500 Meters Is a Result of 6-Minute Walk Test Which Differentiates Patients with High and Low Risk of Postoperative Complications after Lobectomy—A Validation Study
Abstract
1. Introduction
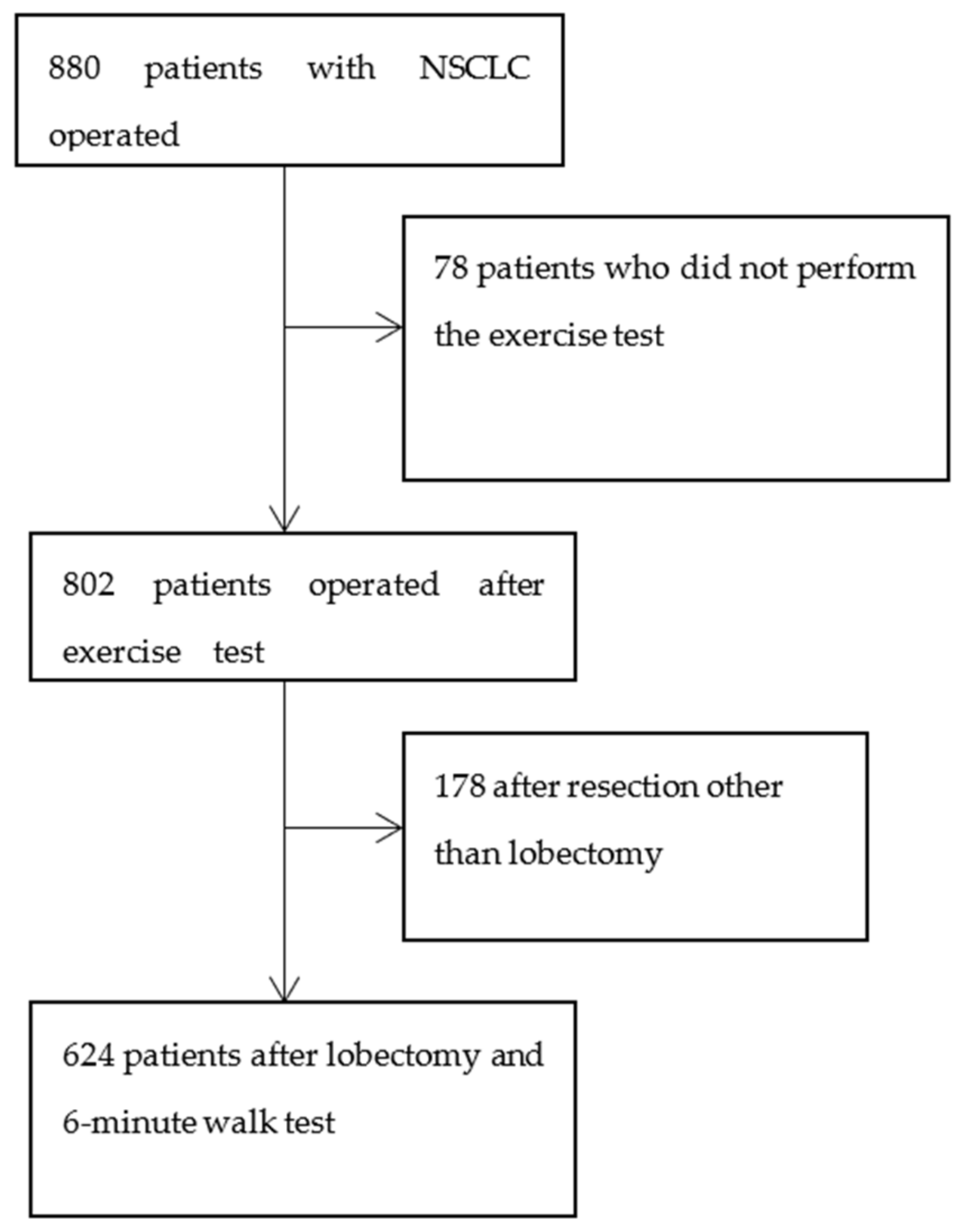
2. Material and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Brunelli, A.; Charloux, A.; Bolliger, C.T.; Rocco, G.; Sculier, J.P.; Varela, G.; Licker, M.; Ferguson, M.K.; Faivre-Finn, C.; Huber, R.M.; et al. European Respiratory Society and European Society of Thoracic Surgeons joint task force on fitness for radical therapy. ERS/ESTS clinical guidelines on fitness for radical therapy in lung cancer patients (surgery and chemo-radiotherapy). Eur. Respir. J. 2009, 34, 17–41. [Google Scholar] [CrossRef] [PubMed]
- Brunelli, A.; Kim, A.W.; Berger, K.I.; Addrizzo-Harris, D.J. Physiologic evaluation of the patient with lung cancer being considered for resectional surgery: Diagnosis and management of lung cancer, 3rd ed; American College of Chest Physicians evidence-based clinical practice guidelines. Chest 2013, 143, 166–190. [Google Scholar] [CrossRef]
- Brunelli, A.; Al Refai, M.; Monteverde, M.; Borri, A.; Salati, M.; Fianchini, A. Stair climbing test predicts cardiopulmonary complications after lung resection. Chest 2002, 121, 1106–1110. [Google Scholar] [CrossRef] [PubMed]
- Win, T.; Jackson, A.; Groves, A.M.; Sharples, L.D.; Charman, S.C.; Laroche, C.M. Comparison of shuttle walk with measured peak oxygen consumption in patients with operable lung cancer. Thorax 2006, 61, 57–60. [Google Scholar] [CrossRef] [PubMed]
- Toker, A.; Ziyade, S.; Bayrak, Y.; Tanju, S.; Senturk, M.; Dilege, S.; Kalayci, G. Prediction of cardiopulmonary morbidity after resection for lung cancer: Stair climbing test complications after lung cancer surgery. J. Thorac. Cardiovasc. Surg. 2007, 55, 253–256. [Google Scholar] [CrossRef]
- Win, T.; Jackson, A.; Groves, A.M.; Wells, F.C.; Ritchie, A.J.; Munday, H.; Laroche, C.M. Relationship of shuttle walk test and lung cancer surgical outcome. Eur. J. Cardiothorac. Surg. 2004, 26, 1216–1219. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Taylor, L.J.; Julliard, W.A.; Maloney, J.D. Predictive value of pulmonary function measures for short-term outcomes following lung resection: Analysis of a single high-volume institution. J. Thorac. Dis. 2018, 10, 1072–1076. [Google Scholar] [CrossRef] [PubMed]
