Indications of Peptide Receptor Radionuclide Therapy (PRRT) in Gastroenteropancreatic and Pulmonary Neuroendocrine Tumors: An Updated Review
Abstract
1. Introduction
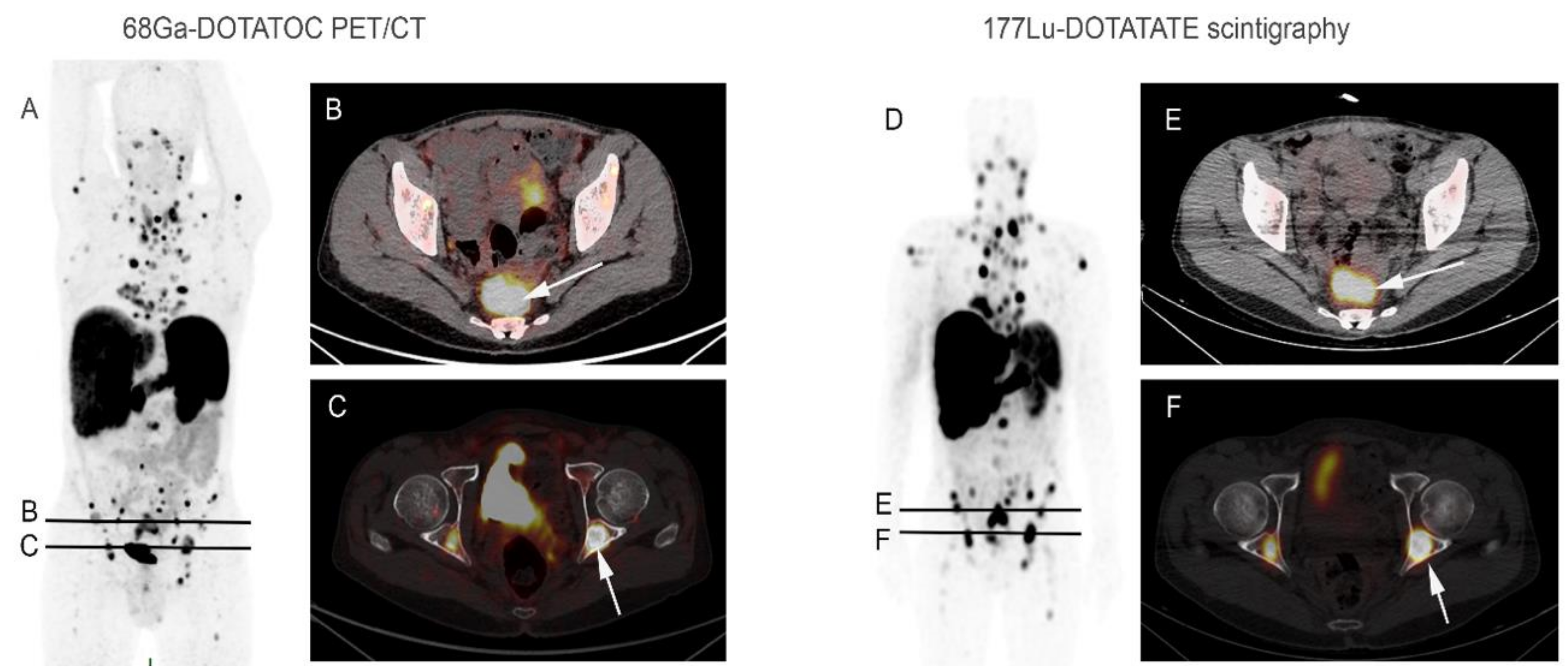
2. Somatostatin Receptors (SSTR) and Radio-Labelled Somatostatin Analogues
3. Modalities of Realization and Patients Selection
4. Indications of PRRT in NETs
4.1. Gastrointestinal NET
4.2. Pancreatic NET
| Type of Study | Reference | Total Population | panNET Subgroup | Response Criteria | CR n(%) | PR n(%) | MR n(%) | SD n(%) | PD n(%) | ORR n(%) | DCR n(%) | PFS | OS | Grade 3–4 Toxicity n(%) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Median in Months (95% CI) | ||||||||||||||
| Phase 1/2 | Bodei 2011 [11] | unresectable or metastatic tumor (n = 51) | n = 14 | RECIST modified * | 0(0) | 8(57) | 1(7) | 2(14) | 3(21) | 9(64) | 11(79) | NS | NS | HematoT: 2 (4) |
| Phase 2 | Sansovini 2013 [23] | advanced G1/G2 panNET (n = 52) | n = 52 | SWOG | 4(8) | 11(21) | N/A | 27(52) | 10(19) | 15(29) | 42(81) | 29 (19–39) | NR | 0% |
| Retrospective | Ezzedin 2014 [21] | metastatic G1/G2 panNET (n = 68) | n = 68 | RECIST v1.1 | 0(0) | 39(57) | N/A | 19(28) | 10(15) | 39(57) | 58(85) | NS | NS | HematoT: 6% NephroT: 0% |
| SWOG modified * | 0(0) | 41(60) | 8(12) | 9(13) | 10(15) | 49(72) | 58(85) | 34 (26–42) | 53 (46–60) | |||||
| baseline SD (n = 22) | NS | NS | NS | NS | NS | NS | 19(86) | NS | 48 (43–52) | |||||
| baseline PD (n = 46) | NS | NS | NS | NS | NS | NS | 39(85) | NS | 54 (46–61) | |||||
| Non functional (n = 50) | NS | NS | NS | NS | NS | NS | 44(88) | NS | 63 (48–78) | |||||
| Functional (n = 18) | NS | NS | NS | NS | NS | NS | 14(78) | NS | 45 (37–53) | |||||
| Retrospective | Ezziddin 2014 [6] | G1/G2 GEP NET (n = 74) | n = 33 | SWOG modified * | 0(0) | 18(55) | 6(18) | 6(18) | 3(9) | 24(77) | 30(91) | 25(17–33) | 57 (48–66) | NS |
| Retrospective | Brabander 2017 [10] | GEP and bronchial NET (n = 443) | n = 133 | RECIST v1.1 | 6(5) | 66(50) | N/A | 40(30) | 17(13) | 72(54) | 112 (84) | 30 | 71 | AL: 4 (0.7) MDS: 9 (1.5) NephroT: 0 |
| -baseline SD (n = 21) | 1(5) | 9(43) | N/A | 10(48) | 1(5) | 10(48) | 20(95) | 31 | NR | |||||
| -baseline PD (n = 66) | 2(3) | 36(55) | N/A | 15(23) | 10(15) | 38(58) | 53(80) | 31 | 71 | |||||
| Functional (n = 21) | 1(5) | 12(57) | N/A | 4(19) | 3(14) | 13(62) | 17(81) | 30 | NR | |||||
| Non functional (n = 112) | 5(4) | 54(48) | N/A | 36(32) | 14(13) | 59(53) | 95(85) | 30 | 69 | |||||
| Expanded access trial | Hamiditabar 2017 [12] | NET with baseline progressive disease (n = 144) | n = 48 | RECIST | 0(0) | 6(13) | N/A | 18(38) | 23(48) | 6(13) | 24(50) | NS | NS | HematoT: 16 (11) HepatoT: 3 (3) NephroT: 0 |
| Phase 2 | Sansovini 2017 [24] | unresectable or metastatic G1/G2 panNET baseline PD (n = 60) | n = 60 | SWOG | 4(7) | 14(23) | N/A | 31(52) | 11(18) | 18(30) | 49(82) | 29 (20–54) | NR | HematoT: 0 NephroT: 1.6% |
