Preoperative Cognitive Impairment as a Predictor of Postoperative Outcomes in Elderly Patients Undergoing Spinal Surgery for Degenerative Spinal Disease
Abstract
1. Introduction
2. Materials and Methods
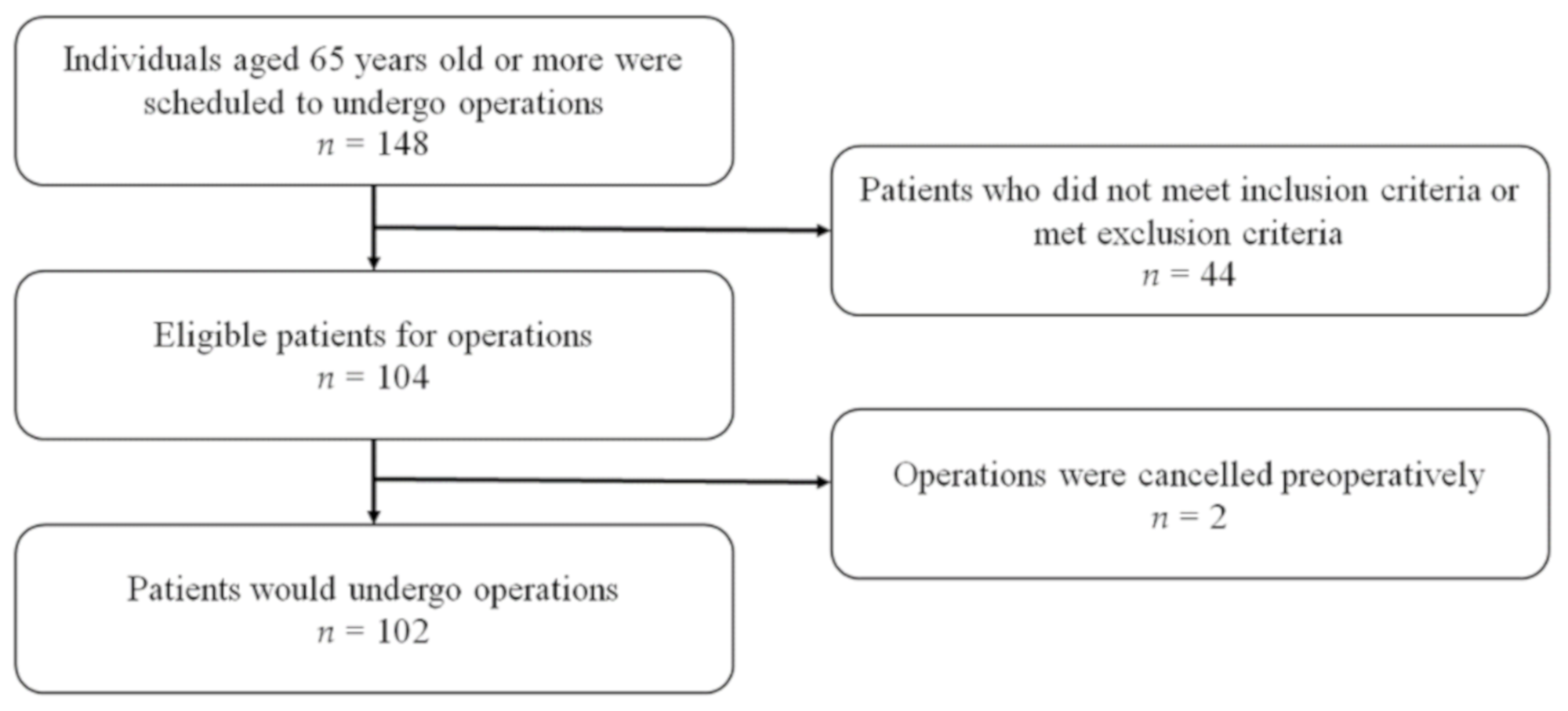
2.1. Patient Enrollment
2.2. Perioperative Patient Assessment
2.3. Statistical Analysis
3. Results
3.1. Patient Data
3.2. Outcome Data
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Gajdos, C.; Kile, D.; Hawn, M.T.; Finlayson, E.; Henderson, W.G.; Robinson, T.N. The significance of preoperative impaired sensorium on surgical outcomes in nonemergent general surgical operations. JAMA Surg. 2015, 150, 30–36. [Google Scholar] [CrossRef]
- Kim, S.; Brooks, A.K.; Groban, L. Preoperative assessment of the older surgical patient: Honing in on geriatric syndromes. Clin. Interv. Aging 2015, 10, 13–27. [Google Scholar] [PubMed]
- Fehlings, M.G.; Tetreault, L.; Nater, A.; Choma, T.; Harrop, J.; Mroz, T.; Santaguida, C.; Smith, J.S. The aging of the global population: The changing epidemiology of disease and spinal disorders. Neurosurgery 2015, 77 (Suppl. 4), S1–S5. [Google Scholar] [CrossRef]
- Lee, C.-H.; Chung, C.K.; Kim, C.H.; Kwon, J.-W. Health care burden of spinal diseases in the republic of korea: Analysis of a nationwide database from 2012 through 2016. Neurospine 2018, 15, 66–76. [Google Scholar] [CrossRef] [PubMed]
- Tan, J.Y.-W.; Kaliya-Perumal, A.-K.; Oh, J.Y.-L. Is spinal surgery safe for elderly patients aged 80 and above? Predictors of mortality and morbidity in an asian population. Neurospine 2019, 16, 764–769. [Google Scholar] [CrossRef] [PubMed]
- Takami, T. Spine surgeons are facing the great challenge of contributing to the realization of a society of health and longevity. Neurospine 2019, 16, 770–771. [Google Scholar] [CrossRef]
- Umekawa, M.; Takai, K.; Taniguchi, M. Complications of spine surgery in elderly japanese patients: Implications for future of world population aging. Neurospine 2019, 16, 780–788. [Google Scholar] [CrossRef]
- Lee, Y.S.; Kim, Y.B.; Lee, S.H.; Park, Y.S.; Park, S.W. The prevalence of undiagnosed presurgical cognitive impairment and its postsurgical clinical impact in older patients undergoing lumbar spine surgery. J. Korean Neurosurg. Soc. 2016, 59, 287–291. [Google Scholar] [CrossRef] [PubMed]
- Wilson, C.A.; Roffey, D.M.; Chow, D.; Alkherayf, F.; Wai, E.K. A systematic review of preoperative predictors for postoperative clinical outcomes following lumbar discectomy. Spine J. 2016, 16, 1413–1422. [Google Scholar] [CrossRef]
