Takahashi, H.; Iwasaki, N.; Kanehira, M.; Finger, W.J. Two- and three-body wear of composite resins. Dent. Mater. 2012, 28, 1261–1270. [Google Scholar] [CrossRef] [PubMed]
- Palaniappan, S.; Elsen, L.; Lijnen, I.; Peumans, M.; Van Meerbeek, B.; Lambrechts, P. Nanohybrid and microfilled hybrid versus conventional hybrid composite restorations: 5-year clinical wear performance. Clin. Oral Investig. 2012, 16, 181–190. [Google Scholar] [CrossRef]
- Curtis, A.R.; Palin, W.M.; Fleming, G.J.; Shortall, A.C.; Marquis, P.M. The mechanical properties of nanofilled resin-based composites: The impact of dry and wet cyclic pre-loading on bi-axial flexure strength. Dent. Mater. 2009, 25, 188–197. [Google Scholar] [CrossRef]
- De Moraes, R.R.; Gonçalves, L.S.; Lancellotti, A.C.; Consani, S.; Correr-Sobrinho, L.; Sinhoreti, M.A. Nanohybrid resin composites: Nanofiller loaded materials or traditional microhybrid resins. Oper. Dent. 2009, 34, 551–557. [Google Scholar] [CrossRef]
- Lucey, S.; Lynch, C.D.; Ray, N.J.; Burke, F.M.; Hannigan, A. Effect of pre-heating on the viscosity and microhardness of a resin composite. J. Oral Rehabil. 2010, 37, 278–282. [Google Scholar] [CrossRef] [PubMed]
- Froes-Salgado, N.R.; Silva, L.M.; Kawano, Y.; Francci, C.; Reis, A.; Loguercio, A.D. Composite pre-heating: Effects on marginal adaptation, degree of conversion and mechanical properties. Dent. Mater. 2010, 26, 908–914. [Google Scholar] [CrossRef]
| Gender | Patient Age (Years) | Treated Teeth | Observation Period (Years) | |
|---|---|---|---|---|
| 1 | Male | 45 | 17, 16, 15, 14, 24, 25, 26, 27, 37, 36, 35, 34, 44, 45, 47 | 10.6 |
| 2 | Male | 39 | 37, 36, 35, 34, 44, 45, 46, 47 | 11.2 |
| 3 | Female | 55 | 37, 36, 35, 34, 44, 45, 46, 47 | 10.8 |
| 4 | Male | 43 | 16, 15, 14, 24, 25, 26, 37, 36, 35, 34, 44, 45, 46, 47 | 10.2 |
| 5 | Male | 42 | 17, 16, 15, 14, 25, 26, 37, 36, 35, 34, 44, 45, 46, 47 | 10.8 |
| 45 ± 6 | n = 59 | 10.7 ± 0.4 |
| Gender | Patient Age (Years) | Treated Teeth | Observation Period (Years) | |
|---|---|---|---|---|
| 1 | Female | 28 | 36, 35, 34, 44, 45, 46 | 6.4 |
| 2 | Male | 38 | 17, 16, 15, 14, 24, 25, 26, 27, 37, 36, 35, 44, 45, 46, 47 | 7.2 |
| 3 | Male | 48 | 17, 16, 15, 14, 24, 25, 26, 27, 37, 36, 35, 34, 44, 45, 46, 47 | 3.9 |
| 4 | Male | 50 | 16, 15, 24, 25, 27, 36, 35, 34, 44, 45, 47 | 4.1 |
| 5 | Male | 36 | 17, 16, 15, 14, 24, 25, 26, 27, 37, 36, 35, 34, 44, 45, 46, 47 | 6.8 |
| 6 | Female | 27 | 17, 16, 15, 14, 24, 25, 26, 27, 37, 36, 35, 34, 44, 45, 46, 47 | 5.1 |
| 7 | Male | 51 | 17, 16, 15, 14, 24, 25, 26, 27, 37, 36, 35, 34, 44, 45, 46, 47 | 4.9 |
| 8 | Female | 56 | 15, 14, 24, 25, 38, 35, 34, 44, 45 | 3.4 |
| 42 ± 11 | n = 105 | 5.2 ± 1.4 |
| Alpha | Bravo | Charlie | Delta | |
|---|---|---|---|---|
| Surface texture | Sound | Rough | - | - |
| Anatomical form | Sound | Loss of material within the composite | Loss of material extending to the tooth surface | Complete or partial (>50%) loss of the bulk |
| Marginal integrity | Sound | Positive/negative step, removable by finishing | Negative step, not removable by finishing | Strong negative step, not removable in major parts |
| Marginal discoloration | None | Slight discoloration, removable by finishing | Discoloration, localized, not removable | Strong discoloration in many parts, not removable |
| Secondary caries | None | - | Caries present | - |
| Marginal inflammation | None No pockets > 3 mm, no bleeding | Slight No pockets > 3 mm, bleeding | Moderate Pockets 4–5 mm, bleeding | Severe Pockets ≥ 6 mm, bleeding |
| Restoration color stability | No change | Change of color as compared to baseline | - | - |
| Color match | Sound | Non-perceptible at talking distance | Perceptible at talking distance | Total mismatch |
| Postoperative sensitivity (air) | None | Moderate | Severe | - |
| Rating | Patient | Total | ||||||
|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | n | % | ||
| Surface texture | Alpha | 5 | 2 | 7 | 5 | 10 | 29 | 52 |
| Bravo | 10 | 6 | 1 | 7 | 3 | 27 | 48 | |
| Charlie | - | - | - | - | - | |||