| Prospective | Garske-Roman 2018 [13] | metastatic NET (n = 200) | panNET or Duodenal NET (n = 49) | RECIST v1.1 | 1(2) | 21(43) | N/A | 24(49) | 2(4) | 22(45) | 46(94) | 27 (17–33) | 42 (31–NR) | AL: 3(1.5) HematoT: 30(15) NephroT: 1(0.5) |
| Functional panNET or Duodenal NET(n = 20) | 1(5) | 8(40) | N/A | 11(55) | 0(0) | 9(45) | 20 (100) | 24 (12–37) | 39 (24–53) | |||||
| Non functional panNET or Duodenal NET(n = 29) | 0(0) | 13(45) | N/A | 13(45) | 2(7) | 13(45) | 26(90) | 27 (14–33) | NR | |||||
| Retrospective | Demirci 2018 [9] | Unresectable or metastatic G1–G3 NET (n = 186) | n = 62 | RECIST | 3(5) | 35(56) | N/A | 5(8) | 19(31) | 38(61) | 43(69) | Mean 42 (35–49) | Mean 57 (52–62) | HematoT: 2(1) NephroT: 2(1) |
| Retrospective | Zandee 2019 [25] | Metastatic functional G1/G2 panNET (n = 34) | n = 34 | RECIST | 1(3) | 19(56) | N/A | 8(24) | 6(18) | 20(59) | 28(82) | 18 (3–36) | NR | HematoT: 15% MDS (3%) |
| Meta-analysis | Satapathy 2019 [22] | Advanced G1–G3 panNET (n = 674) | n = 674 | RECIST SWOG WHO | NS | NS | NS | NS | NS | 47% | 546 (81) | 26 (19–32) | NR | HematoT 5% (0.3–15%) NephroT 1% |
4.3. Pulmonary NET
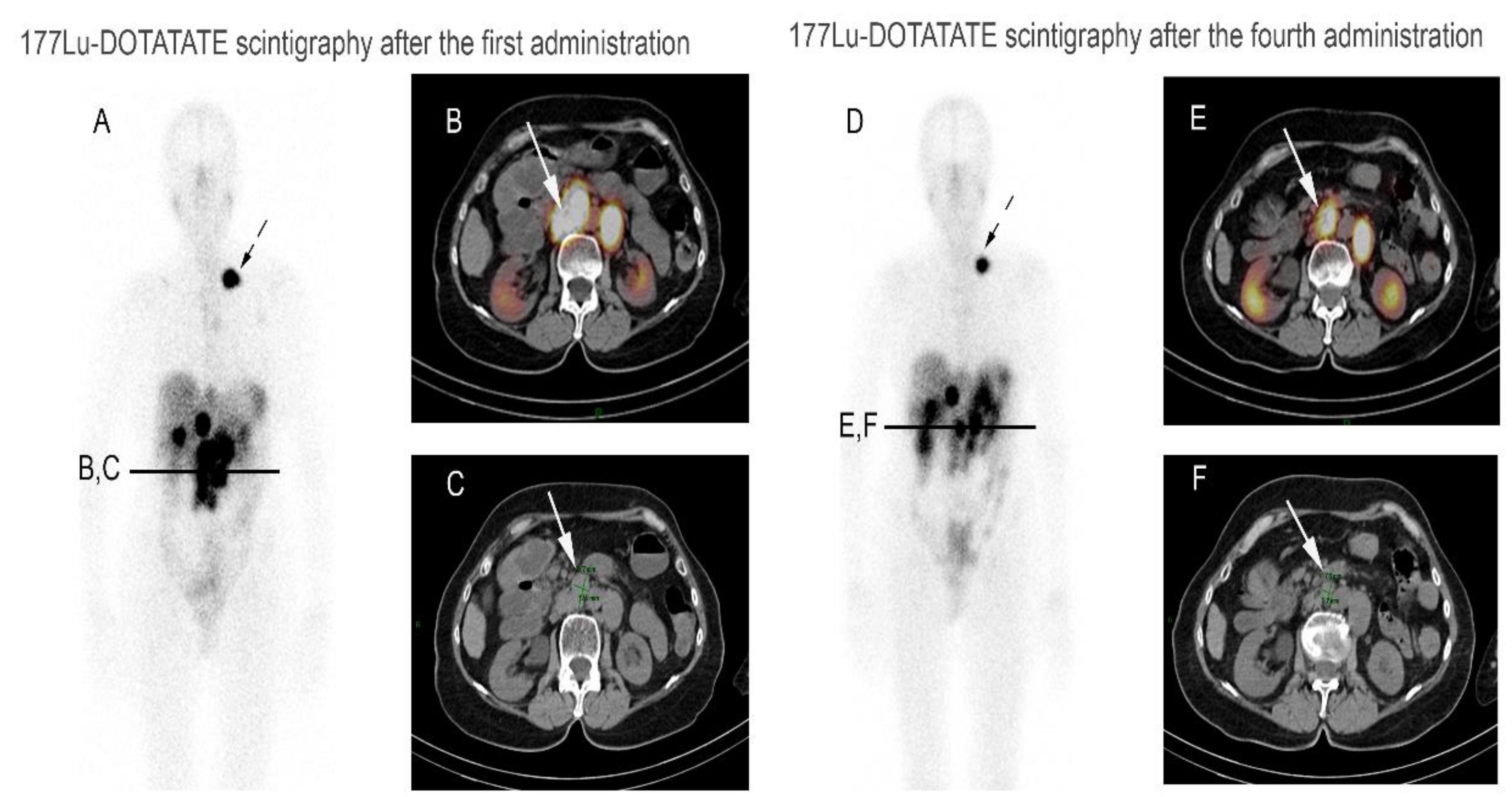
4.4. Retreatment PRRT after PRRT Failure
4.5. Side Effects of PRRT
4.5.1. Subacute Effects
4.5.2. Long-Term Effects
5. Perspectives, Ongoing Studies
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Conflicts of Interest
Abbreviations
| PRRT | Peptide Receptor Radionuclide Therapy |
| SSTR | Somatostatin Receptor |
| RECIST | Response evaluation in solid tumors |
| SUV | Standardize Uptake Value |
| LAR | Long acting release |
| NET | Neuroendocrine tumor |
| SSA | Somatostatin Analogs |
| GBq | Giga Becquerel |
References
- Dasari, A.; Shen, C.; Halperin, D.; Zhao, B.; Zhou, S.; Xu, Y.; Shih, T.; Yao, J. Trends in the incidence, prevalence, and survival outcomes in patients with neuroendocrine tumors in the United States. JAMA Oncol. 2017, 3, 1335–1342. [Google Scholar] [CrossRef] [PubMed]
- Strosberg, J.; El-Haddad, G.; Wolin, E.; Hendifar, A.; Yao, J.; Chasen, B.; Mittra, E.; Kunz, P.; Kulke, M.; Jacene, H.; et al. Phase 3 trial of (177)Lu-dotatate for midgut neuroendocrine tumors. N. Engl. J. Med. 2017, 376, 125–135. [Google Scholar] [CrossRef]
- Capello, A.; Krenning, E.P.; Breeman, W.A.P.; Bernard, B.F.; de Jong, M. Peptide receptor radionuclide therapy in vitro using [111In-DTPA0]Octreotide n.d.:8. J. Nucl. Med. 2003, 44, 98–104. [Google Scholar]
- Pool, S.E.; Krenning, E.P.; Koning, G.A.; van Eijck, C.H.J.; Teunissen, J.J.M.; Kam, B.; Valkema, R.; Kwekkeboom, D.J.; de Jong, M.; Valkema, R.; et al. Preclinical and clinical studies of peptide receptor radionuclide therapy. Semin. Nucl. Med. 2010, 40, 209–218. [Google Scholar] [CrossRef] [PubMed]
