Comparing Intensive Trauma-Focused Treatment Outcome on PTSD Symptom Severity in Older and Younger Adults
Abstract
1. Introduction
2. Materials and Methods
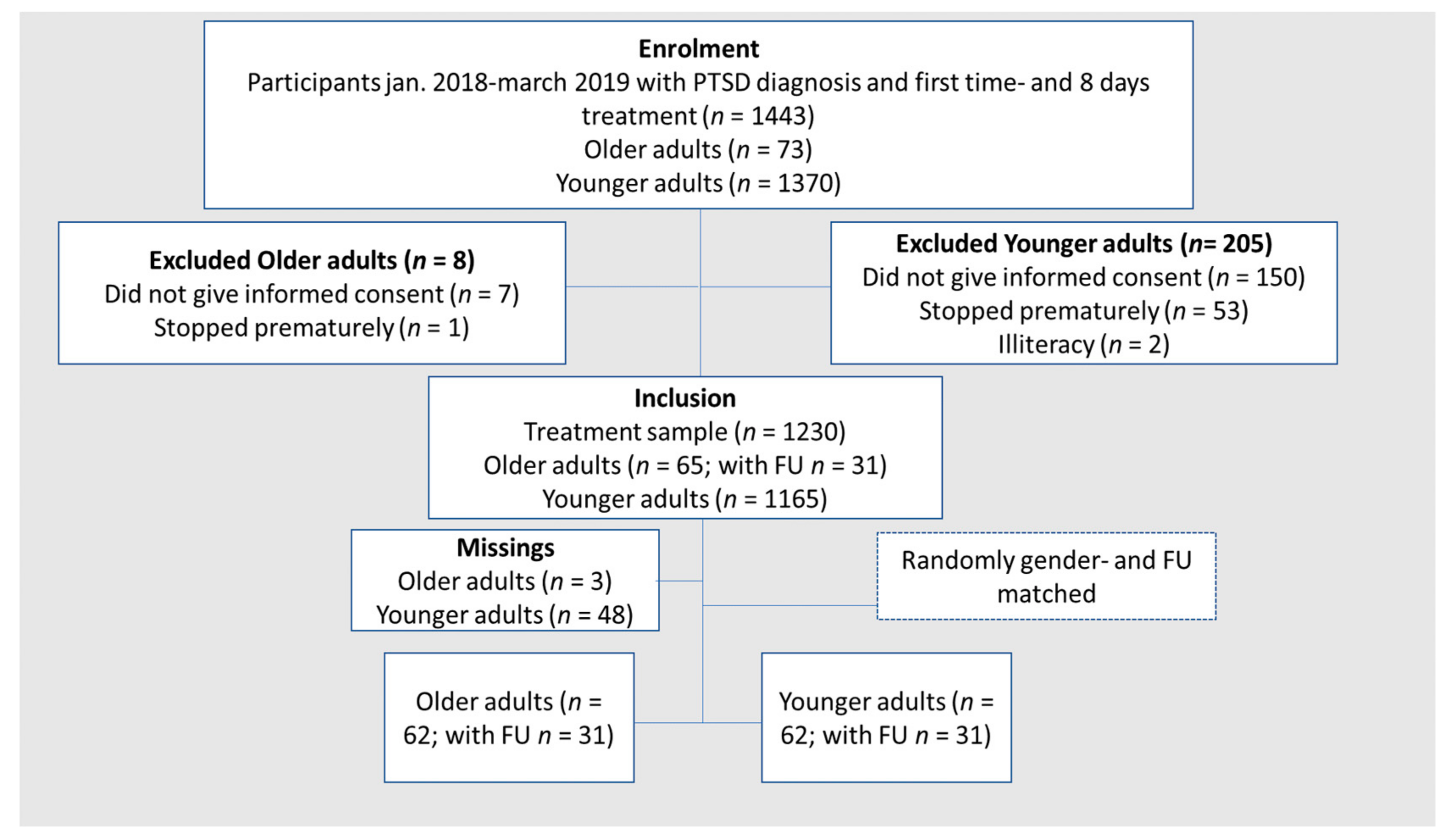
2.1. Participants
2.2. Procedure
2.3. Therapies
2.4. Measures
2.5. Data Analysis
3. Results
3.1. Baseline Sample Characteristics
3.2. Treatment Effect from Pre- to Post-Treatment for the Total Group (n = 124)
3.3. Treatment Effect at Six-Month Follow-Up for a Subsample (n = 62)
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Pietrzak, R.H.; Goldstein, R.B.; Southwick, S.M.; Grant, B.F. Prevalence and axis i comorbidity of full and partial post-traumatic stress disorder in the united states: Results from wave 2 of the national epidemiologic survey on alcohol and related conditions. J. Anxiety Disord. 2011, 25, 456–465. [Google Scholar] [CrossRef]
- Chopra, M.P.; Zhang, H.; Pless Kaiser, A.; Moye, J.A.; Llorente, M.D.; Oslin, D.W.; Spiro, A., 3rd. PTSD is a chronic, fluctuating disorder affecting the mental quality of life in older adults. Am. J. Geriatr. Psychiatry 2014, 22, 86–97. [Google Scholar] [CrossRef]
- van Zelst, W.H.; de Beurs, E.; Beekman, A.T.; van Dyck, R.; Deeg, D.D. Well-being, physical functioning, and use of health services in the elderly with PTSD and subthreshold PTSD. Int. J. Geriatr. Psychiatry 2006, 21, 180–188. [Google Scholar] [CrossRef]
- Kang, B.; Xu, H.; McConnell, E.S. Neurocognitive and psychiatric comorbidities of post-traumatic stress disorder among older veterans: A systematic review. Int. J. Geriatr. Psychiatry 2019, 34, 522–538. [Google Scholar] [CrossRef]
- Lohr, J.B.; Palmer, B.W.; Eidt, C.A.; Aailaboyina, S.; Mausbach, B.T.; Wolkowitz, O.M.; Thorp, S.R.; Jeste, D.V. Is post-traumatic stress disorder associated with premature senescence? A review of the literature. Am. J. Geriatr. Psychiatry 2015, 23, 709–725. [Google Scholar] [CrossRef]
- Dinnen, S.; Simiola, V.; Cook, J.M. Post-traumatic stress disorder in older adults: A systematic review of the psychotherapy treatment literature. Aging Ment. Health 2015, 19, 144–150. [Google Scholar] [CrossRef]
- Pless Kaiser, A.; Cook, J.M.; Glick, D.M.; Moye, J. Posttraumatic stress disorder in older adults: A conceptual review. Clin. Gerontol. 2019, 42, 359–376. [Google Scholar] [CrossRef] [PubMed]
