Does Dynamic Anterior Plate Fixation Provide Adequate Stability for Traumatic Subaxial Cervical Spine Fractures at Mid-Term Follow-Up?
Abstract
1. Introduction
2. Materials and Methods
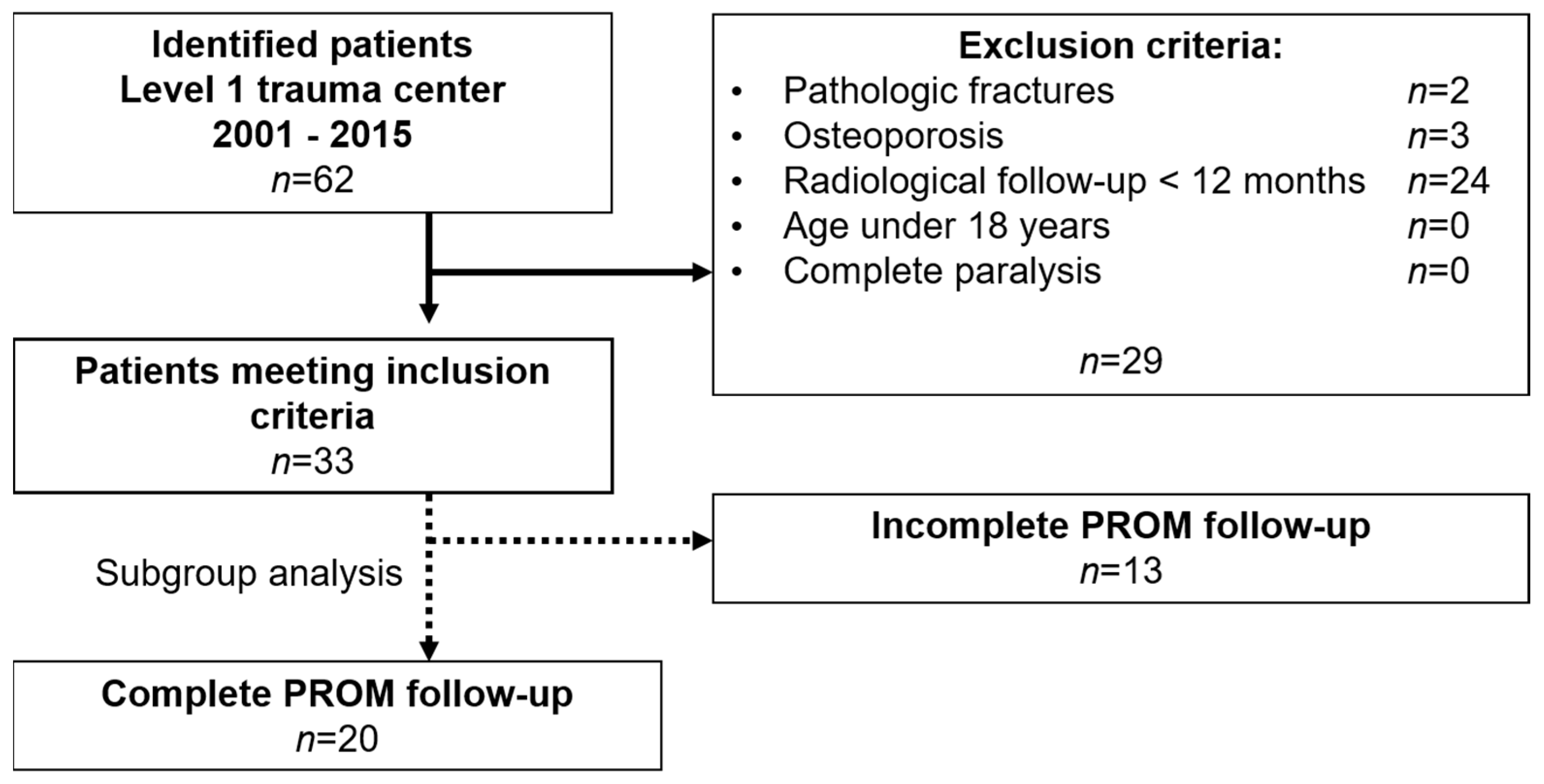
2.1. Inclusion and Exclusion Criteria
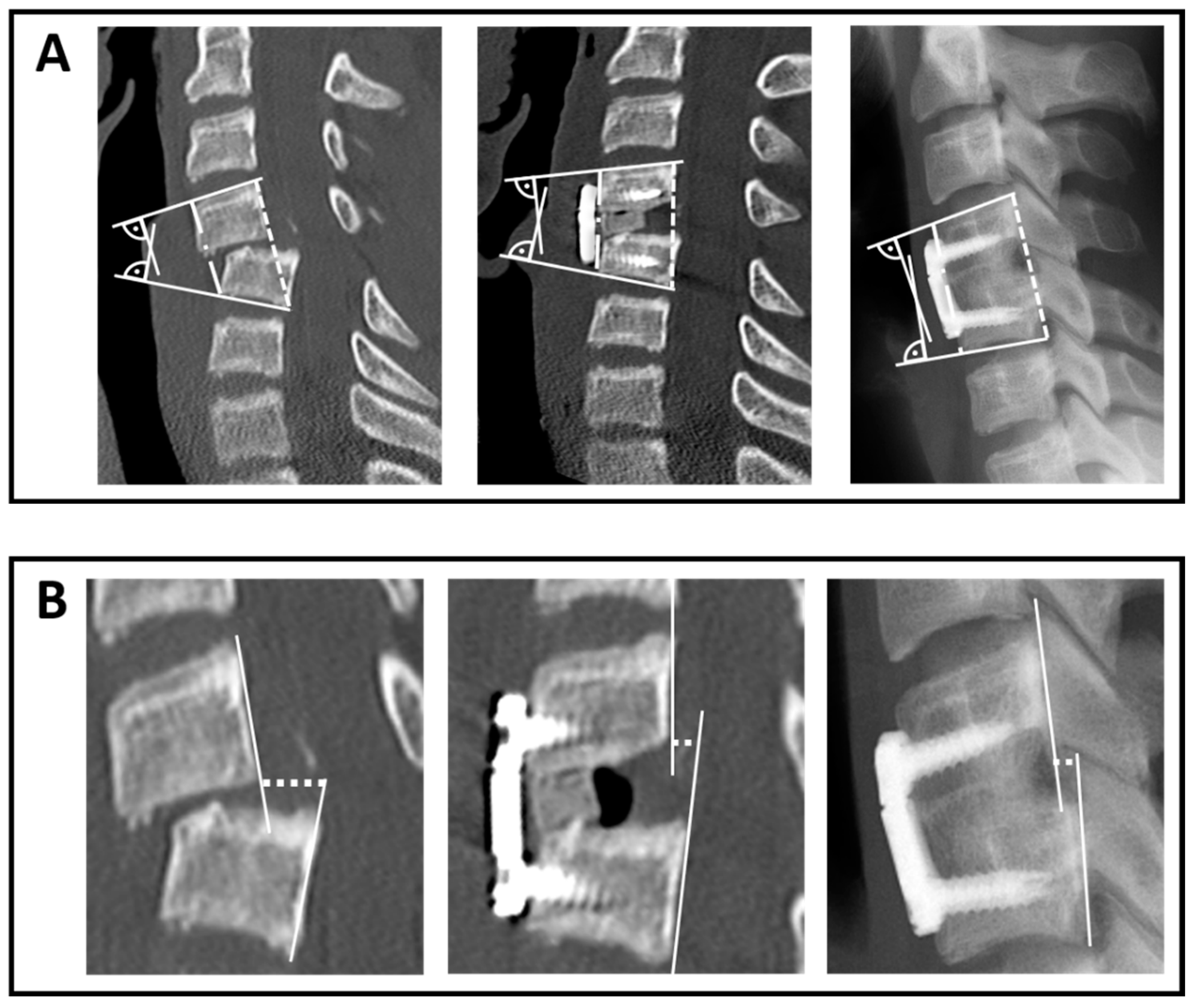
2.2. Radiographic Assessment
2.3. Patient-Reported Outcome Measures (PROM)
2.4. Statistics
3. Results
3.1. Demographics
3.2. Trauma Mechanism and Fracture Classification
3.3. Treatment Strategy and Complications
3.4. Adverse Events
3.5. Radiological Outcome
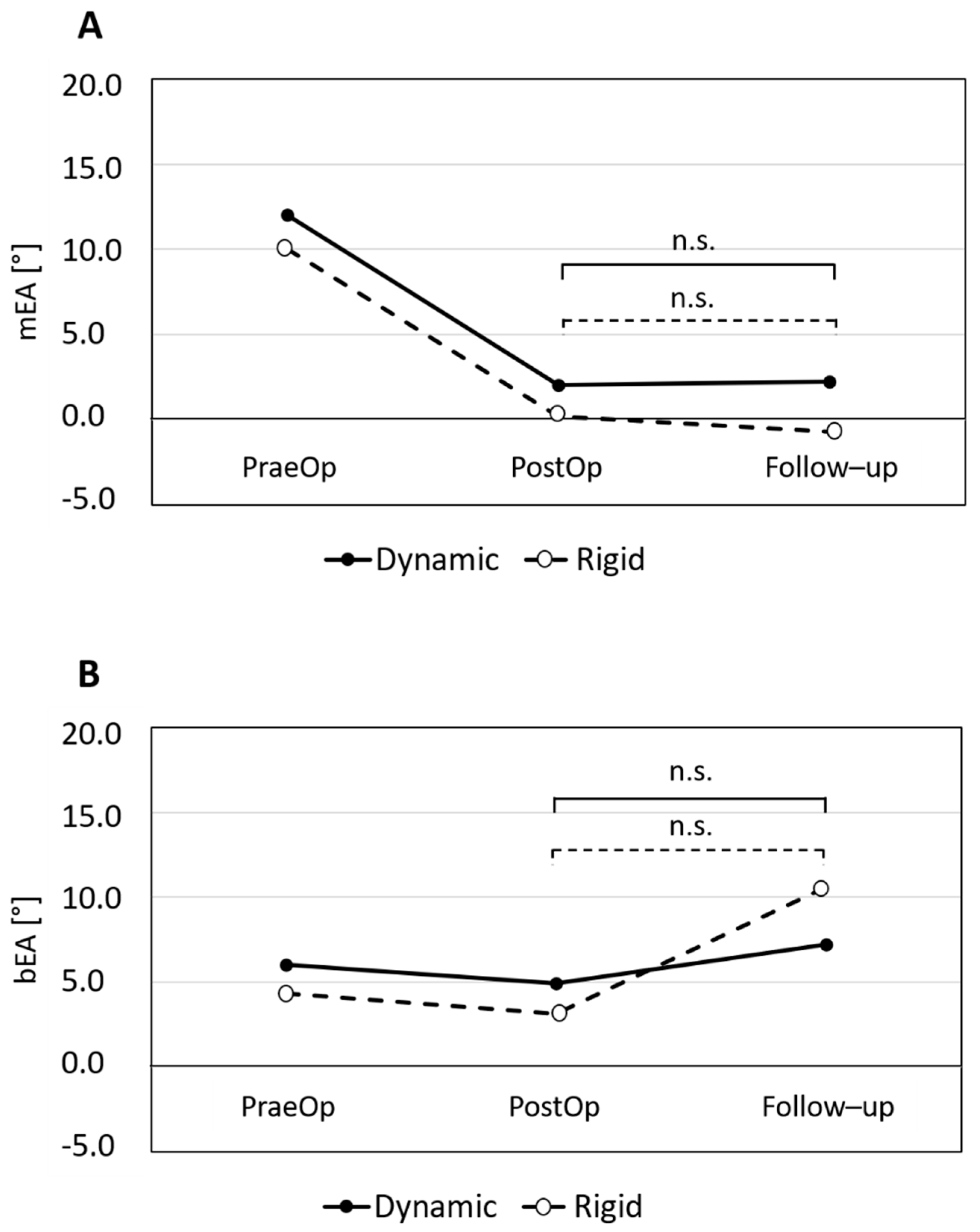
3.5.1. Reduction and Loss of Reduction in Terms of mEA and bEA
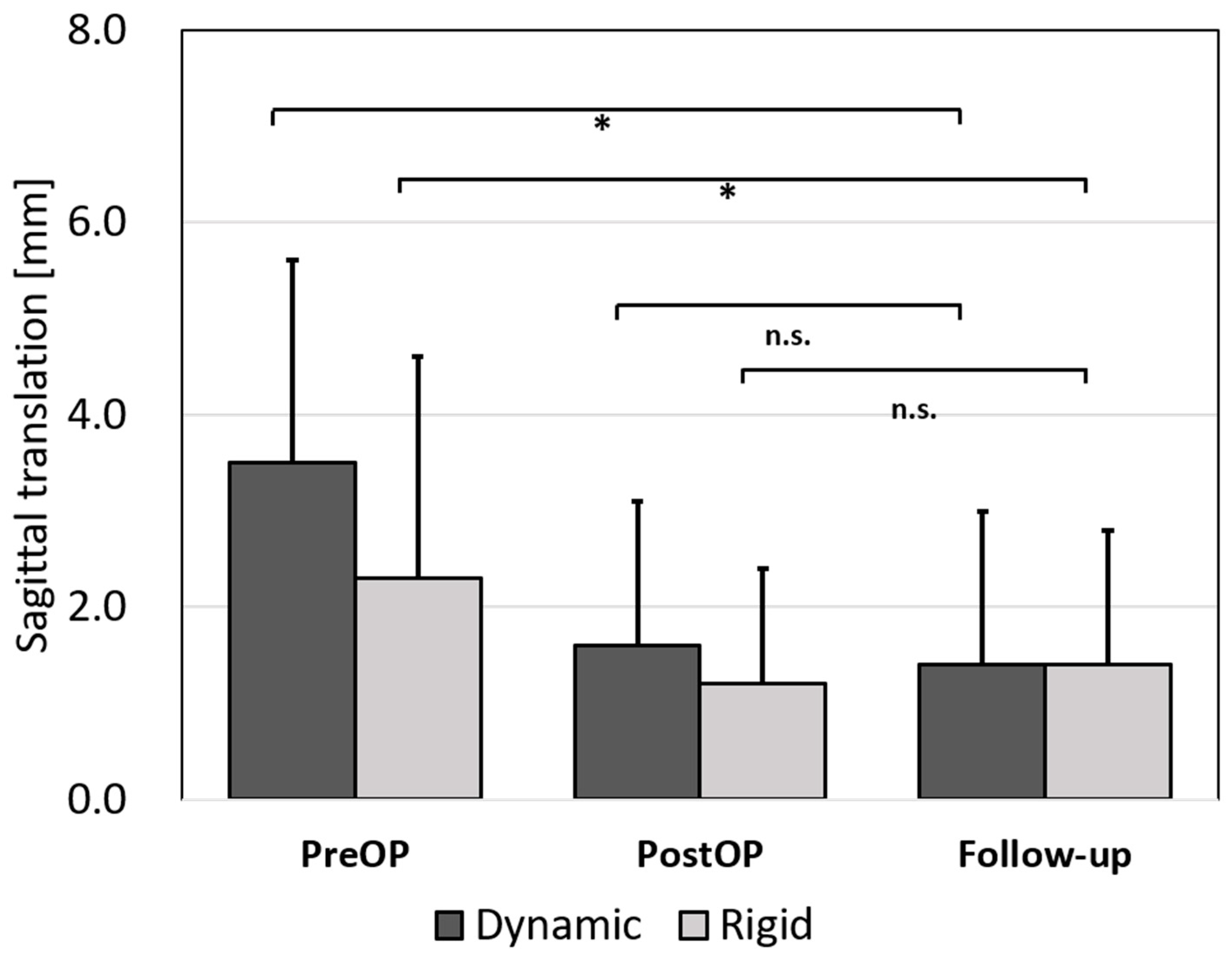
3.5.2. Anterior Translation
3.5.3. The Anterior Wall and Posterior Elements
3.5.4. Fusion Rate
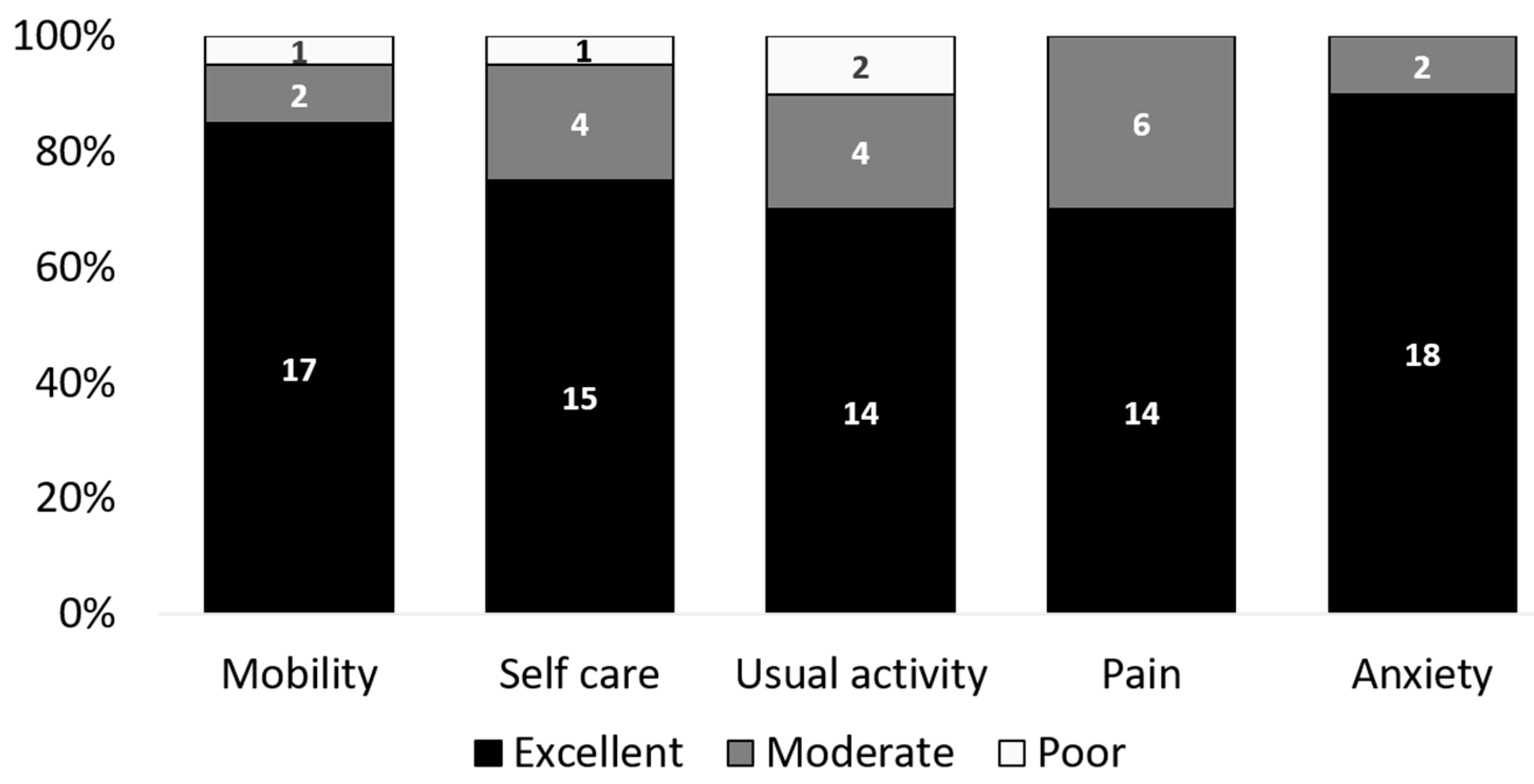
3.6. Health-Related Quality of Life
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Srikhande, N.N.; Kumar, V.K.; Kiran, N.S.; Ghosh, A.; Pal, R.; Moscote-Salazar, L.R.; Kumar, V.A.; Reddy, V.V.; Agrawal, A. Clinical presentation and outcome after anterior cervical discectomy and fusion for degenerative cervical disc disease. J. Craniovertebral Junction Spine 2019, 10, 28–32. [Google Scholar]
