Critical Timepoint 2: Surgical Creation of a Neovagina
Since 1988 the laparoscopically assisted creation of a neovagina (modified Vecchietti technique) is successfully performed at the Department for Women’s Health in Tübingen. This state-of-the-art procedure enables the mainly adolescent MRKHS patients to have a normal sexually active life.
The main reason for surgery was the wish to be able to cohabitate (86%), followed by the wish to feel like a complete and normal woman (65%) and to be seen by the sexual partner like any other woman (52%). 54% of the MRKHS patients were minors at the time of surgery (
n = 82). The youngest patient who underwent surgery was 15.3, the oldest 43.4 years of age and the average age at surgery was 20 years. In average the patients waited 29.7 months between receiving the diagnosis and surgical therapy. 87% of the patients did not use self-dilation before surgery. Overall, the MRKHS patients are very satisfied with the surgery, the hospital care and the functional results, similar to the literature [
14,
41,
42,
43]. In order to receive the postoperative result 94% wore the phantom for 4.2 months postoperatively. Retrospectively, the postoperative pain on the intermediate care unit with the traction device in place was rated with 6 but tolerable in view of the success of surgery. Nevertheless, the possible postoperative pain situation should be explained and prepared extensively in advance. The use of a pain diary may be an option in order to optimize the monitoring of the pain after surgery. Already preoperatively, the management of former critical situations and individual coping strategies should be detected.
The postoperative measures were accepted and guaranteed the surgical success, which made sexual intercourse possible after four weeks. In average after 10.4 weeks our patients initiated regular sexual intercourse and 99 % of the MRKHS patients would recommend the method to others.
Mental disorders pre- and postoperatively (PHQ-D)
The stress caused by MRKHS did not lead to a higher risk for mental disorders in our patients compared to a healthy reference sample and our patients were better off compared to a mentally ill reference sample. There was no aggravation or improvement concerning somatic symptoms over the time. Nevertheless, 16% of the patients showed preoperatively and 20% twelve months postoperatively a moderate to severe somatization.
The symptoms of a somatization disorder are not intentionally provoked and are often associated with the coping of a disease. Bean et al. reported that the language used can influence the experience of a woman with MRKHS positively or negatively [
7]. Our specialized team of gynecologists is empathic and alert concerning psychosomatic symptoms which might develop in MRKHS patients over the time. The patients are offered psychosocial support at an early moment and not only focused on the physical anomaly. The early education that the diagnosis itself and especially the associated infertility will need a coping process, prevents a somatization disorder from developing.
Depressive symptoms
A depressive disorder is one of the commonest mental disorders implying relevant consequences. It is a collective term for different characteristics and diseases. In the study for adult health in Germany (DEGS1) it was found that the prevalence of depressive symptoms is age-dependent and that women are with 10% more often affected than men with 6%. Additionally, the prevalence is highest in the age group of 18–19 years of age (12%) and decreases thereafter [
44].
Our patient cohort belongs to a high-risk group for developing depressive symptoms due to the MRKHS diagnosis, the age between 18–29, being female and infertile. Hypothetically, we assumed persisting depressive values not only preoperatively but also postoperatively, because Langer et al. described 36% (
n = 11) MRKHS patients being depressive postoperatively [
45]. Möbus et al. identified higher depressive scores even after a successful creation of a neovagina in 44 MRKHS patients [
46]. The results were explained by the persisting infertility. Epstein and Rosenberg had proven a significantly higher depressive stress due to primary infertility [
47] and recently Chen et al. documented depressive symptoms even in 75% of the examined MRKHS patients as well as in one third of the patients a higher risk for depressive disorders [
48].
