Physicochemical Properties of Lipoproteins Assessed by Nuclear Magnetic Resonance as a Predictor of Premature Cardiovascular Disease. PRESARV-SEA Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Population
2.2. Variables Included
2.3. Sample Collection
2.4. Methods
2.4.1. Lipoprotein Precipitation Techniques
2.4.2. Nuclear Magnetic Resonance (NMR) Analysis
2.5. Statistical Analysis
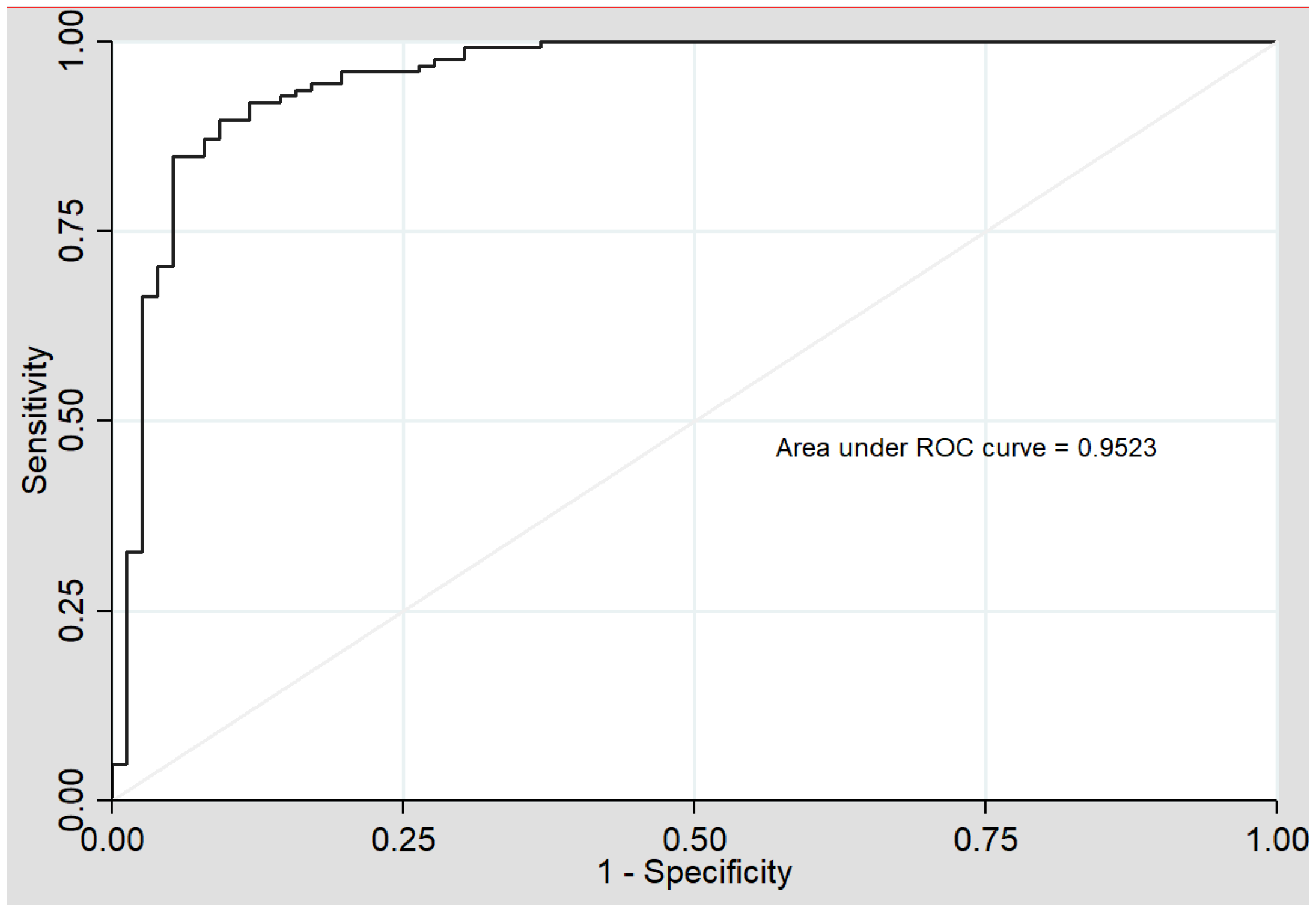
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Vikulova, D.N.; Grubisic, M.; Zhao, Y.; Lynch, K.; Humphries, K.H.; Pimstone, S.N.; Brunham, L.R. Premature Atherosclerotic Cardiovascular Disease: Trends in Incidence, Risk Factors, and Sex-Related Differences, 2000 to 2016. J. Am. Heart Assoc. 2019, 8, e012178. [Google Scholar] [CrossRef]
- Piepoli, M.F.; Hoes, A.W.; Agewall, S.; Albus, C.; Brotons, C.; Catapano, A.L.; Cooney, M.T.; Corrà, U.; Cosyns, B.; Deaton, C.; et al. 2016 European Guidelines on cardiovascular disease prevention in clinical practice: The Sixth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of 10 societies and by invited experts) Developed with the special contribution of the European Association for Cardiovascular Prevention & Rehabilitation (EACPR). Eur. Heart J. 2016, 37, 2315–2381. [Google Scholar]
- Ambegaonkar, B.; Bash, L.; Chirovsky, D.; Jameson, K.; Grant, S.; Nocea, G.; Pettersson, B.; Sazonov, V. Attainment of normal lipid levels among high cardiovascular risk patients: Pooles analysis of observational studies from the United Kingdom, Sweden, Spain and Canada. Eur. J. Intern. Med. 2013, 24, 656–663. [Google Scholar] [CrossRef]
- Dawber, T.R.; Moore, F.E.; Mann, G.V., II. Coronary Heart Disease in the Framingham Study. Int. J. Epidemiol. 2015, 44, 1767–1780. [Google Scholar] [CrossRef]
- Sampson, U.K.; Fazio, S.; Linton, M.F. Residual cardiovascular risk despite optimal LDL-cholesterol reduction with statins: The evidence, etiology, and therapeutic challenges. Curr. Atheroscler. Rep. 2012, 14, 1–10. [Google Scholar] [CrossRef]
- Fernández-Friera, L.; Fuster, V.; López-Melgar, B.; Oliva, B.; García-Ruiz, J.M.; Mendiguren, J.; Bueno, H.; Pocock, S.; Ibáñez, B.; Fernández-Ortiz, A.; et al. Normal LDL-Cholesterol Levels Are Associated with Subclinical Atherosclerosis in the Absence of Risk Factors. J. Am. Coll. Cardiol. 2017, 70, 2979–2991. [Google Scholar] [CrossRef]