- Gravier, F.E.; Bonnevie, T.; Boujibar, F.; Médrinal, C.; Prieur, G.; Combret, Y.; Muir, J.F.; Baste, J.M.; Debeaumont, D.; Cuvelier, A. Cardiopulmonary exercise testing in patients with non-small cell lung cancer: Trust the V˙ O2peak? J. Thorac. Dis. 2020, 12, 5313–5323. [Google Scholar] [CrossRef]
- Marjanski, T.; Wnuk., D.; Bosakowski., D.; Szmuda., T.; Sawicka, W.; Rzyman, W. Patients who do not reach a distance of 500 m during the 6-min walk test have an increased risk of postoperative complications and prolonged hospital stay after lobectomy. Eur. J. Cardiothorac. Surg. 2015, 47, 213–219. [Google Scholar] [CrossRef]
- ATS Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories. ATS statement: Guidelines for the six-minute walk test. Am. J. Respir. Crit. Care Med. 2002, 166, 111–117. [Google Scholar] [CrossRef]
- Enright, P.L.; Sherrill, D.L. Reference equations for the six-minute walk in healthy adults. Am. J. Respir. Crit. Care Med. 1998, 158, 1384–1387. [Google Scholar] [CrossRef] [PubMed]
- Gu, Z.; Wang, H.; Mao, T.; Ji, C.; Xiang, Y.; Zhu, Y.; Xu, P.; Fang, W. Pulmonary function changes after different extent of pulmonary resection under video-assisted thoracic surgery. J. Thorac. Dis. 2018, 10, 2331–2337. [Google Scholar] [CrossRef] [PubMed]
- Pompili, C. Quality of life after lung resection for lung cancer. J. Thorac. Dis. 2015, 7, 138–144. [Google Scholar] [CrossRef]
- Homma, T.; Doki, Y.; Yamamoto, Y.; Ojima, T.; Shimada, Y.; Kitamura, N.; Yoshimura, N. Risk factors of neuropathic pain after thoracic surgery. J. Thorac. Dis. 2018, 10, 2898–2907. [Google Scholar] [CrossRef]
- Benzo, R.; Kelley, G.A.; Recchi, L.; Hofman, A.; Sciurba, F. Complications of lung resection and exercise capacity: A meta-analysis. Respir. Med. 2007, 101, 1790–1797. [Google Scholar] [CrossRef]
- Holden, D.A.; Rice, T.W.; Stelmach, K.; Meeker, D.P. Exercise testing, 6-min walk, and stair climb in the evaluation of patients at high risk for pulmonary resection. Chest 1992, 102, 1774–1779. [Google Scholar] [CrossRef]
- Hattori, K.; Matsuda, T.; Takagi, Y.; Nagaya, M.; Inoue, T.; Nishida, Y.; Hasegawa, Y.; Kawaguchi, K.; Fukui, T.; Ozeki, N.; et al. Preoperative six-minute walk distance is associated with pneumonia after lung resection. Interact. Cardiovasc. Thorac. Surg. 2018, 26, 277–283. [Google Scholar] [CrossRef] [PubMed]
