A Retrospective Case Series of Thiamine Deficiency in Non-Alcoholic Hospitalized Veterans: An Important Cause of Delirium and Falling?
Abstract
1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Whitfield, K.C.; Bourassa, M.W.; Adamolekun, B.; Bergeron, G.; Bettendorff, L.; Brown, K.H.; Cox, L.; Fattal-Valevski, A.; Fischer, P.R.; Frank, E.L.; et al. Thiamine Deficiency Disorders: Diagnosis, Prevalence, and a Roadmap for Global Control Programs. Ann. N. Y. Acad. Sci. 2018, 1430, 3–43. [Google Scholar] [CrossRef] [PubMed]
- Attaluri, P.; Castillo, A.; Edriss, H.; Nugent, K. Thiamine Deficiency: An Important Consideration in Critically Ill Patients. Am. J. Med. Sci. 2018, 356, 382–390. [Google Scholar] [CrossRef]
- Lonsdale, D. Thiamin. In Advances in Food and Nutrition Research, 1st ed.; Michael Eskin, N.A., Ed.; Academic Press Inc.: Cambridge, MA, USA, 2018; Volume 83, pp. 1–56. [Google Scholar] [CrossRef]
- Galvin, R.; Bråthen, G.; Ivashynka, A.; Hillbom, M.; Tanasescu, R.; Leone, M.A. EFNS Guidelines for Diagnosis, Therapy and Prevention of Wernicke Encephalopathy. Eur. J. Neurol. 2010, 17, 1408–1418. [Google Scholar] [CrossRef]
- Lee, D.C.; Chu, J.; Satz, W.; Silbergleit, R. Low Plasma Thiamine Levels in Elder Patients Admitted through the Emergency Department. Acad. Emerg. Med. 2000, 7, 1156–1159. [Google Scholar] [CrossRef]
- Lemoine, A.; Le Devehat, C.; Codaccioni, J.L. Vitamin B1, B2, B6, and C Status in Hospital Inpatients. Am. J. Clin. Nutr. 1980, 33, 2595–2600. [Google Scholar] [CrossRef]
- O’Keeffe, S.T.; Tormey, W.P.; Glasgow, R.; Lavan, J.N. Thiamine Deficiency in Hospitalized Elderly Patients. Gerontology 1994, 40, 18–24. [Google Scholar] [CrossRef]
- Pepersack, T.; Garbusinski, J.; Robberecht, J.; Beyer, I.; Willems, D.; Fuss, M. Clinical Relevance of Thiamine Status amongst Hospitalized Elderly Patients. Gerontology 1999, 45, 96–101. [Google Scholar] [CrossRef]
- Donnino, M.W.; Carney, E.; Cocchi, M.N.; Barbash, I.; Chase, M.; Joyce, N.; Chou, P.P.; Ngo, L. Thiamine Deficiency in Critically Ill Patients with Sepsis. J. Crit. Care 2010, 25, 576–581. [Google Scholar] [CrossRef]