- Al Rifai, M.; Martin, S.S.; McEvoy, J.W.; Nasir, K.; Blankstein, R.; Yeboah, J.; Miedema, M.; Shea, S.J.; Polak, J.F.; Ouyang, P.; et al. The prevalence and correlates of subclinical atherosclerosis among adults with low-density lipoprotein cholesterol <70 mg/dL: The Multi-Ethnic Study of Atherosclerosis (MESA) and Brazilian Longitudinal Study of Adult Health (ELSA-Brasil). Atherosclerosis 2018, 274, 61–66. [Google Scholar] [CrossRef]
- Higashioka, M.; Sakata, S.; Honda, T.; Hata, J.; Yoshida, D.; Hirakawa, Y.; Shibata, M.; Goto, K.; Kitazono, T.; Osawa, H.; et al. Small Dense Low-Density Lipoprotein Cholesterol and the Risk of Coronary Heart Disease in a Japanese Community. J. Atheroscler. Thromb. 2020, 27, 669–682. [Google Scholar] [CrossRef]
- Mora, S.; Otvos, J.; Rifai, N.; Rosenson, R.; Buring, J.; Ridker, P. Lipoprotein particle profiles by nuclear magnetic resonance compared with standard lipids and apolipoproteins in predicting incident cardiovascular disease in women. Circulation 2009, 119, 931–939. [Google Scholar] [CrossRef]
- Hoogeveen, R.C.; Gaubatz, J.W.; Sun, W.; Dodge, R.C.; Crosby, J.R.; Jiang, J.; Couper, D.; Virani, S.S.; Kathiresan, S.; Boerwinkle, E.; et al. Small dense low-density lipoprotein-cholesterol concentrations predict risk for coronary heart disease. Arterioscler. Thromb. Vasc. Biol. 2014, 34, 1069–1077. [Google Scholar] [CrossRef]
- Pintó, X.; Masana, L.; Civeira, F.; Real, J.; Ibarretxe, D.; Candas, B.; Puzo, J.; Díaz, J.L.; Amigó, N.; Esteban, M.; et al. Consensus document of an expert group from the Spanish Society of Arteriosclerosis (SEA) on the clinical use of nuclear magnetic resonance to assess lipoprotein metabolism (Liposcale®). Clin. Investig. Arterioscler. 2020, 32, 219–229. [Google Scholar] [CrossRef]
- Hirano, T.; Ito, Y.; Saegusa, H.; Yoshino, G. A novel and simple method for quantification of small, dense LDL. J. Lipid Res. 2003, 44, 2193–2201. [Google Scholar] [CrossRef] [PubMed]
- Otvos, J.; Mora, S.; Shalaurova, I.; Greenland, P.; Mackey, R.; Goff, D. Clinical implications of discordance between low-density lipoprotein cholesterol and particle number. J. Clin. Lipidol. 2011, 5, 105–113. [Google Scholar] [CrossRef]
- Fernández-Cidón, B.; Padró-Miquel, A.; Alía-Ramos, P.; Castro-Castro, M.J.; Fanlo-Maresma, M.; Dot-Bach, D.; Valero-Politi, J.; Pintó-Sala, X.; Candás-Estébanez, B. Reference values assessment in a Mediterranean population for small dense low-density lipoprotein concentration isolated by an optimized precipitation method. Vasc. Health Risk Manag. 2017, 13, 201–207. [Google Scholar] [CrossRef]