- Oliver, J.D.; Goncalves, S.; Kerezoudis, P.; Alvi, M.A.; Freedman, B.A.; Nassr, A.; Bydon, M. Comparison of Outcomes for Anterior Cervical Discectomy and Fusion with and Without Anterior Plate Fixation: A Systematic Review and Meta-Analysis. Spine 2018, 43, E413–E422. [Google Scholar] [CrossRef] [PubMed]
- Bailey, R.W.; Badgley, C.E. Stabilization of the cervical spine by anterior fusion. J. Bone Jt. Surg. Am. 1960, 42-A, 565–594. [Google Scholar] [CrossRef]
- Smith, G.W.; Robinson, R.A. The treatment of certain cervical-spine disorders by anterior removal of the intervertebral disc and interbody fusion. J. Bone Jt. Surg. Am. 1958, 40-A, 607–624. [Google Scholar] [CrossRef]
- Geisler, F.H.; Caspar, W.; Pitzen, T.; Johnson, T.A. Reoperation in patients after anterior cervical plate stabilization in degenerative disease. Spine 1998, 23, 911–920. [Google Scholar] [CrossRef]
- Caspar, W.; Geisler, F.H.; Pitzen, T.; Johnson, T.A. Anterior cervical plate stabilization in one- and two-level degenerative disease: Overtreatment or benefit? J. Spinal Disord. 1998, 11, 1–11. [Google Scholar] [CrossRef]
