The Effect of the 2019 Novel Coronavirus Pandemic on Stroke and TIA Patient Admissions: Perspectives and Risk Factors
Abstract
1. Introduction
Aims
2. Materials and Methods
2.1. Specialist Stroke Unit
2.2. Admissions Data Analysis
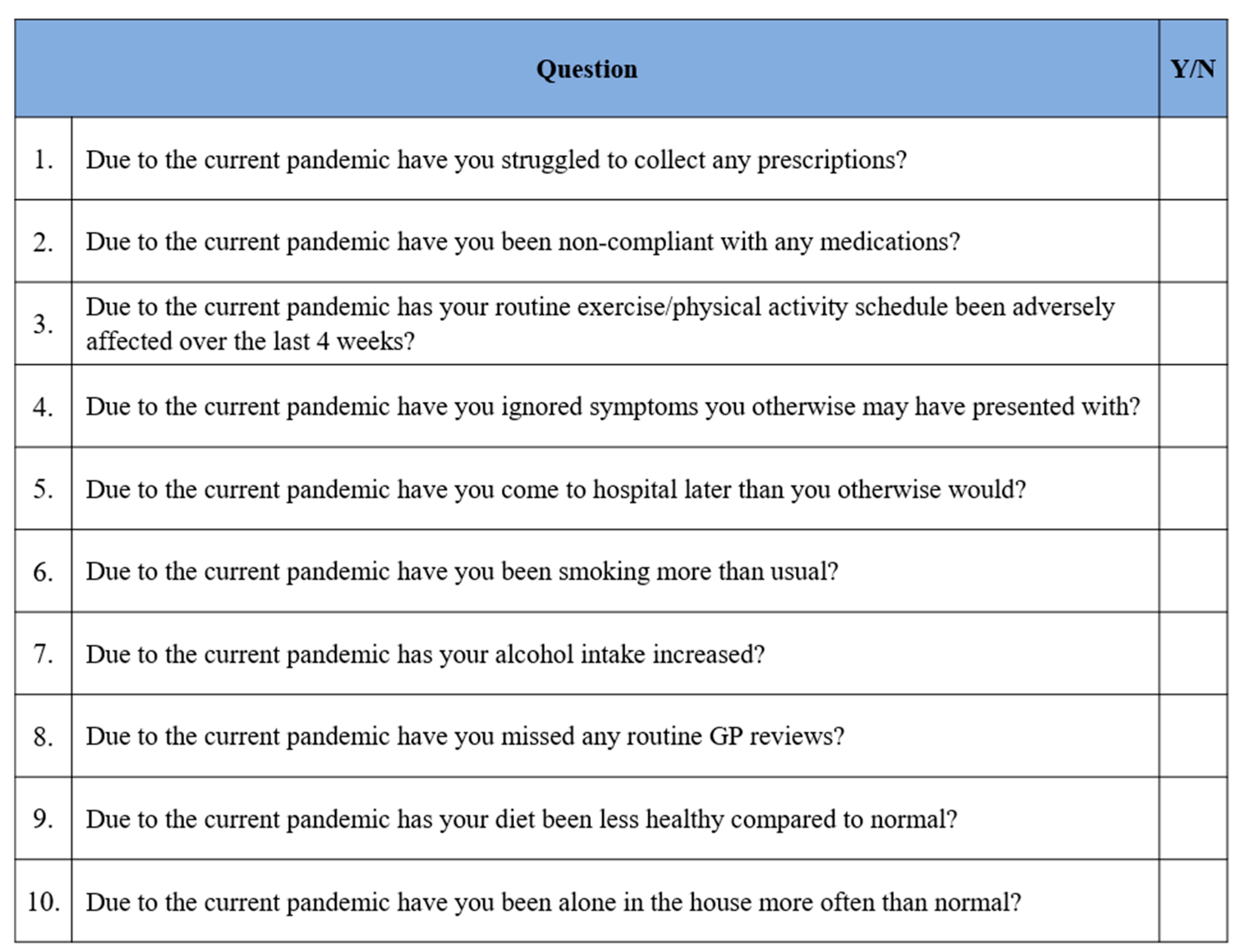
2.3. COVID-19 Patient Questionnaire
3. Results
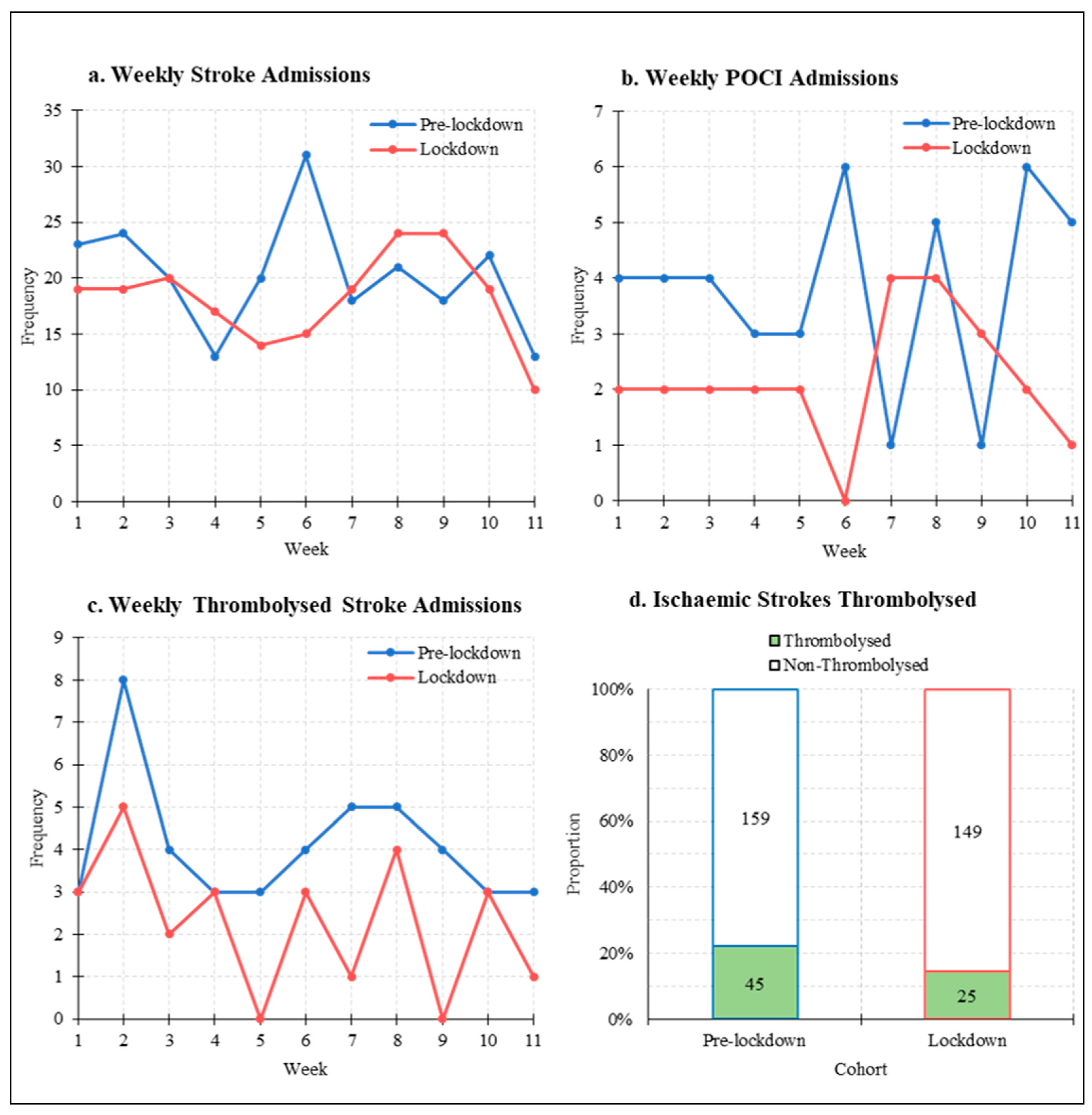
3.1. Stroke Admissions
3.2. Stroke Mimic Admissions and TIA Referrals
3.3. COVID-19 Patient Questionnaire
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Zhu, N.; Zhang, D.; Wang, W.; Li, X.; Yang, B.; Song, J.; Zhao, X.; Huang, B.; Shi, W.; Lu, R.; et al. A novel coronavirus from patients with pneumonia in China, 2019. N. Engl. J. Med. 2020, 382, 727–733. [Google Scholar] [CrossRef] [PubMed]
- WHO WHO/Europe|Coronavirus Disease (COVID-19) Outbreak—WHO Announces COVID-19 Outbreak a Pandemic. Available online: https://www.euro.who.int/en/health-topics/health-emergencies/coronavirus-covid-19/news/news/2020/3/who-announces-covid-19-outbreak-a-pandemic (accessed on 23 March 2021).
