The Sankara Nethralaya Tamil Nadu Essilor Myopia (STEM) Study—Defining a Threshold for Non-Cycloplegic Myopia Prevalence in Children
Abstract
1. Introduction
2. Materials and Methods
2.1. Vision Screening and Non-Cycloplegic Autorefraction
2.2. Cycloplegic Autorefraction
2.3. Definition of Cycloplegic Refractive Error
2.4. Statistical Analysis
3. Results
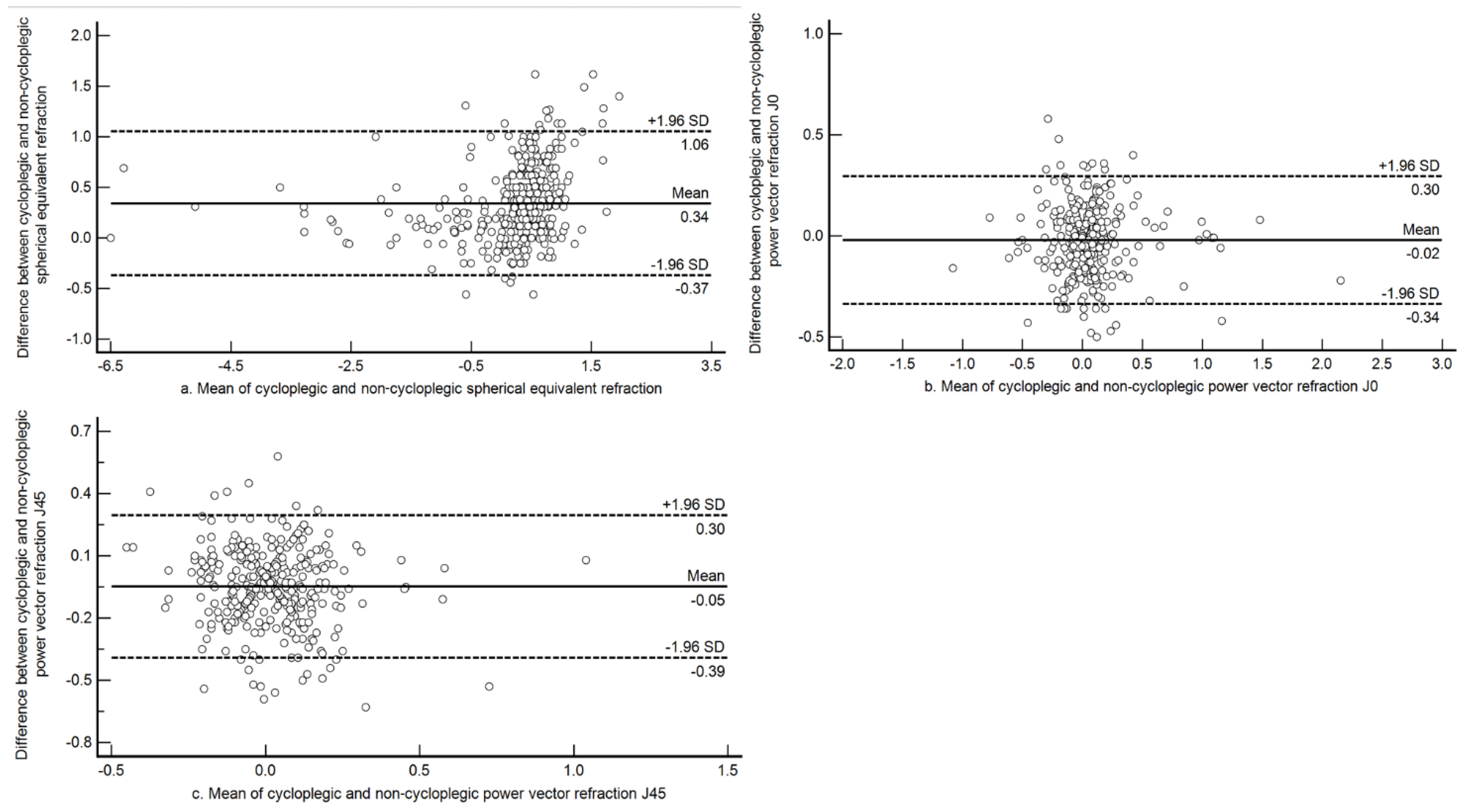
3.1. Agreement between Cycloplegic and Non-Cycloplegic Refraction in the Entire Sample
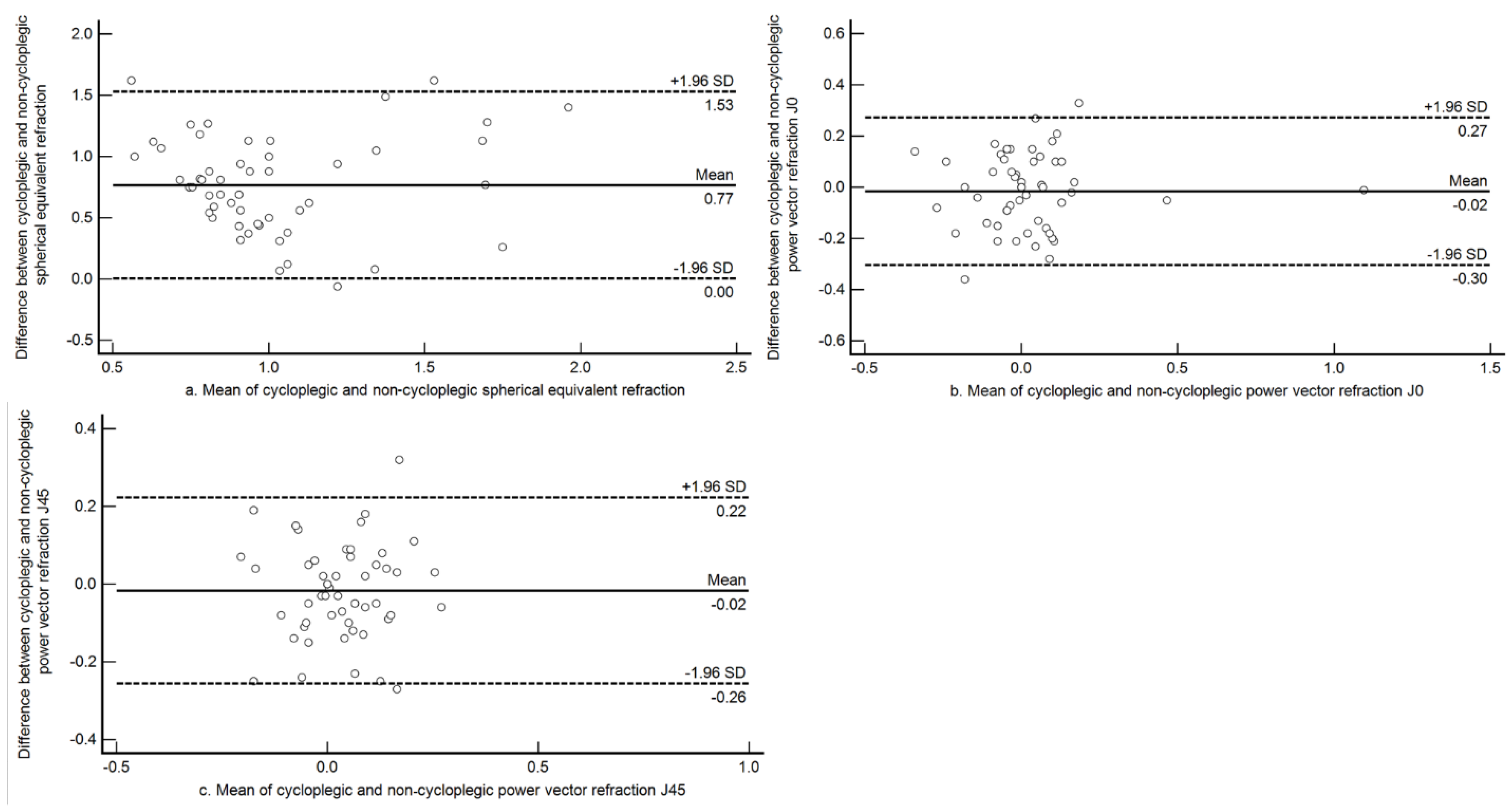
3.2. Agreement between Cycloplegic and Non-Cycloplegic Refraction among Myopes
3.3. Agreement between Cycloplegic and Non-Cycloplegic Refraction among Hyperopes:
3.4. Sensitivity and Specificity
3.5. Prevalence Estimates of Myopia with Different Thresholds of Myopia (Non-Cycloplegic) Compared to Standard Cycloplegic Refraction Threshold
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Dandona, R.; Dandona, L. Childhood blindness in India: A population based perspective. Br. J. Ophthalmol. 2003, 87, 263–265. [Google Scholar] [CrossRef]
- Naidoo, K.S.; Jaggernath, J. Uncorrected refractive errors. Indian J. Ophthalmol. 2012, 60, 432–437. [Google Scholar] [PubMed]
- Holden, B.A.; Fricke, T.R.; Wilson, D.A.; Jong, M.; Naidoo, K.S.; Sankaridurg, P.; Tien, Y.W.; Resnikoff, S. Global prevalence of myopia and high myopia and temporal trends from 2000 through 2050. J. Ophthalmol. 2016, 123, 1036–1042. [Google Scholar] [CrossRef] [PubMed]
- Flitcroft, D.I. The complex interactions of retinal, optical and environmental factors in myopia aetiology. Prog. Retin. Eye Res. 2012, 31, 622–660. [Google Scholar] [CrossRef]
- Murthy, G.V.S.; Gupta, S.K.; Ellwein, L.B.; Munoz, S.R.; Pokharel, G.P.; Sanga, L.; Bachani, D. Refractive error in children in an urban population in New Delhi. Investig. Ophthalmol. Vis. Sci. 2002, 43, 623–631. [Google Scholar]
- Dandona, R.; Dandona, L.; Srinivas, M.; Sahare, P.; Narsaiah, S.; Munoz, S.R.; Pokharel, G.P.; Ellwein, L.B. Refractive error in children in a rural population in India. Investig. Ophthalmol. Vis. Sci. 2002, 43, 615–622. [Google Scholar]