- Voorhies, R.M.; Jiang, X.; Thomas, N. Predicting outcome in the surgical treatment of lumbar radiculopathy using the pain drawing score, mcgill short form pain questionnaire, and risk factors including psychosocial issues and axial joint pain. Spine J. 2007, 7, 516–524. [Google Scholar] [CrossRef]
- Shin, M.H.; Lee, Y.M.; Park, J.M.; Kang, C.J.; Lee, B.D.; Moon, E.; Chung, Y.I. A combination of the korean version of the mini-mental state examination and korean dementia screening questionnaire is a good screening tool for dementia in the elderly. Psychiatry Investig. 2011, 8, 348–353. [Google Scholar] [CrossRef]
- Folstein, M.F.; Folstein, S.E.; McHugh, P.R. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J. Psychiatr. Res. 1975, 12, 189–198. [Google Scholar] [CrossRef]
- Tombaugh, T.N.; McIntyre, N.J. The mini-mental state examination: A comprehensive review. J. Am. Geriatr. Soc. 1992, 40, 922–935. [Google Scholar] [CrossRef]
- O’Connor, D.W.; Pollitt, P.A.; Hyde, J.B.; Fellows, J.L.; Miller, N.D.; Brook, C.P.; Reiss, B.B. The reliability and validity of the mini-mental state in a british community survey. J. Psychiatr. Res. 1989, 23, 87–96. [Google Scholar] [CrossRef]
- Beck, A.T.; Steer, R.A.; Carbin, M.G. Psychometric properties of the beck depression inventory: Twenty-five years of evaluation. Clin. Psychol. Rev. 1988, 8, 77–100. [Google Scholar] [CrossRef]
- Duthie, A.; Chew, D.; Soiza, R.L. Non-psychiatric comorbidity associated with alzheimer’s disease. QJM 2011, 104, 913–920. [Google Scholar] [CrossRef] [PubMed]
- Bynum, J.P.; Rabins, P.V.; Weller, W.; Niefeld, M.; Anderson, G.F.; Wu, A.W. The relationship between a dementia diagnosis, chronic illness, medicare expenditures, and hospital use. J. Am. Geriatr. Soc. 2004, 52, 187–194. [Google Scholar] [CrossRef]
- Phelan, E.A.; Borson, S.; Grothaus, L.; Balch, S.; Larson, E.B. Association of incident dementia with hospitalizations. JAMA 2012, 307, 165–172. [Google Scholar] [CrossRef]
- Robinson, T.N.; Wu, D.S.; Pointer, L.F.; Dunn, C.L.; Moss, M. Preoperative cognitive dysfunction is related to adverse postoperative outcomes in the elderly. J. Am. Coll. Surg. 2012, 215, 12–17, discussions 17–18. [Google Scholar] [CrossRef] [PubMed]
- Gray, S.L.; Mahoney, J.E.; Blough, D.K. Medication adherence in elderly patients receiving home health services following hospital discharge. Ann. Pharmacother. 2001, 35, 539–545. [Google Scholar] [CrossRef] [PubMed]
- Preyde, M.; Chapman, T. Psychosocial profile of elderly patients discharged from a community hospital. Soc. Work Health Care 2007, 45, 77–95. [Google Scholar] [CrossRef]
