Admission High-Sensitive Cardiac Troponin T Level Increase Is Independently Associated with Higher Mortality in Critically Ill Patients with COVID-19: A Multicenter Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Settings
2.2. Participants
2.3. Data Collection
2.4. Statistical Analysis
3. Results
3.1. Study Population
3.2. Outcomes
3.3. Factors Associated with In-Hospital Mortality
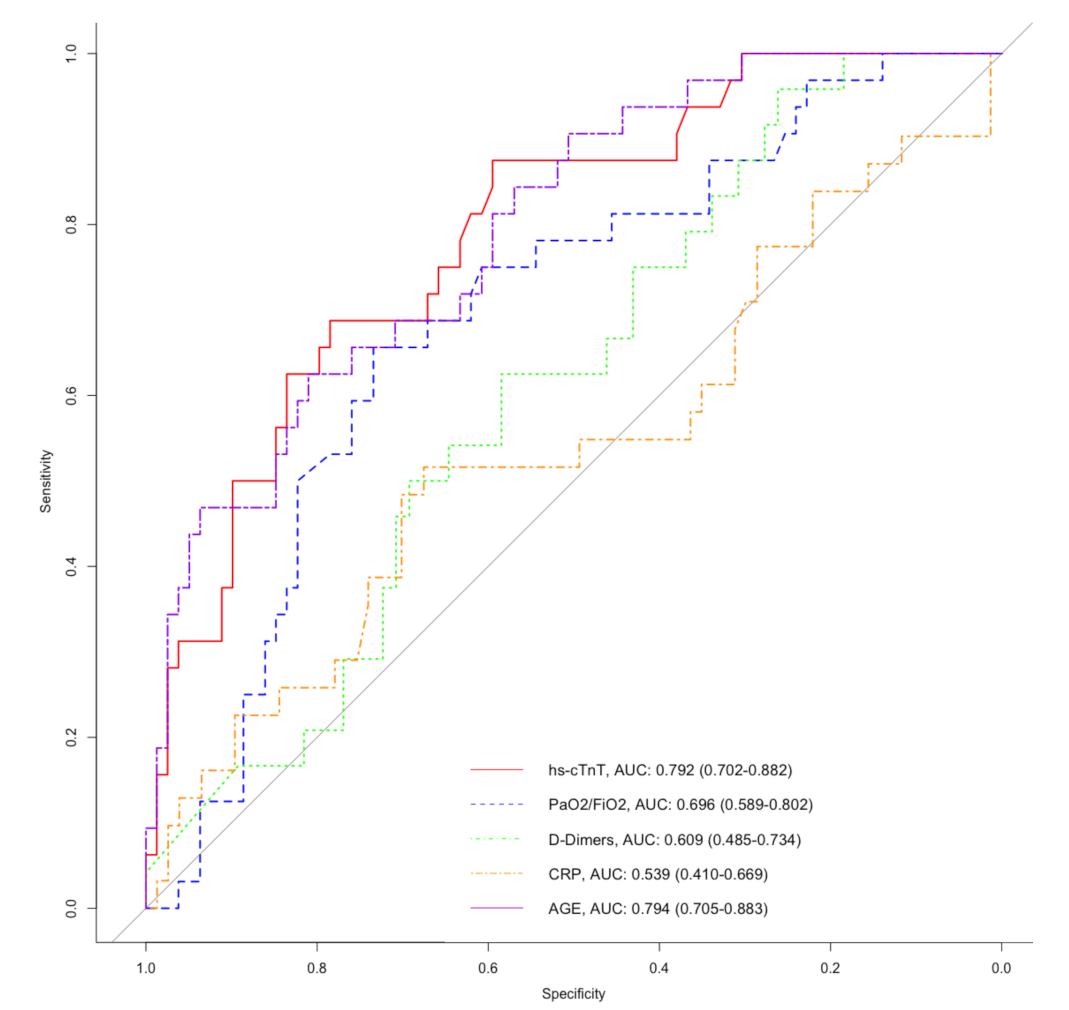
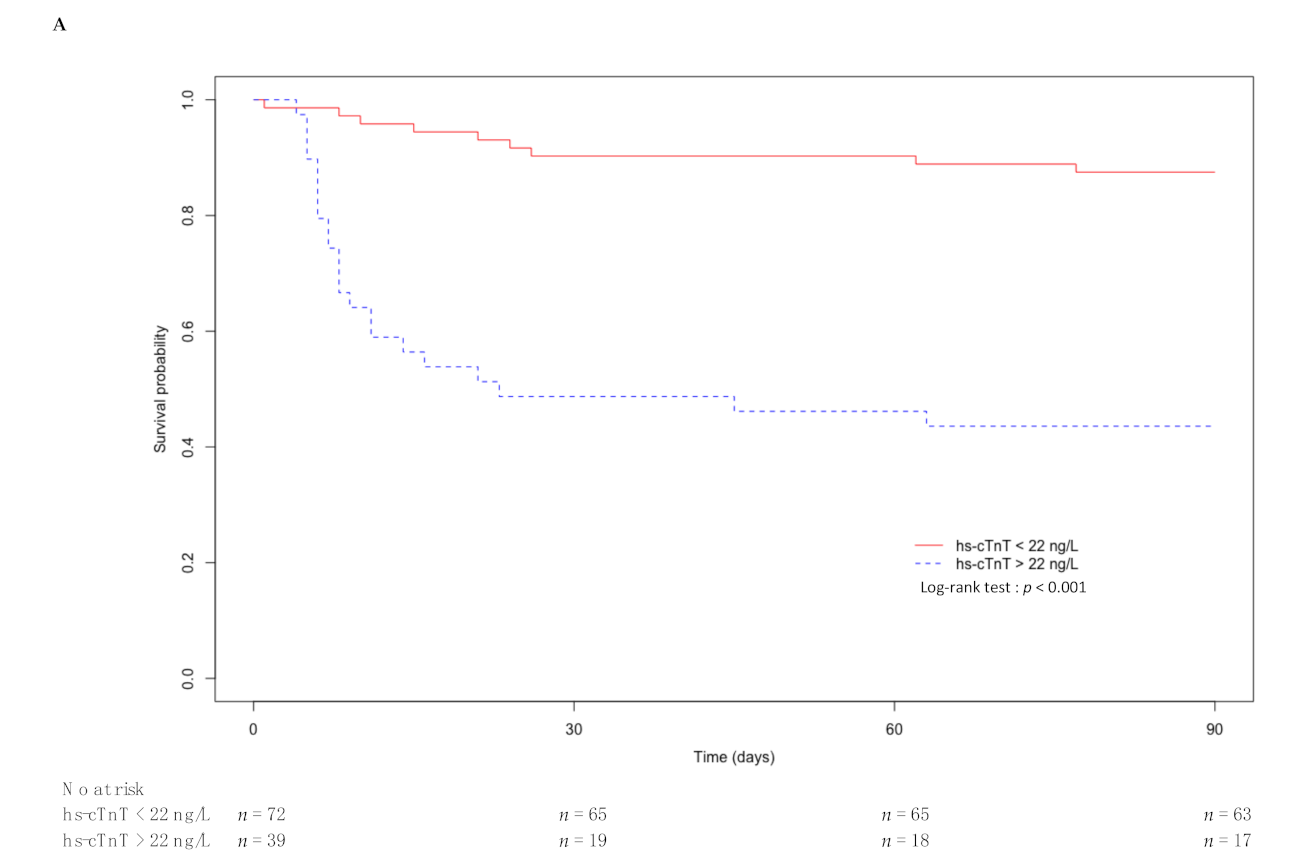
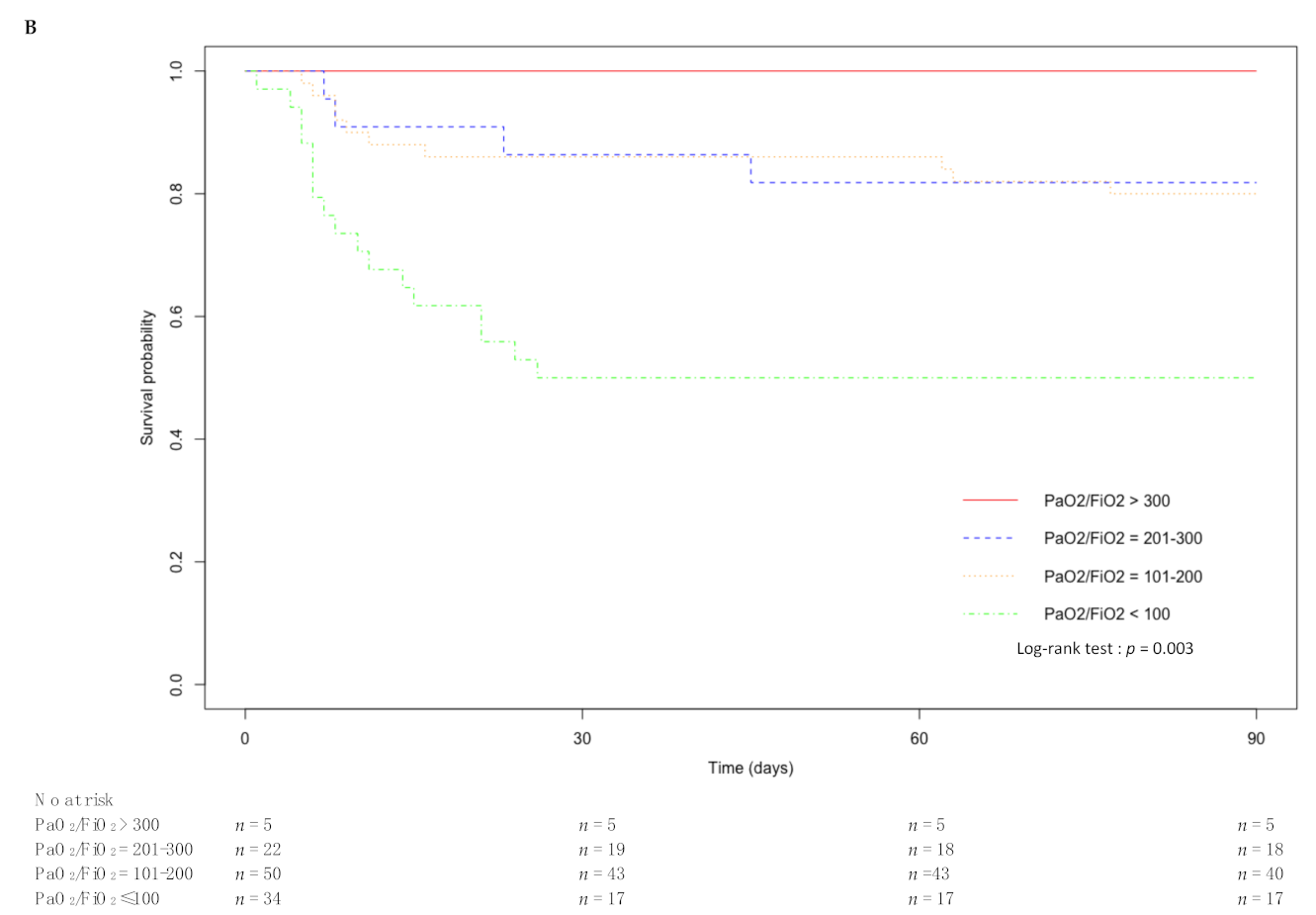
3.4. ROC Curves of the Main Prognostic Factors of Mortality at ICU Admission
3.5. Factors Associated with Invasive Mechanical Ventilation Needs
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Guan, W.J.; Ni, Z.Y.; Hu, Y.; Liang, W.H.; Ou, C.Q.; He, J.X.; Liu, L.; Shan, H.; Lei, C.L.; Hui, D.S.C.; et al. Clinical Characteristics of Coronavirus Disease 2019 in China. N. Engl. J. Med. 2020, 382, 1708–1720. [Google Scholar] [CrossRef] [PubMed]
- Alhazzani, W.; Møller, M.H.; Arabi, Y.M.; Loeb, M.; Gong, M.N.; Oczkowski, S.; Levy, M.M.; Derde, L.; Dzierba, A.; Du, B.; et al. Surviving Sepsis Campaign: Guidelines on the Management of Critically Ill Adults with Coronavirus Disease 2019 (COVID-19). Intensive Care Med. 2020, 104, 854–887. [Google Scholar] [CrossRef] [PubMed]
- Zheng, Y.-Y.; Ma, Y.-T.; Zhang, J.-Y.; Xie, X. COVID-19 and the cardiovascular system. Nat. Rev. Cardiol. 2020, 17, 259–260. [Google Scholar] [CrossRef] [PubMed]
- Madjid, M.; Safavi-Naeini, P.; Solomon, S.D.; Vardeny, O. Potential Effects of Coronaviruses on the Cardiovascular System: A Review. JAMA Cardiol. 2020, 5, 831. [Google Scholar] [CrossRef] [PubMed]
- Fried, J.A.; Ramasubbu, K.; Bhatt, R.; Topkara, V.K.; Clerkin, K.J.; Horn, E.; Rabbani, L.; Brodie, D.; Jain, S.S.; Kirtane, A.J.; et al. The Variety of Cardiovascular Presentations of COVID-19. Circulation 2020, 141, 1930–1936. [Google Scholar] [CrossRef]
- Li, L.; Hill, J.; Spratt, J.C.; Jin, Z. Myocardial injury in severe COVID-19: Identification and management. Resuscitation 2021, 160, 16–17. [Google Scholar] [CrossRef]
- Inciardi, R.M.; Adamo, M.; Lupi, L.; Cani, D.S.; Di Pasquale, M.; Tomasoni, D.; Italia, L.; Zaccone, G.; Tedino, C.; Fabbricatore, D.; et al. Characteristics and outcomes of patients hospitalized for COVID-19 and cardiac disease in Northern Italy. Eur. Heart J. 2020, 41, 1821–1829. [Google Scholar] [CrossRef]