- Kalikivayi, V.; Naduvilath, T.J.; Bansal, A.K.; Dandona, L. Visual impairment in school children in Southern India. Indian J. Ophthalmol. 1997, 45, 129–134. [Google Scholar]
- Saxena, R.; Vashist, P.; Tandon, R.; Pandey, R.M.; Bharadwaj, A.; Menon, V.; Mani, K. Prevalence of myopia and its risk factors in urban school children in Delhi: The North India myopia study (NIM study). PLoS ONE 2015, 10, e0117349. [Google Scholar] [CrossRef] [PubMed]
- Sun, Y.Y.; Wei, S.F.; Li, S.M.; Hu, J.P.; Yang, X.H.; Cao, K.; Lin, C.X.; Du, J.L.; Guo, J.Y.; Li, H.; et al. Cycloplegic refraction by 1% cyclopentolate in young adults: Is it the gold standard? The Anyang University Students Eye Study (AUSES). Br. J. Ophthalmol. 2019, 103, 654. [Google Scholar] [CrossRef]
- Fotedar, R.; Rochtchina, E.; Morgan, I.; Wang, J.J.; Mitchell, P.; Rose, K.A. Necessity of Cycloplegia for Assessing Refractive Error in 12-Year-Old Children: A Population-Based Study. Am. J. Ophthalmol. 2007, 144, 307–309. [Google Scholar] [CrossRef]
- Fotouhi, A.; Morgan, I.G.; Iribarren, R.; Khabazkhoob, M.; Hashemi, H. Validity of noncycloplegic refraction in the assessment of refractive errors: The Tehran Eye Study. Acta ophthalmol. 2012, 90, 380–386. [Google Scholar] [CrossRef] [PubMed]
- Kuo, Y.C.; Wang, J.H.; Chiu, C.J. Comparison of open-field autorefraction, closed-field autorefraction, and retinoscopy for refractive measurements of children and adolescents in Taiwan. J. Formos. Med. Assoc. 2020, 119, 1251–1258. [Google Scholar] [CrossRef] [PubMed]
- Sheppard, A.L.; Davies, L.N. Clinical evaluation of the Grand Seiko Auto Ref/Keratometer WAM-5500. Ophthalmic Physiol Opt 2010, 30, 143–151. [Google Scholar] [CrossRef]
- Morgan, I.G.; Iribarren, R.; Fotouhi, A.; Grzybowski, A. Cycloplegic refraction is the gold standard for epidemiological studies. Acta ophthalmol. 2015, 93, 581–585. [Google Scholar] [CrossRef]
- Wilson, L.B.; Melia, M.; Kraker, R.T.; Vanderveen, D.K.; Huthinson, A.K.; Pineles, S.L.; Galvin, J.A.; Lambert, S.R. Accuracy of Autorefraction in Children: A Report by the American Academy of Ophthalmology. J. Ophthalmol. 2020, 127, 1259–1267. [Google Scholar]
