Alignment of Physical Activity in Older Couples Affected by Osteoarthritis: Investigation by Accelerometry and Questionnaire
Abstract
:1. Introduction
2. Materials and Methods
2.1. Sample Recruitment and Data Collection
2.2. Instruments
2.3. Statistical Analysis
3. Results
3.1. Clinical and Sociodemographic Characteristics of the Study Population
3.1.1. Group-Specific Interrelatedness of PA Assessments
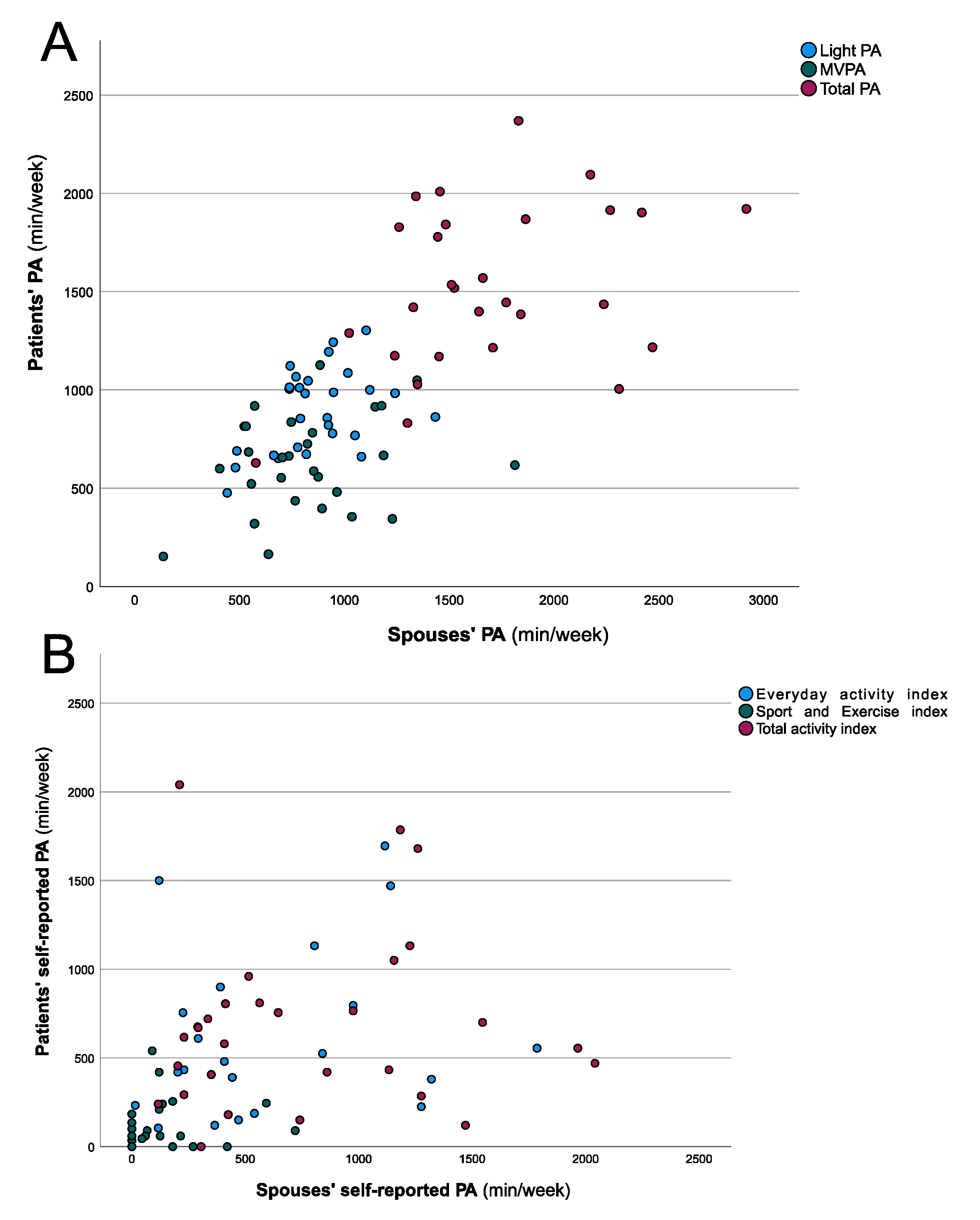
3.1.2. Alignment of PA Between the OA Patients and Their Spouses
4. Discussion
4.1. PA in OA Patients and Their Spouses under Everyday Conditions
4.2. Correlation of PA Assessed by Different Methods
4.3. Strengths and Limitations of the Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Cross, M.; Smith, E.; Hoy, D.; Nolte, S.; Ackerman, I.; Fransen, M.; Bridgett, L.; Williams, S.; Guillemin, F.; Hill, C.L. The global burden of hip and knee osteoarthritis: Estimates from the global burden of disease 2010 study. Ann. Rheum. Dis. 2014. [Google Scholar] [CrossRef] [PubMed]
- Gay, C.; Chabaud, A.; Guilley, E.; Coudeyre, E. Educating patients about the benefits of physical activity and exercise for their hip and knee osteoarthritis. Systematic literature review. Ann. Phys. Rehabil. Med. 2016, 59, 174–183. [Google Scholar] [CrossRef] [PubMed]
- Sliepen, M.; Mauricio, E.; Lipperts, M.; Grimm, B.; Rosenbaum, D. Objective assessment of physical activity and sedentary behaviour in knee osteoarthritis patients—beyond daily steps and total sedentary time. BMC Musculoskelet. Disord. 2018, 19, 64. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fransen, M.; McConnell, S. Land-based exercise for osteoarthritis of the knee: A metaanalysis of randomized controlled trials. J. Rheumatol. 2009, 36, 1109–1117. [Google Scholar] [CrossRef] [PubMed]
- De Groot, I.; Bussmann, J.; Stam, H.; Verhaar, J. Actual everyday physical activity in patients with end-stage hip or knee osteoarthritis compared with healthy controls. Osteoarthr. Cartil. 2008, 16, 436–442. [Google Scholar] [CrossRef] [Green Version]
- Wallis, J.A.; Webster, K.E.; Levinger, P.; Taylor, N.F. What proportion of people with hip and knee osteoarthritis meet physical activity guidelines? A systematic review and meta-analysis. Osteoarthr. Cartil. 2013, 21, 1648–1659. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- La Guardia, J.G.; Patrick, H. The influence of the social environment on health behavior. In Human Motivation and Interpersonal Relationships; Weinstein, N., Ed.; Springer International Publishing: Cham, Switzerland, 2014; pp. 299–315. [Google Scholar]
- Hoppmann, C.A.; Gerstorf, D. Biobehavioral pathways underlying spousal health dynamics: Its nature, correlates, and consequences. Gerontology 2014, 60, 458–465. [Google Scholar] [CrossRef] [Green Version]
