Association of Prolonged Fluoroscopy Time with Procedural Success of Percutaneous Coronary Intervention for Stable Coronary Artery Disease with and without Chronic Total Occlusion
Abstract
1. Introduction
2. Materials and Methods
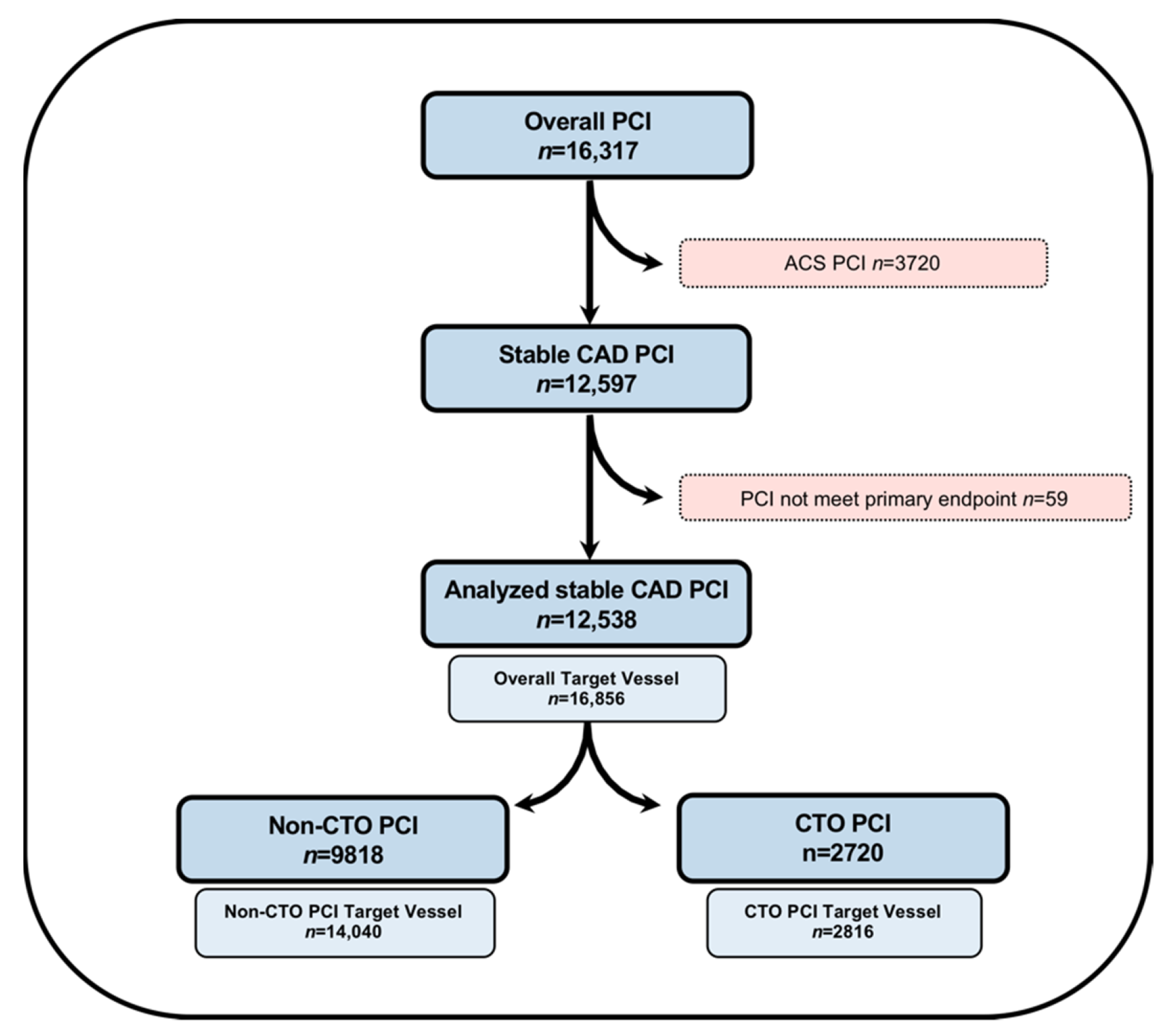
2.1. Study Population and Patient Selection
2.2. Endpoints and Definitions
2.3. Statistical Analysis
3. Results
3.1. Clinical, Angiographic and Procedural Characteristics of the Study Cohort
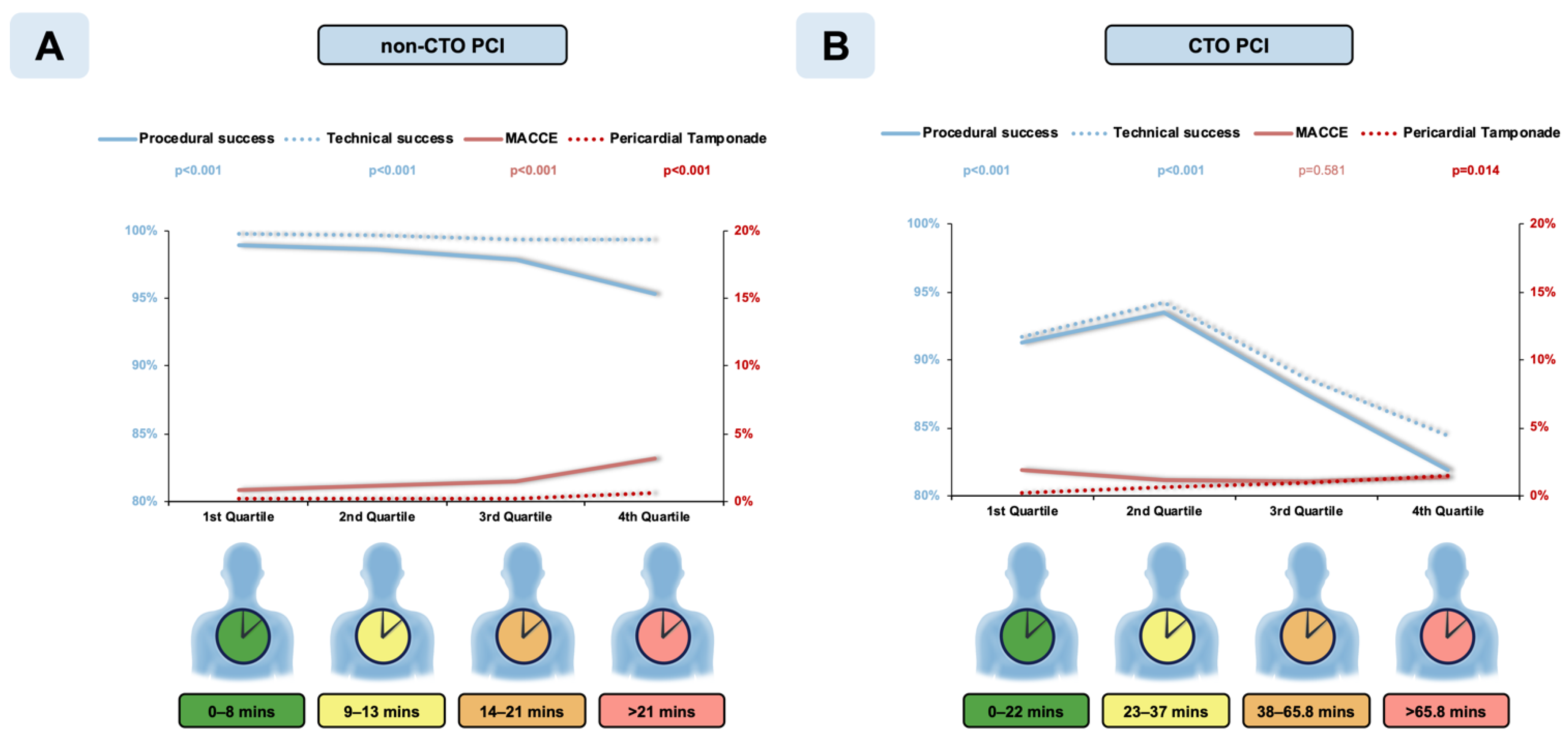
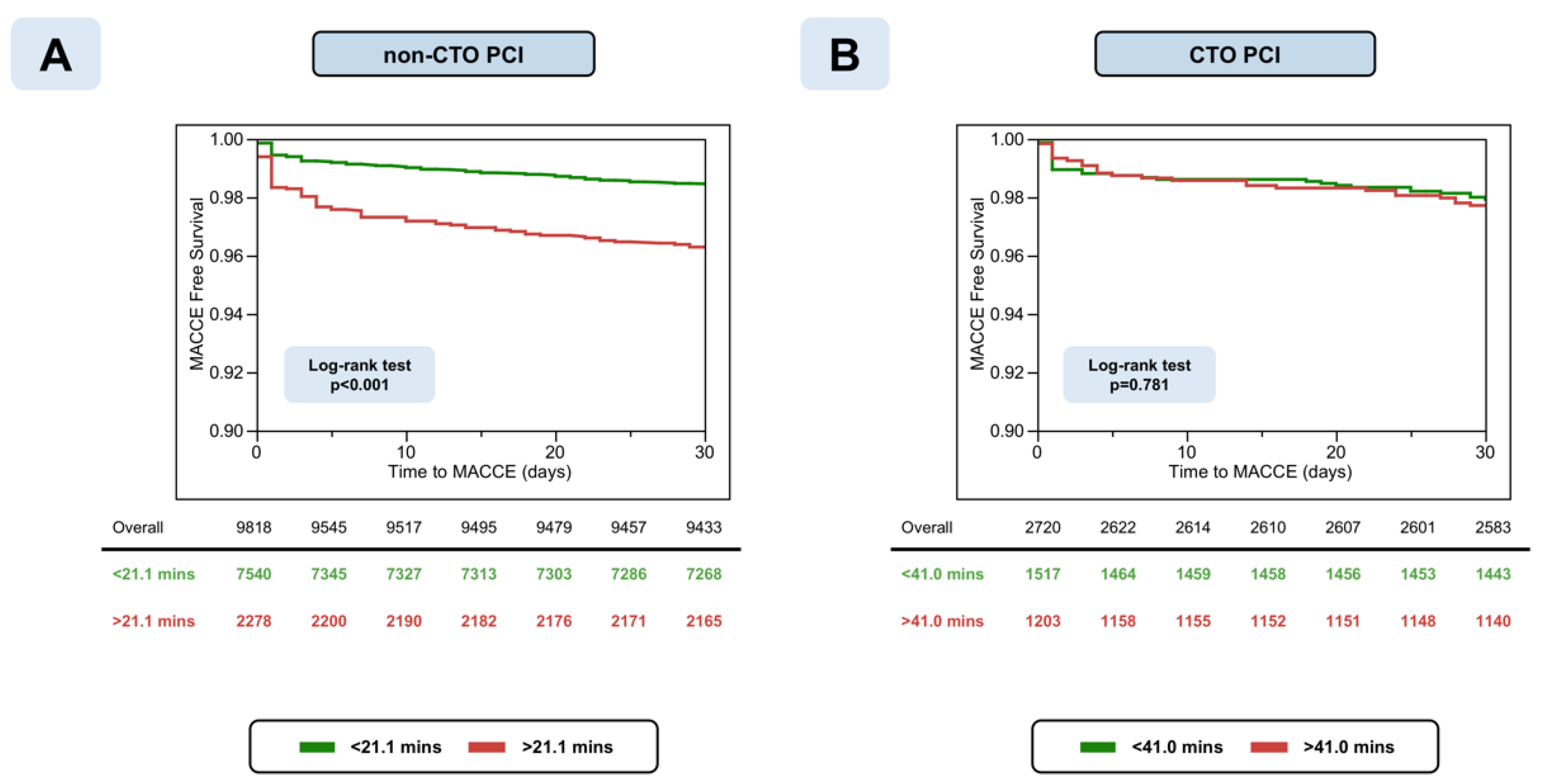
3.2. Secondary Analysis in Non-CTO PCI Subset
3.3. Secondary Analysis of CTO PCI Subset
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kirtane, A.J.; Doshi, D.; Leon, M.B.; Lasala, J.M.; Magnus Ohman, E.; O’Neill, W.W.; Shroff, A.; Cohen, M.G.; Palacios, I.F.; Beohar, N.; et al. Treatment of Higher-Risk Patients with an Indication for Revascularization: Evolution Within the Field of Contemporary Percutaneous Coronary Intervention. Circulation 2016, 134, 422–431. [Google Scholar] [CrossRef] [PubMed]
- Nikolsky, E.; Pucelikova, T.; Mehran, R.; Balter, S.; Kaufman, L.; Fahy, M.; Lansky, A.J.; Leon, M.B.; Moses, J.W.; Stone, G.W.; et al. An evaluation of fluoroscopy time and correlation with outcomes after percutaneous coronary intervention. J. Invasive Cardiol. 2007, 19, 208–213. [Google Scholar] [PubMed]
- Thygesen, K.; Alpert, J.S.; Jaffe, A.S.; Chaitman, B.R.; Bax, J.J.; Morrow, D.A.; White, H.D.; Mickley, H.; Crea, F.; Van De Werf, F.; et al. Fourth Universal Definition of Myocardial Infarction. J. Am. Coll. Cardiol. 2018, 72, 2231–2264. [Google Scholar] [CrossRef] [PubMed]