- Wesolowski, S.; Orlowski, T.M.; Kram, M. The 6-min walk test in the functional evaluation of patients with lung cancer qualified for lobectomy. Interact. Cardiovasc. Thorac. Surg. 2020, 30, 559–564. [Google Scholar] [CrossRef]
- Pierce, R.J.; Copland, J.M.; Sharpe, K.; Barter, C.E. Preoperative risk evaluation for lung cancer resection: Predicted postoperative product as a predictor of surgical mortality. Am. J. Respir. Crit. Care Med. 1994, 150, 947–955. [Google Scholar] [CrossRef] [PubMed]
- Santos, B.F.; Souza, H.C.; Miranda, A.P.; Cipriano, F.G.; Gastaldi, A.C. Performance in the 6-min walk test and postoperative pulmonary complications in pulmonary surgery: An observational study. Braz. J. Phys. Ther. 2016, 20, 66–72. [Google Scholar] [CrossRef]
- Marjanski, T.; Badocha, M.; Wnuk, D.; Dziedzic, R.; Ostrowski, M.; Sawicka, W.; Rzyman, W. Result of the 6-min walk test is an independent prognostic factor of surgically treated non-small-cell lung cancer. Interact. Cardiovasc. Thorac. Surg. 2019, 28, 368–374. [Google Scholar] [CrossRef] [PubMed]
- Smith, J.L.; Verrill, T.A.; Boura, J.A.; Sakwa, M.P.; Shannon, F.L.; Franklin, B.A. Effect of cardiorespiratory fitness on short-term morbidity and mortality after coronary artery bypass grafting. Am. J. Cardiol. 2013, 112, 1104–1109. [Google Scholar] [CrossRef] [PubMed]
- Grant, S.W.; Hickey, G.L.; Wisely, N.A.; Carlson, E.D.; Hartley, R.A.; Pichel, A.C.; Atkinson, D.; McCollum, C.N. Cardiopulmonary exercise testing and survival after elective abdominal aortic aneurysm repair†. Br. J. Anaesth. 2015, 114, 430–436. [Google Scholar] [CrossRef] [PubMed]
- Moran, J.; Wilson, F.; Guinan, E.; McCormick, P.; Hussey, J.; Moriarty, J. Role of cardiopulmonary exercise testing as a risk-assessment method in patients undergoing intra-abdominal surgery: A systematic review. Br. J. Anaesth. 2016, 116, 177–191. [Google Scholar] [CrossRef] [PubMed]
- Sathyaprasad, S.L.; Thomas, M.; Philip, F.A.; Krishna, K.J. Performance in 6-min walk test in prediction of post-operative pulmonary complication in major oncosurgeries: A prospective observational study. Indian J. Anaesth. 2020, 64, 55–61. [Google Scholar] [CrossRef]
- Inoue, T.; Ito, S.; Kanda, M.; Niwa, Y.; Nagaya, M.; Nishida, Y.; Hasegawa, Y.; Koike, M.; Kodera, Y. Preoperative six-minute walk distance as a predictor of postoperative complication in patients with esophageal cancer. Dis. Esophagus 2020, 33, 50. [Google Scholar] [CrossRef]
