The Anatomical Conditions of the Alveolar Process of the Anterior Maxilla in Terms of Immediate Implantation—Radiological Retrospective Case Series Study
Abstract
1. Introduction
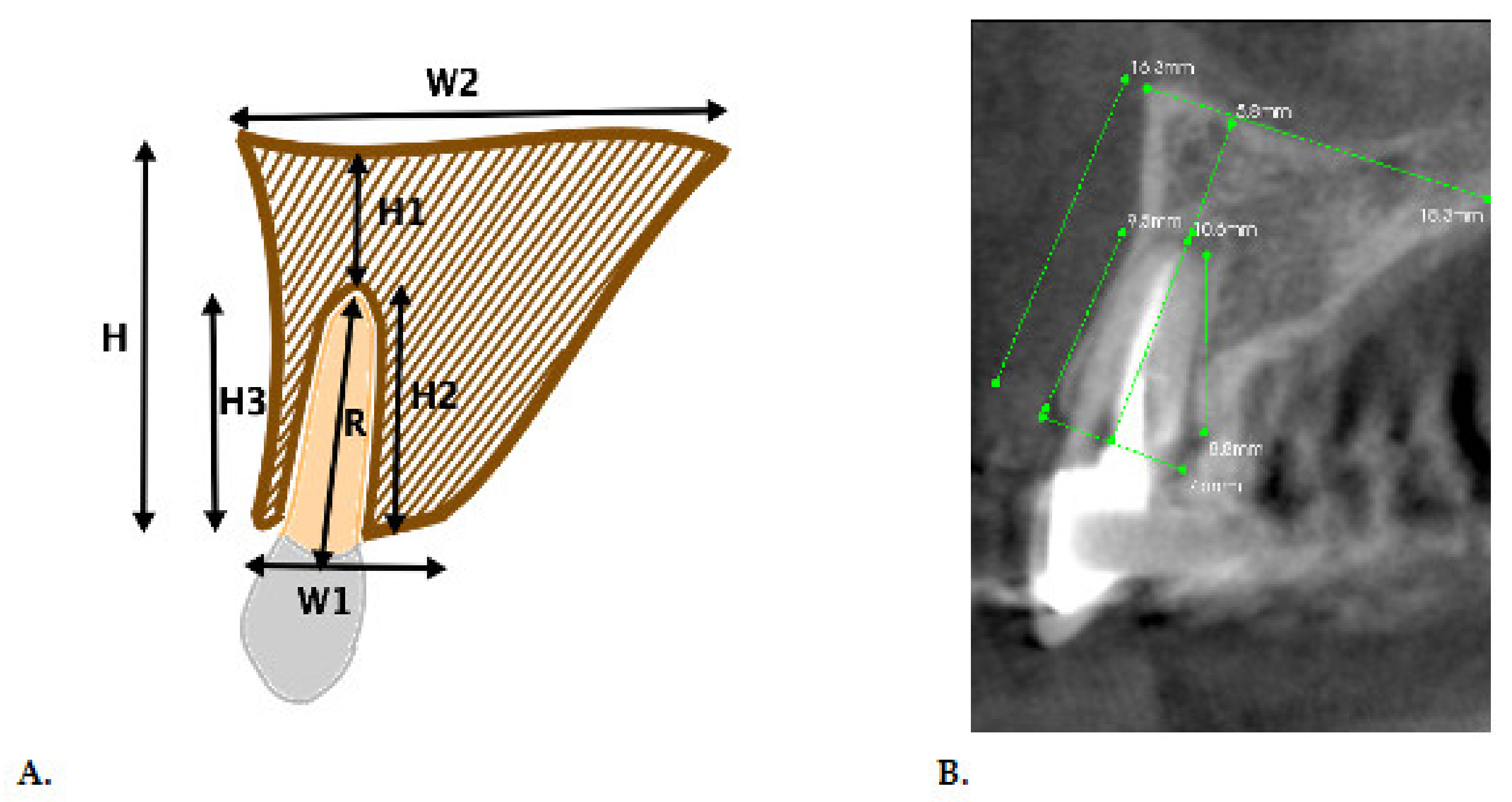
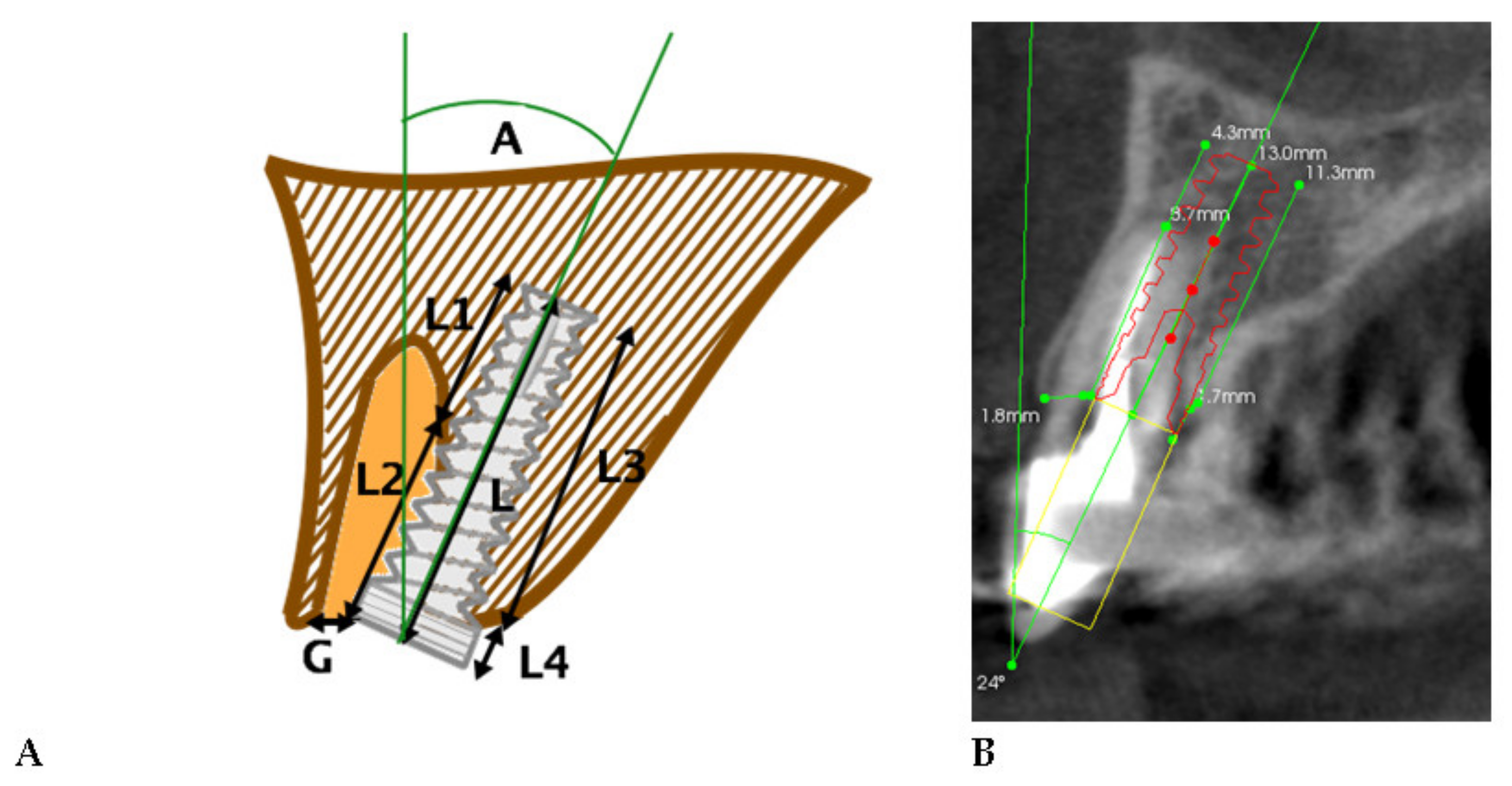
2. Material and Methods
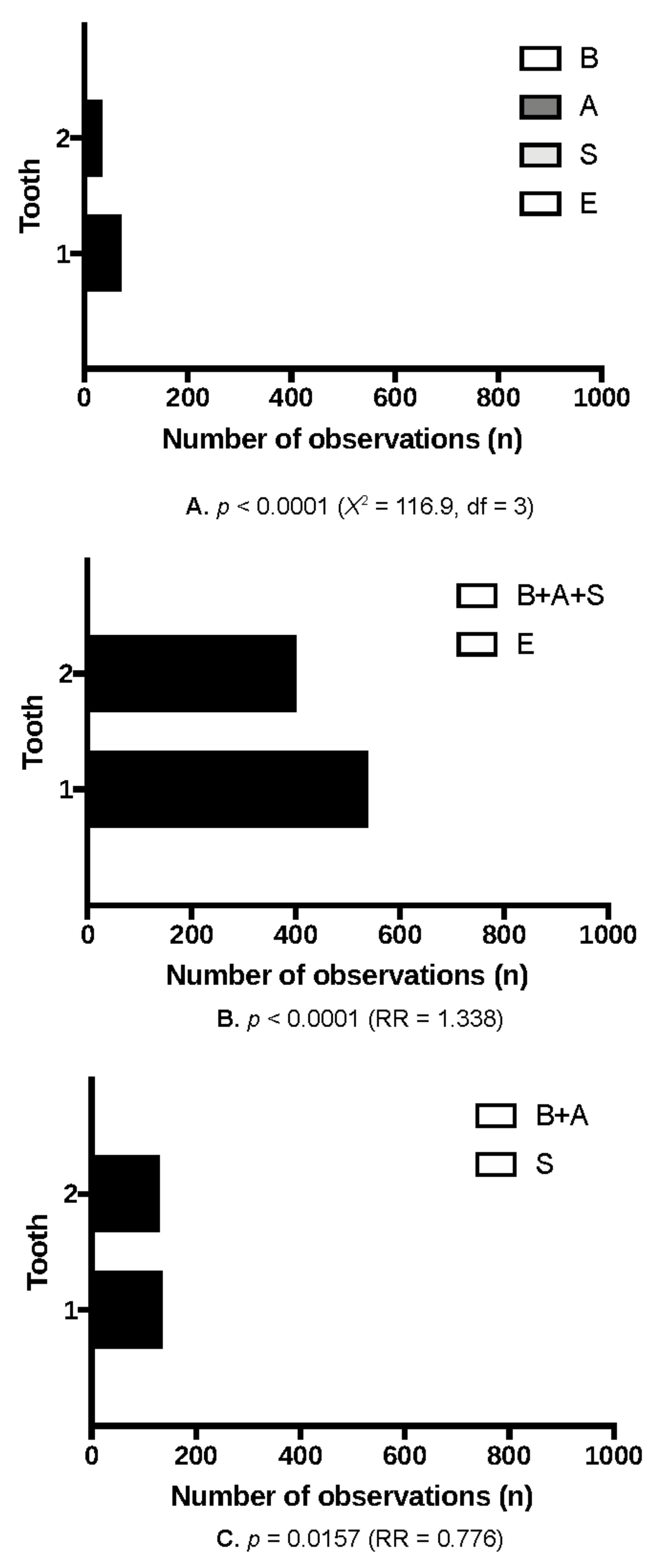
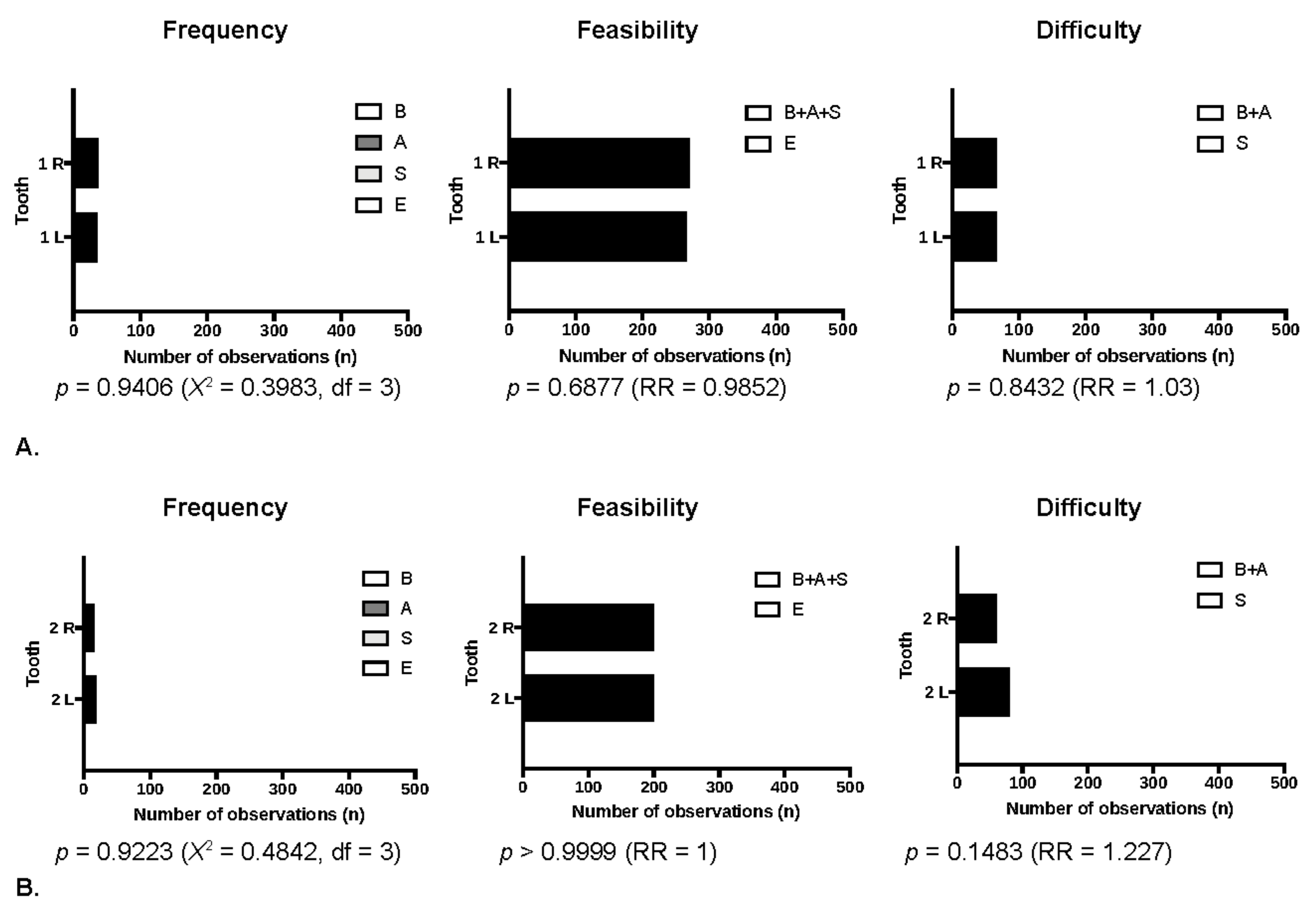
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Cosola, S.; Marconcini, S.; Giammarinaro, E.; Poli, G.L.; Covani, U.; Barone, A. Oral health-related quality of life and clinical outcomes of immediately or delayed loaded implants in the rehabilitation of edentulous jaws: A retrospective comparative study. Minerva. Stomatol. 2018, 67, 189–195. [Google Scholar]
- Doornewaard, R.; Bruyn, H.; Matthys, C.; Bronkhorst, E.; Vandeweghe, S.; Vervaeke, S. The Long-Term Effect of Adapting the Vertical Position of Implants on Peri-Implant Health: A 5-Year Intra-Subject Comparison in the Edentulous Mandible Including Oral Health-Related Quality of Life. J. Clin. Med. 2020, 9, 3320. [Google Scholar] [CrossRef]
- Kohal, R.J.; Spies, B.C.; Vach, K.; Balmer, M.; Pieralli, S. A Prospective Clinical Cohort Investigation on Zirconia Implants: 5-Year Results. J. Clin. Med. 2020, 9, 2585. [Google Scholar] [CrossRef]
- Lopez-Valverde, N.; Flores-Fraile, J.; Ramírez, J.M.; Sousa, B.M.; Herrero-Hernández, S.; López-Valverde, A. Bioactive Surfaces vs. Conventional Surfaces in Titanium Dental Implants: A Comparative Systematic Review. J. Clin. Med. 2020, 9, 2047. [Google Scholar] [CrossRef]
- Wychowanski, P.; Szubinska-Lelonkiewicz, D.; Osiak, M.; Nowak, M.; Kosieradzki, M.; Fiedor, P. New Approach to Treatment of High-Risk Allograft Recipients under Chronic Immunosuppression with Tooth Loss. Evaluation of Safety and Longevity of Dental Implants: A Case Report. Transplant. Proc. 2020, 52, 2558–2562. [Google Scholar] [CrossRef]
- Moraschini, V.; Barboza, E. Success of dental implants in smokers and non-smokers: A systematic review and meta-analysis. Int. J. Oral Maxillofac. Surg. 2016, 45, 205–215. [Google Scholar] [CrossRef] [PubMed]