- Moussa, I.D.; Klein, L.W.; Shah, B.; Mehran, R.; Mack, M.J.; Brilakis, E.S.; Reilly, J.P.; Zoghbi, G.; Holper, E.; Stone, G.W. Consideration of a new definition of clinically relevant myocardial infarction after coronary revascularization: An expert consensus document from the society for cardiovascular angiography and interventions (SCAI). Catheter. Cardiovasc. Interv. 2013, 83, 27–36. [Google Scholar] [CrossRef] [PubMed]
- Ryan, T.J.; Faxon, D.P.; Gunnar, R.M.; Kennedy, J.W.; King, S.B.; Loop, F.D.; Peterson, K.L.; Reeves, T.J.; Williams, D.O.; Winters, W.L. Guidelines for percutaneous transluminal coronary angioplasty. A report of the American College of Cardiology/American Heart Association Task Force on Assessment of Diagnostic and Therapeutic Cardiovascular Procedures (Subcommittee on Percutaneous Transluminal Coronary Angioplasty). Circulation 1988, 78, 486–502. [Google Scholar] [PubMed]
- Galassi, A.R.; Werner, G.S.; Boukhris, M.; Azzalini, L.; Mashayekhi, K.; Carlino, M.; Avran, A.; Konstantinidis, N.V.; Grancini, L.; Bryniarski, L.; et al. Percutaneous recanalisation of chronic total occlusions: 2019 consensus document from the EuroCTO Club. EuroIntervention 2019, 15, 198–208. [Google Scholar] [CrossRef] [PubMed]
- Michael, T.T.; Karmpaliotis, D.; Brilakis, E.S.; AlOmar, M.; Abdullah, S.M.; Kirkland, B.L.; Mishoe, K.L.; Lembo, N.; Kalynych, A.; Carlson, H.; et al. Temporal trends of fluoroscopy time and contrast utilization in coronary chronic total occlusion revascularization: Insights from a multicenter united states registry. Catheter. Cardiovasc. Interv. 2015, 85, 393–399. [Google Scholar] [CrossRef] [PubMed]
- Fazel, R.; Curtis, J.; Wang, Y.; Curtis, J.; Wang, Y.; Einstein, A.J.; Smith-Bindman, R.; Tsai, T.T.; Chen, J.; Shah, N.D.; et al. Determinants of fluoroscopy time for invasive coronary angiography and percutaneous coronary intervention: Insights from the NCDR((R)). Catheter. Cardiovasc. Interv. 2013, 82, 1091–1105. [Google Scholar] [CrossRef] [PubMed]