- Hayashi, K.; Fukumoto, K.; Yokoi, K.; Nagaya, M.; Inoue, T.; Ito, S.; Nakajima, H.; Hattori, K.; Kadono, I.; Nishida, Y. Post-operative delayed ambulation after thymectomy is associated withpre-operative six-minute walk distance. Disabil. Rehabil. 2018, 40, 1900–1905. [Google Scholar] [CrossRef] [PubMed]
- Paisani, D.M.; Fiore, J.F., Jr.; Lunardi, A.C.; Colluci, D.B.; Santoro, I.L.; Carvalho, C.R.; Chiavegato, L.D.; Faresin, S.M. Preoperative 6-min walking distance does not predict pulmonary complications in upper abdominal surgery. Respirology 2012, 17, 1013–1017. [Google Scholar] [CrossRef]
- Vaz Fragoso, C.A.; McAvay, G.; Van Ness, P.H.; Casaburi, R.; Jensen, R.L.; MacIntyre, N.; Gill, T.M.; Yaggi, H.K.; Concato, J. Phenotype of normal spirometry in an aging population. Am. J. Respir. Crit. Care Med. 2015, 192, 817–825. [Google Scholar] [CrossRef] [PubMed]
- Graham, B.L.; Steenbruggen, I.; Miller, M.R.; Barjaktarevic, I.Z.; Cooper, B.G.; Hall, G.L.; Hallstrand, T.S.; Kaminsky, D.A.; McCarthy, K.; McCormack, M.C.; et al. Standardization of Spirometry 2019 Update. An Official American Thoracic Society and European Respiratory Society Technical Statement. Am. J. Respir. Crit. Care Med. 2019, 200, 70–88. [Google Scholar] [CrossRef] [PubMed]
- Brunelli, A.; Sabbatini, A.; Xiume’, F.; Borri, A.; Salati, M.; Marasco, R.D.; Fianchini, A. Inability to perform maximal stair climbing test before lung resection: A propensity score analysis on early outcome. Eur. J. Cardiothorac. Surg. 2005, 27, 367–372. [Google Scholar] [CrossRef]
- Depypere, L.P.; Daddi, N.; Gooseman, M.R.; Batirel, H.F.; Brunelli, A. The impact of coronavirus disease 2019 on the practice of thoracic oncology surgery: A survey of members of the European Society of Thoracic Surgeons (ESTS). Eur. J. Cardiothorac. Surg. 2020, 58, 752–762. [Google Scholar] [CrossRef]
| Smoking | 92.0% |
| Age | 64 (±6) |
| Pack-years | 40 (±17.35) |
| FEV1 [dm3] | 2.28 (±0.79) |
| FEV1% | 88 (±20.13) |
| FVC [dm3] | 3.09 (±0.91) |
| FVC% | 96.5% (±21.16) |
| Complications rate | 17.9% |
| Hospital mortality | 1 (1.12%) |
| 30-day mortality | 0 (0.0%) |
| 90-day mortality | 3 (3.4%) |
| Median postoperative stay [days] | 7 (±6.16) |
| Clinical Feature |
<500 m n = 191 |