- Kessler, E.M.; Blachetta, C. Age cues in patients’ descriptions influence treatment attitudes. Aging Ment. Health 2020, 24, 193–196. [Google Scholar] [CrossRef] [PubMed]
- Mody, L.; Miller, D.K.; McGloin, J.M.; Freeman, M.; Marcantonio, E.R.; Magaziner, J.; Studenski, S. Recruitment and retention of older adults in aging research. J. Am. Geriatr. Soc. 2008, 56, 2340–2348. [Google Scholar] [CrossRef] [PubMed]
- Thorp, S.R.; Glassman, L.H.; Wells, S.Y.; Walter, K.H.; Gebhardt, H.; Twamley, E.; Golshan, S.; Pittman, J.; Penski, K.; Allard, C.; et al. A randomized controlled trial of prolonged exposure therapy versus relaxation training for older veterans with military-related PTSD. J. Anxiety Disord. 2019, 64, 45–54. [Google Scholar] [CrossRef] [PubMed]
- Lely, J.C.G.; Knipscheer, J.W.; Moerbeek, M.; Ter Heide, F.J.J.; van den Bout, J.; Kleber, R.J. Randomised controlled trial comparing narrative exposure therapy with present-centred therapy for older patients with post-traumatic stress disorder. Br. J. Psychiatry 2019, 214, 369–377. [Google Scholar] [CrossRef]
- Bichescu, D.; Neuner, F.; Schauer, M.; Elbert, T. Narrative exposure therapy for political imprisonment-related chronic posttraumatic stress disorder and depression. Behav. Res. Ther. 2007, 45, 2212–2220. [Google Scholar] [CrossRef] [PubMed]
- Knaevelsrud, C.; Böttche, M.; Pietrzak, R.H.; Freyberger, H.J.; Kuwert, P. Efficacy and feasibility of a therapist-guided internet-based intervention for older persons with childhood traumatization: A randomized controlled trial. Am. J. Geriatr. Psychiatry 2017, 25, 878–888. [Google Scholar] [CrossRef]
- Kline, A.C.; Cooper, A.A.; Rytwinski, N.K.; Feeny, N.C. The effect of concurrent depression on ptsd outcomes in trauma-focused psychotherapy: A meta-analysis of randomized controlled trials. Behav. Ther. 2021, 52, 250–266. [Google Scholar] [CrossRef]
- Chard, K.M.; Schumm, J.A.; Owens, G.P.; Cottingham, S.M. A comparison of OEF and OIF veterans and Vietnam veterans receiving cognitive processing therapy. J. Trauma. Stress 2010, 23, 25–32. [Google Scholar] [CrossRef]