- Wychowański, P.; Starzyńska, A.; Jereczek-Fossa, B.A.; Iwanicka-Grzegorek, E.; Kosewski, P.; Adamska, P.; Woliński, J. The Effects of Smoking Cigarettes on Immediate Dental Implant Stability—A Prospective Case Series Study. Appl. Sci. 2021, 11, 27. [Google Scholar] [CrossRef]
- Windael, S.; Vervaeke, S.; De Buyser, S.; De Bruyn, H.; Collaert, B. The Long-Term Effect of Smoking on 10 Years’ Survival and Success of Dental Implants: A Prospective Analysis of 453 Implants in a Non-University Setting. J. Clin. Med. 2020, 9, 1056. [Google Scholar] [CrossRef] [PubMed]
- Schropp, L.; Wenzel, A.; Kostopoulos, L.; Karring, T. Bone healing and soft tissue contour changes following single-tooth extraction: A clinical and radiographic 12-month prospective study. Int. J. Periodontics Restor. Dent. 2003, 23, 313–323. [Google Scholar]
- Van Doorne, L.; Gholami, P.; D’haese, J.; Hommez, G.; Meijer, G.; De Bruyn, H. Three-Dimensional Radiographic Outcome of Free-Handed Flaplessly Placed Mini Dental Implants in Edentulous Maxillae after 2-Years Function. J. Clin. Med. 2020, 9, 2120. [Google Scholar] [CrossRef]
- Torres-Alemany, A.; Fernández-Estevan, L.; Agustín-Panadero, R.; Montiel-Company, J.M.; Labaig-Rueda, C.; Mañes-Ferrer, J.F. Clinical Behavior of Short Dental Implants: Systematic Review and Meta-Analysis. J. Clin. Med. 2020, 9, 3271. [Google Scholar] [CrossRef] [PubMed]
- Aleksandrowicz, P.; Kusa-Podkańska, M.; Grabowska, K.; Kotuła, L.; Szkatuła-Łupina, A.; Wysokińska-Miszczuk, J. Extra-Sinus Zygomatic Implants to Avoid Chronic Sinusitis and Prosthetic Arch Malposition: 12 Years of Experience. J. Oral Implantol. 2019, 45, 73–78. [Google Scholar] [CrossRef]
- Chroscicka, A.; Jaegermann, Z.; Wychowański, P.; Ratajska, A.; Sadło, J.; Hoser, G.; Michałowski, S.; Lewandowska-Szumiel, M. Synthetic Calcite as a Scaffold for Osteoinductive Bone Substitutes. Ann. Biomed. Eng. 2016, 44, 2145–2157. [Google Scholar] [CrossRef]