≥500 m n = 433 | p |
<100% n = 191 |
≥100% n = 433 | p |
|---|---|---|---|---|---|---|
| Smoking | 172 (90.1%) | 405 (93.5%) | 0.129 | 180 (94.2%) | 397 (91.7%) | 0.265 |
| Pack-years | 40 ± 16.6 | 35 ± 19.2 | 0.713 | 40 ± 18.4 | 35 ± 18.3 | 0.002 |
| Age | 70 ± 6.8 | 63 ± 8.5 | <0.001 | 64 ± 9.9 | 65 ± 7.8 | 0.151 |
| FEV1 | 1.97 ± 0.6 | 2.37 ± 2.39 | <0.001 | 2.34 ± 0.8 | 2.21 ± 2.4 | 0.379 |
| FEV1% | 84 ± 20.3 | 88 ± 20.5 | 0.041 | 81 ± 19.8 | 90 ± 20.3 | <0.001 |
| FVC | 2.79 ± 5.2 | 3.39 ± 0.9 | <0.001 | 3.37 ± 5.1 | 3.16 ± 0.9 | 0.096 |
| FVC% | 94 ± 19.7 | 100 ± 19.2 | 0.003 | 93 ± 18.7 | 101 ± 19.5 | 0.002 |
| 6MWD | 445 ± 65.4 | 567 ± 52.8 | <0.001 | 469.5 ± 101.1 | 558 ± 65.4 | <0.001 |
| 6MWD% | 95.47 ± 18.8 | 110.49 ± 12.1 | <0.001 | 92.8 ± 13.5 | 112.66 ± 10.0 | <0.001 |
| VATS | 51 (26.7%) | 150 (34.7%) | 0.05 | 53 (27.7%) | 148 (34.2%) | 0.113 |
| Tis | 3 (1.6%) | 8 (1.9%) | 0.793 | 2 (1.0%) | 9 (2.1%) | 0.357 |
| pIA | 64 (33.5%) | 143 (33.0%) | 0.996 | 65 (34.0%) | 142 (32.8%) | 0.850 |
| pIB | 52 (27.2%) | 116 (26.8%) | 0.988 | 46 (24.1%) | 122 (28.2%) | 0.247 |
| pIIA | 24 (12.6%) | 67 (15.5%) | 0.311 | 20 (10.5%) | 71 (16.4%) | 0.046 |
| pIIB | 23 (12.0%) | 42 (9.7%) | 0.409 | 29 (15.2%) | 36 (8.3%) | 0.012 |
| pIIIA | 23 (12.0%) | 49 (11.3%) | 0.839 | 26 (13.6%) | 46 (10.6%) | 0.309 |
| pIIIB | 0 (0%) | 2 (0.5%) | 0.344 | 1 (0.5%) | 1 (0.2%) | 0.558 |
| pIV | 2 (1.0%) | 0 (0%) | 0.034 | 2 (1.0%) | 0 (0%) | 0.034 |
| CCI 0–3 | 61 (38.1%) | 249 (66.6%) | <0.001 | 81 (51.9%) | 229 (60.6%) | 0.066 |
| CCI 4+ | 99 (61.9%) | 125 (33.4%) | <0.001 | 75 (48.1%) | 149 (39.4%) | 0.066 |
| Clinical Feature |
<500 m n = 191 |
≥500 m n = 433 | p | OR (95% CI) |
|---|---|---|---|---|
| Complication rate | 100 (52.4%) | 183 (42.3%) | 0.019 | 1.501 (1.066–2.114) |
| Cardiopulmonary complications rate | 76 (39.8%) | 149 (34.4%) | 0.198 | 1.260 (0.887–1.790) |
| Atrial arrythmia | 33 (17.3%) | 63 (14.6%) | 0.385 | 1.227 (0.774–1.944) |
| Persistent air leak | 16 (8.4%) | 43 (9.9%) | 0.541 | 0.829 (0.455–1.513) |
| Atelectasis requiring aspiration | 24 (12.6%) | 45 (10.4%) | 0.426 | 1.239 (0.731–2.100) |
| Transfusion of >2 units of blood | 7 (3.7%) | 7 (1.6%) | 0.121 | 2.315 (0.801–6.695) |
| Drainage time | 4 (0–25) | 4 (1–25) | 0.506 | - |
| Hospital stay | 7 (0–102) | 6 (0–83) | 0.010 | - |