- Martire, L.M.; Stephens, M.A.P.; Mogle, J.; Schulz, R.; Brach, J.; Keefe, F.J. Daily spousal influence on physical activity in knee osteoarthritis. Ann. Behav. Med. 2012, 45, 213–223. [Google Scholar] [CrossRef] [Green Version]
- Harada, K.; Masumoto, K.; Kondo, N. Spousal Concordance for Objectively Measured Sedentary Behavior and Physical Activity Among Middle-Aged and Older Couples. Res. Q. Exerc. Sport 2018, 89, 440–449. [Google Scholar] [CrossRef]
- Berli, C.; Luscher, J.; Luszczynska, A.; Schwarzer, R.; Scholz, U. Couples’ daily self-regulation: The Health Action Process Approach at the dyadic level. PLoS ONE 2018, 13, e0205887. [Google Scholar] [CrossRef]
- Jackson, S.E.; Steptoe, A.; Wardle, J. The influence of partner’s behavior on health behavior change: The English Longitudinal Study of Ageing. JAMA Intern. Med. 2015, 175, 385–392. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, K.K.; Cardinal, B.J.; Acock, A.C. Concordance of Physical Activity Trajectories Among Middle-Aged and Older Married Couples: Impact of Diseases and Functional Difficulties. J. Gerontol. Ser. B Psychol. Sci. Soc. Sci. 2013, 68, 794–806. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Meyler, D.; Stimpson, J.P.; Peek, M.K. Health concordance within couples: A systematic review. Soc. Sci. Med. 2007, 64, 2297–2310. [Google Scholar] [CrossRef]
- Smith, K.R.; Zick, C.D. Linked lives, dependent demise? Survival analysis of husbands and wives. Demography 1994, 31, 81–93. [Google Scholar] [CrossRef] [PubMed]
- Skoyen, J.A.; Blank, E.; Corkery, S.A.; Butler, E.A. The interplay of partner influence and individual values predicts daily fluctuations in eating and physical activity. J. Soc. Pers. Relatsh. 2013, 30, 1000–1019. [Google Scholar] [CrossRef]
- Pauly, T.; Keller, J.; Knoll, N.; Michalowski, V.I.; Hohl, D.H.; Ashe, M.C.; Gerstorf, D.; Madden, K.M.; Hoppmann, C.A. Moving in Sync: Hourly Physical Activity and Sedentary Behavior are Synchronized in Couples. Ann. Behav. Med. 2020, 54, 10–21. [Google Scholar] [CrossRef]
- Manne, S.; Badr, H. Intimacy and relationship processes in couples’ psychosocial adaptation to cancer. Cancer 2008, 112, 2541–2555. [Google Scholar] [CrossRef] [Green Version]
- Moellenbeck, B.; Kalisch, T.; Gosheger, G.; Horst, F.; Seeber, L.; Theil, C.; Schmidt-Braekling, T.; Dieckmann, R. Behavioral Conformity of Physical Activity and Sedentary Behavior in Older Couples with One Partner Suffering from End-Stage Osteoarthritis. Clin. Interv. Aging 2020, 15, 61–74. [Google Scholar] [CrossRef] [Green Version]
- Sliepen, M.; Brandes, M.; Rosenbaum, D. Current Physical Activity Monitors in Hip and Knee Osteoarthritis: A Review. Arthritis Care Res. 2017, 69, 1460–1466. [Google Scholar] [CrossRef] [Green Version]