- Shi, S.; Qin, M.; Cai, Y.; Liu, T.; Shen, B.; Yang, F.; Cao, S.; Liu, X.; Xiang, Y.; Zhao, Q.; et al. Characteristics and clinical significance of myocardial injury in patients with severe coronavirus disease 2019. Eur. Heart J. 2020, 41, 2070–2079. [Google Scholar] [CrossRef]
- Huang, C.; Wang, Y.; Li, X.; Ren, L.; Zhao, J.; Hu, Y.; Zhang, L.; Fan, G.; Xu, J.; Gu, X.; et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020, 395, 497–506. [Google Scholar] [CrossRef]
- Zhou, F.; Yu, T.; Du, R.; Fan, G.; Liu, Y.; Liu, Z.; Xiang, J.; Wang, Y.; Song, B.; Gu, X.; et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. Lancet 2020, 395, 1054–1062. [Google Scholar] [CrossRef]
- Chen, R.; Liang, W.; Jiang, M.; Guan, W.; Zhan, C.; Wang, T.; Tang, C.; Sang, L.; Liu, J.; Ni, Z.; et al. Risk Factors of Fatal Outcome in Hospitalized Subjects With Coronavirus Disease 2019 From a Nationwide Analysis in China. Chest 2020, 158, 97–105. [Google Scholar] [CrossRef]
- Wang, Y.; Lu, X.; Li, Y.; Chen, H.; Chen, T.; Su, N.; Huang, F.; Zhou, J.; Zhang, B.; Yan, F.; et al. Clinical Course and Outcomes of 344 Intensive Care Patients with COVID-19. Am. J. Respir. Crit. Care Med. 2020, 201, 1430–1434. [Google Scholar] [CrossRef]
- Guo, T.; Fan, Y.; Chen, M.; Wu, X.; Zhang, L.; He, T.; Wang, H.; Wan, J.; Wang, X.; Lu, Z. Cardiovascular Implications of Fatal Outcomes of Patients With Coronavirus Disease 2019 (COVID-19). JAMA Cardiol. 2020, 5, 811–818. [Google Scholar] [CrossRef] [PubMed]
- Lippi, G.; Lavie, C.J.; Sanchis-Gomar, F. Cardiac troponin I in patients with coronavirus disease 2019 (COVID-19): Evidence from a meta-analysis. Prog. Cardiovasc. Dis. 2020, 63, 390–391. [Google Scholar] [CrossRef]
- Du, R.-H.; Liang, L.-R.; Yang, C.-Q.; Wang, W.; Cao, T.-Z.; Li, M.; Guo, G.-Y.; Du, J.; Zheng, C.-L.; Zhu, Q.; et al. Predictors of mortality for patients with COVID-19 pneumonia caused by SARS-CoV-2: A prospective cohort study. Eur. Respir. J. 2020, 55, 2000524. [Google Scholar] [CrossRef] [PubMed]
- Wang, D.; Hu, B.; Hu, C.; Zhu, F.; Liu, X.; Zhang, J.; Wang, B.; Xiang, H.; Cheng, Z.; Xiong, Y.; et al. Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus–Infected Pneumonia in Wuhan, China. JAMA 2020, 323, 1061–1069. [Google Scholar] [CrossRef] [PubMed]