- Cho, M.S.; Ahn, J.-M.; Lee, C.-H.; Kang, D.-Y.; Lee, J.-B.; Lee, P.H.; Kang, S.-J.; Lee, S.-W.; Kim, Y.-H.; Park, S.-W.; et al. Differential Rates and Clinical Significance of Periprocedural Myocardial Infarction After Stenting or Bypass Surgery for Multivessel Coronary Disease According to Various Definitions. JACC Cardiovasc. Interv. 2017, 10, 1498–1507. [Google Scholar] [CrossRef] [PubMed]


| Variable | Overall (n = 12,538) | Procedural Success (n = 12,000) | Procedural Failure (n = 538) | p Value |
|---|---|---|---|---|
| Age (years) * | 69.3 ± 10.4 | 69.3 ± 10.4 | 69.9 ± 10.2 | 0.402 |
| Men | 77.2% | 77.2% | 77.5% | 0.871 |
| BMI (kg/m2) * | 28.0 ± 4.6 | 28.0 ± 4.6 | 27.8 ± 4.7 | 0.342 |
| Diabetes Mellitus | 29.7% | 29.4% | 35.4% | 0.005 |
| Hypercholesterinemia | 88.5% | 88.4% | 90.8% | 0.103 |
| Hypertension | 86.8% | 86.7% | 89.0% | 0.125 |
| Smoking (current) | 14.6% | 14.5% | 15.8% | 0.413 |
| Left Ventricular Ejection Fraction ‡ | 0.069 | |||
| ● Normal | 71.9% | 72.1% | 66.6% | |
| ● Moderately reduced | 16.0% | 15.9% | 18.9% | |
| ● Reduced | 7.5% | 7.5% | 8.7% | |
| ● Low | 4.6% | 4.5% | 5.8% | |
| Family History of CAD | 41.3% | 41.5% | 37.6% | 0.099 |
| Heart Failure | 4.1% | 5.6% | 4.1% | 0.099 |
| NYHA Classification | 0.523 | |||
| ● I | 17.2% | 17.2% | 17.4% | |
| ● II | 47.7% | 47.8% | 44.4% | |
| ● III | 32.2% | 32.1% | 35.3% | |
| ● IV | 2.9% | 2.9% | 2.9% | |
| Prior MI | 29.5% | 29.3% | 34.5% | 0.015 |
| Prior CABG | 14.4% | 14.0% | 22.1% | <0.001 |
| eGFR (mL/min/1.732) * | 71.3 ± 19.5 | 71.9 ± 19.4 | 69.4 ± 20.9 | 0.038 |
| Baseline Creatinine (mg/dL) † | 1.00 (0.88, 1.20) | 1.00 (0.88, 1.20) | 1.00 (0.88, 1.22) | 0.096 |