- Nath, A.; Tran, T.; Shope, T.R.; Koch, T.R. Prevalence of Clinical Thiamine Deficiency in Individuals with Medically Complicated Obesity. Nutr. Res. 2017, 37, 29–36. [Google Scholar] [CrossRef] [PubMed]
- Hung, S.C.; Hung, S.H.; Tarng, D.C.; Yang, W.C.; Chen, T.W.; Huang, T.P. Thiamine Deficiency and Unexplained Encephalopathy in Hemodialysis and Peritoneal Dialysis Patients. Am. J. Kidney Dis. 2001, 38, 941–947. [Google Scholar] [CrossRef] [PubMed]
- Bleggi-Torres, L.F.; De Medeiros, B.C.; Werner, B.; Zanis Neto, J.; Loddo, G.; Pasquini, R.; De Medeiros, C.R. Neuropathological Findings after Bone Marrow Transplantation: An Autopsy Study of 180 Cases. Bone Marrow Transplant. 2000, 25, 301–307. [Google Scholar] [CrossRef] [PubMed]
- Isenberg-Grzeda, E.; Alici, Y.; Hatzoglou, V.; Nelson, C.; Breitbart, W. Nonalcoholic Thiamine-Related Encephalopathy (Wernicke-Korsakoff Syndrome) Among Inpatients with Cancer: A Series of 18 Cases. Psychosomatics 2016, 57, 71–81. [Google Scholar] [CrossRef] [PubMed]
- Levavi, H.; Park, D.; Tannenbaum, J.; Steinberg, A. Retrospective Analysis of Thiamine Deficiency in Allogeneic Stem Cell Transplant Patients. Ann. Hematol. 2019, 98, 1499–1500. [Google Scholar] [CrossRef]
- Abou-Hashem, R.M.; Maamoun, M.M.A.; Hamza, S.A.; Fahmy, H.M.; Mortagy, A.K. Thiamine Level in Hospitalized Elderly Egyptian Patients with Congestive Heart Failure and Left Ventricular Systolic Dysfunction. J. Am. Geriatr. Soc. 2009, 57, 2165–2166. [Google Scholar] [CrossRef] [PubMed]
- Brady, J.A.; Rock, C.L.; Horneffer, M.R. Thiamin Status, Diuretic Medications, and the Management of Congestive Heart Failure. J. Am. Diet. Assoc. 1995, 95, 541–544. [Google Scholar] [CrossRef]
- Hanninen, S.A.; Darling, P.B.; Sole, M.J.; Barr, A.; Keith, M.E. The Prevalence of Thiamin Deficiency in Hospitalized Patients with Congestive Heart Failure. J. Am. Coll. Cardiol. 2006, 47, 354–361. [Google Scholar] [CrossRef]
- Jain, A.; Mehta, R.; Al-Ani, M.; Hill, J.A.; Winchester, D.E. Determining the Role of Thiamine Deficiency in Systolic Heart Failure: A Meta-Analysis and Systematic Review. J. Card. Fail. 2015, 21, 1000–1007. [Google Scholar] [CrossRef] [PubMed]
- Gold, M.; Chen, M.; Johnson, K. Plasma and Red Blood Cell Thiamine Deficiency in Patients with Dementia of the Alzheimer’s Type. Arch. Neurol. 1995, 52, 1081–1086. [Google Scholar] [CrossRef]