- Campos, R.R.; Botelho, R.V. Systematic review of the effect of dynamic fixation systems compared with rigid fixation in the anterior cervical spine. Eur. Spine J. 2014, 23, 298–304. [Google Scholar] [CrossRef] [PubMed]
- Li, H.; Min, J.; Zhang, Q.; Yuan, Y.; Wang, D. Dynamic cervical plate versus static cervical plate in the anterior cervical discectomy and fusion: A systematic review. Eur. J. Orthop. Surg. Traumatol. Orthop. Traumatol. 2013, 23 (Suppl. 1), S41–S46. [Google Scholar] [CrossRef]
- Nunley, P.D.; Jawahar, A.; Kerr, E.J.; Cavanaugh, D.A.; Howard, C.; Brandao, S.M. Choice of plate may affect outcomes for single versus multilevel ACDF: Results of a prospective randomized single-blind trial. Spine J. Off. J. N. Am. Spine Soc. 2009, 9, 121–127. [Google Scholar] [CrossRef] [PubMed]
- Pitzen, T.R.; Chrobok, J.; Stulik, J.; Ruffing, S.; Drumm, J.; Sova, L.; Kucera, R.; Vyskocil, T.; Steudel, W.I. Implant complications, fusion, loss of lordosis, and outcome after anterior cervical plating with dynamic or rigid plates: Two-year results of a multi-centric, randomized, controlled study. Spine 2009, 34, 641–646. [Google Scholar] [CrossRef]