- Kratochwil, C.; Stefanova, M.; Mavriopoulou, E.; Holland-Letz, T.; Dimitrakopoulou-Strauss, A.; Afshar-Oromieh, A.; Mier, W.; Haberkorn, U.; Giesel, F.L. SUV of [68Ga]DOTATOC-PET/CT predicts response probability of PRRT in neuroendocrine tumors. Mol. Imaging Biol. 2015, 17, 313–318. [Google Scholar] [CrossRef]
- Ezziddin, S.; Attassi, M.; Yong-Hing, C.J.; Ahmadzadehfar, H.; Willinek, W.; Grunwald, F.; Guhlke, S.; Biersack, H.-J.; Sabet, A. Predictors of long-term outcome in patients with well-differentiated gastroenteropancreatic neuroendocrine tumors after peptide receptor radionuclide therapy with 177Lu-Octreotate. J. Nucl. Med. 2014, 55, 183–190. [Google Scholar] [CrossRef]
- Imhof, A.; Brunner, P.; Marincek, N.; Briel, M.; Schindler, C.; Rasch, H.; Mäcke, H.R.; Rochlitz, C.; Müller-Brand, J.; Walter, M.A. Response, survival, and long-term toxicity after therapy with the radiolabeled somatostatin analogue [ 90 Y-DOTA]-TOC in metastasized neuroendocrine cancers. J. Clin. Oncol. 2011, 29, 2416–2423. [Google Scholar] [CrossRef]
- Sabet, A.; Dautzenberg, K.; Haslerud, T.; Aouf, A.; Sabet, A.; Simon, B.; Mayer, K.; Biersack, H.-J.; Ezziddin, S. Specific efficacy of peptide receptor radionuclide therapy with 177Lu-octreotate in advanced neuroendocrine tumours of the small intestine. Eur. J. Nucl. Med. Mol. Imaging 2015, 42, 1238–1246. [Google Scholar] [CrossRef]
- Demirci, E.; Kabasakal, L.; Toklu, T.; Ocak, M.; Şahin, O.E.; Alan-Selcuk, N.; Araman, A. 177Lu-DOTATATE therapy in patients with neuroendocrine tumours including high-grade (WHO G3) neuroendocrine tumours: Response to treatment and long-term survival update. Nucl. Med. Commun. 2018, 39, 789–796. [Google Scholar] [CrossRef]
- Brabander, T.; van der Zwan, W.A.; Teunissen, J.J.M.; Kam, B.L.R.; Feelders, R.A.; de Herder, W.W.; van Eijck, C.H.J.; Franssen, G.J.H.; Krenning, E.P.; Kwekkeboom, D.J. Long-term efficacy, survival, and safety of [ 177 Lu-DOTA 0,Tyr 3 ]octreotate in patients with gastroenteropancreatic and bronchial neuroendocrine tumors. Clin. Cancer Res. 2017, 23, 4617–4624. [Google Scholar] [CrossRef] [PubMed]
- Bodei, L.; Cremonesi, M.; Grana, C.M.; Fazio, N.; Iodice, S.; Baio, S.M.; Bartolomei, M.; Lombardo, D.; Ferrari, M.E.; Sansovini, M.; et al. Peptide receptor radionuclide therapy with 177Lu-DOTATATE: The IEO phase I-II study. Eur. J. Nucl. Med. Mol. Imaging 2011, 38, 2125–2135. [Google Scholar] [CrossRef] [PubMed]
- Hamiditabar, M.; Ali, M.; Roys, J.; Wolin, E.M.; OʼDorisio, T.M.; Ranganathan, D.; Tworowska, I.; Strosberg, J.R.; Delpassand, E.S. Peptide Receptor radionuclide therapy with 177LU-octreotate in patients with somatostatin receptor expressing neuroendocrine tumors: Six yearsʼ assessment. Clin. Nucl. Med. 2017, 42, 436–443. [Google Scholar] [CrossRef]