- Vognar, L.; Stoukides, J. The Role of Low Plasma Thiamin Levels in Cognitively Impaired Elderly Patients Presenting with Acute Behavioral Disturbances. J. Am. Geriatr. Soc. 2009, 57, 2166–2168. [Google Scholar] [CrossRef]
- Lin, S.; Leppla, I.E.; Yan, H.; Probert, J.M.; Randhawa, P.A.; Leoutsakos, J.M.S.; Probasco, J.C.; Neufeld, K.J. Prevalence and Improvement of Caine-Positive Wernicke-Korsakoff Syndrome in Psychiatric Inpatient Admissions. Psychosomatics 2020, 61, 31–38. [Google Scholar] [CrossRef]
- Ehsanian, R.; Anderson, S.; Schneider, B.; Kennedy, D.; Mansourian, V. Prevalence of Low Plasma Vitamin B1 in the Stroke Population Admitted to Acute Inpatient Rehabilitation. Nutrients 2020, 12, 1034. [Google Scholar] [CrossRef]
- Moskowitz, A.; Graver, A.; Giberson, T.; Berg, K.; Liu, X.; Uber, A.; Gautam, S.; Donnino, M.W. The Relationship between Lactate and Thiamine Levels in Patients with Diabetic Ketoacidosis. J. Crit. Care 2014, 29, 182-e5. [Google Scholar] [CrossRef]
- Shah, H.N.; Bal, B.S.; Finelli, F.C.; Koch, T.R. Constipation in Patients with Thiamine Deficiency after Roux-En-Y Gastric Bypass Surgery. Digestion 2013, 88, 119–124. [Google Scholar] [CrossRef]
- Zulman, D.M.; Chee, C.P.; Wagner, T.H.; Yoon, J.; Cohen, D.M.; Holmes, T.H.; Ritchie, C.; Asch, S.M. Multimorbidity and Healthcare Utilisation among High-Cost Patients in the US Veterans Affairs Health Care System. BMJ Open 2015, 5, 7771. [Google Scholar] [CrossRef]
- de Luis, D.; Lopez Guzman, A. Nutritional Status of Adult Patients Admitted to Internal Medicine Departments in Public Hospitals in Castilla y Leon, Spain—A Multi-Center Study. Eur. J. Intern. Med. 2006, 17, 556–560. [Google Scholar] [CrossRef] [PubMed]
- Kaiser, M.J.; Bauer, J.M.; Rämsch, C.; Uter, W.; Guigoz, Y.; Cederholm, T.; Thomas, D.R.; Anthony, P.S.; Charlton, K.E.; Maggio, M.; et al. Frequency of Malnutrition in Older Adults: A Multinational Perspective Using the Mini Nutritional Assessment. J. Am. Geriatr. Soc. 2010, 58, 1734–1738. [Google Scholar] [CrossRef] [PubMed]
- Win, A.Z.; Ceresa, C.; Arnold, K.; Allison, T.A. High Prevalence of Malnutrition among Elderly Veterans in Home Based Primary Care. J. Nutr. Heal. Aging 2017, 21, 610–613. [Google Scholar] [CrossRef] [PubMed]