- Pitzen, T.; Lane, C.; Goertzen, D.; Dvorak, M.; Fisher, C.; Barbier, D.; Steudel, W.I.; Oxland, T. Anterior cervical plate fixation: Biomechanical effectiveness as a function of posterior element injury. J. Neurosurg. 2003, 99 (Suppl. 1), 84–90. [Google Scholar] [CrossRef]
- Schleicher, P.; Kobbe, P.; Kandziora, F.; Scholz, M.; Badke, A.; Brakopp, F.; Ekkerlein, H.; Gercek, E.; Hartensuer, R.; Hartung, P.; et al. Treatment of Injuries to the Subaxial Cervical Spine: Recommendations of the Spine Section of the German Society for Orthopaedics and Trauma (DGOU). Glob. Spine J. 2018, 8 (Suppl. 2), 25S–33S. [Google Scholar] [CrossRef]
- Bullinger, M. German translation and psychometric testing of the SF-36 Health Survey: Preliminary results from the IQOLA Project. International Quality of Life Assessment. Soc. Sci. Med. 1995, 41, 1359–1366. [Google Scholar] [CrossRef]
- Vernon, H. The Neck Disability Index: State-of-the-art, 1991–2008. J. Manip. Physiol. Ther. 2008, 31, 491–502. [Google Scholar] [CrossRef]
- Ellert, U.; Kurth, B.M. Health related quality of life in adults in Germany: Results of the German Health Interview and Examination Survey for Adults (DEGS1). Bundesgesundheitsblatt Gesundh. Gesundh. 2013, 56, 643–649. [Google Scholar] [CrossRef]