- Khurana, R.; Tibrewal, S.; Ganesh, S.; Tarkar, R.; Nguyen, P.T.T.; Siddiqui, Z.; Dasgupta, S. Accuracy of noncycloplegic refraction performed at school screening camps. Indian J. Ophthalmol. 2018, 66, 806–811. [Google Scholar]
- Guha, S.; Shah, S.; Shah, K.; Hurakadli, P.; Majee, D.; Gandhi, S. A comparison of cycloplegic autorefraction and retinoscopy in Indian children. Clin. Exp. Optom. 2017, 100, 73–78. [Google Scholar] [CrossRef]
- Yazdani, N.; Sadeghi, R.; Momeni-Moghaddam, H.; Zarifmahmoudi, L.; Ehsaei, A. Comparison of cyclopentolate versus tropicamide cycloplegia: A systematic review and meta-analysis. J. Optom. 2018, 11, 135–143. [Google Scholar] [CrossRef]
- Wolffsohn, J.S.; Kollbaum, P.S.; Berntsen, D.A.; Atchison, D.A.; Benavente, A.; Bradley, A.; Buckhurst, H.; Collins, M.; Fujikado, T.; Hiraoka, T.; et al. IMI—Clinical Myopia Control Trials and Instrumentation Report. Investig. Ophthalmol. Vis. Sci. 2019, 60, M132–M160. [Google Scholar] [CrossRef]
- Lin, L.L.; Shih, Y.F.; Hsiao, C.K.; Chen, C.J. Prevalence of myopia in Taiwanese schoolchildren: 1983 to 2000. Ann. Acad. Med. Singap. 2004, 33, 27–33. [Google Scholar] [PubMed]
- Alrahili, N.H.R.; Jadidy, E.S.; Alahmadi, B.S.H.; Abdula’al, M.F.; Jadidy, A.S.; Alhusaini, A.A.; Mojaddidi, M.A.; Al-Barry, M.A. Prevalence of uncorrected refractive errors among children aged 3–10 years in western Saudi Arabia. Saudi Med. J. 2017, 38, 804–810. [Google Scholar] [CrossRef] [PubMed]
- Li, T.; Zhou, X.; Chen, X.; Qi, H.; Gao, Q. Refractive Error in Chinese Preschool Children: The Shanghai Study. Eye Contact Lens 2019, 45, 182–187. [Google Scholar] [CrossRef]
- Flitcroft, D.I.; He, M.; Jonas, J.B.; Jong, M.; Naidoo, K.; Ohno-Matsui, K.; Rahi, J.; Resnikoff, S.; Vitale, S.; Yannuzzi, L. IMI–Defining and classifying myopia: A proposed set of standards for clinical and epidemiologic studies. Investig. Ophthalmol. Vis. Sci. 2019, 60, M20–M30. [Google Scholar] [CrossRef]