- Dizdar, O.S.; Yıldız, A.; Gul, C.B.; Gunal, A.I.; Ersoy, A.; Gundogan, K. The Effect of Hemodialysis, Peritoneal Dialysis and Renal Transplantation on Nutritional Status and Serum Micronutrient Levels in Patients with End-Stage Renal Disease; Multicenter, 6-Month Period, Longitudinal Study. J. Trace Elem. Med. Biol. 2020, 60, 126498. [Google Scholar] [CrossRef] [PubMed]
- Evans, W.J.; Morley, J.E.; Argilés, J.; Bales, C.; Baracos, V.; Guttridge, D.; Jatoi, A.; Kalantar-Zadeh, K.; Lochs, H.; Mantovani, G.; et al. Cachexia: A New Definition. Clin. Nutr. 2008, 27, 793–799. [Google Scholar] [CrossRef] [PubMed]
- Jensen, G.L.; Mirtallo, J.; Compher, C.; Dhaliwal, R.; Forbes, A.; Figueredo Grijalba, R.; Hardy, G.; Kondrup, J.; Labadarios, D.; Nyulasi, I.; et al. Adult Starvation and Disease-Related Malnutrition: A Proposal for Etiology-Based Diagnosis in the Clinical Practice Setting from the International Consensus Guideline Committee. J. Parenter. Enter. Nutr. 2010, 34, 156–159. [Google Scholar] [CrossRef]
- Keller, U. Nutritional Laboratory Markers in Malnutrition. J. Clin. Med. 2019, 8, 775. [Google Scholar] [CrossRef]
- Gabay, C.; Kushner, I. Acute-Phase Proteins and Other Systemic Responses to Inflammation. N. Engl. J. Med. 1999, 340, 448–454. [Google Scholar] [CrossRef]
- Pahwa, R.; Jialal, I. Chronic Inflammation—StatPearls—NCBI Bookshelf; StatPearls Publishing: Treasure Island, FL, USA, 2019; p. 1. [Google Scholar]
- White, J.V.; Guenter, P.; Jensen, G.; Malone, A.; Schofield, M. Consensus Statement: Academy of Nutrition and Dietetics and American Society for Parenteral and Enteral Nutrition: Characteristics Recommended for the Identification and Documentation of Adult Malnutrition (Undernutrition). J. Parenter. Enter. Nutr. 2012, 36, 275–283. [Google Scholar] [CrossRef]
- Caine, D.; Halliday, G.M.; Kril, J.J.; Harper, C.G. Operational Criteria for the Classification of Chronic Alcoholics: Identification of Wernicke’s Encephalopathy. J. Neurol. Neurosurg. Psychiatry 1997, 62, 51–60. [Google Scholar] [CrossRef]
