Posterior Shoulder Dislocation with Engaging Reverse Hill–Sachs Lesion: A Retrospective Study of Ten Patients Treated with Arthroscopy or Open Reduction and Stabilization
Abstract
1. Introduction
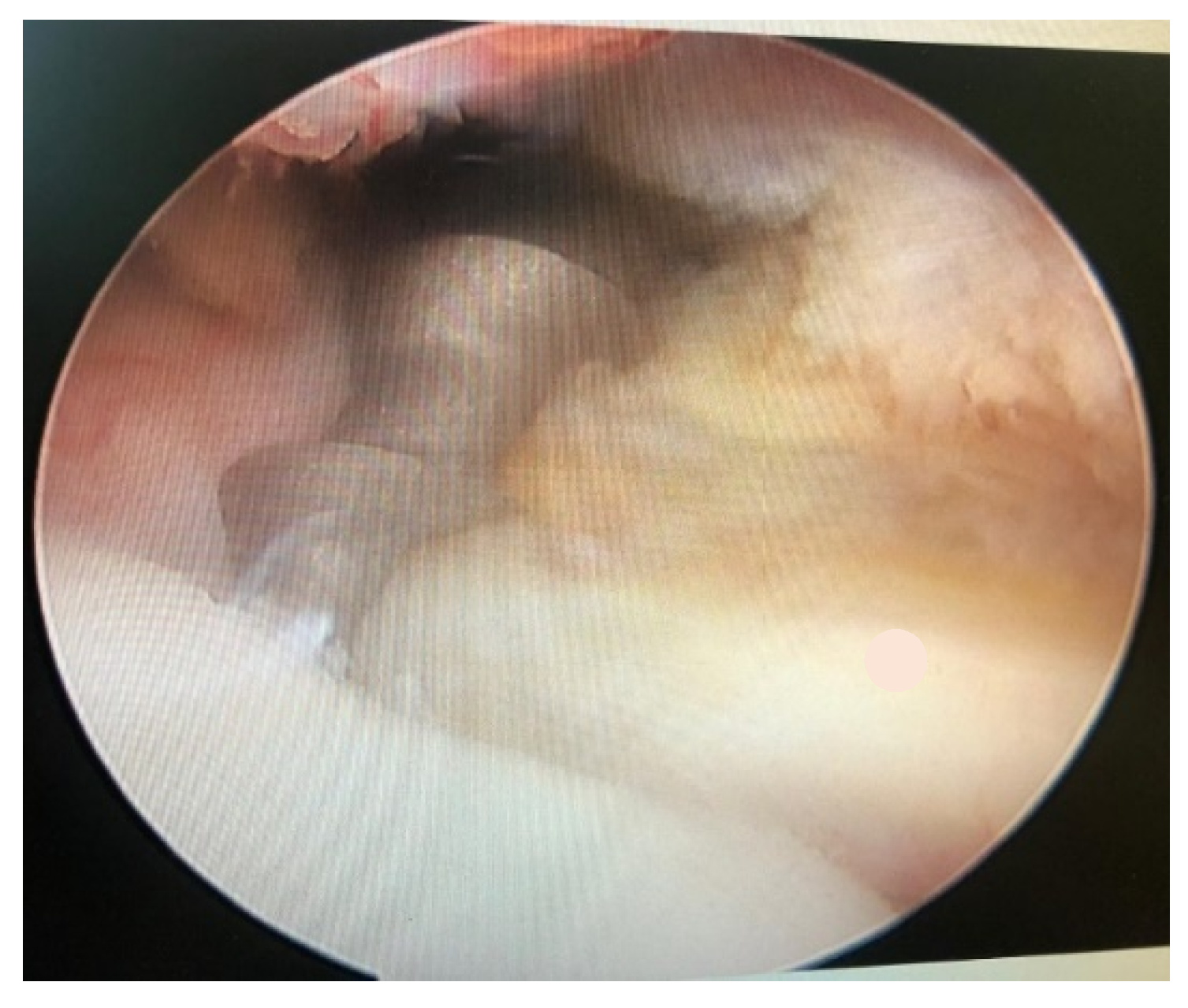
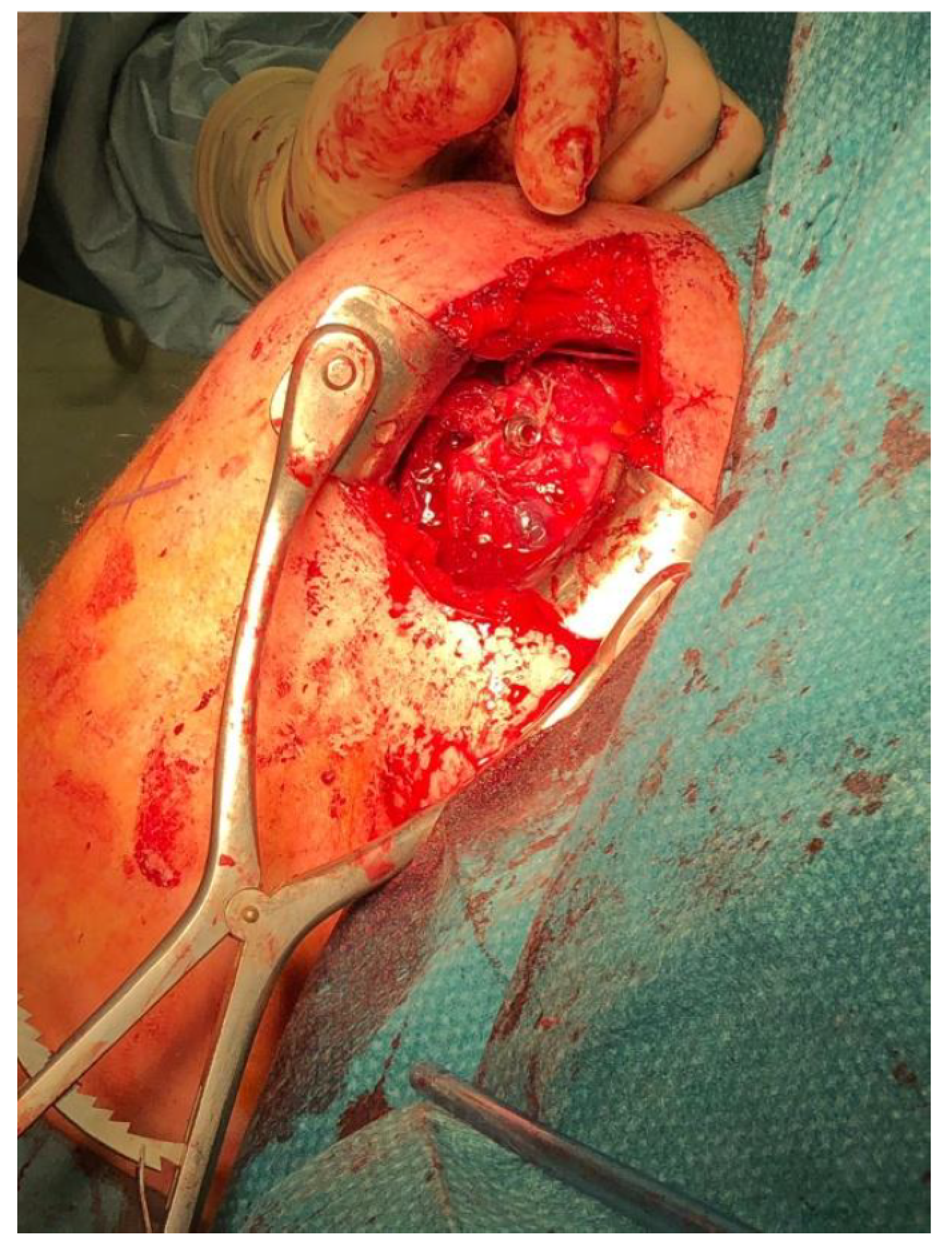
2. Materials and Methods
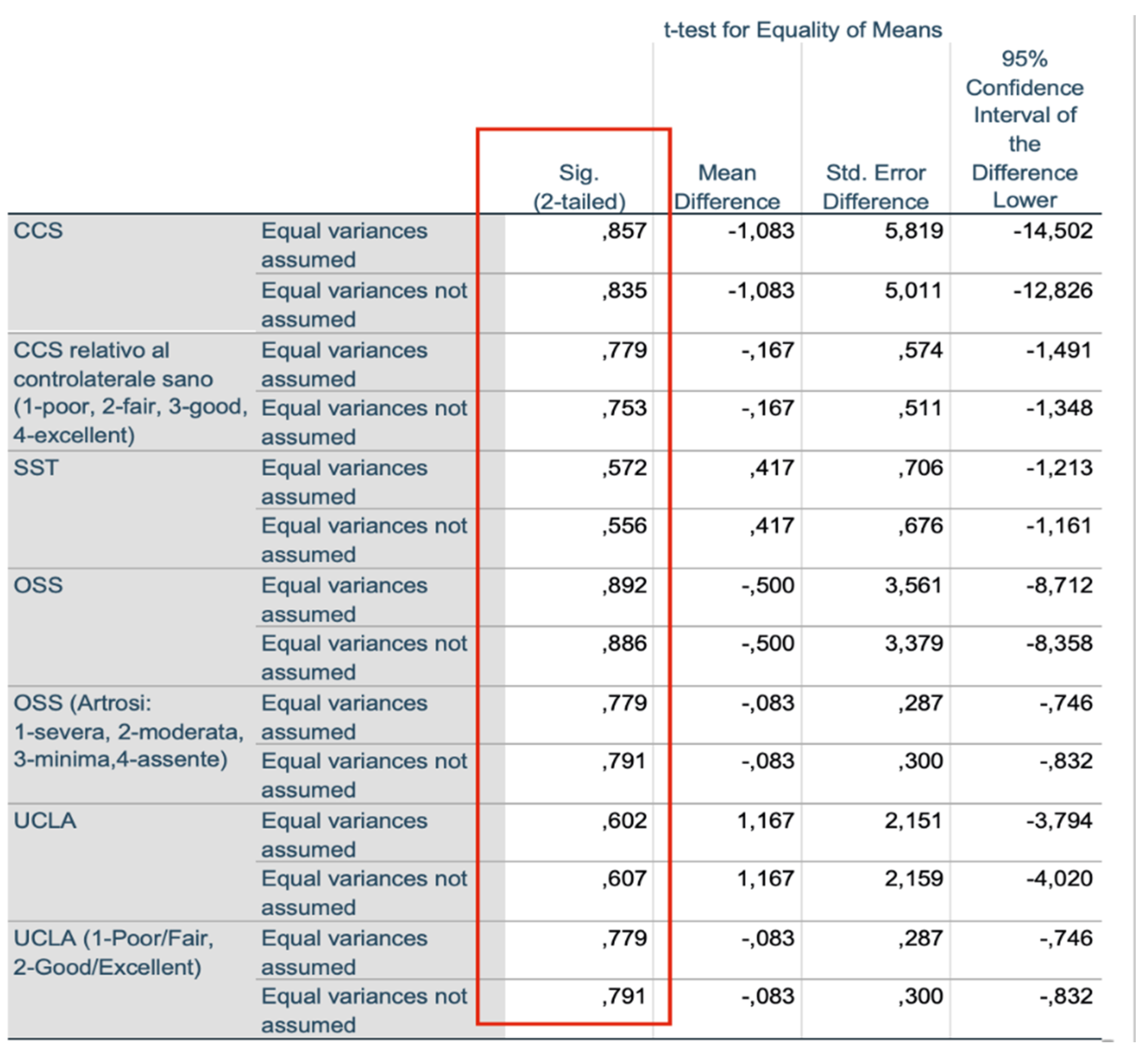
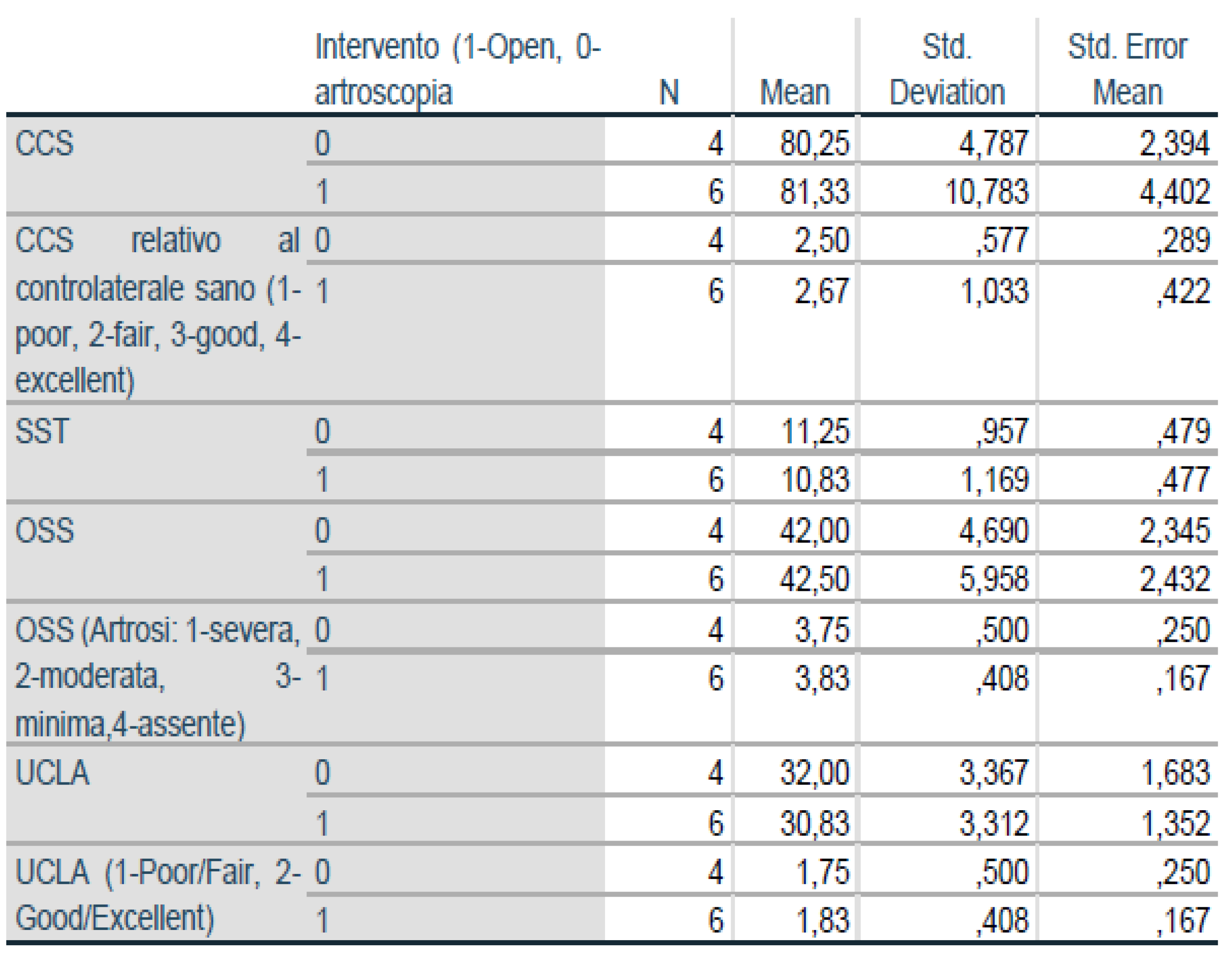
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Rodia, F.; Ventura, A.; Touloupakis, G.; Theodorakis, E.; Ceretti, M. Missed posterior shoulder dislocation and McLaughlin lesion after an electrocution accident. Chin. J. Traumatol. 2012, 15, 376–378. [Google Scholar] [PubMed]
- Constant, C.R.; Murley, A.H. A clinical method of functional assessment of the shoulder. Clin. Orthop. Relat. Res. 1987, 214, 160–164. [Google Scholar] [CrossRef]
- Antosh, I.J.; Tokish, J.M.; Owens, B.D. Posterior Shoulder Instability: Current Surgical Management. Orthop. Surg. 2016. [Google Scholar] [CrossRef] [PubMed]
- Dhir, J.; Willis, M.; Watson, L.; Somerville, L.; Sadi, J. Evidence-Based Review of Clinical Diagnostic Tests and Predictive Clinical Tests That Evaluate Response to Conservative Rehabilitation for Posterior Glenohumeral Instability: A Systematic Review. Sports Health 2018, 10, 141–145. [Google Scholar] [CrossRef] [PubMed]