- Wychowanski, P.; Woliński, J.; Morawiec, T.; Kownacki, P.; Starzynska, A.; Kosieradzki, M.; Fiedor, P. Preliminary Clinical Data and the Comparison of the Safety and Efficacy of Autogenous Bone Grafts Versus Xenograft Implantations in Vertical Bone Deficiencies Before Dental Implant Installation. Transplant. Proc. 2020, 52, 2248–2251. [Google Scholar] [CrossRef] [PubMed]
- Hattingh, A.; De Bruyn, H.; Van Weehaeghe, M.; Hommez, G.; Vandeweghe, S. Contour Changes Following Immediate Placement of Ultra-Wide Implants in Molar Extraction Sockets without Bone Grafting. J. Clin. Med. 2020, 9, 2504. [Google Scholar] [CrossRef]
- Arora, H.; Khzam, N.; Roberts, D.; Bruce, W.L.; Ivanovski, S. Immediate implant placement and restoration in the anterior maxilla: Tissue dimensional changes after 2–5 year follow up. Clin. Implant. Dent. Relat. Res. 2017, 19, 694–702. [Google Scholar] [CrossRef]
- Schulte, W.; Heimke, G. The Tubinger immediate implant. Quintessenz 1976, 27, 17–23. [Google Scholar]
- Ross, S.E.; Strauss, T.; Crossetti, H.W.; Gargiulo, A.W. The immediate placement of an endosseous implant into an extraction wound: A clinical case report using the RosTR System. Int. J. Periodontics Restor. Dent. 1989, 9, 34–41. [Google Scholar]
- Lazzara, R.J. Immediate implant placement into extraction sites: Surgical and restorative advantages. Int. J. Periodontics Restor. Dent. 1989, 9, 332–343. [Google Scholar]
- Buser, D.; Chappuis, V.; Belser, U.C.; Chen, S. Implant placement post extraction in esthetic single tooth sites: When immediate, when early, when late? Periodontol. 2000 2017, 73, 84–102. [Google Scholar] [CrossRef]
- Wychowański, P.; Woliński, J.; Kacprzak, M.; Tomkiewicz, W.; Bartłomiej, I.; Szubińska-Lelonkiewicz, D.; Wojtowicz, A.; Nevins, M. Immediate Palatal Molar Implants: A Simple, Safe, Minimally Invasive Technique. Int. J. Periodontics Restor. Dent. 2017, 37, e297–e301. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Wychowanski, P.; Starzynska, A.; Woliński, J.; Kosieradzki, M.; Fiedor, P. New Surgical Technique Using Xenograft as a Microinvasive Method to Avoid Extensive Bone Reconstruction in Patients with Compromised General Health: Promising Surgical Methodology and First Clinical Results. Transplant. Proc. 2020, 52, 2244–2247. [Google Scholar] [CrossRef]
- De Santis, D.; Sinigaglia, S.; Pancera, P.; Faccioni, P.; Portelli, M.; Luciano, U.; Cosola, S.; Penarrocha, D.; Bertossi, D.; Nocini, R.; et al. An overview of socket preservation. J. Biol. Regul. Homeost. Agents 2019, 33, 55–59. [Google Scholar] [PubMed]
- Atieh, M.A.; Alsabeeha, N.; Duncan, W.J. Stability of tapered and parallel-walled dental implants: A systematic review and meta-analysis. Clin. Implant. Dent. Relat. Res. 2018, 20, 634–645. [Google Scholar] [CrossRef]
- Grunder, U.; Gracis, S.; Capelli, M. Influence of the 3-D bone-to-implant relationship on esthetics. Int. J. Periodontics Restor. Dent. 2005, 25, 113–119. [Google Scholar]
- Javed, F.; Ahmed, H.B.; Crespi, R.; Romanos, G.E. Role of primary stability for successful osseointegration of dental implants: Factors of influence and evaluation. Interv. Med. Appl. Sci. 2013, 5, 162–167. [Google Scholar] [CrossRef]
- Cosola, S.; Marconcini, S.; Boccuzzi, M.; Menchini Fabris, G.B.; Covani, U.; Peñarrocha-Diago, M.; Peñarrocha-Oltra, D. Radiological Outcomes of Bone-Level and Tissue-Level Dental Implants: Systematic Review. Int. J. Environ. Res. Public Health 2020, 17, 6920. [Google Scholar] [CrossRef] [PubMed]
- Cosola, S.; Toti, P.; Peñarrocha-Diago, M.; Covani, U.; Brevi, B.C.; Peñarrocha-Oltra, D. Standardization of three-dimensional pose of cylindrical implants from intraoral radiographs: A preliminary study. BMC Oral Health 2021, 21, 100. [Google Scholar] [CrossRef]
- D’Haese, J.; Van De Velde, T.; Komiyama, A.; Hultin, M.; De Bruyn, H. Accuracy and complications using computer-designed stereolithographic surgical guides for oral rehabilitation by means of dental implants: A review of the literature. Clin. Implant. Dent. Relat. Res. 2012, 14, 321–335. [Google Scholar] [CrossRef] [PubMed]