| Variable | Overall (n = 16,856) | Procedural Success (n = 16,208) | Procedural Failure (n = 648) | p Value |
|---|---|---|---|---|
| Target vessel | 0.015 | |||
| ● RCA | 27.8% | 27.6% | 32.4% | |
| ● LAD | 35.8% | 36.1% | 29.5% | |
| ● LM | 6.5% | 6.6% | 5.3% | |
| ● CX | 28.0% | 27.8% | 31.6% | |
| ● Arterial Graft | 0.2% | 0.2% | 0.0% | |
| ● Venous Graft | 1.8% | 1.8% | 1.2% | |
| Lesion Length | <0.001 | |||
| ● <10 mm | 15.1% | 15.3% | 10.8% | |
| ● 10–20 mm | 43.8% | 44.3% | 31.7% | |
| ● >20 mm | 41.1% | 40.4% | 57.5% | |
| Calcification | <0.001 | |||
| ● None | 7.2% | 7.3% | 3.8% | |
| ● Mild (spots) | 46.0% | 46.8% | 26.2% | |
| ● Moderate | 27.2% | 27.3% | 25.2% | |
| ● Severe | 19.6% | 18.6% | 44.8% | |
| Proximal Vessel Tortuosity | 17.5% | 17.0% | 28.8% | <0.001 |
| Intralesion Angulation | < 0.001 | |||
| ● None | 11.3% | 11.3% | 10.7% | |
| ● Discrete (<45) | 47.2% | 47.7% | 34.5% | |
| ● Moderate (45–90) | 37.0% | 36.7% | 44.5% | |
| ● Severe (>90) | 4.5% | 4.3% | 10.3% | |
| CTO Target Vessel | 17.0% | 15.6% | 50.8% | <0.001 |
| Multiple Target Vessels | 46.4% | 46.5% | 44.3% | 0.265 |
| In-stent Restenosis | 12.7% | 12.8% | 10.6% | 0.117 |
| AHA/ACC Lesion Class | <0.001 | |||
| ● Type A | 4.4% | 4.5% | 0.9% | |
| ● Type B1 | 22.4% | 22.9% | 9.0% | |
| ● Type B2 | 33.1% | 33.6% | 21.4% | |
| ● Type C | 40.1% | 39.0% | 68.6% |
| Variable | Overall (n = 12,538) | Procedural Success (n = 12,000) | Procedural Failure (n = 538) | p Value |
|---|---|---|---|---|
| Femoral Access Used | 38.3% | 37.5% | 57.4% | <0.001 |
| Guide Catheter Size * | 6.2 ± 0.5 | 6.1 ± 0.5 | 6.2 ± 0.5 | <0.001 |
| Rotational atherectomy | 3.9% | 3.9% | 4.5% | 0.519 |
| CTO PCI | 21.7% | 20.1% | 58.0% | <0.001 |
| CTO Crossing Strategies Used ‡ | 0.082 | |||
| Antegrade only | 70.9% | 71.4% | 66.7% | |