- Verlaan, L.; Bolink, S.A.; Van Laarhoven, S.N.; Lipperts, M.; Heyligers, I.C.; Grimm, B.; Senden, R. Accelerometer-based Physical Activity Monitoring in Patients with Knee Osteoarthritis: Objective and Ambulatory Assessment of Actual Physical Activity During Daily Life Circumstances. Open Biomed. Eng. J. 2015, 9, 157–163. [Google Scholar] [CrossRef] [Green Version]
- Lee, J.; Chang, R.W.; Ehrlich-Jones, L.; Kwoh, C.K.; Nevitt, M.; Semanik, P.A.; Sharma, L.; Sohn, M.W.; Song, J.; Dunlop, D.D. Sedentary behavior and physical function: Objective evidence from the Osteoarthritis Initiative. Arthritis Care Res. 2015, 67, 366–373. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Segura-Jiménez, V.; Álvarez-Gallardo, I.C.; Romero-Zurita, A.; Camiletti-Moirón, D.; Munguía-Izquierdo, D.; Carbonell-Baeza, A.; Ruiz, J.R. Comparison of physical activity using questionnaires (leisure time physical activity instrument and physical activity at home and work instrument) and accelerometry in fibromyalgia patients: The Al-Ándalus project. Arch. Phys. Med. Rehabil. 2014, 95, 1903–1911.e2. [Google Scholar] [CrossRef] [PubMed]
- Shephard, R.J. Limits to the measurement of habitual physical activity by questionnaires. Br. J. Sports Med. 2003, 37, 197–206. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Waddell, K.J.; Lang, C.E. Comparison of self-report versus sensor-based methods for measuring the amount of upper limb activity outside the clinic. Arch. Phys. Med. Rehabil. 2018, 99, 1913–1916. [Google Scholar] [CrossRef] [PubMed]
- Liu, S.-H.; Eaton, C.B.; Driban, J.B.; McAlindon, T.E.; Lapane, K.L. Comparison of self-report and objective measures of physical activity in US adults with osteoarthritis. Rheumatol. Int. 2016, 36, 1355–1364. [Google Scholar] [CrossRef]
- Altman, R.; Asch, E.; Bloch, D.; Bole, G.; Borenstein, D.; Brandt, K.; Christy, W.; Cooke, T.; Greenwald, R.; Hochberg, M. Development of criteria for the classification and reporting of osteoarthritis: Classification of osteoarthritis of the knee. Arthritis Rheum. Off. J. Am. Coll. Rheumatol. 1986, 29, 1039–1049. [Google Scholar] [CrossRef] [PubMed]
- Shih, M.; Hootman, J.M.; Kruger, J.; Helmick, C.G. Physical activity in men and women with arthritis: National Health Interview Survey, 2002. Am. J. Prev. Med. 2006, 30, 385–393. [Google Scholar] [CrossRef]
- Dunlop, D.D.; Song, J.; Lee, J.; Gilbert, A.L.; Semanik, P.A.; Ehrlich-Jones, L.; Pellegrini, C.A.; Pinto, D.; Ainsworth, B.; Chang, R.W. Physical activity minimum threshold predicting improved function in adults with lower-extremity symptoms. Arthritis Care Res. 2017, 69, 475–483. [Google Scholar] [CrossRef]