- D’Haese, J.; Ackhurst, J.; Wismeijer, D.; De Bruyn, H.; Tahmaseb, A. Current state of the art of computer-guided implant surgery. Periodontol. 2000 2017, 73, 121–133. [Google Scholar] [CrossRef]
- Zhang, W.; Skrypczak, A.; Weltman, R. Anterior maxilla alveolar ridge dimension and morphology measurement by cone beam computerized tomography (CBCT) for immediate implant treatment planning. BMC Oral Health 2015, 15, 65. [Google Scholar] [CrossRef] [PubMed]
- Lin, G.H.; Chan, H.L.; Wang, H.L. Effects of currently available surgical and restorative interventions on reducing midfacial mucosal recession of immediately placed single-tooth implants: A systematic review. J. Periodontol. 2014, 85, 92–102. [Google Scholar] [CrossRef]
- Chappuis, V.; Araujo, M.G.; Buser, D. Clinical relevance of dimensional bone and soft tissue alterations post-extraction in esthetic sites. Periodontol. 2000 2017, 73, 73–83. [Google Scholar] [CrossRef]
- Blanco, J.; Carral, C.; Argibay, O.; Liñares, A. Implant placement in fresh extraction sockets. Periodontol. 2000 2019, 79, 151–167. [Google Scholar] [CrossRef] [PubMed]
- Kan, J.Y.; Roe, P.; Rungcharassaeng, K.; Patel, R.D.; Waki, T.; Lozada, J.L.; Zimmerman, G. Classification of sagittal root position in relation to the anterior maxillary osseous housing for immediate implant placement: A cone beam computed tomography study. Int. J. Oral Maxillofac. Implant. 2011, 26, 873–876. [Google Scholar]
- Lekholm, U. Surgical considerations and possible shortcomings of host sites. J. Prosthet. Dent. 1998, 79, 43–48. [Google Scholar] [CrossRef]
- Corbella, S.; Taschieri, S.; Samaranayake, L.; Tsesis, I.; Nemcovsky, C.; Del Fabbro, M. Implant treatment choice after extraction of a vertically fractured tooth. A proposal for a clinical classification of bony defects based on a systematic review of literature. Clin. Oral Implant. Res. 2014, 25, 946–956. [Google Scholar] [CrossRef]