- Arentz, M.; Yim, E.; Klaff, L.; Lokhandwala, S.; Riedo, F.X.; Chong, M.; Lee, M. Characteristics and Outcomes of 21 Critically Ill Patients With COVID-19 in Washington State. JAMA 2020, 323, 1612. [Google Scholar] [CrossRef] [PubMed]
- Bhatraju, P.K.; Ghassemieh, B.J.; Nichols, M.; Kim, R.; Jerome, K.R.; Nalla, A.K.; Greninger, A.L.; Pipavath, S.; Wurfel, M.M.; Evans, L.; et al. Covid-19 in Critically Ill Patients in the Seattle Region—Case Series. N. Engl. J. Med. 2020, 382, 2012–2022. [Google Scholar] [CrossRef] [PubMed]
- Ruan, Q.; Yang, K.; Wang, W.; Jiang, L.; Song, J. Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China. Intensiv. Care Med. 2020, 46, 846–848. [Google Scholar] [CrossRef] [PubMed]
- Charlson, M.; Szatrowski, T.P.; Peterson, J.; Gold, J. Validation of a combined comorbidity index. J. Clin. Epidemiol. 1994, 47, 1245–1251. [Google Scholar] [CrossRef]
- Le Gall, J.-R.; Lemeshow, S.; Saulnier, F. A New Simplified Acute Physiology Score (SAPS II) Based on a European/North American Multicenter Study. JAMA 1993, 270, 2957–2963. [Google Scholar] [CrossRef]
- Force, A.D.T.; Ranieri, V.M.; Rubenfeld, G.D.; Thompson, B.T.; Ferguson, N.D.; Caldwell, E.; Fan, E.; Camporota, L.; Slutsky, A.S. Acute Respiratory Distress Syndrome: The Berlin Definition. JAMA 2012, 307, 2526–2533. [Google Scholar] [CrossRef]
- Karagiannidis, C.; Mostert, C.; Hentschker, C.; Voshaar, T.; Malzahn, J.; Schillinger, G.; Klauber, J.; Janssens, U.; Marx, G.; Weber-Carstens, S.; et al. Case characteristics, resource use, and outcomes of 10 021 patients with COVID-19 admitted to 920 German hospitals: An observational study. Lancet Respir. Med. 2020, 8, 853–862. [Google Scholar] [CrossRef]
- Grasselli, G.; Zangrillo, A.; Zanella, A.; Antonelli, M.; Cabrini, L.; Castelli, A.; Cereda, D.; Coluccello, A.; Foti, G.; Fumagalli, R.; et al. Baseline Characteristics and Outcomes of 1591 Patients Infected with SARS-CoV-2 Admitted to ICUs of the Lombardy Region, Italy. JAMA 2020, 323, 1574–1581. [Google Scholar] [CrossRef]
- Herridge, M.S.; Chu, L.M.; Matte, A.; Tomlinson, G.; Chan, L.; Thomas, C.; Friedrich, J.O.; Mehta, S.; Lamontagne, F.; Levasseur, M.; et al. The RECOVER Program: Disability Risk Groups and 1-Year Outcome after 7 or More Days of Mechanical Ventilation. Am. J. Respir. Crit. Care Med. 2016, 194, 831–844. [Google Scholar] [CrossRef]