- NHS England. A&E Attendances and Emergency Admissions March 2020 Statistical Commentary; NHS England: London, UK, 2020. [Google Scholar]
- Naccarato, M.; Scali, I.; Olivo, S.; Ajčević, M.; Stella, A.B.; Furlanis, G.; Lugnan, C.; Caruso, P.; Peratoner, A.; Cominotto, F.; et al. Has COVID-19 played an unexpected “stroke” on the chain of survival? J. Neurol. Sci. 2020, 414, 116889. [Google Scholar] [CrossRef] [PubMed]
- Slomka, A.; Kowalewski, M.; Żekanowska, E. Haemostasis in coronavirus disease 2019—Lesson from viscoelastic methods: A systematic review. Thromb. Haemost. 2021. [Google Scholar] [CrossRef]
- Levi, M.; Thachil, J.; Iba, T.; Levy, J.H. Coagulation abnormalities and thrombosis in patients with COVID-19. Lancet Haematol. 2020, 7, e438. [Google Scholar] [CrossRef]
- Mao, L.; Jin, H.; Wang, M.; Hu, Y.; Chen, S.; He, Q.; Chang, J.; Hong, C.; Zhou, Y.; Wang, D.; et al. Neurologic Manifestations of Hospitalized Patients with Coronavirus Disease 2019 in Wuhan, China. JAMA Neurol. 2020, 77, 683–690. [Google Scholar] [CrossRef] [PubMed]
- Beyrouti, R.; Adams, M.E.; Benjamin, L.; Cohen, H.; Farmer, S.F.; Goh, Y.Y.; Humphries, F.; Jäger, H.R.; Losseff, N.A.; Perry, R.J.; et al. Characteristics of ischaemic stroke associated with COVID-19. J. Neurol. Neurosurg. Psychiatry 2020, 91, 889–891. [Google Scholar] [CrossRef] [PubMed]
- Yaghi, S.; Ishida, K.; Torres, J.; Mac Grory, B.; Raz, E.; Humbert, K.; Henninger, N.; Trivedi, T.; Lillemoe, K.; Alam, S.; et al. SARS-CoV-2 and Stroke in a New York Healthcare System. Stroke 2020, 51, 2002–2011. [Google Scholar] [CrossRef] [PubMed]
- Gomez, C.R. Editorial: Time is brain! J. Stroke Cerebrovasc. Dis. 1993, 3, 1–2. [Google Scholar] [CrossRef]
- Trialists, S.U. Collaborative systematic review of the randomised trials of organised inpatient (stroke unit) care after stroke. Stroke Unit Trialists’ Collaboration. BMJ 1997, 314, 1151. [Google Scholar]
- RS Team. RStudio: Integrated Development Environment for R; RS Team: Porto, Portugal, 2020. [Google Scholar]
- R Core Team. R: A Language and Environment for Statistical Computing; R Core Team: Vienna, Austria, 2020. [Google Scholar]
- Kassambara, A. ‘ggpubr’: “ggplot2” Based Publication Ready Plots. In R Packag. Version 025; 2020; Available online: http://www.sthda.com/english/articles/24-ggpubr-publication-ready-plots/ (accessed on 23 March 2021).