- Mallol, R.; Amigó, N.; Rodríguez, M.A.; Heras, M.; Vinaixa, M.; Plana, N.; Rock, E.; Ribalta, J.; Yanes, O.; Masana, L.; et al. Liposcale: A novel advanced lipoprotein test based on 2D diffusion ordered 1H NMR spectroscopy. J. Lipid Res. 2015, 56, 737–746. [Google Scholar] [CrossRef] [PubMed]
- Rock, E.; Winklhofer-Roob, B.M.; Ribalta, J.; Scotter, M.; Vasson, M.P.; Brtko, J.; Brigelius-Flohe, R.; Bronner, A.; Azais-Braesco, V. Vitamin A, vitamin E and carotenoid status and metabolism during ageing: Functional and nutritional consequences (VITAGE Project). Nutr. Metab. Cardiovasc. Dis. 2001, 11, 70–73. [Google Scholar] [PubMed]
- Fernandez-Ortiz, A.; Jimenez-Borreguero, L.J.; Penalvo, J.L.; Ordovás, J.M.; Mocoroa, A.; Fernández-Friera, L.; Laclaustra, M.; García, L.; Molina, J.; Mendiguren, J.M.; et al. The Progression and Early detection of Subclinical Atherosclerosis (PESA) study: Rationale and design. Am. Heart J. 2013, 166, 990–998. [Google Scholar] [CrossRef] [PubMed]
- Baigent, C.; Keech, A.; Kearney, P.M.; Blackwell, L.; Buck, G.; Pollicino, C.; Kirby, A.; Sourjina, T.; Peto, R.; Collins, R.; et al. Collaborators. Efficacy and safety of cholesterol-lowering treatment: Prospective meta-analysis of data from 90 056 participants in 14 randomised trials of statins. Lancet 2005, 366, 1267–1278. [Google Scholar] [CrossRef]
- Shiffman, D.; Louie, J.Z.; Caul, M.P.; Nilsson, P.M.; Devlin, J.J.; Melander, O. LDL subfractions are associated with incident cardiovascular disease in the Malmo Prevention Project Study. Atherosclerosis 2017, 263, 287–292. [Google Scholar] [CrossRef]
- Cromwell, W.C.; Otvos, J.D.; Keyes, M.J.; Pencina, M.J.; Sullivan, L.; Vasan, R.S.; Wilson, P.W.; D’Agostino, R.B. LDL Particle Number and Risk of Future Cardiovascular Disease in the Framingham Offspring Study—Implications for LDL Management. J. Clin. Lipidol. 2007, 1, 583–592. [Google Scholar] [CrossRef]
- Aday, A.W.; Lawler, P.R.; Cook, N.R.; Ridker, P.M.; Mora, S.; Pradhan, A.D. Lipoprotein Particle Profiles, Standard Lipids, and Peripheral Artery Disease Incidence. Circulation 2018, 138, 2330–2341. [Google Scholar] [CrossRef]
- Urbina, E.M.; McCoy, C.E.; Gao, Z.; Khoury, P.R.; Shah, A.S.; Dolan, L.M.; Kimball, T.R. Lipoprotein particle number and size predict vascular structure and function better than traditional lipids in adolescents and young adults. J. Clin. Lipidol. 2017, 11, 1023–1031. [Google Scholar] [CrossRef]