- Villar, J.; Ambrós, A.; Soler, J.A.; Martínez, D.; Ferrando, C.; Solano, R.; Mosteiro, F.; Blanco, J.; Martín-Rodríguez, C.; Fernández, M.D.M.; et al. Age, PaO2/FIO2, and Plateau Pressure Score: A Proposal for a Simple Outcome Score in Patients with the Acute Respiratory Distress Syndrome. Crit. Care Med. 2016, 44, 1361–1369. [Google Scholar] [CrossRef] [PubMed]
- Gunduz, R.; Yildiz, B.S.; Ozdemir, I.H.; Cetin, N.; Ozen, M.B.; Bakir, E.O.; Ozgur, S.; Bayturan, O. CHA2DS2-VASc score and modified CHA2DS2-VASc score can predict mortality and intensive care unit hospitalization in COVID-19 patients. J. Thromb. Thrombolysis 2021. [Google Scholar] [CrossRef] [PubMed]
- Danwang, C.; Endomba, F.T.; Nkeck, J.R.; Wouna, D.L.A.; Robert, A.; Noubiap, J.J. A meta-analysis of potential biomarkers associated with severity of coronavirus disease 2019 (COVID-19). Biomark. Res. 2020, 8, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Demir, O.M.; Ryan, M.; Cirillo, C.; Desai, N.; Pericao, A.; Sinclair, H.; Stylianidis, V.; Victor, K.; Alaour, B.; Jones, A.; et al. Impact and Determinants of High-Sensitivity Cardiac Troponin-T Concentration in Patients With COVID-19 Admitted to Critical Care. Am. J. Cardiol. 2021. [Google Scholar] [CrossRef] [PubMed]
- Metkus, T.S.; Sokoll, L.J.; Barth, A.S.; Czarny, M.J.; Hays, A.G.; Lowenstein, C.J.; Michos, E.D.; Nolley, E.P.; Post, W.S.; Resar, J.R.; et al. Myocardial Injury in Severe COVID-19 Compared with Non–COVID-19 Acute Respiratory Distress Syndrome. Circulation 2021, 143, 553–565. [Google Scholar] [CrossRef]
- Sandoval, Y.; Januzzi, J.L.; Jaffe, A.S. Cardiac Troponin for Assessment of Myocardial Injury in COVID-19. J. Am. Coll. Cardiol. 2020, 76, 1244–1258. [Google Scholar] [CrossRef]
- Musher, D.M.; Abers, M.S.; Corrales-Medina, V.F. Acute Infection and Myocardial Infarction. N. Engl. J. Med. 2019, 380, 171–176. [Google Scholar] [CrossRef]
- Collet, J.-P.; Thiele, H.; Barbato, E.; Barthélémy, O.; Bauersachs, J.; Bhatt, D.L.; Dendale, P.; Dorobantu, M.; Edvardsen, T.; Folliguet, T.; et al. 2020 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. Eur. Heart J. 2020, 79. [Google Scholar] [CrossRef]