- Jamieson, C.P.; Obeid, O.A.; Powell-Tuck, J. The Thiamin, Riboflavin and Pyridoxine Status of Patients on Emergency Admission to Hospital. Clin. Nutr. 1999, 18, 87–91. [Google Scholar] [CrossRef]
- Chamorro, A.J.; Rosón-Hernández, B.; Medina-García, J.A.; Muga-Bustamante, R.; Fernández-Solá, J.; Martín-González, M.C.; Seco-Hernández, E.; Novo-Veleiro, I.; Suárez-Cuervo, C.; Mateos-Díaz, A.M.; et al. Differences Between Alcoholic and Nonalcoholic Patients With Wernicke Encephalopathy: A Multicenter Observational Study. Mayo Clin. Proc. 2017, 92, 899–907. [Google Scholar] [CrossRef] [PubMed]
- Liampas, I.; Siokas, V.; Mentis, A.A.; Aloizou, A.; Dastamani, M.; Tsouris, Z.; Aslanidou, P.; Brotis, A.; Dardiotis, E. Serum Homocysteine, Pyridoxine, Folate, and Vitamin B12 Levels in Migraine: Systematic Review and Meta-Analysis. Headache J. Head Face Pain 2020, 60, 1508–1534. [Google Scholar] [CrossRef] [PubMed]
- Soh, Y.; Won, C.W. Association between Frailty and Vitamin B12 in the Older Korean Population. Medicine 2020, 99, e22327. [Google Scholar] [CrossRef]
- van den Berg, K.S.; Arts, M.H.L.; Collard, R.M.; van den Brink, R.H.S.; Comijs, H.C.; Marijnissen, R.M.; Oude Voshaar, R.C. Vitamin D Deficiency and Course of Frailty in a Depressed Older Population. Aging Ment. Health 2020, 24, 49–55. [Google Scholar] [CrossRef] [PubMed]
- Zhou, J.; Huang, P.; Liu, P.; Hao, Q.; Chen, S.; Dong, B.; Wang, J. Association of Vitamin D Deficiency and Frailty: A Systematic Review and Meta-Analysis. Maturitas 2016, 94, 70–76. [Google Scholar] [CrossRef] [PubMed]
- Sanford, A.M.; Flaherty, J.H. Do Nutrients Play a Role in Delirium? Curr. Opin. Clin. Nutr. Metab. Care 2014, 1, 45–50. [Google Scholar] [CrossRef] [PubMed]
- Yang, G.T.; Zhao, H.Y.; Kong, Y.; Sun, N.N.; Dong, A.Q. Correlation between Serum Vitamin B12 Level and Peripheral Neuropathy in Atrophic Gastritis. World J. Gastroenterol. 2018, 24, 1343–1352. [Google Scholar] [CrossRef] [PubMed]
| Risk Factor | Number (%) |
|---|---|
| Insufficient intake | 28 (78%) |
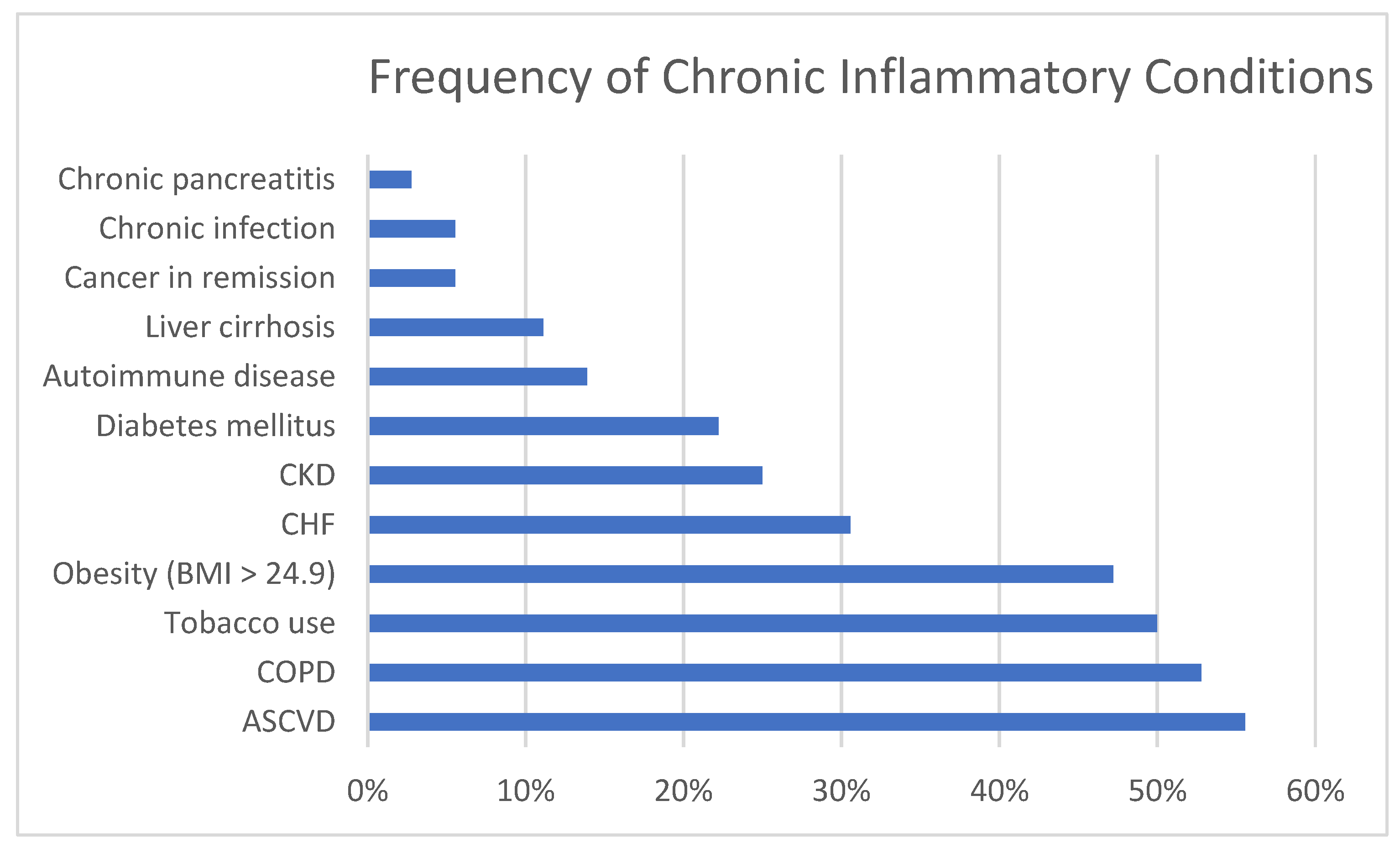
| Inflammatory stress | 36 (100%) |
| 0 Chronic inflammatory condition | 0 |
| 1 Chronic inflammatory condition | 1 (2.7%) |
| 2 Chronic inflammatory conditions | 10 (27.8%) |
| 3 Chronic inflammatory conditions | 10 (27.8%) |