- Doherty, A.; Jackson, D.; Hammerla, N.; Plötz, T.; Olivier, P.; Granat, M.H.; White, T.; Van Hees, V.T.; Trenell, M.I.; Owen, C.G. Large scale population assessment of physical activity using wrist worn accelerometers: The UK biobank study. PLoS ONE 2017, 12, e0169649. [Google Scholar] [CrossRef]
- Choi, L.; Ward, S.C.; Schnelle, J.F.; Buchowski, M.S. Assessment of wear/nonwear time classification algorithms for triaxial accelerometer. Med. Sci. Sports Exerc. 2012, 44, 2009. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Matthew, C.E. Calibration of accelerometer output for adults. Med. Sci. Sports Exerc. 2005, 37, S512–S522. [Google Scholar] [CrossRef]
- Farr, J.N.; Going, S.B.; Lohman, T.G.; Rankin, L.; Kasle, S.; Cornett, M.; Cussler, E. Physical activity levels in patients with early knee osteoarthritis measured by accelerometry. Arthritis Rheum. 2008, 59, 1229–1236. [Google Scholar] [CrossRef] [Green Version]
- Stucki, G.; Sangha, O.; Stucki, S.; Michel, B.A.; Tyndall, A.; Dick, W.; Theiler, R. Comparison of the WOMAC (Western Ontario and McMaster Universities) osteoarthritis index and a self-report format of the self-administered Lequesne–Algofunctional index in patients with knee and hip osteoarthritis. Osteoarthr. Cartil. 1998, 6, 79–86. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lequesne, M. The algofunctional indices for hip and knee osteoarthritis. J. Rheumatol. 1997, 24, 779–781. [Google Scholar]
- Fuchs, R.; Klaperski, S.; Gerber, M.; Seelig, H. Messung der bewegungs-und sportaktivität mit dem BSA-fragebogen: Eine methodische zwischenbilanz. Zeitschrift Gesundheitspsychologie 2015, 23, 60–76. [Google Scholar] [CrossRef]
- Moellenbeck, B.; Horst, F.; Gosheger, G.; Theil, C.; Seeber, L.; Kalisch, T. Sedentary Behavior in Older Patients before and after Total Hip Arthroplasty: A Prospective Cohort Study. Healthcare 2020, 8, 346. [Google Scholar] [CrossRef]
- Nelson, A.E.; Allen, K.D.; Golightly, Y.M.; Goode, A.P.; Jordan, J.M. A systematic review of recommendations and guidelines for the management of osteoarthritis: The chronic osteoarthritis management initiative of the U.S. bone and joint initiative. Semin. Arthritis Rheum. 2014, 43, 701–712. [Google Scholar] [CrossRef]
- Adams, S.A.; Matthews, C.E.; Ebbeling, C.B.; Moore, C.G.; Cunningham, J.E.; Fulton, J.; Hebert, J.R. The effect of social desirability and social approval on self-reports of physical activity. Am. J. Epidemiol. 2005, 161, 389–398. [Google Scholar] [CrossRef] [PubMed]
- Bull, F.C.; Al-Ansari, S.S.; Biddle, S.; Borodulin, K.; Buman, M.P.; Cardon, G.; Carty, C.; Chaput, J.P.; Chastin, S.; Chou, R.; et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br. J. Sports Med. 2020, 54, 1451–1462. [Google Scholar] [CrossRef]