- Gimber, L.H.; Taljanovic, M.S.; Rockov, Z.A.; Krupinski, E.A.; Chadaz, T.S.; Rogers, L.F. The Veil of Obscuration: Additional Radiographic Sign of Posterior Shoulder Dislocation. Acta Med. Acad. 2018, 47, 165–175. [Google Scholar] [CrossRef]
- Guehring, M.; Lambert, S.; Stoeckle, U.; Ziegler, P. Posterior shoulder dislocation with associated reverse Hill-Sachs lesion: Treatment options and functional outcome after a 5-year follow up. BMC Musculoskelet. Disord. 2017, 18, 442. [Google Scholar] [CrossRef] [PubMed]
- Byram, G.W., III; Field, A.C.; Field, L.D. Arthroscopic Management of Locked Posterior Shoulder Dislocations. Arthrosc. Tech. 2018, 7, e945–e949. [Google Scholar] [CrossRef] [PubMed]
- Cruz-Ferreira, E.; Abadied, P.; Godenèchee, A.; Mansatf, P.; Clavertg, P.; Flurind, P. The French Arthroscopy Society, Posterior shoulder instability: Prospective non-randomised comparison of operative and non-operative treatment in 51 patients. Orthop. Traumatol. Surg. Res. 2017, 103, S185–S188. [Google Scholar] [CrossRef] [PubMed]