- Garske-Román, U.; Sandström, M.; Fröss Baron, K.; Lundin, L.; Hellman, P.; Welin, S.; Johansson, S.; Khan, T.; Lundqvist, H.; Eriksson, B.; et al. Prospective observational study of 177Lu-DOTA-octreotate therapy in 200 patients with advanced metastasized neuroendocrine tumours (NETs): Feasibility and impact of a dosimetry-guided study protocol on outcome and toxicity. Eur. J. Nucl. Med. Mol. Imaging 2018, 45, 970–988. [Google Scholar] [CrossRef] [PubMed]
- Yalchin, M.; Oliveira, A.; Theocharidou, E.; Pencharz, D.; Navalkissoor, S.; Quigley, A.-M.; Walker, M.; Caplin, M.; Toumpanakis, C. The impact of radiological response to peptide receptor radionuclide therapy on overall survival in patients with metastatic midgut neuroendocrine tumors. Clin. Nucl. Med. 2017, 42, e135–e141. [Google Scholar] [CrossRef] [PubMed]
- Cives, M.; Strosberg, J. Radionuclide Therapy for neuroendocrine tumors. Curr. Oncol. Rep. 2017, 19, 9. [Google Scholar] [CrossRef]
- Kim, S.-J.; Pak, K.; Koo, P.J.; Kwak, J.J.; Chang, S. The efficacy of 177Lu-labelled peptide receptor radionuclide therapy in patients with neuroendocrine tumours: A meta-analysis. Eur. J. Nucl. Med. Mol. Imaging 2015, 42, 1964–1970. [Google Scholar] [CrossRef]
- Inzani, F.; Petrone, G.; Rindi, G. The new world health organization classification for pancreatic neuroendocrine neoplasia. Endocrinol. Metab. Clin. North Am. 2018, 47, 463–470. [Google Scholar] [CrossRef]
- Zhang, J.; Kulkarni, H.R.; Singh, A.; Niepsch, K.; Müller, D.; Baum, R.P. Peptide receptor radionuclide therapy in grade 3 neuroendocrine neoplasms: Safety and survival analysis in 69 patients. J. Nucl. Med. 2019, 60, 377–385. [Google Scholar] [CrossRef]
- Carlsen, E.A.; Fazio, N.; Granberg, D.; Grozinsky-Glasberg, S.; Ahmadzadehfar, H.; Grana, C.M.; Zandee, W.T.; Cwikla, J.; Walter, M.A.; Oturai, P.S.; et al. Peptide receptor radionuclide therapy in gastroenteropancreatic NEN G3, a multicenter cohort study. Endocr. Relat. Cancer 2019, 26, 227–239. [Google Scholar] [CrossRef] [PubMed]
- Thang, S.P.; Lung, M.S.; Kong, G.; Hofman, M.S.; Callahan, J.; Michael, M.; Hicks, R.J. Peptide receptor radionuclide therapy (PRRT) in European Neuroendocrine Tumour Society (ENETS) grade 3 (G3) neuroendocrine neoplasia (NEN)-a single-institution retrospective analysis. Eur. J. Nucl. Med. Mol. Imaging 2018, 45, 262–277. [Google Scholar] [CrossRef]
- Ezziddin, S.; Khalaf, F.; Vanezi, M.; Haslerud, T.; Mayer, K.; Al Zreiqat, A.; Willinek, W.; Biersack, H.-J.; Sabet, A.; Willinek, W.; et al. Outcome of peptide receptor radionuclide therapy with 177Lu-octreotate in advanced grade 1/2 pancreatic neuroendocrine tumours. Eur. J. Nucl. Med. Mol. Imaging 2014, 41, 925–933. [Google Scholar] [CrossRef] [PubMed]
- Satapathy, S.; Mittal, B.R. 177Lu-DOTATATE peptide receptor radionuclide therapy versus Everolimus in advanced pancreatic neuroendocrine tumors: A systematic review and meta-analysis. Nucl. Med. Commun. 2019, 40, 1195–1203. [Google Scholar] [CrossRef]