- Sabey, A.K.; Jensen, J.; Major, S.; Zinbarg, R.; Pinsof, W. Are older adults unique? Examining presenting issues and changes in therapy across the life span. J. Appl. Gerontol. 2020, 39, 250–258. [Google Scholar] [CrossRef] [PubMed]
- Cuijpers, P.; Karyotaki, E.; Eckshtain, D.; Ng, M.Y.; Corteselli, K.A.; Noma, H.; Quero, S.; Weisz, J.R. Psychotherapy for depression across different age groups: A systematic review and meta-analysis. JAMA Psychiatry 2020, 77, 694–702. [Google Scholar] [CrossRef] [PubMed]
- Kishita, N.; Laidlaw, K. Cognitive behaviour therapy for generalized anxiety disorder: Is CBT equally efficacious in adults of working age and older adults? Clin. Psychol. Rev. 2017, 52, 124–136. [Google Scholar] [CrossRef]
- Gutner, C.A.; Suvak, M.K.; Sloan, D.M.; Resick, P.A. Does timing matter? Examining the impact of session timing on outcome. J. Consult. Clin. Psychol. 2016, 84, 1108–1115. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.W.; Taylor, G.; Drummond, P. The active ingredient in EMDR; is it traditional exposure or dual focus of attention? Clin. Psychol. Psychother. 2006, 13, 97–107. [Google Scholar] [CrossRef]
- Rosenbaum, S.; Vancampfort, D.; Steel, Z.; Newby, J.; Ward, P.B.; Stubbs, B. Physical activity in the treatment of Post-traumatic stress disorder: A systematic review and meta-analysis. Psychiatry Res. 2015, 230, 130–136. [Google Scholar] [CrossRef]
- Wagenmans, A.; Van Minnen, A.; Sleijpen, M.; De Jongh, A. The impact of childhood sexual abuse on the outcome of intensive trauma-focused treatment for PTSD. Eur. J. Psychotraumatol. 2018, 9, 1430962. [Google Scholar] [CrossRef] [PubMed]
- Van Woudenberg, C.; Voorendonk, E.M.; Bongaerts, H.; Zoet, H.A.; Verhagen, M.; Lee, C.W.; van Minnen, A.; De Jongh, A. Effectiveness of an intensive treatment programme combining prolonged exposure and eye movement desensitization and reprocessing for severe post-traumatic stress disorder. Eur. J. Psychotraumatol. 2018, 9, 1487225. [Google Scholar] [CrossRef] [PubMed]
- Böttche, M.; Kuwert, P.; Knaevelsrud, C. Posttraumatic stress disorder in older adults: An overview of characteristics and treatment approaches. Int. J. Geriatr. Psychiatry 2012, 27, 230–239. [Google Scholar] [CrossRef] [PubMed]