- Smith, R.B.; Tarnow, D.P. Classification of molar extraction sites for immediate dental implant placement: Technical note. Int. J. Oral Maxillofac. Implant. 2013, 28, 911–916. [Google Scholar] [CrossRef] [PubMed]
- Rebaudi, A.; Trisi, P.; Cella, R.; Cecchini, G. Preoperative evaluation of bone quality and bone density using a novel CT/microCT-based hard-normal-soft classification system. Int. J. Oral Maxillofac. Implant. 2010, 25, 75–85. [Google Scholar]
- Salama, H.; Salama, M. The role of orthodontic extrusive remodeling in the enhancement of soft and hard tissue profiles prior to implant placement: A systematic approach to the management of extraction site defects. Int. J. Periodontics Restor. Dent. 1993, 13, 312–333. [Google Scholar]
- Nicolielo, L.F.P.; Van Dessel, J.; van Lenthe, G.H.; Lambrichts, I.; Jacobs, R. Computer-based automatic classification of trabecular bone pattern can assist radiographic bone quality assessment at dental implant site. Br. J. Radiol. 2018, 91, 20180437. [Google Scholar] [CrossRef] [PubMed]
- Linck, G.K.; Ferreira, G.M.; De Oliveira, R.C.; Lindh, C.; Leles, C.R.; Ribeiro-Rotta, R.F. The Influence of Tactile Perception on Classification of Bone Tissue at Dental Implant Insertion. Clin. Implant. Dent. Relat. Res. 2016, 18, 601–608. [Google Scholar] [CrossRef] [PubMed]
- Papadimitriou, D.E.; Salari, S.; Gannam, C.; Gallucci, G.O.; Friedland, B. Implant-prosthodontic classification of the edentulous jaw for treatment planning with fixed rehabilitations. Int. J. Prosthodont. 2014, 27, 320–327. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Buser, D.; Martin, W.C.; Belser, U.C. The SAC Classification in Implant Dentistry; Chen, A.D., Ed.; Quintessence Publishing Co Ltd.: Berlin, Germany, 2009. [Google Scholar]
- Marconcini, S.; Denaro, M.; Cosola, S.; Gabriele, M.; Toti, P.; Mijiritsky, E.; Proietti, A.; Basolo, F.; Giammarinaro, E.; Covani, U. Myofibroblast Gene Expression Profile after Tooth Extraction in the Rabbit. Materials 2019, 12, 3697. [Google Scholar] [CrossRef] [PubMed]