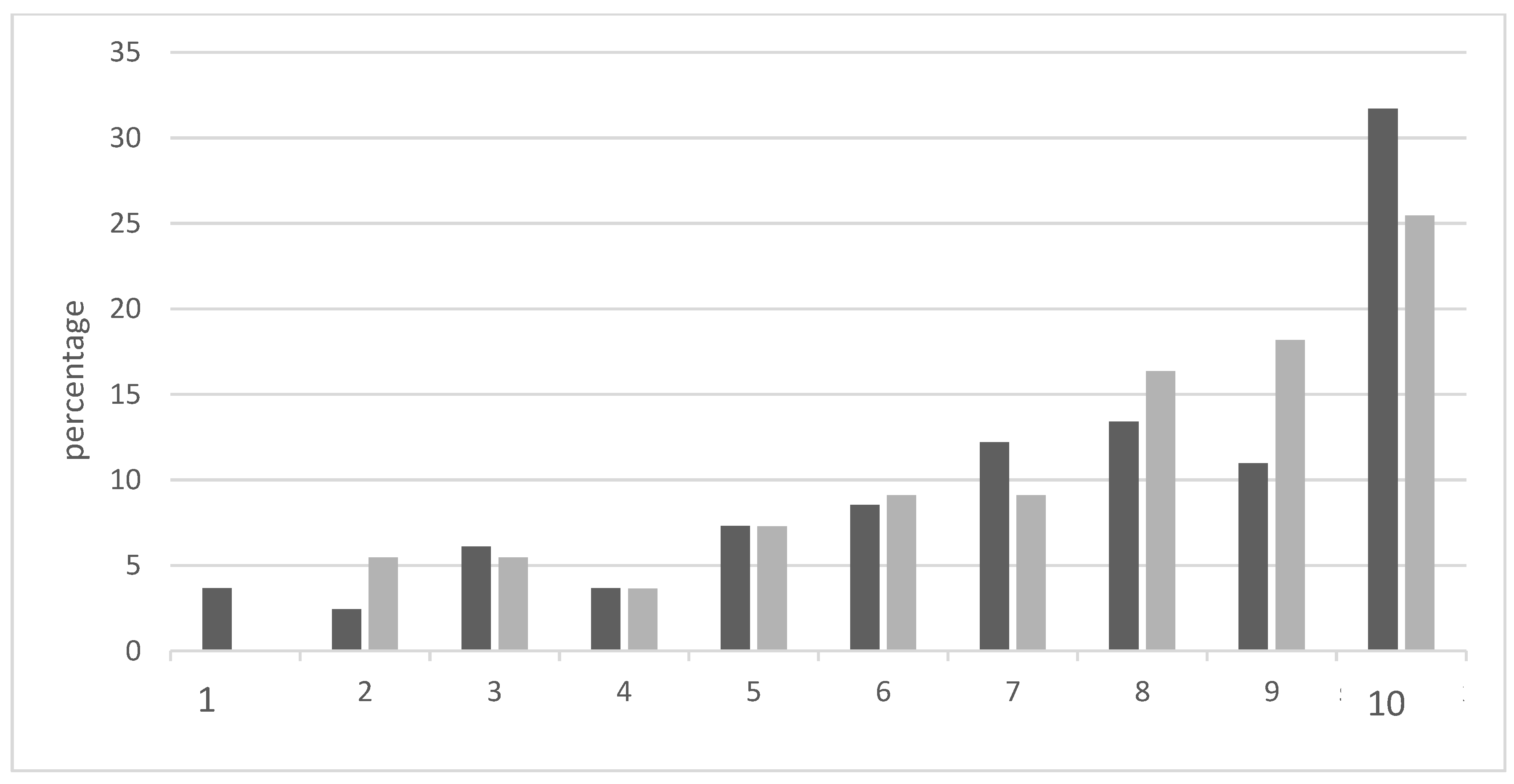
Different from the literature and because of the small sample size, with the PHQ-D we detected a significant mild/subliminal depression preoperatively, with postoperatively no higher prevalence compared to the general population [
44]. Using the SESA questionnaire, nearly 70% of the MRKHS patients did not need a differentiated examination in order to exclude a depressive disorder at any of the timepoints and compared to a depressive reference sample our patients showed significant better scores. For about 25% of our patients a differentiated examination was either necessary or an indicator for a depressive disorder was already present. The reduction of the mild depression from the beginning until TP2 and 3 indicates an initiated coping concerning the psychological abnormalities (inactivity, desperation, depressiveness). Even the prevalence of a major depression decreases postoperatively from 33% to 15% indicating a positive effect of the laparoscopically assisted creation of a neovagina and the thereby possible fulfilled partnership. Additionally, the confrontation with infertility at an early age makes it possible to deal with this issue earlier than usual, which can be an advantage and raise the chances of e.g., a successful adoption. Nevertheless, screening instruments like the PHQ-D should be used regularly in order to be able to support the patients as soon as possible when necessary especially when childbearing becomes an issue in the late twenties.