- Boeschoten, M.A.; Van der Aa, N.; Bakker, A.; Ter Heide, F.J.J.; Hoofwijk, M.C.; Jongedijk, R.A.; Van Minnen, A.; Elzinga, B.M.; Olff, M. Development and evaluation of the dutch clinician-administered PTSD scale for DSM-5 (CAPS-5). Eur. J. Psychotraumatol. 2018, 9, 1546085. [Google Scholar] [CrossRef]
- Association, A.P. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Association: Washington, DC, USA, 2013. [Google Scholar]
- Olff, M. Choosing the right instruments for psychotrauma related research. Eur. J. Psychotraumatol. 2015, 6, 30585. [Google Scholar] [CrossRef]
- Arifin, W.N. Random sampling and allocation using SPSS. Educ. Med. J. 2012, 4, 1546085. [Google Scholar] [CrossRef]
- Van Minnen, A.; Hendriks, L.; Kleine, R.; Hendriks, G.J.; Verhagen, M.; De Jongh, A. Therapist rotation: A novel approach for implementation of trauma-focused treatment in post-traumatic stress disorder. Eur. J. Psychotraumatol. 2018, 9, 1492836. [Google Scholar] [CrossRef]
- Foa, E.B.; Hembree, E.A.; Rothbaum, B.O. Prolonged Exposure Therapy for PTSD: Emotional Processing of Traumatic Experiences: Therapist Guide.; Oxford University Press: New York, NY, USA, 2007. [Google Scholar]
- De Jongh, A.; Ten Broeke, E. Handboek EMDR: Een Geprotocolleerde Behandelmethode voor de Gevolgen van Psychotrauma [Handbook EMDR: A Protocolized Treatment Method for the Consequences of Psychotrauma]; Pearson Assessment and Information B.V: Amsterdam, The Netherlands, 2013. [Google Scholar]
- Shapiro, F. Eye Movement Desesitization and Reprocessing: Basic Principles, Protocols and Procedures, 2nd ed.; Guilford Press: New York, NY, USA, 2001. [Google Scholar]
- Logie, R.D.J.; De Jongh, A. The “flashforward procedure”: Confronting the catastrophe. J. EMDR Pract. Res. 2014, 8, 25–32. [Google Scholar] [CrossRef]
- Weathers, F.W.; Blake, B.D.; Schnurr, P.P.; Kaloupek, D.G.; Marx, B.P.; Keane, T.M. The Life Events Checklist for DSM-5 (LEC-5). 2013. Available online: www.ptsd.va.gov (accessed on 14 August 2013).
- Gray, M.J.; Litz, B.T.; Hsu, J.L.; Lombardo, T.W. Psychometric properties of the life events checklist. Assessment 2004, 11, 330–341. [Google Scholar] [CrossRef]
- Lecrubier, Y.; Sheehan, D.V.; Weiller, E.; Amorim, P.; Bonora, I.; Sheehan, K.H.; Dunbar, G.C. The mini international neuropsychiatric interview (MINI). A short diagnostic structured interview: Reliability and validity according to the CIDI. Eur. Psychiatry 1997, 12, 224–231. [Google Scholar] [CrossRef]