- Sansovini, M.; Severi, S.; Ambrosetti, A.; Monti, M.; Nanni, O.; Sarnelli, A.; Bodei, L.; Garaboldi, L.; Bartolomei, M.; Paganelli, G. Treatment with the radiolabelled somatostatin analog 177 Lu-DOTATATE for advanced pancreatic neuroendocrine tumors. Neuroendocrinology 2013, 97, 347–354. [Google Scholar] [CrossRef] [PubMed]
- Sansovini, M.; Severi, S.; Ianniello, A.; Nicolini, S.; Fantini, L.; Mezzenga, E.; Ferroni, F.; Scarpi, E.; Monti, M.; Bongiovanni, A.; et al. Long-term follow-up and role of FDG PET in advanced pancreatic neuroendocrine patients treated with 177Lu-D OTATATE. Eur. J. Nucl. Med. Mol. Imaging 2017, 44, 490–499. [Google Scholar] [CrossRef]
- Zandee, W.T.; Brabander, T.; Blažević, A.; Kam, B.L.R.; Teunissen, J.J.M.; Feelders, R.A.; Hofland, J.; de Herder, W.W. Symptomatic and radiological response to 177Lu-DOTATATE for the treatment of functioning pancreatic neuroendocrine tumors. J. Clin. Endocrinol. Metab. 2019, 104, 1336–1344. [Google Scholar] [CrossRef]
- van Vliet, E.I.; van Eijck, C.H.; de Krijger, R.R.; van Dijkum, E.J.N.; Teunissen, J.J.; Kam, B.L.; de Herder, W.W.; Feelders, R.A.; Bonsing, B.A.; Brabander, T.; et al. Neoadjuvant treatment of nonfunctioning pancreatic neuroendocrine tumors with [177Lu-DOTA0,Tyr3]Octreotate. J. Nucl. Med. 2015, 56, 1647–1653. [Google Scholar] [CrossRef]
- Ramage, J.; Naraev, B.G.; Halfdanarson, T.R. Peptide receptor radionuclide therapy for patients with advanced pancreatic neuroendocrine tumors. Semin. Oncol. 2018, 45, 236–248. [Google Scholar] [CrossRef] [PubMed]
- Ianniello, A.; Sansovini, M.; Severi, S.; Nicolini, S.; Grana, C.M.; Massri, K.; Bongiovanni, A.; Antonuzzo, L.; Di Iorio, V.; Sarnelli, A.; et al. Peptide receptor radionuclide therapy with 177Lu-DOTATATE in advanced bronchial carcinoids: Prognostic role of thyroid transcription factor 1 and 18F-FDG PET. Eur. J. Nucl. Med. Mol. Imaging 2016, 43, 1040–1046. [Google Scholar] [CrossRef] [PubMed]
- Mariniello, A.; Bodei, L.; Tinelli, C.; Baio, S.M.; Gilardi, L.; Colandrea, M.; Papi, S.; Valmadre, G.; Fazio, N.; Galetta, D.; et al. Long-term results of PRRT in advanced bronchopulmonary carcinoid. Eur. J. Nucl. Med. Mol. Imaging 2016, 43, 441–452. [Google Scholar] [CrossRef] [PubMed]
- Diakatou, E.; Alexandraki, K.I.; Tsolakis, A.V.; Kontogeorgos, G.; Chatzellis, E.; Leonti, A.; Kaltsas, G.A. Somatostatin and dopamine receptor expression in neuroendocrine neoplasms: Correlation of immunohistochemical findings with somatostatin receptor scintigraphy visual scores. Clin. Endocrinol. 2015, 83, 420–428. [Google Scholar] [CrossRef]
- Naraev, B.G.; Ramirez, R.A.; Kendi, A.T.; Halfdanarson, T.R. Peptide receptor radionuclide therapy for patients with advanced lung carcinoids. Clin. Lung Cancer 2019, 20, e376–e392. [Google Scholar] [CrossRef] [PubMed]
- Forrer, F.; Uusijarvi, H.; Storch, D.; Maecke, H.R.; Mueller-Brand, J. Treatment with 177Lu-DOTATOC of Patients with Relapse of Neuroendocrine Tumors After Treatment with 90Y-DOTATOC n.d.:8. J. Nucl. Med. 2005, 46, 1310–1316. [Google Scholar] [PubMed]