- Doyen, D.; Moceri, P.; Ducreux, D.; Dellamonica, J. Myocarditis in a patient with COVID-19: A cause of raised troponin and ECG changes. Lancet 2020, 395, 1516. [Google Scholar] [CrossRef]
- Imazio, M.; Klingel, K.; Kindermann, I.; Brucato, A.; De Rosa, F.G.; Adler, Y.; De Ferrari, G.M. COVID-19 pandemic and troponin: Indirect myocardial injury, myocardial inflammation or myocarditis? Heart 2020, 106, 1127–1131. [Google Scholar] [CrossRef]
- Lala, A.; Johnson, K.W.; Januzzi, J.L.; Russak, A.J.; Paranjpe, I.; Richter, F.; Zhao, S.; Somani, S.; Van Vleck, T.; Vaid, A.; et al. Prevalence and Impact of Myocardial Injury in Patients Hospitalized With COVID-19 Infection. J. Am. Coll. Cardiol. 2020, 76, 533–546. [Google Scholar] [CrossRef]
- Caforio, A.L.P.; Pankuweit, S.; Arbustini, E.; Basso, C.; Gimeno-Blanes, J.; Felix, S.B.; Fu, M.; Heliö, T.; Heymans, S.; Jahns, R.; et al. Current state of knowledge on aetiology, diagnosis, management, and therapy of myocarditis: A position statement of the European Society of Cardiology Working Group on Myocardial and Pericardial Diseases. Eur. Heart J. 2013, 34, 2636–2648. [Google Scholar] [CrossRef]
- Jonigk, D.; Märkl, B.; Helms, J. COVID-19: What the clinician should know about post-mortem findings. Intensiv. Care Med. 2021, 47, 86–89. [Google Scholar] [CrossRef] [PubMed]
- Klok, F.A.; Kruip, M.J.H.A.; van der Meer, N.J.M.; Arbous, M.S.; Gommers, D.A.M.P.J.; Kant, K.M.; Kaptein, F.H.J.; van Paassen, J.; Stals, M.A.M.; Huisman, M.V.; et al. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb. Res. 2020, 191, 145–147. [Google Scholar] [CrossRef]
- Klouche, K.; Pommet, S.; Amigues, L.; Bargnoux, A.S.; Dupuy, A.M.; Machado, S.; Serveaux-Delous, M.; Morena, M.; Jonquet, O.; Cristol, J.P. Plasma Brain Natriuretic Peptide and Troponin Levels in Severe Sepsis and Septic Shock: Relationships with Systolic Myocardial Dysfunction and Intensive Care Unit Mortality. J. Intensiv. Care Med. 2012, 29, 229–237. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.-S.; Kim, M.; Kim, Y.-J.; Ryoo, S.M.; Sohn, C.H.; Ahn, S.; Kim, W.Y. Troponin Testing for Assessing Sepsis-Induced Myocardial Dysfunction in Patients with Septic Shock. J. Clin. Med. 2019, 8, 239. [Google Scholar] [CrossRef] [PubMed]