- Van Vliet, I.M.; De Beurs, E. The MINI international neuropsychiatric interview: A brief structured diagnostic psychiatric interview for DSM-IV and ICD-10 psychiatric disorders. Tijdschr. Voor Psychiatr. 2006, 49, 393–397. [Google Scholar]
- Overbeek, T.; Schruers, K.; Griez, E. MINI: Mini International Neuropsychiatric Interview, Dutch Version 5.0.0 (DSM-IV); Maastricht Univisity: Maastricht, The Netherlands, 1999; pp. 1–15. [Google Scholar]
- Weathers, F.W.; Bovin, M.J.; Lee, D.J.; Sloan, D.M.; Schnurr, P.P.; Kaloupek, D.G.; Keane, T.M.; Marx, B.P. The clinician-administered PTSD scale for DSM-5 (CAPS-5): Development and initial psychometric evaluation in military veterans. Psychol. Assess. 2018, 30, 383–395. [Google Scholar] [CrossRef]
- Nicholson, A.A.; Densmore, M.; Frewen, P.A.; Théberge, J.; Neufeld, R.W.; McKinnon, M.C.; Lanius, R.A. The dissociative subtype of posttraumatic stress disorder: Unique resting-state functional connectivity of basolateral and centromedial amygdala complexes. Neuropsychopharmacology 2015, 40, 2317–2326. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; Lawrence Erlbaum Associates Inc.: Hissdale, NJ, USA, 1998. [Google Scholar]
- Schneider, B.A.; Avivi-Reich, M.; Mozuraitis, M. A cautionary note on the use of the Analysis of Covariance (ANCOVA) in classification designs with and without within-subject factors. Front. Psychol. 2015, 6, 474. [Google Scholar] [CrossRef] [PubMed]
- Field, A. Discovering Statistics Using IBM SPSS Statistics; SAGE Publications: London, UK, 2018. [Google Scholar]
- Wetherell, J.L.; Petkus, A.J.; Thorp, S.R.; Stein, M.B.; Chavira, D.A.; Campbell-Sills, L.; Craske, M.G.; Sherbourne, C.; Bystritsky, A.; Sullivan, G.; et al. Age differences in treatment response to a collaborative care intervention for anxiety disorders. Br. J. Psychiatry 2013, 203, 65–72. [Google Scholar] [CrossRef] [PubMed]
- Labinsky, E.; Blair, W.; Yehuda, R. Longitudinal assessment of dissociation in Holocaust survivors with and without PTSD and nonexposed aged Jewish adults. Ann. N. Y. Acad. Sci. 2006, 1071, 459–462. [Google Scholar] [CrossRef] [PubMed]