- Adogwa, O.; Elsamadicy, A.A.; Sergesketter, A.; Vuong, V.D.; Moreno, J.; Cheng, J.; Karikari, I.O.; Bagley, C.A. Independent association between preoperative cognitive status and discharge location after surgery: A strategy to reduce resource use after surgery for deformity. World Neurosurg. 2018, 110, e67–e72. [Google Scholar] [CrossRef] [PubMed]
- Nazir, A.; LaMantia, M.; Chodosh, J.; Khan, B.; Campbell, N.; Hui, S.; Boustani, M. Interaction between cognitive impairment and discharge destination and its effect on rehospitalization. J. Am. Geriatr. Soc. 2013, 61, 1958–1963. [Google Scholar] [CrossRef] [PubMed]
- Di Capua, J.; Somani, S.; Kim, J.S.; Lee, N.J.; Kothari, P.; Phan, K.; Lugo-Fagundo, N.; Cho, S.K. Predictors for patient discharge destination after elective anterior cervical discectomy and fusion. Spine 2017, 42, 1538–1544. [Google Scholar] [CrossRef] [PubMed]
- Viramontes, O.; Luan Erfe, B.M.; Erfe, J.M.; Brovman, E.Y.; Boehme, J.; Bader, A.M.; Urman, R.D. Cognitive impairment and postoperative outcomes in patients undergoing primary total hip arthroplasty: A systematic review. J. Clin. Anesth. 2019, 56, 65–76. [Google Scholar] [CrossRef]
- Kanaan, S.F.; Waitman, L.R.; Yeh, H.W.; Arnold, P.M.; Burton, D.C.; Sharma, N.K. Structural equation model analysis of the length-of-hospital stay after lumbar spine surgery. Spine J. 2015, 15, 612–621. [Google Scholar] [CrossRef]
- Walid, M.S.; Robinson, E.C.; Robinson, J.S., Jr. Higher comorbidity rates in unemployed patients may significantly impact the cost of spine surgery. J. Clin. Neurosci. 2011, 18, 640–644. [Google Scholar] [CrossRef] [PubMed]
- Deyo, R.A.; Mirza, S.K.; Martin, B.I.; Kreuter, W.; Goodman, D.C.; Jarvik, J.G. Trends, major medical complications, and charges associated with surgery for lumbar spinal stenosis in older adults. JAMA 2010, 303, 1259–1265. [Google Scholar] [CrossRef]
- Siemionow, K.; Pelton, M.A.; Hoskins, J.A.; Singh, K. Predictive factors of hospital stay in patients undergoing minimally invasive transforaminal lumbar interbody fusion and instrumentation. Spine 2012, 37, 2046–2054. [Google Scholar] [CrossRef]
- Mayo, B.C.; Haws, B.E.; Bohl, D.D.; Louie, P.K.; Hijji, F.Y.; Narain, A.S.; Massel, D.H.; Khechen, B.; Singh, K. Postoperative fever evaluation following lumbar fusion procedures. Neurospine 2018, 15, 154–162. [Google Scholar] [CrossRef]
- Hauck, K.; Zhao, X. How dangerous is a day in hospital? A model of adverse events and length of stay for medical inpatients. Med. Care 2011, 49, 1068–1075. [Google Scholar] [CrossRef]
- Neatherlin, J.S.; Brillhart, B.; Henry, J.J. Factors determining length of hospitalization for patients having laminectomy surgery. J. Neurosci. Nurs. 1988, 20, 39–41. [Google Scholar] [CrossRef]