| Delta | - | - | - | - | - | |||
| Anatomical form | Alpha | 3 | 1 | 7 | 5 | 5 | 21 | 38 |
| Bravo | 12 | 6 | 1 | 5 | 8 | 32 | 57 | |
| Charlie | 0 | 1 | 0 | 2 | 0 | 3 | 5 | |
| Delta | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| Marginal integrity | Alpha | 7 | 6 | 5 | 4 | 9 | 31 | 55 |
| Bravo | 8 | 2 | 3 | 7 | 4 | 24 | 43 | |
| Charlie | 0 | 0 | 0 | 1 | 0 | 1 | 2 | |
| Delta | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| Marginal discoloration | Alpha | 5 | 7 | 6 | 3 | 11 | 32 | 57 |
| Bravo | 10 | 1 | 2 | 8 | 2 | 23 | 41 | |
| Charlie | 0 | 0 | 0 | 1 | 0 | 1 | 2 | |
| Delta | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| Secondary caries | Alpha | 15 | 8 | 8 | 12 | 13 | 56 | 100 |
| Bravo | - | - | - | - | - | |||
| Charlie | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| Delta | - | - | - | - | - | |||
| Marginal inflammation | Alpha | 15 | 8 | 5 | 11 | 9 | 48 | 86 |
| Bravo | 0 | 0 | 3 | 1 | 4 | 8 | 14 | |
| Charlie | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| Delta | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| Restoration color stability | Alpha | 15 | 7 | 8 | 12 | 12 | 54 | 96 |
| Bravo | 0 | 1 | 0 | 0 | 1 | 2 | 4 | |
| Charlie | - | - | - | - | - | |||
| Delta | - | - | - | - | - | |||
| Color match | Alpha | 14 | 7 | 2 | 11 | 9 | 43 | 77 |
| Bravo | 1 | 1 | 6 | 1 | 4 | 13 | 23 | |
| Charlie | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| Delta | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| Postoperative sensitivity (air) | Alpha | 15 | 8 | 8 | 12 | 13 | 56 | 100 |
| Bravo | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| Charlie | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| Delta | - | - | - | - | - | |||
| Alpha | Bravo | Charlie | Delta | |||||
|---|---|---|---|---|---|---|---|---|
| Nanofilled | Microhybrid * | Nanofilled | Microhybrid * | Nanofilled | Microhybrid * | Nanofilled | Microhybrid * | |
| Surface texture | 74 | 72 | 26 | 28 | - | - | - | - |
| Anatomical form | 74 | 29 | 17 | 57 | 9 | 13 | 0 | 0 |
| Marginal integrity | 80 | 41 | 19 | 57 | 1 | 5 | 0 | 1 |
| Marginal discoloration | 81 | 39 | 14 | 51 | 5 | 11 | 0 | 0 |
| Secondary caries | 99 | 100 | - | - | 1 | 0 | - | - |
| Marginal inflammation | 41 | 41 | 59 | 59 | 0 | 0 | 0 | 0 |
| Restoration color stability | 91 | 97 | 9 | 3 | - | - | - | - |
| Color match | 72 | 89 | 28 | 11 | 0 | 0 | 0 | 0 |
| Postoperative sensitivity (air) | 100 | 96 | 0 | 4 | 0 | 0 | - | - |
| VAS Score | ||
|---|---|---|
| 5.2-Year Cohort | 10.7-Year Cohort | |
| Chewing comfort (0 = maximal unsatisfied, 10 = maximal satisfied) | 9.7 (0.3) | 8.9 (0.8) |
| Recommend treatment (0 = not at all, 10 = without hesitation, anytime) | 9.5 (0.9) | 9.7 (0.4) |
| Muscle or joint problems (0 = not at all, 10 = maximal) | 0.8 (2.2) | 1.2 (2.2) |
| Cost-benefit ratio (0 = maximal unsatisfied, 10 = maximal satisfied) | 7.6 (2.3) | 9.1 (0.9) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tauböck, T.T.; Schmidlin, P.R.; Attin, T. Vertical Bite Rehabilitation of Severely Worn Dentitions with Direct Composite Restorations: Clinical Performance up to 11 Years. J. Clin. Med. 2021, 10, 1732. https://doi.org/10.3390/jcm10081732
Tauböck TT, Schmidlin PR, Attin T. Vertical Bite Rehabilitation of Severely Worn Dentitions with Direct Composite Restorations: Clinical Performance up to 11 Years. Journal of Clinical Medicine. 2021; 10(8):1732. https://doi.org/10.3390/jcm10081732
Chicago/Turabian StyleTauböck, Tobias T., Patrick R. Schmidlin, and Thomas Attin. 2021. "Vertical Bite Rehabilitation of Severely Worn Dentitions with Direct Composite Restorations: Clinical Performance up to 11 Years" Journal of Clinical Medicine 10, no. 8: 1732. https://doi.org/10.3390/jcm10081732
APA StyleTauböck, T. T., Schmidlin, P. R., & Attin, T. (2021). Vertical Bite Rehabilitation of Severely Worn Dentitions with Direct Composite Restorations: Clinical Performance up to 11 Years. Journal of Clinical Medicine, 10(8), 1732. https://doi.org/10.3390/jcm10081732