- Llamas-Monteagudo, O.; Girbés-Ballester, P.; Viña-Almunia, J.; Peñarrocha-Oltra, D.; Peñarrocha-Diago, M. Clinical parameters of implants placed in healed sites using flapped and flapless techniques: A systematic review. Med. Oral Patol. Oral Cir. Bucal. 2017, 22, e572–e581. [Google Scholar] [CrossRef]
- Wakimoto, M.; Matsumura, T.; Ueno, T.; Mizukawa, N.; Yanagi, Y.; Lida, S. Bone quality and quantity of the anterior maxillary trabecular bone in dental implant sites. Clin. Oral Implant. Res. 2012, 23, 1314–1319. [Google Scholar] [CrossRef] [PubMed]
- Xu, L.; Wang, X.; Zhang, Q.; Yang, W.; Zhu, W.; Zhao, K. Immediate versus early loading of flapless placed dental implants: A systematic review. J. Prosthet. Dent. 2014, 112, 760–769. [Google Scholar] [CrossRef] [PubMed]

| Class | Total | Bimodal | Apex | Slope | Excluded | B+A+E (Immediate Implantation Possible) | ||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Percentage in total | 100 | 9 | 13.08 | 56.25 | 21.67 | 78.33 | ||||||||||||||||||
| Number of implants | 1200 | 108 | 157 | 675 | 260 | 940 | ||||||||||||||||||
| Tooth type | 1 | 2 | 1 | 2 | 1 | 2 | 1 | 2 | 1 | 2 | 1 | 2 | ||||||||||||
| Number of implants | 600 | 600 | 73 | 35 | 62 | 95 | 403 | 272 | 62 | 198 | 538 | 402 | ||||||||||||
| Percentage in class | 50 | 50 | 67.60 | 32.40 | 39.49 | 60.51 | 59.70 | 40.30 | 23.85 | 76.15 | 57.23 | 42.77 | ||||||||||||
| Percentage of all sides | 50 | 60 | 6.08 | 2.92 | 5.16 | 7.92 | 33.59 | 22.66 | 5.17 | 16.50 | 44.83 | 33.50 | ||||||||||||
| Tooth side | L | R | L | R | L | R | L | R | L | R | L | R | ||||||||||||
| Number of implants | 600 | 600 | 53 | 55 | 76 | 81 | 343 | 332 | 128 | 132 | 472 | 468 | ||||||||||||
| Percentage of all sides | 50 | 50 | 49.08 | 50.92 | 48.41 | 51.59 | 50.81 | 49.19 | 49.23 | 50.77 | 50.21 | 49.79 | ||||||||||||
| Tooth type and side | 12 | 11 | 21 | 22 | 12 | 11 | 21 | 22 | 12 | 11 | 21 | 22 | 12 | 11 | 21 | 22 | 12 | 11 | 21 | 22 | 12 | 11 | 21 | 22 |