- Kudo, D.; Miyakoshi, N.; Hongo, M.; Kasukawa, Y.; Ishikawa, Y.; Mizutani, T.; Shimada, Y. Relationship between preoperative serum rapid turnover proteins and early-stage surgical wound infection after spine surgery. Eur. Spine J. 2017, 26, 3156–3161. [Google Scholar] [CrossRef] [PubMed]
- Leu, S.; Kamenova, M.; Mehrkens, A.; Mariani, L.; Scharen, S.; Soleman, J. Preoperative and postoperative factors and laboratory values predicting outcome in patients undergoing lumbar fusion surgery. World Neurosurg. 2016, 92, 323–338. [Google Scholar] [CrossRef] [PubMed]
- Lakomkin, N.; Goz, V.; Cheng, J.S.; Brodke, D.S.; Spiker, W.R. The utility of preoperative laboratories in predicting postoperative complications following posterolateral lumbar fusion. Spine J. 2018, 18, 993–997. [Google Scholar] [CrossRef] [PubMed]
- Wobith, M.; Acikgoz, A.; Grosser, K.; Weimann, A. Preoperative cognitive function in very old patients: Influence on the complication rate and length of hospitalization. Chir. Z. Geb. Oper. Medizen 2019, 90, 930–935. [Google Scholar]
- Pinheiro, M.B.; Ferreira, M.L.; Refshauge, K.; Maher, C.G.; Ordonana, J.R.; Andrade, T.B.; Tsathas, A.; Ferreira, P.H. Symptoms of depression as a prognostic factor for low back pain: A systematic review. Spine J. 2016, 16, 105–116. [Google Scholar] [CrossRef]
- Menger, R.P.; Savardekar, A.R.; Farokhi, F.; Sin, A. A cost-effectiveness analysis of the integration of robotic spine technology in spine surgery. Neurospine 2018, 15, 216–224. [Google Scholar] [CrossRef]
- Zygourakis, C.C.; Liu, C.Y.; Wakam, G.; Moriates, C.; Boscardin, C.; Ames, C.P.; Mummaneni, P.V.; Ratliff, J.; Dudley, R.A.; Gonzales, R. Geographic and hospital variation in cost of lumbar laminectomy and lumbar fusion for degenerative conditions. Neurosurgery 2017, 81, 331–340. [Google Scholar] [CrossRef]
- Lad, S.P.; Babu, R.; Baker, A.A.; Ugiliweneza, B.; Kong, M.; Bagley, C.A.; Gottfried, O.N.; Isaacs, R.E.; Patil, C.G.; Boakye, M. Complications, reoperation rates, and health-care cost following surgical treatment of lumbar spondylolisthesis. J. Bone Joint Surg. Am. 2013, 95, e162. [Google Scholar] [CrossRef]
- McCarthy, I.M.; Hostin, R.A.; Ames, C.P.; Kim, H.J.; Smith, J.S.; Boachie-Adjei, O.; Schwab, F.J.; Klineberg, E.O.; Shaffrey, C.I.; Gupta, M.C.; et al. Total hospital costs of surgical treatment for adult spinal deformity: An extended follow-up study. Spine J. 2014, 14, 2326–2333. [Google Scholar] [CrossRef] [PubMed]