- Raja, M.; Ramamurthy, D.; Srinivasan, K.; Varadharajan, L.S. Development of Pocket Vision Screener and its effectiveness at screening visual acuity deficits. Indian J. Ophthalmol. 2014, 62, 1152–1155. [Google Scholar] [CrossRef]
- Negrel, A.D.; Maul, E.; Pokharel, G.P.; Zhao, J.; Ellwein, L.B. Refractive error study in children: Sampling and measurement methods for a multi-country survey. Am. J. Ophthalmol. 2000, 129, 421–426. [Google Scholar] [CrossRef]
- Thibos, L.N.; Wheeler, W.; Horner, D. Power vectors: An application of Fourier analysis to the description and statistical analysis of refractive error. Optom. Vis. Sci. 1997, 74, 367–375. [Google Scholar] [CrossRef] [PubMed]
- Bland, J.M.; Altman, D.G. Measuring agreement in method comparison studies. Stat. Methods Med. Res. 1999, 8, 135–160. [Google Scholar] [CrossRef] [PubMed]
- Zhao, J.; Mao, J.; Luo, R.; Li, F.; Pokharel, G.P.; Ellwein, L.B. Accuracy of Noncycloplegic Autorefraction in School-Age Children in China. Optom. Vis. Sci. 2004, 81, 49–55. [Google Scholar] [CrossRef] [PubMed]
- Hu, Y.Y.; Wu, J.F.; Lu, T.L.; Wu, H.; Sun, W.; Wang, X.R.; Bi, H.S.; Jonas, J.B. Effect of Cycloplegia on the Refractive Status of Children: The Shandong Children Eye Study. PLoS ONE 2015, 10, e0117482. [Google Scholar] [CrossRef] [PubMed]
- Choong, Y.F.; Chen, A.H.; Goh, P.P. A comparison of autorefraction and subjective refraction with and without cycloplegia in primary school children. Am. J. Ophthalmol. 2006, 142, 68–74. [Google Scholar] [CrossRef]
- Vasudevan, B.; Ciuffreda, K.J.; Meehan, K.; Grk, D.; Cox, M. Comparison of objective refraction in darkness to cycloplegic refraction: A pilot study. Clin. Exp. Optom. 2016, 99, 168–172. [Google Scholar] [CrossRef]
- Suryakumar, R.; Bobier, W.R. The Manifestation of Noncycloplegic Refractive State in Pre-School Children is Dependent on Autorefractor Design. Optom. Vis. Sci. 2003, 80, 578–586. [Google Scholar] [CrossRef]
- Jorge, J.; Queirós, A.; Gonzalez-Meijome, J.; Fernandes, P.; Almeida, J.B.; Parafita, M.A. The influence of cycloplegia in objective refraction. Ophthalmic. Physiol. Opt. 2005, 25, 340–345. [Google Scholar] [CrossRef] [PubMed]