- WHO. Physical Activity Factsheets for the 28 European Union Member States of the WHO. Available online: www.euro.who.int (accessed on 27 October 2020).
- Piercy, K.L.; Troiano, R.P. Physical activity guidelines for Americans from the US Department of Health and Human Services: Cardiovascular benefits and recommendations. Circ. Cardiovasc. Qual. Outcomes 2018, 11, e005263. [Google Scholar] [CrossRef]
- Fredman, L.; Bertrand, R.M.; Martire, L.M.; Hochberg, M.; Harris, E.L. Leisure-time exercise and overall physical activity in older women caregivers and non-caregivers from the Caregiver-SOF Study. Prev. Med. 2006, 43, 226–229. [Google Scholar] [CrossRef]
- Prince, S.A.; Adamo, K.B.; Hamel, M.E.; Hardt, J.; Gorber, S.C.; Tremblay, M. A comparison of direct versus self-report measures for assessing physical activity in adults: A systematic review. Int. J. Behav. Nutr. Phys. Act. 2008, 5, 56. [Google Scholar] [CrossRef] [Green Version]
- Sabia, S.; van Hees, V.T.; Shipley, M.J.; Trenell, M.I.; Hagger-Johnson, G.; Elbaz, A.; Kivimaki, M.; Singh-Manoux, A. Association between questionnaire-and accelerometer-assessed physical activity: The role of sociodemographic factors. Am. J. Epidemiol. 2014, 179, 781–790. [Google Scholar] [CrossRef]
- Skender, S.; Ose, J.; Chang-Claude, J.; Paskow, M.; Brühmann, B.; Siegel, E.M.; Steindorf, K.; Ulrich, C.M. Accelerometry and physical activity questionnaires—a systematic review. BMC Public Health 2016, 16, 515. [Google Scholar] [CrossRef] [Green Version]
- Washburn, R.A.; Jette, A.M.; Janney, C.A. Using age-neutral physical activity questionnaires in research with the elderly. J. Aging Health 1990, 2, 341–356. [Google Scholar] [CrossRef]
- Ewald, B.; McEvoy, M.; Attia, J. Pedometer counts superior to physical activity scale for identifying health markers in older adults. Br. J. Sports Med. 2010, 44, 756–761. [Google Scholar] [CrossRef] [PubMed]
- Cust, A.E.; Smith, B.J.; Chau, J.; van der Ploeg, H.P.; Friedenreich, C.M.; Armstrong, B.K.; Bauman, A. Validity and repeatability of the EPIC physical activity questionnaire: A validation study using accelerometers as an objective measure. Int. J. Behav. Nutr. Phys. Act. 2008, 5, 33. [Google Scholar] [CrossRef] [Green Version]
- Neilson, H.K.; Robson, P.J.; Friedenreich, C.M.; Csizmadi, I. Estimating activity energy expenditure: How valid are physical activity questionnaires? Am. J. Clin. Nutr. 2008, 87, 279–291. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Van Weering, M.; Vollenbroek-Hutten, M.M.R.; Hermens, H.J. The relationship between objectively and subjectively measured activity levels in people with chronic low back pain. Clin. Rehabil. 2011, 25, 256–263. [Google Scholar] [CrossRef]