| 30-day mortality | 4 (2.1%) | 3 (0.7%) | 0.209 | 3.066 (0.679–13.834) |
| 90-day mortality | 6 (3.1%) | 10 (2.3%) | 0.586 | 1.372 (0.491–3.830) |
| Clinical feature | <100% n = 191 | ≥100% n = 433 | p | OR (95% CI) |
| Complication rate | 96 (50.3%) | 187 (43.2%) | 0.102 | 1.329 (0.945–1.871) |
| Cardiopulmonary complications rate | 80 (41.9%) | 145 (33.5%) | 0.045 | 1.432 (1.009–2.031) |
| Atrial arrythmia | 26 (13.6%) | 70 (16.2%) | 0.416 | 0.817 (0.503–1.329) |
| Persistent air leak | 22 (11.5%) | 37 (8.6%) | 0.244 | 1.393 (0.798–2.433) |
| Atelectasis requiring aspiration | 27 (14.1%) | 42 (9.7%) | 0.106 | 1.533 (0.914–2.570) |
| Transfusion of >2 units of blood | 7 (3.7%) | 7 (1.6%) | 0.121 | 2.315 (0.801–6.695) |
| Drainage time | 5 (0–25) | 7 (0–102) | 0.005 | - |
| Hospital stay | 4 (1–25) | 6 (0–83) | <0.001 | - |
| 30-day mortality | 5 (2.6%) | 2 (0.5%) | 0.031 | 5.793 (1.114–30.128) |
| 90-day mortality | 8 (4.2%) | 8 (1.8%) | 0.102 | 2.322 (0.858–6.283) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Marjanski, T.; Wnuk, D.; Dziedzic, R.; Ostrowski, M.; Sawicka, W.; Rzyman, W. 500 Meters Is a Result of 6-Minute Walk Test Which Differentiates Patients with High and Low Risk of Postoperative Complications after Lobectomy—A Validation Study. J. Clin. Med. 2021, 10, 1686. https://doi.org/10.3390/jcm10081686
Marjanski T, Wnuk D, Dziedzic R, Ostrowski M, Sawicka W, Rzyman W. 500 Meters Is a Result of 6-Minute Walk Test Which Differentiates Patients with High and Low Risk of Postoperative Complications after Lobectomy—A Validation Study. Journal of Clinical Medicine. 2021; 10(8):1686. https://doi.org/10.3390/jcm10081686
Chicago/Turabian StyleMarjanski, Tomasz, Damian Wnuk, Robert Dziedzic, Marcin Ostrowski, Wioletta Sawicka, and Witold Rzyman. 2021. "500 Meters Is a Result of 6-Minute Walk Test Which Differentiates Patients with High and Low Risk of Postoperative Complications after Lobectomy—A Validation Study" Journal of Clinical Medicine 10, no. 8: 1686. https://doi.org/10.3390/jcm10081686
APA StyleMarjanski, T., Wnuk, D., Dziedzic, R., Ostrowski, M., Sawicka, W., & Rzyman, W. (2021). 500 Meters Is a Result of 6-Minute Walk Test Which Differentiates Patients with High and Low Risk of Postoperative Complications after Lobectomy—A Validation Study. Journal of Clinical Medicine, 10(8), 1686. https://doi.org/10.3390/jcm10081686