- Hoeboer, C.M.; De Kleine, R.A.; Molendijk, M.L.; Schoorl, M.; Oprel, D.A.C.; Mouthaan, J.; Van der Does, W.; Van Minnen, A. Impact of dissociation on the effectiveness of psychotherapy for post-traumatic stress disorder: Meta-analysis. BJPsych Open 2020, 6, e53. [Google Scholar] [CrossRef] [PubMed]
- Mackenzie, C.S.; Reynolds, K.; Cairney, J.; Streiner, D.L.; Sareen, J. Disorder-specific mental health service use for mood and anxiety disorders: Associations with age, sex, and psychiatric comorbidity. Depress. Anxiety 2012, 29, 234–242. [Google Scholar] [CrossRef]
- Gielkens, E.M.J.; Vink, M.; Sobczak, S.; Rosowsky, E.; Van Alphen, S.P.J. EMDR in older adults with posttraumatic stress disorder. J. EMDR Pract. Res. 2018, 12, 132–141. [Google Scholar] [CrossRef]
| Study | n | Mean Age | % Female | Trauma Type | Outcome Measure | Treatment Type | Number of Sessions | Outcome/Effect Sizes Cohen’s d |
|---|---|---|---|---|---|---|---|---|
| Lely et al. [11] (2019) | 33 | 63.8 | 27.3 | Mixed | CAPS | NET vs. PCT | 11 sessions | Between group 0.44, disappears at follow up |
| Thorp et al. [10] (2019) | 87 | 66.5 | 0 | War | CAPS | PE vs. Relaxation | 12 sessions | Within group 0.89, lost at 6 months follow up |
| Knaevelsrud et al. [13] (2017) | 94 | 71.4 | 64.9 | Childhood trauma | PDS | Therapist-Guided Internet-based Intervention vs. Waiting list | 6 weeks intervention program, 11 sessions | Between group 0.42 maintained at 12 months follow-up |
| Bichescu et al. [12] (2007) | 18 | 69.4 | 5.5 | Political prisoner | CIDI | C1 NET vs. C2 psychoeducation | C1 5 sessions C2 1 session | Within group 3.15 (pre treatment-6 months follow up) |
| Total OG and YG | OG | YG | Significance Level | Effect Size | |
|---|---|---|---|---|---|
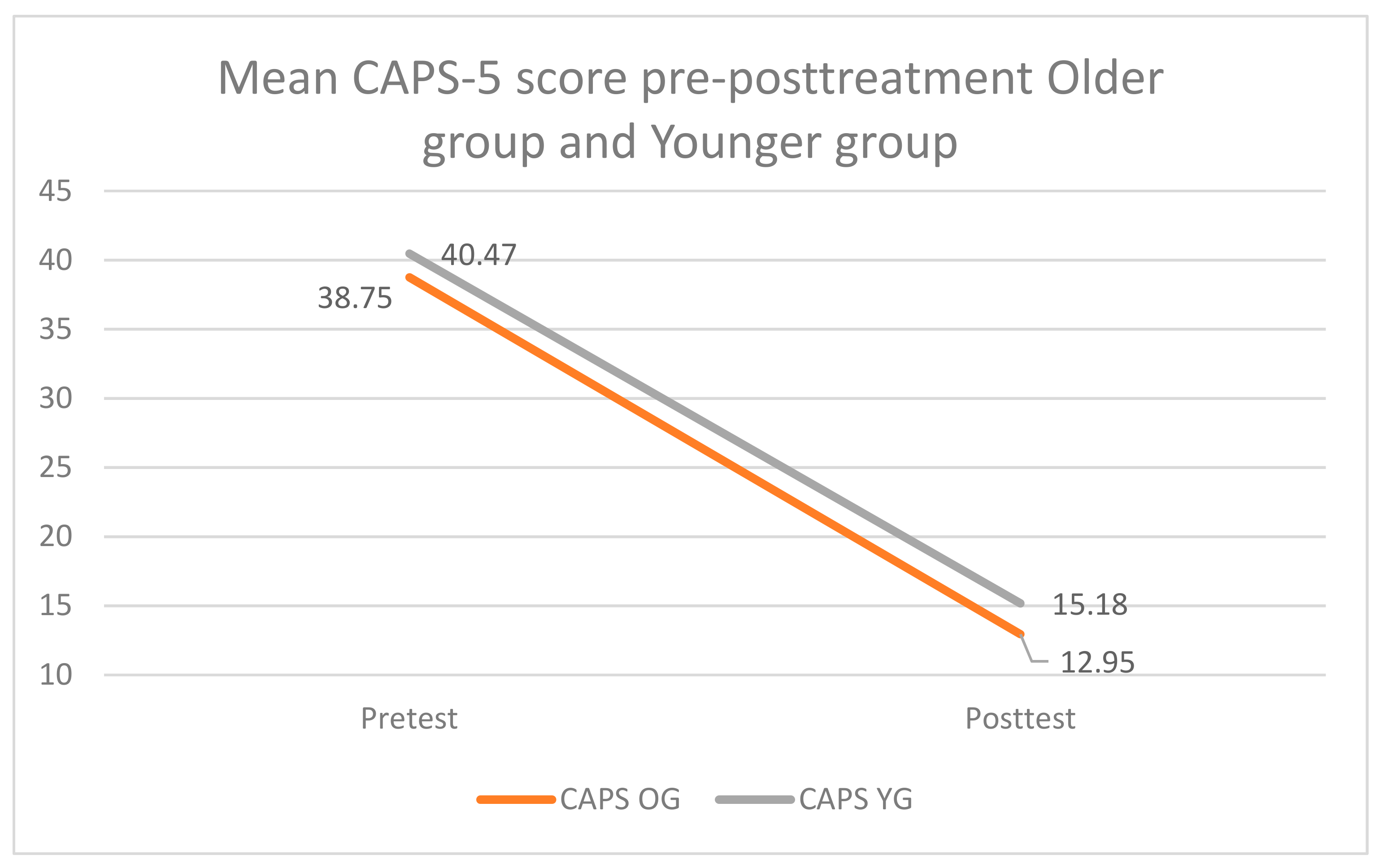
| Mean CAPS score | 39.61 (SD = 7.83) | 38.75 (SD = 8.54) | 40.47 (SD = 7.02) | p = 0.23 | d = 0.22 |
| Total comorbidity rates | 74.2% | 66.1% | 82.3% | p = 0.12 | h = 0.37 |
| 1 comorbidity | 42.7% | 37.1% | 48.4% | p = 0.20 | h = 0.22 |
| 2 or more comorbidities | 31.5% | 29% | 33.9% | p = 0.56 | h = 0.11 |
| Moderate-high suicide risk | 41.9% | 38.7% | 45.2% | p = 0.47 | h = 0.12 |
| Dissociative subtype | 30.6% | 21.0% | 40.3% | p = 0.02 | h = 0.42 |