- Wickham, H.; François, R.; Henry, L.; Müller, K. dplyr: A Grammar of Data Manipulation. R package version. Media 2019, 13, 2020. [Google Scholar]
- Hoyer, C.; Ebert, A.; Huttner, H.B.; Puetz, V.; Kallmünzer, B.; Barlinn, K.; Haverkamp, C.; Harloff, A.; Brich, J.; Platten, M.; et al. Acute Stroke in Times of the COVID-19 Pandemic: A Multicenter Study. Stroke 2020, 51, 2224–2227. [Google Scholar] [CrossRef] [PubMed]
- Diegoli, H.; Magalhães, P.S.C.; Martins, S.C.O.; Moro, C.H.C.; França, P.H.C.; Safanelli, J.; Nagel, V.; Venancio, V.G.; Liberato, R.B.; Longo, A.L. Decrease in Hospital Admissions for Transient Ischemic Attack, Mild, and Moderate Stroke During the COVID-19 Era. Stroke 2020, 51, 2315–2321. [Google Scholar] [CrossRef] [PubMed]
- Frisullo, G.; Brunetti, V.; Di Iorio, R.; Broccolini, A.; Caliandro, P.; Monforte, M.; Morosetti, R.; Piano, C.; Pilato, F.; Calabresi, P.; et al. Effect of lockdown on the management of ischemic stroke: An Italian experience from a COVID hospital. Neurol. Sci. 2020, 41, 2309–2313. [Google Scholar] [CrossRef] [PubMed]
- Arch, A.E.; Weisman, D.C.; Coca, S.; Nystrom, K.V.; Wira, C.R.; Schindler, J.L. Missed Ischemic Stroke Diagnosis in the Emergency Department by Emergency Medicine and Neurology Services. Stroke 2016, 47, 668–673. [Google Scholar] [CrossRef] [PubMed]
- Hand, P.J.; Kwan, J.; Lindley, R.I.; Dennis, M.S.; Wardlaw, J.M. Distinguishing between stroke and mimic at the bedside: The brain attack study. Stroke 2006, 37, 769–775. [Google Scholar] [CrossRef] [PubMed]
- Thornton, J. Stroke: “striking reductions” are seen in number of people with symptoms seeking help. BMJ 2020. [Google Scholar] [CrossRef]
- Morelli, N.; Rota, E.; Terracciano, C.; Immovilli, P.; Spallazzi, M.; Colombi, D.; Zaino, D.; Michieletti, E.; Guidetti, D. The Baffling Case of Ischemic Stroke Disappearance from the Casualty Department in the COVID-19 Era. Eur. Neurol. 2020. [Google Scholar] [CrossRef] [PubMed]
- Mandelzweig, L.; Goldbourt, U.; Boyko, V.; Tanne, D. Perceptual, social, and behavioral factors associated with delays in seeking medical care in patients with symptoms of acute stroke. Stroke 2006, 37, 1248–1253. [Google Scholar] [CrossRef]

| 11-Week Total | Weekly Admissions | ||||||
|---|---|---|---|---|---|---|---|
| Diagnosis | Pre- Lockdown | Lockdown | Change | Pre-Lockdown (Mean ± SD) | Lockdown (Mean ± SD) | 95% CI | p Value |
| All stroke | n = 223 | n = 200 | −10.3% | 20.3 ± 5.1 | 18.2 ± 4.1 | −2.01–6.20 | 0.301 |
| ICH | n = 19 | n = 26 | +26.9% | 1.73 ± 0.9 | 2.36 ± 1.4 | 1.73–2.36 | 0.227 |
| Ischaemic Stroke | n = 204 | n = 174 | −14.7% | 18.5 ± 4.6 | 15.8 ± 3.8 | −1.02–6.47 | 0.144 |
| TACI | n = 43 | n = 32 | −25.6% | 3.91 ± 2.3 | 2.91 ± 2.3 | −1.03–3.03 | 0.316 |
| PACI | n = 50 | n = 55 | +10.0% | Median: 4 (IQR 3.5) | Median: 4 (IQR 2.5) | N/A | 0.616 |
| LACI | n = 62 | n = 59 | −4.8% | 5.64 ± 1.9 | 5.36 ± 1.8 | −1.38–1.93 | 0.734 |
| POCI | n = 42 | n = 24 | −42.9% | 3.82 ± 1.7 | 2.18 ± 1.2 | 0.33–2.94 | 0.017 |
| Infarct NOS | n = 7 | n = 4 | −42.9% | Median: 1 (IQR 1) | Median: 0 (IQR 1) | N/A | 0.350 |
| Thrombolysis | n = 45 | n = 25 | −44.4% | Median: 4 (IQR 1.5) | Median: 3 (IQR 2) | N/A | 0.018 |