- Udeh, B.L.; Costandi, S.; Dalton, J.E.; Ghosh, R.; Yousef, H.; Mekhail, N. The 2-year cost-effectiveness of 3 options to treat lumbar spinal stenosis patients. Pain Pract. 2015, 15, 107–116. [Google Scholar] [CrossRef] [PubMed]
| Characteristic | 0 < MMSE < 20 | 21 ≤ MMSE ≤ 26 | MMSE ≥ 27 | p-Value |
|---|---|---|---|---|
| Demographic data | ||||
| Number of patients | 5 | 43 | 54 | - |
| Age (years) | 73.6 ± 3.3 | 72.3 ± 4.7 | 70.9 ± 4.7 | 0.323 |
| Sex; male, n (%) | 0 | 13 | 21 | 0.083 |
| Graduate | 1.20 ± 2.68 | 6.40 ± 4.22 | 9.83 ± 4.07 | 0.424 |
| Medical history | ||||
| Height (cm) | 152.6 ± 2.8 | 156.1 ± 8.1 | 159.4 ± 8.6 | 0.083 |
| Weight (kg) | 53.6 ± 12.0 | 60.2 ± 7.5 | 62.2 ± 9.4 | 0.208 |
| BMI (kg/m2) | 22.9 ± 4.4 | 24.8 ± 2.8 | 24.4 ± 2.8 | 0.332 |
| Number of medications | 5.8 ± 2.8 | 5.5 ± 3.3 | 4.8 ± 3.1 | 0.866 |
| HTN | 4 (80%) | 28 (65.1%) | 35 (64.8%) | 0.787 |
| DM | 0 (0%) | 12 (27.9%) | 11 (20.4%) | 0.315 |
| Cardiovascular disease | 1 (20.0%) | 9 (20.9%) | 13 (24.1%) | 0.925 |
| Cerebrovascular disease | 0 (0%) | 6 (14.0%) | 2 (3.7%) | 0.140 |
| Parkinson’s disease | 1 (20.0%) | 4 (9.3%) | 8 (14.8%) | 0.637 |
| NP related disease | 1 (20.0%) | 3 (7.0%) | 9 (16.7%) | 0.321 |
| BDI score | 9.40 ± 4.83 | 14.58 ± 8.06 | 14.32 ± 8.68 | 0.329 |
| Surgical method | ||||
| Spinal fusion, n | 2 | 29 | 34 | 0.489 |
| Decompression, n | 3 | 14 | 20 | |
| Laboratory findings | ||||
| Hemoglobin | 13.2 ± 1.7 | 13.3 ± 1.3 | 13.8 ± 1.4 | 0.931 |
| WBC | 6.77 k ± 0.71 k | 7.28 k ± 1.64 k | 6.84 k ± 1.80 k | 0.111 |
| PLT | 212.6 k ± 33.2 k | 233.3 k ± 50.3 k | 233.7 k ± 64.8 k | 0.091 |
| BUN | 17.0 ± 2.9 | 17.1 ± 6.2 | 16.7 ± 4.1 | 0.064 |
| Creatinine | 0.65 ± 0.11 | 0.78 ± 0.22 | 0.78 ± 0.19 | 0.160 |
| Albumin | 3.9 ± 0.3 | 4.1 ± 0.3 | 4.2 ± 0.35 | 0.764 |
| 0 < MMSE < 20 | 21 ≤ MMSE ≤ 26 | MMSE ≥ 27 | p-Value | |
|---|---|---|---|---|
| Number of patients | 5 | 43 | 54 | |
| Length of stay | 10.6 ± 4.9 | 11.2 ± 5.8 | 9.4 ± 5.4 | 0.488 |
| Admission to ICU after surgery, n (%) | 1 (20.0%) | 7 (16.3%) | 5 (9.3%) | 0.520 |
| Discharged to home, n (%) | 3 (60%) | 39 (91%) | 52 (96.3%) | 0.014 |
| Total medical costs ($) | 7483.2 ± 2529.2 | 8644.9 ± 3446.8 | 7319 ± 3403.4 | 0.944 |
| Mean medical cost per day ($) | 765.3 ± 287.5 | 830.7 ± 271.6 | 814.4 ± 260.3 | 0.837 |
| EBL (mL) | 540 ± 454 | 609 ± 521 | 563 ± 641 | 0.762 |
| OT (minutes) | 186.2 ± 25.0 | 197.3 ± 67.6 | 192.3 ± 97.9 | 0.937 |
| Re-admissions, n (%) | 2 (40.0%) | 11 (25.6%) | 14 (25.9%) | 0.796 |
| Revision, n (%) | 0 (0%) | 7 (16.3%) | 4 (7.4%) | 0.273 |
| Overall complications, n (%) | 2 (40.0%) | 16 (37.2%) | 14 (25.9%) | 0.450 |
| Cardiopulmonary, n (%) | 2 (40.0%) | 1 (2.3%) | 2 (3.7%) | 0.037 |