- Hinz, A.; Klaiberg, A.; Brähler, E.; König, H.-H. The Quality of Life Questionnaire EQ-5D: Modelling and norm values for the general population. Psychother. Psychosom. Med. Psychol. 2006, 56, 42–48. [Google Scholar] [CrossRef]
- Aebi, M.; Zuber, K.; Marchesi, D. Treatment of cervical spine injuries with anterior plating. Indications, techniques, and results. Spine 1991, 16 (Suppl. 3), S38–S45. [Google Scholar] [CrossRef] [PubMed]
- Razack, N.; Green, B.A.; Levi, A.D. The management of traumatic cervical bilateral facet fracture-dislocations with unicortical anterior plates. J. Spinal Disord. 2000, 13, 374–381. [Google Scholar] [CrossRef] [PubMed]
- Goldberg, G.; Albert, T.J.; Vaccaro, A.R.; Hilibrand, A.S.; Anderson, D.G.; Wharton, N. Short-term comparison of cervical fusion with static and dynamic plating using computerized motion analysis. Spine 2007, 32, E371–E375. [Google Scholar] [CrossRef]
- Fernández-Fairen, M.; Alvarado, E.; Torres, A. Eleven-Year Follow-Up of Two Cohorts of Patients Comparing Stand-Alone Porous Tantalum Cage Versus Autologous Bone Graft and Plating in Anterior Cervical Fusions. World Neurosurg. 2019, 122, e156–e167. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.Q.; Kow, C.Y.; Ng, J.S.; Chan, P.; Ton, L.; Etherington, G.; Liew, S.; Hunn, M.; Fitzgerald, M.; Tee, J. Correlation of Anterior Interbody Graft Choice with Patient-Reported Outcomes in Cervical Spine Trauma. Glob. Spine J. 2019, 9, 735–742. [Google Scholar] [CrossRef] [PubMed]
- Johnson, M.G.; Fisher, C.G.; Boyd, M.; Pitzen, T.; Oxland, T.R.; Dvorak, M.F. The radiographic failure of single segment anterior cervical plate fixation in traumatic cervical flexion distraction injuries. Spine 2004, 29, 2815–2820. [Google Scholar] [CrossRef] [PubMed]
- DuBois, C.M.; Bolt, P.M.; Todd, A.G.; Gupta, P.; Wetzel, F.T.; Phillips, F.M. Static versus dynamic plating for multilevel anterior cervical discectomy and fusion. Spine J. Off. J. N. Am. Spine Soc. 2007, 7, 188–193. [Google Scholar] [CrossRef] [PubMed]
- Stancić, M.; Margetić, P.; Elabjer, E.; Milosević, M. Axial vs. angular dynamization of anterior cervical fusion implants. Coll. Antropol. 2008, 32, 221–229. [Google Scholar]
| Dynamic Plate Design n = 13 | Rigid Plate Design n = 20 | p | |