| 4 Chronic inflammatory conditions | 9 (25%) |
| 5 Chronic inflammatory conditions | 6 (16.7%) |
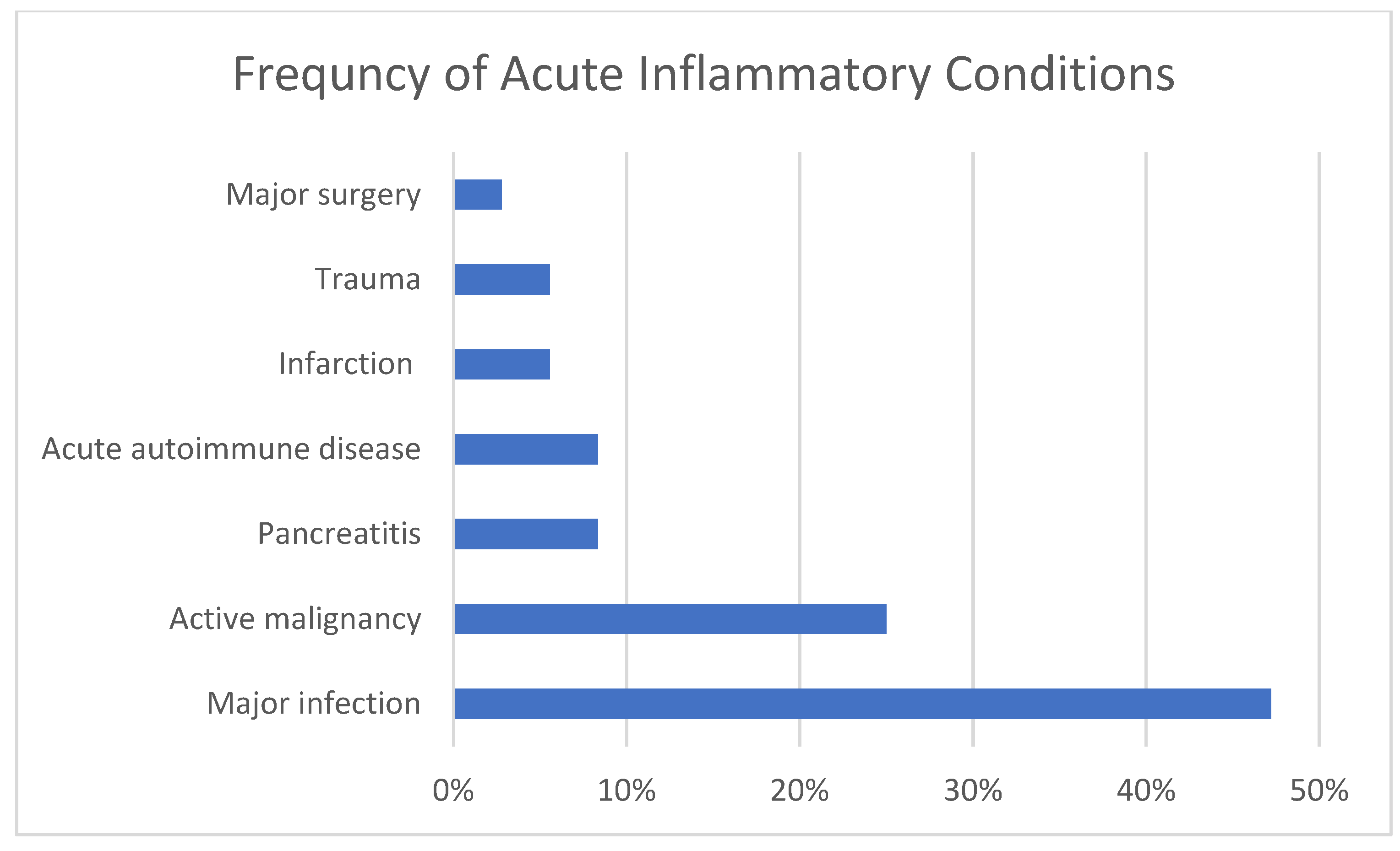
| 0 Acute inflammatory condition | 6 (16.7%) |
| 1 Acute inflammatory condition | 23 (63.9%) |
| 2 Acute inflammatory conditions | 7 (19.4%) |
| Increased losses | 19 (52.8%) |
| Sign | Number of Cases with Data | Number (%) |
|---|---|---|
| BMI less than 18.5 | 36 | 5 (14%) |
| Non-volitional weight loss ≥ 5% of baseline 1 | 34 | 27 (79%) |
| Albumin less than 3.5 g/dL | 36 | 26 (72%) |
| Prealbumin less than 18 mg/dL | 11 | 11 (100%) |
| Reduced energy intake 2 | 28 | 25 (89%) |
| Reduced functional status 3 | 33 | 27 (82%) |
| Physical findings of muscle or fat loss 4 | 19 | 18 (95%) |
| Symptom | Number (%) |
|---|---|
| Weakness or falling | 27 (75%) |
| Neuropsychiatric symptoms | 26 (72%) |
| Gastrointestinal symptoms | 19 (53%) |
| Ataxia | 15 (42%) |
| Polyneuritis | 5 (14%) |
| Peripheral or pulmonary edema | 5 (14%) |
| Ophthalmoplegia | 4 (11%) |
| Non-ischemic congestive heart failure | 3 (8%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mates, E.; Alluri, D.; Artis, T.; Riddle, M.S. A Retrospective Case Series of Thiamine Deficiency in Non-Alcoholic Hospitalized Veterans: An Important Cause of Delirium and Falling? J. Clin. Med. 2021, 10, 1449. https://doi.org/10.3390/jcm10071449
Mates E, Alluri D, Artis T, Riddle MS. A Retrospective Case Series of Thiamine Deficiency in Non-Alcoholic Hospitalized Veterans: An Important Cause of Delirium and Falling? Journal of Clinical Medicine. 2021; 10(7):1449. https://doi.org/10.3390/jcm10071449
Chicago/Turabian StyleMates, Elisabeth, Deepti Alluri, Tailer Artis, and Mark S. Riddle. 2021. "A Retrospective Case Series of Thiamine Deficiency in Non-Alcoholic Hospitalized Veterans: An Important Cause of Delirium and Falling?" Journal of Clinical Medicine 10, no. 7: 1449. https://doi.org/10.3390/jcm10071449
APA StyleMates, E., Alluri, D., Artis, T., & Riddle, M. S. (2021). A Retrospective Case Series of Thiamine Deficiency in Non-Alcoholic Hospitalized Veterans: An Important Cause of Delirium and Falling? Journal of Clinical Medicine, 10(7), 1449. https://doi.org/10.3390/jcm10071449