- Basal, O.; Dincer, R.; Turk, B. Locked posterior dislocation of the shoulder. EFORT Open Rev. 2018, 3, 15–23. [Google Scholar] [CrossRef] [PubMed]
- Paparoidamis, G.; Iliopoulos, E.; Narvani, A.A.; Levy, O.; Tsiridis, E.; Polyzois, I. Posterior shoulder fracture-dislocation: A systematic review of the literature and current aspects of management. Chin. J. Traumatol. 2021, 24, 18–24. [Google Scholar] [CrossRef] [PubMed]
- Schliemann, B.; Muder, D.; Geßmann, J.; Schildhauer, T.A.; Seybold, D. Locked posterior shoulder dislocation: Treatment options and clinical outcomes. Arch. Orthop. Trauma Surg. 2011, 131, 1127–1134. [Google Scholar] [CrossRef] [PubMed]
- Xu, W.; Huang, L.-X.; Guo, J.J.; Jiang, D.-H.; Zhang, Y.; Yang, H.-L. Neglected posterior dislocation of the shoulder: A systematic literature review. J. Orthop. Transl. 2015, 3, 89–94. [Google Scholar] [CrossRef] [PubMed]
- Rouleau, D.M.; Hebert-Davies, J.; Robinson, C.M. Acute traumatic posterior shoulder dislocation. J. Am. Acad. Orthop. Surg. 2014, 22, 145–152. [Google Scholar] [CrossRef] [PubMed]
- Babhulkar, A.; Unnithan, V.; Patil, P. A treatment algorithm for locked posterior dislocation of shoulder. J. Arthrosc. Jt. Surg. 2018, 5, 90–98. [Google Scholar] [CrossRef]