| Retrograde | 29.1% | 28.6% | 33.3% | |
| Number of DES Used † | 1 (1, 2) | 1 (1, 2) | 0 (0, 1) | <0.001 |
| Overall Stent Length † | 24 (16, 38) | 24 (16, 38) | 28 (18, 52) | 0.078 |
| Technical Success | 97.3% | 100.0% | 35.9% | <0.001 |
| Length of Hospital Stay (days) * | 2 (2, 2) | 2 (2, 2) | 2 (2, 4) | <0.001 |
| Procedural Time (min) † | 42 (25, 71) | 41 (24, 68) | 82 (46, 134) | <0.001 |
| Fluoroscopy Time (min) † | 16.0 (9.0, 28.0) | 15.0 (9.0, 26.4) | 34.0 (17.0, 65.0) | <0.001 |
| Contrast Volume (mL) † | 190 (150, 260) | 180 (150, 250) | 250 (170, 380) | <0.001 |
| Dose Area Product (cGy*cm2) † | 5364 (3146, 9000) | 5299 (3124, 8790) | 8554 (4333, 15,422) | <0.001 |
| Variable | Procedural Failure (4th UD MI) | ||
|---|---|---|---|
| OR | CI 95% | p Value | |
| CTO PCI (vs. non-CTO PCI) | 3.67 | 2.99–4.50 | <0.001 |
| Fluoroscopy time (mins) | 1.02 | 1.02–1.02 | <0.001 |
| CTO PCI and Fluoroscopy time (mins) | - | - | <0.001 |
| Variable | Nonadjusted | Adjusted | ||||
|---|---|---|---|---|---|---|
| OR | CI 95% | p Value | OR | CI 95% | p Value | |
| Technical failure | 3.34 | 2.05–5.44 | <0.001 | 2.10 | 1.19–3.71 | 0.010 |
| Major complications * | 2.99 | 2.21–4.04 | <0.001 | 2.96 | 1.93–4.56 | <0.001 |
| Perforation | 4.94 | 2.98–8.31 | <0.001 | 4.34 | 2.53–7.60 | <0.001 |
| Bleeding | 2.77 | 1.90–4.03 | <0.001 | 2.45 | 1.45–4.15 | <0.001 |
| 30-days MACCE †§ | 2.41 | 1.82–3.19 | <0.001 | 2.08 | 1.41–3.05 | <0.001 |
| Variable | Nonadjusted | Adjusted | ||||
|---|---|---|---|---|---|---|
| OR | CI 95% | p Value | OR | CI 95% | p Value | |
| Technical failure | 2.16 | 1.70–2.79 | <0.001 | 2.25 | 1.65–3.10 | <0.001 |
| Major complications * | 1.51 | 0.90–2.59 | 0.120 | 1.53 | 0.89–2.65 | 0.124 |