|---|---|---|---|
| Mean age [years] | 47.9 ± 24.5 | 48.5 ± 21.3 | 0.95 |
| Female | n = 4 (30.8%) | n = 4 (20.0%) | |
| Male | n = 9 (69.2%) | n = 16 (80.0%) | 0.49 |
| Polytrauma | n = 6 (46.2%) | n = 8 (40.0%) | 0.73 |
| ICBG | n = 10 (76.9%) | n = 17 (85.0%) | 0.71 |
| Cage | n = 3 (23.1%) | n = 3 (15.0%) | |
| AO Type A | n = 4 (30.8%) | n = 3 (15.0%) | 0.64 |
| AO Type B | n = 2 (15.4%) | n = 5 (25.0%) | |
| AO Type C | n = 7 (53.8%) | n = 12 (60.0%) |
| SF-36 Item | German Reference Population 2013 [15] | Study Population ISS < 16 (n = 13) | p |
|---|---|---|---|
| Physical functioning | 89.5 (88.3–90.7) | 75.0 ± 33.8 | 0.166 |
| Role physical | 85.5 (84.1–86.9) | 68.8 ± 37.1 | 0.146 |
| Role emotional | 86.8 (85.3–88.2) | 69.4 ± 38.8 | 0.150 |
| Vitality | 60.7 (59.4–61.9) | 55.8 ± 20.5 | 0.429 |
| Emotional Well-Being | 72.8 (71.6–73.9) | 74.7 ± 18.2 | 0.730 |
| Social functioning | 85.6 (84.2–87.1) | 82.3 ± 27.4 | 0.684 |
| Bodily Pain | 75.3 (73.6–76.9) | 76.1 ± 23.4 | 0.910 |