- Colley, R.C.; Butler, G.; Garriguet, D.; Prince, S.A.; Roberts, K.C. Comparison of self-reported and accelerometer-measured physical activity in Canadian adults. Health Rep. 2018, 29, 3–15. [Google Scholar] [PubMed]
- Troiano, R.P.; McClain, J.J.; Brychta, R.J.; Chen, K.Y. Evolution of accelerometer methods for physical activity research. Br. J. Sports Med. 2014, 48, 1019–1023. [Google Scholar] [CrossRef] [Green Version]
- Haskell, W.L. Physical activity by self-report: A brief history and future issues. J. Phys. Act. Health 2012, 9 (Suppl. 1), S5–S10. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Thiel, C.; Gabrys, L.; Vogt, L. Measuring Physical Activity with Wearable Accelerometers. Deutsche Zeitschrift Sportmedizin 2016, 2016, 44–48. [Google Scholar] [CrossRef]
- Skender, S.; Schrotz-King, P.; Böhm, J.; Abbenhardt, C.; Gigic, B.; Chang-Claude, J.; Siegel, E.M.; Steindorf, K.; Ulrich, C.M. Repeat physical activity measurement by accelerometry among colorectal cancer patients—Feasibility and minimal number of days of monitoring. BMC Res. Notes 2015, 8, 222. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Variable | OA Patients (n or M ± SD) | Spouses (n or M ± SD) | Difference between Groups | Couple-Specific Deviation (M ± SD) |
|---|---|---|---|---|
| Age | 71.11 ± 5.47 (range 61–81 years) | 70.82 ± 7.29 (range 58–83 years) | p = 0.869 | 2.93 ± 2.11 |
| Gender | 11 male, 17 female | 17 male, 11 female | χ2 = 2.571; p = 0.109 | - |
| BMI a | 23.03 ± 3.72 | 26.98 ± 3.95 | p = 0.964 | 3.08 ± 2.90 |
| Education b | 7 sl1, 15 sl2, 3 tl § | 11 sl1, 12 sl2, 3 tl § | χ2 = 1.203; p = 0.548 | 0.46 ± 0.58 |
| Professional status c | 24 r, 2 pt, 2 ft | 24 r, 2 pt, 2 ft | χ2 = 0; p = 1 | 0.14 ± 0.45 |
| Comorbidities d | 1.29 ± 0.76 | 0.93 ± 0.81 | p = 0.096 | 0.79 ± 0.74 |
| Pain medication e | 7 n, 11 i, 2 w, 3 ww, 5 d | - | - | - |
| Test | OA Patients | Spouses | Difference in Activity |
|---|---|---|---|
| Accelerometry (min/week) | M ± SD | t-test | |
| Sedentary Behavior | 4190.06 ± 585.85 | 4178.97 ± 657.15 | p = 0.947 |
| Light PA | 897.20 ± 209.32 | 864.31 ± 223.46 | p = 0.572 |
| MVPA | 630.72 ± 247.80 | 828.47 ± 335.43 | p = 0.015 * |
| Total PA | 1527.93 ± 415.93 | 1692.78 ± 503.33 | p = 0.187 |
| Self-report [min/week] | Mdn (IQR) | Mann–Whitney test | |
| Everyday activity index | 456.25 (226.88–785.00) | 427.50 (290.63–1080.00) | U = 371.00, Z = −0.344, p = 0.731 |
| Sport and exercise index | 60.00 (0.0–171.56) | 63.75 (0.0–180.0) | U = 382.50, Z = −0.161, p = 0.872 |
| Total activity index | 598.13 (320.88–808.75) | 603.75 (312.50–1214.38) | U = 357.5, Z = −0.565, p = 0.572 |
| Patients’ PA | Light PA/ Everyday Activity Index | MVPA/ Sport and Exercise Index | Total PA/ Total Activity Index |
|---|---|---|---|