- DeLong, J.M.; Jiang, K.; Bradley, J.P. Posterior instability of the shoulder: A systematic review and meta-analysis of clinical outcomes. Am. J. Sports Med. 2015, 43, 1805–1817. [Google Scholar] [CrossRef] [PubMed]
- Spencer, E.E., Jr.; Brems, J.J. A simple technique for management of locked posterior shoulder dislocations: Report of two cases. J. Shoulder Elbow. Surg. 2005, 14, 650–652. [Google Scholar] [CrossRef] [PubMed]
- Frank, R.M.; Romeo, A.A.; Provencher, M.T. Posterior glenohumeral instability: Evidence-based treatment. J. Am. Acad. Ortho Surg. 2017, 25, 610–623. [Google Scholar] [CrossRef] [PubMed]
- Lavender, C.D.; Hanzlik, S.R.; Pearson, S.E.; Caldwell, P.E. Arthroscopic reverse remplissage for posterior instability. Arthrosc. Tech. 2016, 5, e43–e47. [Google Scholar] [CrossRef] [PubMed]
- Castagna, A.; Conti, M.; Garofalo, R. Soft tissue-based techniques for treatment of posterior shoulder instability. Obere Extrem. 2017, 12, 82–89. [Google Scholar] [CrossRef] [PubMed]



| Patient (First Group) | Constant Scale | SST (Simple Shoulder Test) Scale | Oxford Scale | UCLA (University of California—Los Angeles |