- Queirós, A.; González-Méijome, J.; Jorge, J. Influence of fogging lenses and cycloplegia on open-field automatic refraction. Ophthalmic Physiol Opt 2008, 28, 387–392. [Google Scholar] [CrossRef] [PubMed]
- Leone, J.F.; Mitchell, P.; Morgan, I.G.; Kifley, A.; Rose, K.A. Use of Visual Acuity to Screen for Significant Refractive Errors in Adolescents: Is It Reliable? Arch Ophthalmol. 2010, 128, 894–899. [Google Scholar] [CrossRef]
- He, X.; Zou, H.; Lu, L.; Zhao, R.; Zhao, H.; Li, Q.; Zhu, J. Axial length/corneal radius ratio: Association with refractive state and role on myopia detection combined with visual acuity in Chinese schoolchildren. PLoS ONE 2015, 10, e0111766. [Google Scholar] [CrossRef]
- Lai, Y.H.; Tseng, H.Y.; Hsu, H.T.; Chang, S.J.; Wang, H.Z. Uncorrected Visual Acuity and Noncycloplegic Autorefraction Predict Significant Refractive Errors in Taiwanese Preschool Children. J. Ophthalmol. 2013, 120, 271–276. [Google Scholar] [CrossRef] [PubMed]
- Sankaridurg, P.; He, X.; Naduvilath, T.; LV, M.; Ho, A.; Smith, E., III; Erickson, P.; Zhu, J.; Zou, H.; Xu, X. Comparison of noncycloplegic and cycloplegic autorefraction in categorizing refractive error data in children. Acta Ophthalmol. 2017, 95, e633–e640. [Google Scholar] [CrossRef] [PubMed]
- Agrawal, D.; Sahu, A.; Agrawal, D. Prevalence of ocular morbidities among school children in Raipur district, India. Indian J. Ophthalmol. 2020, 68, 340–344. [Google Scholar]
- Hashia, R.; Slathia, A. Pattern of refractive errors in primary school children in rural areas of the Jammu City of Jammu and Kashmir, India. Int. J. Sci. Stud. 2017, 5, 115–119. [Google Scholar]
- Padhye, A.S.; Khandekar, R.; Dharmadhikari, S.; Dole, K.; Gogate, P.; Deshpande, M. Prevalence of uncorrected refractive error and other eye problems among urban and rural school children. Middle East Afr. J. Ophthalmol. 2009, 16, 69–74. [Google Scholar] [PubMed]
- Saxena, R.; Vashist, P.; Menon, V. Is myopia a public health problem in India? Indian J. Community Med. 2013, 38, 83–85. [Google Scholar] [CrossRef] [PubMed]