Psychological anomalies: eating disorders and alcohol syndrome
Descriptively, in the majority of cases our study showed less indicators for psychological disorders after surgery. Compared to the general population (females between 18 and 34 years of age) there was no higher prevalence of psychological disorders except for eating disorders (mainly bulimia nervosa and binge eating) and the alcohol syndrome. Heller-Boersma et al. also found conspicuous values of an eating disorder [
18]. Langer et al. reported the overlap of the MRKHS diagnosis and an abnormal body image [
45]. Eating disorders are known to be associated with disturbed body perceptions and therefore the malformation can increase the risk for the development of an eating disorder. As our study participants are mean between 19.9 and 21.4 years of age, they are within a period of life when they find and develop an own body image without MRKHS necessarily influencing this process. However, as the mentioned types of eating disorders are known to serve to deal with unpleasant emotions like stress, anxiety and desperation, which belong to the coping with MRKHS, patients should be offered psychotherapeutic help at any time.
The alcohol syndrome can be seen as a normal sign of development of an own identity during puberty and adolescence and is not necessarily related to the MRKHS diagnosis.
Body image disturbance pre-/postoperatively (FKB-20)
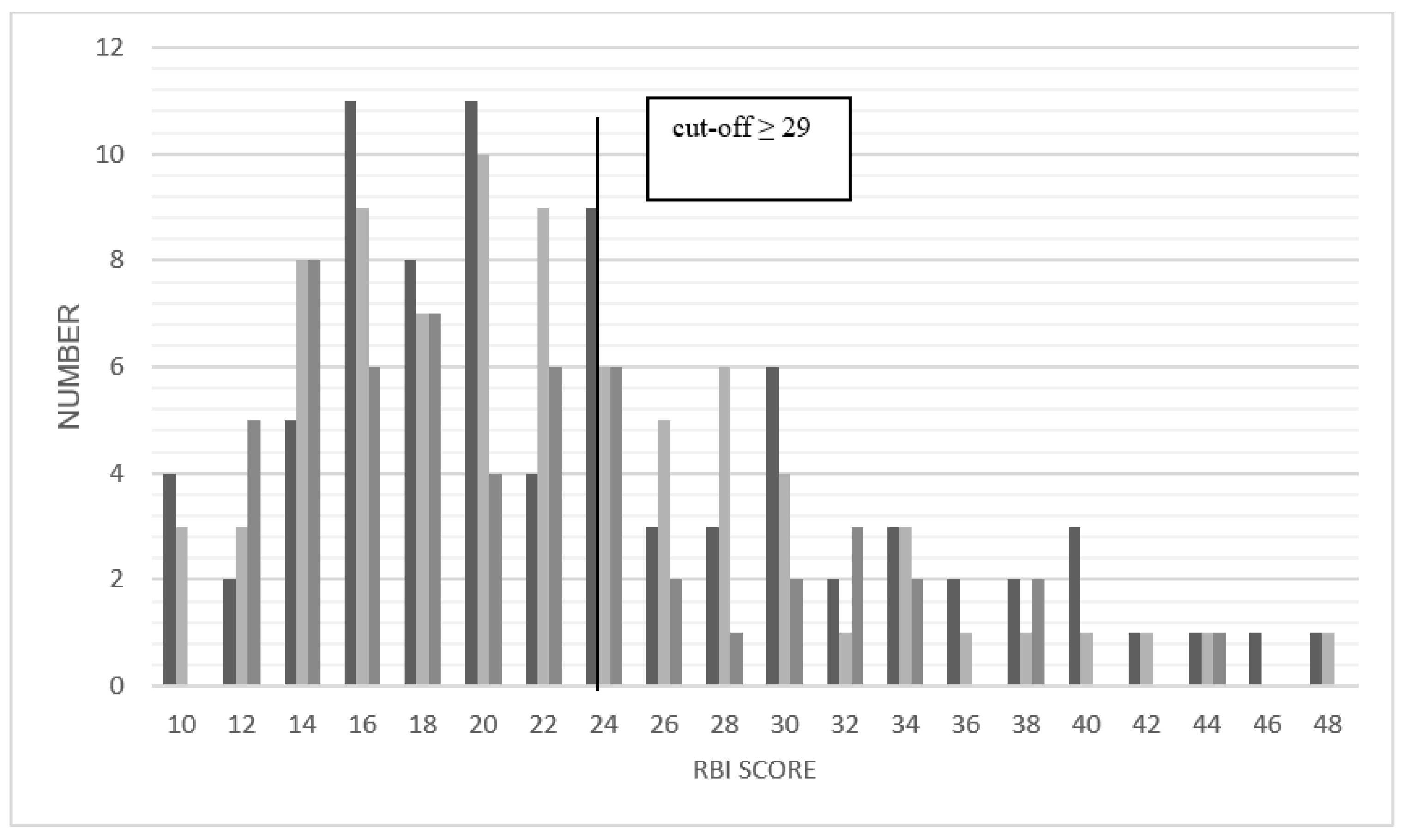
According to developmental psychology, adolescence with its physical changes and maturation crises has to be finished before a stable body image can develop. The mean values for the rejecting body evaluation (RBI) were for all three timepoints and the majority of the patients within the normal range and stable. 27% of the patients had a negative body image preoperatively, decreasing to 18% postoperatively. The vital body dynamics (VBD) shows similar results: still 31% of the MRKHS patients show a body image disturbance at TP3. An overlap on both scales (RBI and VBD) indicates a body image disturbance in 18% before and 13 to 14% after surgery. Compared to a patient sample with a wide range of symptoms and diagnoses MRKHS patients were significantly better.