| Number of implants | 300 | 300 | 300 | 300 | 16 | 37 | 36 | 19 | 46 | 30 | 32 | 49 | 139 | 204 | 199 | 133 | 99 | 29 | 33 | 99 | 201 | 271 | 267 | 201 |
| Percentage of all sides | 25 | 25 | 25 | 25 | 1.34 | 3.08 | 3 | 1.58 | 3.83 | 2.50 | 2.67 | 4.08 | 11.58 | 17 | 16.58 | 11.09 | 8.25 | 2.42 | 2.75 | 8.25 | 16.75 | 22.58 | 22.25 | 16.75 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wychowański, P.; Starzyńska, A.; Osiak, M.; Kowalski, J.; Jereczek-Fossa, B.A.; Seklecka, B.; Morawiec, T.; Adamska, P.; Woliński, J. The Anatomical Conditions of the Alveolar Process of the Anterior Maxilla in Terms of Immediate Implantation—Radiological Retrospective Case Series Study. J. Clin. Med. 2021, 10, 1688. https://doi.org/10.3390/jcm10081688
Wychowański P, Starzyńska A, Osiak M, Kowalski J, Jereczek-Fossa BA, Seklecka B, Morawiec T, Adamska P, Woliński J. The Anatomical Conditions of the Alveolar Process of the Anterior Maxilla in Terms of Immediate Implantation—Radiological Retrospective Case Series Study. Journal of Clinical Medicine. 2021; 10(8):1688. https://doi.org/10.3390/jcm10081688
Chicago/Turabian StyleWychowański, Piotr, Anna Starzyńska, Martyna Osiak, Jan Kowalski, Barbara Alicja Jereczek-Fossa, Blanka Seklecka, Tadeusz Morawiec, Paulina Adamska, and Jarosław Woliński. 2021. "The Anatomical Conditions of the Alveolar Process of the Anterior Maxilla in Terms of Immediate Implantation—Radiological Retrospective Case Series Study" Journal of Clinical Medicine 10, no. 8: 1688. https://doi.org/10.3390/jcm10081688
APA StyleWychowański, P., Starzyńska, A., Osiak, M., Kowalski, J., Jereczek-Fossa, B. A., Seklecka, B., Morawiec, T., Adamska, P., & Woliński, J. (2021). The Anatomical Conditions of the Alveolar Process of the Anterior Maxilla in Terms of Immediate Implantation—Radiological Retrospective Case Series Study. Journal of Clinical Medicine, 10(8), 1688. https://doi.org/10.3390/jcm10081688