- Severi, S.; Sansovini, M.; Ianniello, A.; Bodei, L.; Nicolini, S.; Ibrahim, T.; Di Iorio, V.; D’Errico, V.; Caroli, P.; Monti, M.; et al. Feasibility and utility of re-treatment with 177Lu-DOTATATE in GEP-NENs relapsed after treatment with 90Y-DOTATOC. Eur. J. Nucl. Med. Mol. Imaging 2015, 42, 1955–1963. [Google Scholar] [CrossRef] [PubMed]
- de Keizer, B.; van Aken, M.O.; Feelders, R.A.; de Herder, W.W.; Kam, B.L.R.; van Essen, M.; Krenning, E.P.; Kwekkeboom, D.J. Hormonal crises following receptor radionuclide therapy with the radiolabeled somatostatin analogue [177Lu-DOTA0,Tyr3]octreotate. Eur. J. Nucl. Med. Mol. Imaging 2008, 35, 749–755. [Google Scholar] [CrossRef]
- Bodei, L.; Kwekkeboom, D.J.; Kidd, M.; Modlin, I.M.; Krenning, E.P. Radiolabeled somatostatin analogue therapy of gastroenteropancreatic cancer. Semin. Nucl. Med. 2016, 46, 225–238. [Google Scholar] [CrossRef] [PubMed]
- Sabet, A.; Khalaf, F.; Yong-Hing, C.J.; Sabet, A.; Haslerud, T.; Ahmadzadehfar, H.; Guhlke, S.; Grünwald, F.; Biersack, H.-J.; Ezziddin, S. Can peptide receptor radionuclide therapy be safely applied in florid bone metastases? Nuklearmedizin 2014, 53, 54–59. [Google Scholar] [CrossRef]
- Bodei, L.; Kidd, M.; Paganelli, G.; Grana, C.M.; Drozdov, I.; Cremonesi, M.; Lepensky, C.; Kwekkeboom, D.J.; Baum, R.P.; Krenning, E.P.; et al. Long-term tolerability of PRRT in 807 patients with neuroendocrine tumours: The value and limitations of clinical factors. Eur. J. Nucl. Med. Mol. Imaging 2015, 42, 5–19. [Google Scholar] [CrossRef] [PubMed]
- Kwekkeboom, D.J.; de Herder, W.W.; Kam, B.L.; van Eijck, C.H.; van Essen, M.; Kooij, P.P.; Feelders, R.A.; van Aken, M.O.; Krenning, E.P. Treatment with the radiolabeled somatostatin analog [177Lu-DOTA0,Tyr3]Octreotate: Toxicity, efficacy, and survival. J. Clin. Oncol. 2008, 26, 2124–2130. [Google Scholar] [CrossRef]
- Brieau, B.; Hentic, O.; Lebtahi, R.; Palazzo, M.; Ben Reguiga, M.; Rebours, V.; Maire, F.; Hammel, P.; Ruszniewski, P.; Fenaux, P. High risk of myelodysplastic syndrome and acute myeloid leukemia after 177Lu-octreotate PRRT in NET patients heavily pretreated with alkylating chemotherapy. Endocr. Relat. Cancer 2016, 23, L17–L23. [Google Scholar] [CrossRef][Green Version]
- Bodei, L.; Schöder, H.; Baum, R.P.; Herrmann, K.; Strosberg, J.; Caplin, M.; Öberg, K.; Modlin, I.M. Molecular profiling of neuroendocrine tumours to predict response and toxicity to peptide receptor radionuclide therapy. Lancet Oncol. 2020, 21, e431–e443. [Google Scholar] [CrossRef]
- Roussy, G.; Cancer Campus; Grand Paris. Antitumor Efficacy of Peptide Receptor Radionuclide Therapy with 177Lutetium -Octreotate Randomized vs Sunitinib in Unresectable Progressive Well-Differentiated Neuroendocrine Pancreatic Tumor: First Randomized Phase II. 2018. Available online: clinicaltrials.gov (accessed on 23 July 2018).