Klingele et al. described 2003 in 55% of their patients a better self-image after surgery. Postoperatively, 62% were satisfied with their total body appearance [
49]. Riessen et al. could show a significant improvement in body image six months after our procedure [
50]. A stable body image was not possible yet to develop in our patients and adolescence itself certainly has a relevant impact on our findings. The laparoscopically assisted creation of a neovagina for sure has a positive effect, but a screening for body image disturbances is to be recommended and therapeutic options discussed.
Health related quality of life pre-/postoperatively (SF-12)
The diagnosis MRKHS poses a big challenge for the affected adolescents concerning their health-related quality of life, as even after creation of a neovagina they will not be able to carry a pregnancy.
For physical health (PCS) the patients show better values than the reference sample of chronically ill and even of healthy patients. Data for mental health indicate a significant impairment caused by MRKHS in all four areas: vitality, social functionality, emotional role function, mental wellbeing. This finding is confirmed by the comparison with the reference sample of chronically ill patients. Although the impairment decreases after surgery it remains within a low level and significant compared to the chronically ill 14–20 year olds pre-, as well as the 21–30-year-olds at TP1 and 2. The health related quality of life of MRKHS patients so far was only evaluated in a small number of studies: Kaloo et al. did not detect any difference, Klingele et al. could detect an improvement in quality of life of the MRKHS patients compared to the general population in 79% and Keckstein et al. 2008 in general, but with small sample sizes [
49,
51,
52]. Only Liao et al. differentiated between physical and mental health, reporting better values in physical and worse values in mental health [
53].
MRKHS patients in our study seemed to be physically unstressed but mentally impaired, and the higher values on the PCS can be explained by a familiarization with the MRKHS diagnosis and the surgical therapy and the normal “operation” in daily life. On the contrary, chronically ill patients usually have a relevant physical impairment.
Interesting is the fact, that MRKHS patients have a stronger mental impairment than chronically ill patients. This might be due to the fact that the SF-12 does not specifically distinguish between infertility and other reasons and therefore MRKHS patients seem to be more mentally impaired. The burden of infertility remains a focus throughout different phases of life, different from other chronic diseases which will be less and more relevant depending on the actual personal situation. The use of instruments other than the SF-12, which more specifically focus on quality of life can be useful in order to develop targeted coping strategies for MRKHS patients.
Altered self-acceptance after surgical creation of a neovagina (SESA)
With the SESA questionnaire we focused on the course of time and its effect on the self-esteem. We hypothesized that MRKHS patients have a lower self-acceptance before compared to after surgery. The hypothesis could be confirmed as the patients preoperatively had a lower self-esteem compared to the healthy reference sample. After surgery there was a normal self-acceptance and patients did not significantly differ from the reference sample. This is in contrast to the common hypothesis that MRKHS patients have a reduced self-esteem in general. Literature concerning self-acceptance in MRKHS is diverse. Heller-Boersma et al. supposed doubts concerning the own identity, a lower self-acceptance and self-esteem as a result of the information about the diagnosis [
8]. Morgan and Quint reported values within the average range [
33]. Möbus et al. and Klingele et al. as well as Keckstein et al. showed a significantly improved self-esteem after surgery [
46,
49,
52]. All these evaluations were performed retrospectively and did not include pre- and postoperative data.