| Perforation | 3.40 | 2.00–6.03 | <0.001 | 3.07 | 1.76–5.58 | <0.001 |
| Bleeding | 3.94 | 2.30–7.09 | <0.001 | 4.05 | 2.25–7.61 | <0.001 |
| 30-days MACCE †§ | 1.10 | 0.65–1.84 | 0.719 | 1.14 | 0.67–1.91 | 0.626 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tajti, P.; Ayoub, M.; Nuehrenberg, T.; Ferenc, M.; Behnes, M.; Buettner, H.J.; Neumann, F.-J.; Mashayekhi, K. Association of Prolonged Fluoroscopy Time with Procedural Success of Percutaneous Coronary Intervention for Stable Coronary Artery Disease with and without Chronic Total Occlusion. J. Clin. Med. 2021, 10, 1486. https://doi.org/10.3390/jcm10071486
Tajti P, Ayoub M, Nuehrenberg T, Ferenc M, Behnes M, Buettner HJ, Neumann F-J, Mashayekhi K. Association of Prolonged Fluoroscopy Time with Procedural Success of Percutaneous Coronary Intervention for Stable Coronary Artery Disease with and without Chronic Total Occlusion. Journal of Clinical Medicine. 2021; 10(7):1486. https://doi.org/10.3390/jcm10071486
Chicago/Turabian StyleTajti, Peter, Mohamed Ayoub, Thomas Nuehrenberg, Miroslaw Ferenc, Michael Behnes, Heinz Joachim Buettner, Franz-Josef Neumann, and Kambis Mashayekhi. 2021. "Association of Prolonged Fluoroscopy Time with Procedural Success of Percutaneous Coronary Intervention for Stable Coronary Artery Disease with and without Chronic Total Occlusion" Journal of Clinical Medicine 10, no. 7: 1486. https://doi.org/10.3390/jcm10071486
APA StyleTajti, P., Ayoub, M., Nuehrenberg, T., Ferenc, M., Behnes, M., Buettner, H. J., Neumann, F.-J., & Mashayekhi, K. (2021). Association of Prolonged Fluoroscopy Time with Procedural Success of Percutaneous Coronary Intervention for Stable Coronary Artery Disease with and without Chronic Total Occlusion. Journal of Clinical Medicine, 10(7), 1486. https://doi.org/10.3390/jcm10071486