| Diagnosis | Pre-Lockdown | Lockdown | Change | p Value | ||
|---|---|---|---|---|---|---|
| Ischaemic Stroke | n = 204/223 | (91.5%) | n = 174/200 | (87.0%) | −4.5% | 0.822 |
| ICH | n = 19/223 | (8.5%) | n = 26/200 | (13.0%) | +4.5% | 0.822 |
| TACI | n = 43/204 | (21.1%) | n = 32/174 | (18.4%) | −2.7% | 0.521 |
| PACI | n = 50/204 | (24.5%) | n = 55/174 | (31.6%) | +7.1% | 0.135 |
| LACI | n = 62/204 | (30.4%) | n = 59/174 | (33.9%) | +3.5% | 0.507 |
| POCI | n = 42/204 | (20.5%) | n = 24/174 | (13.8%) | −6.7% | 0.103 |
| Infarct NOS | n = 7/204 | (3.4%) | n = 4/174 | (2.3%) | −1.1% | 0.557 |
| Ischaemic Strokes Thrombolysed | n = 45/204 | (22.1%) | n = 25/174 | (14.4%) | −7.7% | 0.063 |
| Pre-Lockdown Onset-To-Presentation Time | Lockdown Onset-To-Presentation Time | |||||||
|---|---|---|---|---|---|---|---|---|
| Diagnosis | Size | Median (h) | IQR (h) | Size | Median (h) | IQR (h) | Change (h) | p Value |
| Stroke | n = 175 | 4.83 | 13.1 | n = 165 | 5.42 | 13.1 | +0.59 | 0.323 |
| Ischaemic Stroke | n = 161 | 5.22 | 13.2 | n = 142 | 6.11 | 13.0 | +0.89 | 0.249 |
| ICH | n = 14 | 2.19 | 7.5 | n = 23 | 2.68 | 12.0 | +0.49 | 0.673 |
| TACI | n = 35 | 2.25 | 7.0 | n = 26 | 2.88 | 5.5 | +0.63 | 0.218 |
| PACI | n = 39 | 3.68 | 8.7 | n = 40 | 4.28 | 11.6 | +0.60 | 0.222 |
| LACI | n = 51 | 8.12 | 14.6 | n = 53 | 6.98 | 14 | −1.14 | 0.833 |
| POCI | n = 31 | 11.82 | 15.6 | n = 20 | 13.67 | 42.5 | +1.85 | 0.401 |
| Infarct NOS | n = 5 | 2.25 | 0.91 | n = 2 | 8.04 | 3.89 | +5.79 | N/A |
| 11-Week Total | Weekly Admissions | ||||||
|---|---|---|---|---|---|---|---|
| Diagnosis | Pre-Lockdown | Lockdown | Change | Pre-Lockdown (Mean ± SD) | Lockdown (Mean ± SD) | 95% CI | p Value |
| Stroke-Mimic Admissions | n = 193 | n = 102 | −47.2% | 17.5 ± 3.3 | 9.3 ± 4.1 | 4.95–11.6 | <0.001 |
| Total Referrals | n = 152 | n = 105 | −30.9% | Median: 12 (IQR 6.5) | Median: 9 (IQR 5.5) | N/A | 0.037 |
| TIA Referrals | n = 57 | n = 53 | −7.02% | Median: 4 (IQR 2.5) | Median: 5 (IQR 4.5) | N/A | 0.552 |
| Non-TIA Referrals | n = 95 | n = 52 | −54.7% | 8.64 ± 3.1 | 4.73 ± 2.1 | 4.73–8.64 | 0.002 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Carson, L.; Kui, C.; Smith, G.; Dixit, A.K. The Effect of the 2019 Novel Coronavirus Pandemic on Stroke and TIA Patient Admissions: Perspectives and Risk Factors. J. Clin. Med. 2021, 10, 1357. https://doi.org/10.3390/jcm10071357
Carson L, Kui C, Smith G, Dixit AK. The Effect of the 2019 Novel Coronavirus Pandemic on Stroke and TIA Patient Admissions: Perspectives and Risk Factors. Journal of Clinical Medicine. 2021; 10(7):1357. https://doi.org/10.3390/jcm10071357
Chicago/Turabian StyleCarson, Luke, Christopher Kui, Gemma Smith, and Anand K. Dixit. 2021. "The Effect of the 2019 Novel Coronavirus Pandemic on Stroke and TIA Patient Admissions: Perspectives and Risk Factors" Journal of Clinical Medicine 10, no. 7: 1357. https://doi.org/10.3390/jcm10071357
APA StyleCarson, L., Kui, C., Smith, G., & Dixit, A. K. (2021). The Effect of the 2019 Novel Coronavirus Pandemic on Stroke and TIA Patient Admissions: Perspectives and Risk Factors. Journal of Clinical Medicine, 10(7), 1357. https://doi.org/10.3390/jcm10071357