| Stroke, n (%) | 0 (0%) | 0 (0%) | 1 (1.0%) | 0.527 |
| Wound infection, n (%) | 0 (0%) | 1 (1.3%) | 2 (3.7%) | 0.794 |
| Postoperative pain, n (%) | 0 (0%) | 2 (4.7%) | 1 (1.9%) | 0.628 |
| ASD, n (%) | 0 (0%) | 2 (4.7%) | 4 (7.4%) | 0.624 |
| Postoperative delirium, n (%) | 0 (0%) | 10 (23.3%) | 5 (9.3%) | 0.098 |
| Variables | Univariate Analysis | Multivariate Analysis | ||||||
|---|---|---|---|---|---|---|---|---|
| β-Coefficients | 95.0% CI | p-Value | β-Coefficients | 95.0% CI | p-Value | |||
| Lower Bound | Upper Bound | Lower Bound | Upper Bound | |||||
| Age | −0.049 | −0.292 | 0.176 | 0.623 | ||||
| EBL | 0.312 | 0.001 | 0.005 | 0.001 | 0.046 | −0.002 | 0.003 | 0.716 |
| OT | 0.321 | 0.009 | 0.034 | 0.001 | 0.244 | 0.000 | 0.032 | 0.049 |
| WBC | −0.136 | −0.001 | −0.000 | 0.174 | −0.229 | −0.001 | 0.000 | 0.022 |
| Hb | −0.147 | −10.411 | 0.200 | 0.139 | −0.031 | −0.912 | 0.657 | 0.748 |
| PLT | 0.241 | 0.005 | 0.042 | 0.015 | 0.250 | 0.005 | 0.043 | 0.013 |
| MMSE | −0.169 | −0.737 | 0.055 | 0.090 | −0.196 | −0.763 | −0.032 | 0.033 |
| BDI | 0.240 | 0.030 | 0.277 | 0.015 | 0.190 | 0.005 | 0.238 | 0.041 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, H.C.; An, S.B.; Jeon, H.; Kim, T.W.; Oh, J.K.; Shin, D.A.; Yi, S.; Kim, K.N.; Lee, P.H.; Kang, S.Y.; et al. Preoperative Cognitive Impairment as a Predictor of Postoperative Outcomes in Elderly Patients Undergoing Spinal Surgery for Degenerative Spinal Disease. J. Clin. Med. 2021, 10, 1385. https://doi.org/10.3390/jcm10071385
Kim HC, An SB, Jeon H, Kim TW, Oh JK, Shin DA, Yi S, Kim KN, Lee PH, Kang SY, et al. Preoperative Cognitive Impairment as a Predictor of Postoperative Outcomes in Elderly Patients Undergoing Spinal Surgery for Degenerative Spinal Disease. Journal of Clinical Medicine. 2021; 10(7):1385. https://doi.org/10.3390/jcm10071385
Chicago/Turabian StyleKim, Hyung Cheol, Seong Bae An, Hyeongseok Jeon, Tae Woo Kim, Jae Keun Oh, Dong Ah Shin, Seong Yi, Keung Nyun Kim, Phil Hyu Lee, Suk Yun Kang, and et al. 2021. "Preoperative Cognitive Impairment as a Predictor of Postoperative Outcomes in Elderly Patients Undergoing Spinal Surgery for Degenerative Spinal Disease" Journal of Clinical Medicine 10, no. 7: 1385. https://doi.org/10.3390/jcm10071385
APA StyleKim, H. C., An, S. B., Jeon, H., Kim, T. W., Oh, J. K., Shin, D. A., Yi, S., Kim, K. N., Lee, P. H., Kang, S. Y., & Ha, Y. (2021). Preoperative Cognitive Impairment as a Predictor of Postoperative Outcomes in Elderly Patients Undergoing Spinal Surgery for Degenerative Spinal Disease. Journal of Clinical Medicine, 10(7), 1385. https://doi.org/10.3390/jcm10071385