- Advanced Accelerator Applications. A Phase III Multi-Center, Randomized, Open-label Study to Evaluate the Efficacy and Safety of Lutathera in Patients with Grade 2 and Grade 3 Advanced GEP-NET. 2020. Available online: clinicaltrials.gov (accessed on 19 December 2020).
- Nicolini, S.; Bodei, L.; Bongiovanni, A.; Sansovini, M.; Grassi, I.; Ibrahim, T.; Monti, M.; Caroli, P.; Sarnelli, A.; Diano, D.; et al. Combined use of 177Lu-DOTATATE and metronomic capecitabine (Lu-X) in FDG-positive gastro-entero-pancreatic neuroendocrine tumors. Eur. J. Nucl. Med. Mol. Imaging 2021. [Google Scholar] [CrossRef] [PubMed]
- Memorial Sloan Kettering Cancer Center. A Pilot Study Investigating Intrahepatic Arterial and Intravenous Infusion of the Radiolabeled Somatostatin Agonist 177Lu-DOTATATE in Patients with Liver-Dominant Metastatic Pancreatic Neuroendocrine Tumors. 2020. Available online: clinicaltrials.gov (accessed on 17 March 2021).
- Singh, S.; Bergsland, E.K.; Card, C.M.; Hope, T.A.; Kunz, P.L.; Laidley, D.T.; Lawrence, B.; Leyden, S.; Metz, D.C.; Michael, M.; et al. Commonwealth neuroendocrine tumour research collaboration and the north american neuroendocrine tumor society guidelines for the diagnosis and management of patients with lung neuroendocrine tumors: An international collaborative endorsement and update of the 2015 European Neuroendocrine tumor society expert consensus guidelines. J. Thorac. Oncol. 2020, 15, 1577–1598. [Google Scholar] [CrossRef] [PubMed]
| Type of Study | Reference | Total Population | Midgut NET Subgroup | Response Criteria | CR n(%) | PR n (%) | MR n(%) | SD n(%) | PD n(%) | ORR n(%) | DCR n(%) | PFS | OS | Grade 3–4 Toxicity n(%) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Median in Months (95% CI) | ||||||||||||||
| Phase 1/2 | Bodei 2011 [11] | unresectable or metastatic tumor (n = 51) | n = 19 | RECIST modified * | 0(0) | 2(10) | 6(32) | 7(37) | 4(21) | 2(11) | 15(80) | NS | NS | HematoT: 2(4) |
| Retrospective | Sabet 2015 [8] | Unresectable, metastatic G1/G2 midgut NET (n = 61) | n = 61 | SWOG modified * RECIST v1.1 | 0(0) | 8 (13) | 19 (31) | 29(48) | 5(8) | 8(13) | 56(92) | 33(25–41) | 61 (N/A) | HematoT: 5(8) NephroT: 0(0) |
| Phase 3 | Strosberg 2017 [2] | Unresectable or metastatic G1/G2 midgut NET progressive under octreotide LAR (n = 229) | n = 201 evaluable for objective response | RECIST v1.1 | 1(1) | 17 (17) | N/A | 60(60) | 23(23) | 18(18) | 78(78) | 65(50–77) ** | NS | HematoT: 11(5) NephroT: 0(0) |
| Expanded access trial | Hamiditabar 2017 [12] | NET with baseline progressive disease (n = 144) | n = 53 | RECIST | 0(0) | 2 (4) | N/A | 32(60) | 19(36) | 2(4) | 34(64) | NS | NS | HematoT: 16 (11) HepatoT: 3(3) NephroT: 0(0) |
| Retrospective | Brabander 2017 [10] | GEP and bronchial NET (n = 443) | n = 181 | RECIST v1.1 | 2(1) | 55 (30) | N/A | 99(55) | 16(9) | 57(31) | 156(86) | 30 | 60 | AL: 4(0.7) MDS: 9(1.5) NephroT: 0(0) |
| with baseline SD (n = 32) | 0(0) | 10 (31) | N/A | 18(56) | 3(9) | 10(31) | 28(87) | 24 | 82 | |||||
| with baseline PD (n = 94) | 1(1) | 28 (30) | N/A | 50(53) | 9(10) | 29(31) | 79(84) | 29 | 50 | |||||
| Retrospective | Yalchin 2017 [14] | metastatic midgut NET (n = 133) *** | n = 133 | RECIST v1.1 | 0(0) | 12 (9) | N/A | 67(50) | 54(41) | 12(9) | 79(59) | 29 | 34 | NS |
| Prospective | Garske Roman 2018 [13] | metastatic NET (n = 200) | n = 108 | RECIST v1.1 | 0(0) | 13 (12) | N/A | 87(79) | 2(2) | 13(12) | 100(91) | 29(23–35) | 48(40–60) | AL: 3(1.5) HematoT: 30(15) NephroT:1(0.5) |