- Shah, A.S.; Davidson, W.S.; Gao, Z.; Dolan, L.M.; Kimball, T.R.; Urbina, E.M. Superiority of lipoprotein particle number to detect associations with arterial thickness and stiffness in obese youth with and without prediabetes. J. Clin. Lipidol. 2016, 10, 610–618. [Google Scholar] [CrossRef] [PubMed]
- Kathiresan, S.; Otvos, J.D.; Sullivan, L.M.; Keyes, M.J.; Schaefer, E.J.; Wilson, P.W.; D’Agostino, R.B.; Vasan, R.S.; Robins, S.J. Increased small low-density lipoprotein particle number: A prominent feature of the metabolic syndrome in the Framingham Heart Study. Circulation 2006, 113, 20–29. [Google Scholar] [CrossRef]
- Holmes, M.V.; Millwood, I.Y.; Kartsonaki, C.; Hill, M.R.; Bennett, D.A.; Boxall, R.; Guo, Y.; Xu, X.; Bian, Z.; Hu, R.; et al. Lipids, Lipoproteins, and Metabolites and Risk of Myocardial Infarction and Stroke. J. Am. Coll. Cardiol. 2018, 71, 620–632. [Google Scholar] [CrossRef] [PubMed]
- Ip, S.; Lichtenstein, A.H.; Chung, M.; Lau, J.; Balk, E.M. Systematic review: Association of low-density lipoprotein subfractions with cardiovascular outcomes. Ann. Intern. Med. 2009, 150, 474–484. [Google Scholar] [CrossRef] [PubMed]
- Mora, S.; Buring, J.E.; Ridker, P.M. Discordance of low-density lipoprotein (LDL) cholesterol with alternative LDL-related measures and future coronary events. Circulation 2014, 129, 553–561. [Google Scholar] [CrossRef]
- Mudd, J.O.; Borlaug, B.A.; Johnston, P.V.; Kral, B.G.; Rouf, R.; Blumenthal, R.S.; Kwiterovich, P.O., Jr. Beyond low density lipoprotein cholesterol: Defining the role of low-density lipoprotein heterogeneity in coronary artery disease. J. Am. Coll. Cardiol. 2007, 50, 1735–1741. [Google Scholar] [CrossRef]
- Kontush, A.; Chantepie, S.; Chapman, M.J. Small, dense HDL particles exert potent protection of atherogenic LDL against oxidative stress. Arterioscler. Thromb. Vasc. Biol. 2003, 23, 1881–1888. [Google Scholar] [CrossRef]
- Albers, J.J.; Slee, A.; Fleg, J.L.; O’Brien, K.D.; Marcovina, S.M. Relationship of baseline HDL subclasses, small dense LDL and LDL triglyceride to cardiovascular events in the AIM-HIGH clinical trial. Atherosclerosis 2016, 251, 454–459. [Google Scholar] [CrossRef][Green Version]
- Fernández-Castillejo, S.; Pedret, A.; Catalán, Ú.; Valls, R.M.; Farràs, M.; Rubió, L.; Castañer, O.; Macià, A.; Fitó, M.; Motilva, M.J.; et al. Virgin Olive Oil Phenolic Compounds Modulate the HDL Lipidome in Hypercholesterolaemic Subjects: A Lipidomic Analysis of the VOHF Study. Mol. Nutr. Food Res. 2021, e2001192. [Google Scholar] [CrossRef] [PubMed]