- Narayanan, A.; Ramani, K.K. Effectiveness of interventions in improving compliance to spectacle wear and referral in school vision screening. Clin. Exp. Optom. 2018, 101, 752–757. [Google Scholar] [CrossRef] [PubMed]

| State of Refraction (n) | Mean (SD) | Range |
|---|---|---|
| Myopia (45) | −1.69 D (1.38 D) | −0.50 D to −6.50 D |
| Hyperopia (6) | +2.30 D (0.21 D) | +2.08 D to +2.66 D |
| Astigmatism (33) | −1.63 D (0.75 D) | −1.00 D to −4.17 D |
| Emmetropia (314) | +0.31 D (0.32 D) | −0.49 D to +1.99 D |
| Myopia Threshold for Non-Cycloplegic SE | Sensitivity | Specificity | Accuracy |
|---|---|---|---|
| ≤−0.50 D | 96 | 97 | 97 |
| ≤−0.75 D | 84 | 98 | 96 |
| ≤−1.00 D | 64 | 99 | 95 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gopalakrishnan, A.; Hussaindeen, J.R.; Sivaraman, V.; Swaminathan, M.; Wong, Y.L.; Armitage, J.A.; Gentle, A.; Backhouse, S. The Sankara Nethralaya Tamil Nadu Essilor Myopia (STEM) Study—Defining a Threshold for Non-Cycloplegic Myopia Prevalence in Children. J. Clin. Med. 2021, 10, 1215. https://doi.org/10.3390/jcm10061215
Gopalakrishnan A, Hussaindeen JR, Sivaraman V, Swaminathan M, Wong YL, Armitage JA, Gentle A, Backhouse S. The Sankara Nethralaya Tamil Nadu Essilor Myopia (STEM) Study—Defining a Threshold for Non-Cycloplegic Myopia Prevalence in Children. Journal of Clinical Medicine. 2021; 10(6):1215. https://doi.org/10.3390/jcm10061215
Chicago/Turabian StyleGopalakrishnan, Aparna, Jameel Rizwana Hussaindeen, Viswanathan Sivaraman, Meenakshi Swaminathan, Yee Ling Wong, James Andrew Armitage, Alex Gentle, and Simon Backhouse. 2021. "The Sankara Nethralaya Tamil Nadu Essilor Myopia (STEM) Study—Defining a Threshold for Non-Cycloplegic Myopia Prevalence in Children" Journal of Clinical Medicine 10, no. 6: 1215. https://doi.org/10.3390/jcm10061215
APA StyleGopalakrishnan, A., Hussaindeen, J. R., Sivaraman, V., Swaminathan, M., Wong, Y. L., Armitage, J. A., Gentle, A., & Backhouse, S. (2021). The Sankara Nethralaya Tamil Nadu Essilor Myopia (STEM) Study—Defining a Threshold for Non-Cycloplegic Myopia Prevalence in Children. Journal of Clinical Medicine, 10(6), 1215. https://doi.org/10.3390/jcm10061215