| Retrospective | Demirci 2018 [9] | Unresectable or metastatic G1–G3 NET (n = 186) | n = 42 | RECIST | 2(5) | 17 (41) | N/A | 15(37) | 7(17) | 19(46) | 34(83) | 38(31-44) | 57(54-61) | HematoT: 2(1) NephroT: 2(1) |
| Type of Study | Reference | Total Population | Bronchial NET Subgroup | Response Criteria | CR n(%) | PR n(%) | MR n(%) | SD n(%) | PD n(%) | ORR n(%) | DCR n(%) | PFS | OS | Grade 3–4 Toxicity n(%) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Median in Months (95% CI) | ||||||||||||||
| Phase 1/2 | Bodei 2011 [11] | unresectable or metastatic tumor (n = 51) | n = 5 | RECIST modified * | 0(0) | 2(40) | 2(40) | 1(20) | 0(0) | 2(40) | 5(100) | NS | NS | HematoT: 2(4) |
| Phase 2 | Ianniello 2016 [28] | unresectable or metastatic bronchial carcinoids NET (n = 34) | n = 34 | SWOG | 1(3) | 4(12) | N/A | 16(47) | 13(38) | 5(15) | 21(62) | 19 (13–26) | 49 (26–69) | HematoT: 0(0) NephroT: 0(0) |
| Retrospective | Mariniello 2016 [29] | unresectable or metastatic bronchopulminar carcinoid NET (n = 114) | n = 114 | RECIST modified * | 0(0) | 15(13) | 15(13) | 46(41) | 38(33) | 30(26) | 76(67) | 28 (15–45) | 59 (32–92) | HematoT: 7(6) NephroT: 0(0) |
| Expanded access trial | Hamiditabar 2017 [12] | baseline progressive disease (n = 144) | n = 14 | RECIST | 0(0) | 2(14) | N/A | 6(43) | 5(36) | 2(14) | 8(60) | NS | NS | HematoT: 16(13) HepatoT: 3(3) NephroT: 0(0) |
| Retrospective | Brabander 2017 [10] | GEP and bronchial NET (n = 443) | n = 23 | RECIST v1.1 | 0(0) | 7(30) | N/A | 7(30) | 6(26) | 7(30) | 14(61) | 20 | 52 | AL: 4(0.7) MDS: 9(2) NephroT: 0(0) |
| Prospective | Garske Roman 2018 [13] | Metastatic NET (n = 200) | n = 6 | RECIST v1.1 | 0(0) | 1(17) | N/A | 5(83) | 0(0) | 1(17) | 6(100) | 18 (12–43) | NR (19–NR) | AL: 3(1.5) HematoT: 30(15) NephroT:1(0.5) |
| Retrospective | Demirci 2018 [9] | Unresectable or metastatic G1-G3 NET (n = 186) | n = 22 | RECIST | 0(0) | 9(41) | N/A | 4(18) | 9(41) | 9(41) | 13(59) | 32 (24–40) | 44 (37–52) | HematoT: 2(1) NephroT: 2(1) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Camus, B.; Cottereau, A.-S.; Palmieri, L.-J.; Dermine, S.; Tenenbaum, F.; Brezault, C.; Coriat, R. Indications of Peptide Receptor Radionuclide Therapy (PRRT) in Gastroenteropancreatic and Pulmonary Neuroendocrine Tumors: An Updated Review. J. Clin. Med. 2021, 10, 1267. https://doi.org/10.3390/jcm10061267
Camus B, Cottereau A-S, Palmieri L-J, Dermine S, Tenenbaum F, Brezault C, Coriat R. Indications of Peptide Receptor Radionuclide Therapy (PRRT) in Gastroenteropancreatic and Pulmonary Neuroendocrine Tumors: An Updated Review. Journal of Clinical Medicine. 2021; 10(6):1267. https://doi.org/10.3390/jcm10061267
Chicago/Turabian StyleCamus, Baptiste, Anne-Ségolène Cottereau, Lola-Jade Palmieri, Solène Dermine, Florence Tenenbaum, Catherine Brezault, and Romain Coriat. 2021. "Indications of Peptide Receptor Radionuclide Therapy (PRRT) in Gastroenteropancreatic and Pulmonary Neuroendocrine Tumors: An Updated Review" Journal of Clinical Medicine 10, no. 6: 1267. https://doi.org/10.3390/jcm10061267
APA StyleCamus, B., Cottereau, A.-S., Palmieri, L.-J., Dermine, S., Tenenbaum, F., Brezault, C., & Coriat, R. (2021). Indications of Peptide Receptor Radionuclide Therapy (PRRT) in Gastroenteropancreatic and Pulmonary Neuroendocrine Tumors: An Updated Review. Journal of Clinical Medicine, 10(6), 1267. https://doi.org/10.3390/jcm10061267