- Gayat, E.; Cariou, A.; Deye, N.; Vieillard-Baron, A.; Jaber, S.; Damoisel, C.; Lu, Q.; Monnet, X.; Rennuit, I.; Azoulay, E.; et al. Determinants of long-term outcome in ICU survivors: Results from the FROG-ICU study. Crit. Care 2018, 22, 1–10. [Google Scholar] [CrossRef]
- Landesberg, G.; Jaffe, A.S.; Gilon, D.; Levin, P.D.; Goodman, S.; Abu-Baih, A.; Beeri, R.; Weissman, C.; Sprung, C.L.; Landesberg, A. Troponin Elevation in Severe Sepsis and Septic Shock: The Role of Left Ventricular Diastolic Dysfunction and Right Ventricular Dilatation. Crit. Care Med. 2014, 42, 790–800. [Google Scholar] [CrossRef] [PubMed]
- Moutchia, J.; Pokharel, P.; Kerri, A.; McGaw, K.; Uchai, S.; Nji, M.; Goodman, M. Clinical laboratory parameters associated with severe or critical novel coronavirus disease 2019 (COVID-19): A systematic review and meta-analysis. PLoS ONE 2020, 15, e0239802. [Google Scholar] [CrossRef] [PubMed]
- Auld, S.C.; Caridi-Scheible, M.; Blum, J.M.; Robichaux, C.; Kraft, C.; Jacob, J.T.; Jabaley, C.S.; Carpenter, D.; Kaplow, R.; Hernandez-Romieu, A.C.; et al. ICU and Ventilator Mortality Among Critically Ill Adults with Coronavirus Disease 2019. Crit. Care Med. 2020. [Google Scholar] [CrossRef]

| Total (n = 111) | Non-Survivor (n = 32) | Survivor (n = 79) | p-Value | |
|---|---|---|---|---|
| Age (years), median (IQR) | 67 (58–75) | 75 (67–81) | 63.0 (56–72) | <0.001 |
| Male, n (%) | 75 (68%) | 16 (50%) | 59 (75%) | 0.01 |
| BMI 1 (kg/m²), median (IQR) | 28 (25–32) | 26 (23–31) | 28 (25–32) | 0.57 |
| Hypertension, n (%) | 52 (47%) | 18 (56%) | 34 (43%) | 0.21 |
| Diabetes, n (%) | 33 (31%) | 12 (38%) | 22 (28%) | 0.32 |
| Chronic heart disease, n (%) | 22 (20%) | 10 (31%) | 12 (15%) | 0.06 |
| Chronic kidney disease, n (%) | 14 (13%) | 8 (25%) | 6 (8%) | 0.02 |
| Chronic pulmonary disease, n (%) | 22 (20%) | 11 (34%) | 11 (14%) | 0.02 |
| Charlson Index, median (IQR) | 3 (2–5) | 5 (4–8) | 3 (2–4) | <0.001 |
| SAPS II 2, median (IQR) | 37 (27–48) | 43 (34–54) | 33 (25–46) | 0.01 |
| PaO2/FiO2, median (IQR) | 140 (98–154) | 100 (85–139) | 160 (105–206) | 0.003 |
| PaO2/FiO2 ≤100, n (%) | 34 (31%) | 17 (53%) | 17 (22%) | 0.002 |
| Invasive mechanical ventilation, n (%) | 75 (68%) | 25 (78%) | 50 (63%) | 0.14 |
| Duration (days), median (IQR) | 10 (5–19) | 9 (6–16) | 12 (5–18) | - |