| More than 5 traumatic experiences | 80.60% | 82.30% | 79.00% | p = 0.65 | h = 0.08 |
| More than 10 traumatic experiences | 22.60% | 22.60% | 22.60% | p > 0.99 | h = 0.00 |
| Sexual abuse | 83.10% | 87.10% | 79.00% | p = 0.23 | h = 0.21 |
| Physical | 92.70% | 90.30% | 95.20% | p = 0.30 | h = 0.19 |
| Natural disasters, accidents, and victims of war | 83.10% | 85.50% | 80.60% | p = 0.47 | h = 0.06 |
| Life-threatening illness, severe suffering, sudden death | 89.50% | 90.30% | 88.70% | p = 0.77 | h = 0.03 |
| Any other stressful event, captivity, (satanic) torture | 74.20% | 74.20% | 74.20% | p > 0.99 | h = 0.00 |
| Pre-test | Post-test | FU | ||||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | |
| CAPS OG | 40.06 | 9.88 | 15.90 | 14.26 | 16.10 | 15.28 |
| CAPS YG | 39.52 | 7.23 | 15.16 | 15.97 | 13.65 | 15.24 |
| CAPS total group | 39.79 | 8.59 | 15.53 | 15.02 | 14.87 | 15.19 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gielkens, E.M.J.; de Jongh, A.; Sobczak, S.; Rossi, G.; van Minnen, A.; Voorendonk, E.M.; Rozendaal, L.; van Alphen, S.P.J. Comparing Intensive Trauma-Focused Treatment Outcome on PTSD Symptom Severity in Older and Younger Adults. J. Clin. Med. 2021, 10, 1246. https://doi.org/10.3390/jcm10061246
Gielkens EMJ, de Jongh A, Sobczak S, Rossi G, van Minnen A, Voorendonk EM, Rozendaal L, van Alphen SPJ. Comparing Intensive Trauma-Focused Treatment Outcome on PTSD Symptom Severity in Older and Younger Adults. Journal of Clinical Medicine. 2021; 10(6):1246. https://doi.org/10.3390/jcm10061246
Chicago/Turabian StyleGielkens, Ellen M. J., Ad de Jongh, Sjacko Sobczak, Gina Rossi, Agnes van Minnen, Eline M. Voorendonk, Linda Rozendaal, and Sebastiaan P. J. van Alphen. 2021. "Comparing Intensive Trauma-Focused Treatment Outcome on PTSD Symptom Severity in Older and Younger Adults" Journal of Clinical Medicine 10, no. 6: 1246. https://doi.org/10.3390/jcm10061246
APA StyleGielkens, E. M. J., de Jongh, A., Sobczak, S., Rossi, G., van Minnen, A., Voorendonk, E. M., Rozendaal, L., & van Alphen, S. P. J. (2021). Comparing Intensive Trauma-Focused Treatment Outcome on PTSD Symptom Severity in Older and Younger Adults. Journal of Clinical Medicine, 10(6), 1246. https://doi.org/10.3390/jcm10061246