| Sedentary behavior | ACC: r = −0.169, p = 0.196 X: r = −0.332, p = 0.042 * | ACC: r = −0.660, p < 0.001 * X: r = 0.006, p = 0.489 | ACC: r = −0.478, p = 0.005 * X: r = −0.361, p = 0.030 * |
| Light PA/ Everyday activity index | X: r = 0.410, p = 0.015 * | ACC: r = 0.653, p < 0.001 * QST: r = 0.121, p = 0.270 X: r = −0.058, p = 0.384 | ACC: r = 0.893, p < 0.001 * QST: r = 0.925, p < 0.001 * X: r = 0.315, p = 0.051 |
| MVPA/ Sport and exercise index | X: r = 0.367, p = 0.027 * | X: r = −0.053, p = 0.395 | ACC: r = 0.925, p < 0.001 * QST: r = 0.396, p < 0.018 * X: r = 0.307, p = 0.056 |
| Total PA/ Total activity index | X: r = 0.430, p = 0.011 * | X: r = −0.092, p = 0.321 | X: r = 0.338, p = 0.039 * |
| Spouses’ PA | Light PA/ Everyday activity index | MVPA/ Sport and exercise index | Total PA/ Total activity index |
| Sedentary behavior | ACC: r = −0.433, p = 0.011 * X: r = −0.490, p = 0.004 * | ACC: r = −0.670, p < 0.001 * X: r = −0.307, p = 0.056 | ACC: r = −0.638, p < 0.001 * X: r = −0.609, p = 0.001 * |
| Light PA/ Everyday activity index | X: r = 0.567, p < 0.001 * | ACC: r = 0.606, p < 0.001 * QST: r = 0.157, p = 0.213 X: r = 0.148, p = 0.227 | ACC: r = 0.884, p < 0.001 * QST: r = 0.947, p < 0.001 * X: r = 0.572, p < 0.001 |
| MVPA/ Sport and exercise index | X: r = 0.444, p = 0.009 * | X: r = 0.175, p = 0.186 | ACC: r = 0.936, p < 0.001 * QST: r = 0.381, p < 0.023 * X: r = 0.537, p = 0.002 * |
| Total PA/ Total activity index | X: r = 0.555, p < 0.001 * | X: r = −0.119, p = 0.274 | X: r = 0.601, p < 0.001 * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Moellenbeck, B.; Horst, F.; Gosheger, G.; Theil, C.; Seeber, L.; Kalisch, T. Alignment of Physical Activity in Older Couples Affected by Osteoarthritis: Investigation by Accelerometry and Questionnaire. J. Clin. Med. 2021, 10, 1544. https://doi.org/10.3390/jcm10071544
Moellenbeck B, Horst F, Gosheger G, Theil C, Seeber L, Kalisch T. Alignment of Physical Activity in Older Couples Affected by Osteoarthritis: Investigation by Accelerometry and Questionnaire. Journal of Clinical Medicine. 2021; 10(7):1544. https://doi.org/10.3390/jcm10071544
Chicago/Turabian StyleMoellenbeck, Burkhard, Frank Horst, Georg Gosheger, Christoph Theil, Leonie Seeber, and Tobias Kalisch. 2021. "Alignment of Physical Activity in Older Couples Affected by Osteoarthritis: Investigation by Accelerometry and Questionnaire" Journal of Clinical Medicine 10, no. 7: 1544. https://doi.org/10.3390/jcm10071544
APA StyleMoellenbeck, B., Horst, F., Gosheger, G., Theil, C., Seeber, L., & Kalisch, T. (2021). Alignment of Physical Activity in Older Couples Affected by Osteoarthritis: Investigation by Accelerometry and Questionnaire. Journal of Clinical Medicine, 10(7), 1544. https://doi.org/10.3390/jcm10071544