| Prone positioning, n (%) | 38 (34%) | 14 (44%) | 24 (30%) | 0.02 |
| ECMO 3, n (%) | 3 (3%) | 1 (3%) | 2 (3%) | 0.86 |
| Duration (days), median (IQR) | 17 (14–20) | - | - | - |
| Norepinephrine (>1 µg/kg/min), n (%) | 41 (37%) | 17 (53%) | 24 (30%) | 0.03 |
| Duration (days), median (IQR) | 7 (4–12) | 9 (5–15) | 5 (3–10) | - |
| RRT 4, n (%) | 17 (15%) | 10 (31%) | 7 (9%) | 0.005 |
| Duration (days), median (IQR) | 14 (4–31) | 10 (3–19) | 22 (10–38) | - |
| Creatininemia (µmol/L), median (IQR) | 84 (62–111) | 92 (72–168) | 82 (57–101) | 0.01 |
| hs-cTnT 5 (ng/L), median (IQR) | 16.0 (10.2–31.9) | 35.0 (16.8–106.0) | 12.5 (7.5–20.0) | <0.001 |
| CRP 6 (mg/L), median (IQR) | 153 (112–222) | 134 (93–215) | 154 (115–223) | 0.45 |
| PCT 7 (ng/mL), median (IQR) | 0.4 (0.2–0.9) | 0.6 (0.3–1.3) | 0.3 (0.2–0.9) | 0.11 |
| Lactatemia (mmol/L), median (IQR) | 1.3 (0.9–1.7) | 1.3 (0.8–1.8) | 1.3 (1.0–1.6) | 0.62 |
| D-dimer (ng/mL), median (IQR) | 890 (572–1950) | 1340 (658–1958) | 859 (497–1861) | 0.09 |
| LVEF 8 (%), median (IQR) | 60 (50–60) | 55 (50–60) | 60 (50–60) | 0.28 |
| TAPSE 9 (mm), median (IQR) | 18 (16–22) | 18 (14–23) | 18 (17–22) | 0.49 |
| ICU LOS 10 (days), median (IQR) | 10 (6–18) | 8 (5–17) | 10 (6–18) | - |
| Hospital LOS (days), median (IQR) | 19 (11–31) | 10 (7–22) | 21 (13–34) | - |
| Death, n (%) | 32 (29%) | - | - | - |
| Univariable Analysis Hazard Ratio (IC 95%) | p-Value | Multivariable Analysis Hazard Ratio (IC 95%) | p-Value | |
|---|---|---|---|---|
| Age | 1.1 (1.1–1.2) | 0.01 | 1.06 (0.99–1.14) | 0.11 |
| Male sex | 0.4 (0.2–0.81) | <0.001 | 0.50 (0.21–1.05) | 0.64 |
| BMI 1 | 0.99 (0.93–1.1) | 0.68 | ||
| Smokers | 0.5 (0.068–3.6) | 0.49 | ||
| Charlson Index | 1.3 (1.2–1.4) | <0.001 | 4.46 (0.26–75.55) | 0.30 |
| SAPS II 2 | 10 (1.7–58) | 0.01 | 1.06 (0.08–13.36) | 0.96 |
| PaO2/FiO2 ≤100 | 3.4 (1.7–6.8) | <0.001 | 4.65 (1.81–11.97) | 0.001 |
| Invasive mechanical ventilation | 1.8 (0.76–4.1) | 0.19 | 2.88 (0.76–10.97) | 0.12 |
| Norepinephrine (>1 µg/kg/min) | 2.1 (1–4.1) | 0.04 | 1.08 (0.30–2.84) | 0.90 |
| Renal replacement therapy | 2.9 (1.4–6.2) | 0.005 | 1.58 (0.58–4.31) | 0.37 |
| Creatininemia (log10) | 8.5 (2.3–32) | 0.002 | 1.45 (0.20–10.73) | 0.71 |
| Hs-cTnT 3 (log10) | 4.3 (2.5–7.2) | <0.001 | 4.96 (1.92–12.86) | <0.001 |