- Duparc, T.; Ruidavets, J.B.; Genoux, A.; Ingueneau, C.; Najib, S.; Ferrières, J.; Perret, B.; Martinez, L.O. Serum level of HDL particles are independently associated with long-term prognosis in patients with coronary artery disease: The GENES study. Sci. Rep. 2020, 10, 8138. [Google Scholar] [CrossRef] [PubMed]
- Sniderman, A.D.; Thanassoulis, G.; Glavinovic, T.; Navar, A.M.; Pencina, M.; Catapano, A.; Ference, B.A. Apolipoprotein B Particles and Cardiovascular Disease: A Narrative Review. JAMA Cardiol. 2019, 4, 1287–1295. [Google Scholar] [CrossRef] [PubMed]
- Kim, D.S.; Li, Y.K.; Bell, G.A.; Burt, A.A.; Vaisar, T.; Hutchins, P.M.; Furlong, C.E.; Otvos, J.D.; Polak, J.F.; Arnan, M.K.; et al. Concentration of Smaller High-Density Lipoprotein Particle (HDL-P) Is Inversely Correlated with Carotid Intima Media Thickening After Confounder Adjustment: The Multi Ethnic Study of Atherosclerosis (MESA). J. Am. Heart Assoc. 2016, 5, e002977. [Google Scholar] [CrossRef]
- Würtz, P.; Raiko, J.R.; Magnussen, C.G.; Soininen, P.; Kangas, A.J.; Tynkkynen, T.; Thomson, R.; Laatikainen, R.; Savolainen, M.J.; Laurikka, J.; et al. High-throughput quantifi cation of circulating metabolites improves prediction of subclinical atherosclerosis. Eur. Heart J. 2012, 33, 2307–2316. [Google Scholar] [CrossRef]
- Rosenson, R.S.; Davidson, M.H.; Pourfarzib, R. Underappreciated opportunities for low-density lipoprotein management in patients with cardiometabolic risk. Atherosclerosis 2010, 213, 1–7. [Google Scholar] [CrossRef]
- Garber, A.J.; Abrahamson, M.J.; Barzilay, J.I.; Blonde, L.; Bloomgarden, Z.T.; Bush, M.A.; Dagogo-Jack, S.; DeFronzo, R.A.; Einhorn, D.; Fonseca, V.A.; et al. Consensus statement by the american association of clinical endocrinologists and american college of endocrinology on the comprehensive type 2 diabetes management algorithm—2016 executive summary. Endocr. Pract. 2016, 22, 84–113. [Google Scholar] [CrossRef] [PubMed]
- Cole, T.G.; Contois, J.H.; Csako, G.; McConnell, J.P.; Remaley, A.T.; Devaraj, S.; Hoefner, D.M.; Mallory, T.; Sethi, A.A.; Warnick, G.R. Association of apolipoprotein B and nuclear magnetic resonance spectroscopy-derived LDL particle number with outcomes in 25 clinical studies: Assessment by the AACC Lipoprotein and Vascular Diseases Division Working Group on Best Practices. Clin. Chem. 2013, 59, 752–770. [Google Scholar] [CrossRef] [PubMed]
| Variables (Units) | Control Group n = 190 | PCVD Group n = 125 |
|---|---|---|