| General health | 69.9 (68.8–71.1) | 67.0 ± 19.3 | 0.608 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lang, S.; Neumann, C.; Fiedler, L.; Alt, V.; Loibl, M.; Kerschbaum, M. Does Dynamic Anterior Plate Fixation Provide Adequate Stability for Traumatic Subaxial Cervical Spine Fractures at Mid-Term Follow-Up? J. Clin. Med. 2021, 10, 1185. https://doi.org/10.3390/jcm10061185
Lang S, Neumann C, Fiedler L, Alt V, Loibl M, Kerschbaum M. Does Dynamic Anterior Plate Fixation Provide Adequate Stability for Traumatic Subaxial Cervical Spine Fractures at Mid-Term Follow-Up? Journal of Clinical Medicine. 2021; 10(6):1185. https://doi.org/10.3390/jcm10061185
Chicago/Turabian StyleLang, Siegmund, Carsten Neumann, Lasse Fiedler, Volker Alt, Markus Loibl, and Maximilian Kerschbaum. 2021. "Does Dynamic Anterior Plate Fixation Provide Adequate Stability for Traumatic Subaxial Cervical Spine Fractures at Mid-Term Follow-Up?" Journal of Clinical Medicine 10, no. 6: 1185. https://doi.org/10.3390/jcm10061185
APA StyleLang, S., Neumann, C., Fiedler, L., Alt, V., Loibl, M., & Kerschbaum, M. (2021). Does Dynamic Anterior Plate Fixation Provide Adequate Stability for Traumatic Subaxial Cervical Spine Fractures at Mid-Term Follow-Up? Journal of Clinical Medicine, 10(6), 1185. https://doi.org/10.3390/jcm10061185