Besides the postoperatively better self-esteem, our patients could easier engage into a partnership after surgery and approach men with a better self-esteem. Patients see themselves more competent in coping with MRKHS in different situations.
Critical Timepoint 3: Relationships and Sexuality
Impairment of the mother and mother-daughter-relationship
The mother is the number one person of trust for 76% of our MRKHS patients. The unconditional love between mother and daughter is put to the test during puberty and the finding of the own identity. The latter makes discrimination and own experiences necessary, and the peer-group becomes more important. The mother often has the feeling of losing something. The MRKHS diagnosis for the majority of the patients falls into this vulnerable phase of life and the mother changes into a passive role. The stress intensity of the mother on a scale between 1 and 10 was reported by the patients with an average value of 6.6 at TP2 (n = 79) and of 6.0 at TP3 (n = 54). The mother-daughter-relationship is mainly rated as positive and unchanged over the course of time. There was no relevant pressure by the mother to undergo diagnostic procedures (only in 13.4%) or surgical creation of a neovagina (only in 2.5%).
It is known that the mother-daughter-relationship has a critical influence on the development of female sexuality and the body image. The positive regard through the mother can have a positive effect on the postoperative results and improve the coping [
7,
54]. In a study by Leithner et al. MRKHS patients (
n = 10) describe their mothers as especially caring [
34]. Because of the reported stress intensity of the mothers, support should be offered, in order to be able to process their emotions, to recognize grief and sense of guilt and finally be able to support their daughters adequately.
Social support
Yearly patient days at the Department for Women’s Health in Tübingen could prove that MRKHS patients benefit from the personal exchange with others affected. In different seminars and workshops not only patients, but also relatives, partners and friends can talk to each other.
Ernst et al. reported that the contact and the communication about the MRKHS diagnosis among peers during adolescence under adequate guidance can be a source of support and strengthen relationships and self-esteem [
55]. In addition to the patient day 45% of our patients had contact to others affected or patient groups and the majority found these contacts helpful [
56]. For the motivation to tell others of the peer group about the diagnosis a strong confidence in the relationship is needed. The commonest reason not to tell others is the fear to meet with a refusal or be seen as a freak [
45,
57]. 5% of our patients did not take anyone into their confidence concerning the MRKHS diagnosis. It has been described before that some MRKHS patients wish to keep the diagnosis as their secret [
40,
57]. Nevertheless, 50% of the MRKHS patients share their worries with their family and friends twelve months after surgery. The removal of taboos and an open handling with the diagnosis are important factors. Patients must receive careful support concerning the topics how to describe and explain the malformation and to whom. Social support can thereby help to cope with the MRKHS diagnosis.
Partnership and sexuality
The issues partnership and sexuality are in association with the laparoscopically assisted creation of a neovagina two critical aspects: after surgery the patients were more often within a stable relationship than before surgery. 31% were more open and self-confident towards men after surgery than before. In our study sexual activity before and after surgery could be compared. Ismail-Pratt et al. found an evaluation of the preoperative sexuality not useful, because patients were not sexually active [
58]. We could not confirm this opinion, because 39% of our patients stated to have been sexually active before surgery with petting being the commonest form of sexual contact in 59%. The frequency of sexual contacts and the satisfaction with these increased constantly with the time from surgery. Moreover, the number of sexual partners increased. In total, the results can be seen as success as the patients develop their sexuality and dare to approach potential partners without too much fear.
FSFI-d
By using the FSFI-d we were able to confirm previous studies concerning sexual function [
20,
34,
42]: preoperatively it was, as expected, limited and normalized postoperatively after creation of a neovagina. Six and twelve months after surgery the scores lay within the normal range for the majority of patients. Concerning satisfaction patients even reached a significant higher score compared to a normal reference sample. A normal sexuality is confirmed by 40% of the MRKHS patients twelve months after surgery. All domains improve with the time from pre- to postoperatively.
In comparison with the FSFI-d total score with the cut off value by Wiegel et al. 34% of the patients indicate sexual dysfunction twelve months after surgery. It is questionable if this means a dysfunctional neovagina or exaggerated expectations especially as both samples differ in age.