| Age (years) | 47 (3.7) | 46.5 (4.4) |
| Male (%) | 150 (78.9%) | 99 (79.2%) |
| Coronary artery disease | - | 79 (63.2%) |
| Stroke or TIA | - | 46 (36.8%) a |
| BMI (kg/m2) | 26.7(3.6) | 29 (4.98) a |
| Diabetes mellitus | 3 (1.6%) | 16 (12.8%) a |
| Hypertension | 22 (11.6%) | 48 (38.4%) |
| Smoking | 59 (31%) | 32 (25.6%) |
| Lipid-lowering drugs | 20 (10.5%) | 116 (92.8%) a |
| Anti-platelet drugs | 3 (1.6%) | 118 (94.4%) a |
| Cholesterol (mg/dL) | 207.4 (33.3) | 155.3 (40.8) a |
| HDL-Cholesterol (mg/dL) | 56.8 (12.4) | 44.5 (14.8) a |
| Triglycerides (mg/dL) | 121.1 (98.6) | 140.6 (99.6) |
| LDL-C (mg/dL) | 144.38 (12.5) | 96.49 (7.9) a |
| Variables (Units) | Control Group (n = 190) | PCVD Group (n = 125) | p Value |
|---|---|---|---|
| Very Low Density Lipoprotein | |||
| Cholesterol (mg/dL) | 12.27 (6.90–21.16) | 14.21 (8.44–19.94) | 0.173 |
| Triglycerides (mg/dL) | 56.72 (33.74–82.68) | 61.15 (43.67–92.71) | 0.06 |
| Total particles (nmol/L) | 41.22 (23.86–62.63) | 41.57 (30.93–64.28) | 0.143 |
| Large particles (nmol/L) | 0.85 (0.53–1.29) | 1.27 (0.94–1.76) | <0.0001 |
| Medium particles (nmol/L) | 4.57 (3.05–6.39) | 5.04 (3.21–8.13) | 0.245 |
| Small particles (nmol/L) | 36.00 (20.21–54.55) | 35.11 (27.05–55.86) | 0.138 |
| Diameter (nm) | 42.13 (42.01–42.25) | 42.28 (42.14–42.43) | <0.0001 |
| Intermediate Density Lipoprotein | |||
| Cholesterol (mg/dL) | 8.16 (5.53–11.05) | 9.07 (7.22–11.43) | 0.074 |
| Triglycerides (mg/dL) | 10.05 (7.91–12.96) | 9.81 (8.27–11.60) | 0.683 |
| Low Density Lipoprotein | |||
| Cholesterol (mg/dL) | 144.38 (134.08–169.37) | 96.49 (83.14–112.22) | <0.0001 |
| Triglycerides (mg/dL) | 19.27 (11.61–23.86) | 12.07 (9.66–15.01) | <0.0001 |
| Total particles (nmol/L) | 1457.93 (1312.05–1648.66) | 994.78 (880.20–1144.72) | <0.0001 |
| Large particles (nmol/L) | 221.12 (186.67–238.65) | 158.76 (139.20–175.46) | <0.0001 |
| Medium particles (nmol/L) | 519.99 (422.60–605.56) | 246.81 (187.99–308.80) | <0.0001 |
| Small particles (nmol/L) | 724.35 (642.38–861.24) | 587.73 (532.41–671.76) | <0.0001 |
| Cholesterol small particles (mmol/L) | 320.00 (180.15–460.06) | 420.38 (265.28–704.79) | <0.0001 |
| Diameter (nm) | 21.16 (20.99–21.33) | 20.91 (20.78–21.06) | <0.0001 |
| High Density Lipoprotein | |||
| Cholesterol (mg/dL) | 48.86 (38.76–57.78) | 45.47(39.92–51.72) | 0.101 |
| Triglycerides (mg/dL) | 7.88 (6.07–9.85) | 14.61(11.41–17.52) | <0.0001 |
| Total particles (µmol/L) | 24.78 (20.18–28.12) | 24.18 (21.05–27.86) | 0.855 |