|---|---|---|---|---|
| F.G. (53) | 63 | 11 | 32 | 25 |
| C.M. (44) | 75 | 9 | 41 | 30 |
| F.P. (64) | 92 | 12 | 48 | 34 |
| D.M. (39) | 82 | 10 | 41 | 31 |
| B.D. (46) | 89 | 12 | 46 | 34 |
| F.P. (62) | 87 | 11 | 47 | 31 |
| Patient (Second Group) | Constant Scale | SST (Simple Shoulder Test) Scale | Oxford Scale | UCLA (University of California—Los Angeles |
|---|---|---|---|---|
| I.M. (58) | 75 | 10 | 35 | 27 |
| C.U. (39) | 82 | 12 | 45 | 34 |
| R.M. (37) | 86 | 11 | 44 | 33 |
| R.S. (38) | 78 | 12 | 44 | 34 |
| Our Study (2021) | Cruz-Ferreira and AL. (2017) | Clavert and AL. (2017) | N. Aydin and AL. (2019) | O. Basal and AL. (2018) | |
|---|---|---|---|---|---|
| Constant Scale (Average Value) | 80.75 | 78 | 82 | 79.25 | 82.5 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ippolito, G.; Zitiello, M.; De Marinis, G.; D’Angelo, F.; Surace, M.F.; Ronga, M.; Sepe, V.; Garro, L.; Faoro, L.; Ferraro, S. Posterior Shoulder Dislocation with Engaging Reverse Hill–Sachs Lesion: A Retrospective Study of Ten Patients Treated with Arthroscopy or Open Reduction and Stabilization. J. Clin. Med. 2021, 10, 1410. https://doi.org/10.3390/jcm10071410