| CRP 4 (log10) | 0.83 (0.37–1.9) | 0.65 | ||
| PCT 5 (log10) | 1.7 (1–2.9) | 0.05 | 1.60 (0.60–4.25) | 0.3 |
| Lactatemia (log10) | 1.8 (0.21–16) | 0.58 | ||
| D-dimer (log10) | 2.4 (0.81–6.9) | 0.12 | 1.21 (0.17–3.95) | 0.8 |
| Sensibility (%) | Specificity (%) | PPV 1 (%) | NPV 2 (%) | |
|---|---|---|---|---|
| age ≥ 74 years old | 63 | 81 | 57 | 84 |
| hs-cTnT 3 ≥ 22 ng/L | 69 | 79 | 56 | 86 |
| PaO2/FiO2 ≤ 115 | 66 | 73 | 50 | 84 |
| PaO2/FiO2 ≤ 100 | 50 | 82 | 53 | 80 |
| D-dimer ≥ 500 ng/L | 96 | 26 | 34 | 94 |
| CRP 4 ≥ 135 mg/L | 52 | 68 | 39 | 78 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Larcher, R.; Besnard, N.; Akouz, A.; Rabier, E.; Teule, L.; Vandercamere, T.; Zozor, S.; Amalric, M.; Benomar, R.; Brunot, V.; et al. Admission High-Sensitive Cardiac Troponin T Level Increase Is Independently Associated with Higher Mortality in Critically Ill Patients with COVID-19: A Multicenter Study. J. Clin. Med. 2021, 10, 1656. https://doi.org/10.3390/jcm10081656
Larcher R, Besnard N, Akouz A, Rabier E, Teule L, Vandercamere T, Zozor S, Amalric M, Benomar R, Brunot V, et al. Admission High-Sensitive Cardiac Troponin T Level Increase Is Independently Associated with Higher Mortality in Critically Ill Patients with COVID-19: A Multicenter Study. Journal of Clinical Medicine. 2021; 10(8):1656. https://doi.org/10.3390/jcm10081656
Chicago/Turabian StyleLarcher, Romaric, Noemie Besnard, Aziz Akouz, Emmanuelle Rabier, Lauranne Teule, Thomas Vandercamere, Samuel Zozor, Matthieu Amalric, Racim Benomar, Vincent Brunot, and et al. 2021. "Admission High-Sensitive Cardiac Troponin T Level Increase Is Independently Associated with Higher Mortality in Critically Ill Patients with COVID-19: A Multicenter Study" Journal of Clinical Medicine 10, no. 8: 1656. https://doi.org/10.3390/jcm10081656
APA StyleLarcher, R., Besnard, N., Akouz, A., Rabier, E., Teule, L., Vandercamere, T., Zozor, S., Amalric, M., Benomar, R., Brunot, V., Corne, P., Barbot, O., Dupuy, A.-M., Cristol, J.-P., & Klouche, K. (2021). Admission High-Sensitive Cardiac Troponin T Level Increase Is Independently Associated with Higher Mortality in Critically Ill Patients with COVID-19: A Multicenter Study. Journal of Clinical Medicine, 10(8), 1656. https://doi.org/10.3390/jcm10081656