| Large particles (µmol/L) | 0.23 (0.19–0.27) | 0.26 (0.24–0.30) | <0.0001 |
| Medium particles (µmol/L) | 6.80 (5.66–8.69) | 9.02 (7.93–10.43) | <0.0001 |
| Small particles (µmol/L) | 16.83 (13.93–19.34) | 14.98 (12.08–17.57) | 0.003 |
| Diameter (µmol/L) | 8.21 (8.17–8.25) | 8.30 (8.24–8.34) | <0.0001 |
| Variables (Units) | OR | [CI 95%] | p Value | R2 |
|---|---|---|---|---|
| Constant | 27.367 | 1.650 to 453.845 | 0.021 | 0.730 |
| sdLDL-C (mmol/L) | 1.002 | 1.000 to 1.003 | 0.030 | |
| HDL-Tg (mg/dL) | 1.622 | 1.296 to 1.764 | <0.0001 | |
| lLDL-P (nmol/L) | 0.956 | 0.941 to 0.967 | <0.0001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fernández-Cidón, B.; Candás-Estébanez, B.; Gil-Serret, M.; Amigó, N.; Corbella, E.; Rodríguez-Sánchez, M.Á.; Padró-Miquel, A.; Brotons, C.; Hernández-Mijares, A.; Calmarza, P.; et al. Physicochemical Properties of Lipoproteins Assessed by Nuclear Magnetic Resonance as a Predictor of Premature Cardiovascular Disease. PRESARV-SEA Study. J. Clin. Med. 2021, 10, 1379. https://doi.org/10.3390/jcm10071379
Fernández-Cidón B, Candás-Estébanez B, Gil-Serret M, Amigó N, Corbella E, Rodríguez-Sánchez MÁ, Padró-Miquel A, Brotons C, Hernández-Mijares A, Calmarza P, et al. Physicochemical Properties of Lipoproteins Assessed by Nuclear Magnetic Resonance as a Predictor of Premature Cardiovascular Disease. PRESARV-SEA Study. Journal of Clinical Medicine. 2021; 10(7):1379. https://doi.org/10.3390/jcm10071379
Chicago/Turabian StyleFernández-Cidón, Bárbara, Beatriz Candás-Estébanez, Miriam Gil-Serret, Núria Amigó, Emili Corbella, M. Ángeles Rodríguez-Sánchez, Ariadna Padró-Miquel, Carlos Brotons, Antonio Hernández-Mijares, Pilar Calmarza, and et al. 2021. "Physicochemical Properties of Lipoproteins Assessed by Nuclear Magnetic Resonance as a Predictor of Premature Cardiovascular Disease. PRESARV-SEA Study" Journal of Clinical Medicine 10, no. 7: 1379. https://doi.org/10.3390/jcm10071379
APA StyleFernández-Cidón, B., Candás-Estébanez, B., Gil-Serret, M., Amigó, N., Corbella, E., Rodríguez-Sánchez, M. Á., Padró-Miquel, A., Brotons, C., Hernández-Mijares, A., Calmarza, P., Jarauta, E., Brea, A. J., Mauri, M., Guijarro, C., Vila, À., Valdivielso, P., Corbella, X., & Pintó, X. (2021). Physicochemical Properties of Lipoproteins Assessed by Nuclear Magnetic Resonance as a Predictor of Premature Cardiovascular Disease. PRESARV-SEA Study. Journal of Clinical Medicine, 10(7), 1379. https://doi.org/10.3390/jcm10071379