Ippolito G, Zitiello M, De Marinis G, D’Angelo F, Surace MF, Ronga M, Sepe V, Garro L, Faoro L, Ferraro S. Posterior Shoulder Dislocation with Engaging Reverse Hill–Sachs Lesion: A Retrospective Study of Ten Patients Treated with Arthroscopy or Open Reduction and Stabilization. Journal of Clinical Medicine. 2021; 10(7):1410. https://doi.org/10.3390/jcm10071410
Chicago/Turabian StyleIppolito, Giorgio, Michele Zitiello, Giancarlo De Marinis, Fabio D’Angelo, Michele F. Surace, Mario Ronga, Vincenzo Sepe, Luca Garro, Luca Faoro, and Sergio Ferraro. 2021. "Posterior Shoulder Dislocation with Engaging Reverse Hill–Sachs Lesion: A Retrospective Study of Ten Patients Treated with Arthroscopy or Open Reduction and Stabilization" Journal of Clinical Medicine 10, no. 7: 1410. https://doi.org/10.3390/jcm10071410
APA StyleIppolito, G., Zitiello, M., De Marinis, G., D’Angelo, F., Surace, M. F., Ronga, M., Sepe, V., Garro, L., Faoro, L., & Ferraro, S. (2021). Posterior Shoulder Dislocation with Engaging Reverse Hill–Sachs Lesion: A Retrospective Study of Ten Patients Treated with Arthroscopy or Open Reduction and Stabilization. Journal of Clinical Medicine, 10(7), 1410. https://doi.org/10.3390/jcm10071410






